Need Breakfast In A Hurry? Here’s Your Answer
You’re in a hurry to get the kids out the door to school.
And you have an early appointment or a deadline to make at work.
But your little ones need something tasty and nutritious to eat.
You should eat, too, but who has time to feed yourself?
Take a deep breath to calm your stress levels. Because we’ve got an egg-cellent idea.
This egg recipe makes it easy to feed your kids in the morning. It also snatches away all your excuses to deprive yourself of much-needed nutrients.
It’s perfect for breakfasts on the run or something healthy to put in your kid’s lunch box. Or maybe you want a high-protein snack to balance your blood sugar and take away those cravings for sweets.
If you’re pregnant, it’s a great way to give your baby’s brain extra choline, a nutrient your little one needs for good memory.
When I learned this egg-making hack, I never went back. I doubt you will either!
My absolute favorite part of this recipe? The eggs peel effortlessly – no more stuck-on shell!
Helpful hints: Use the freshest, pasture-raised eggs possible. And watch your timer. If you forget, there are no refunds. ☺ The shell may stick.
Perfect Steamed, Not Boiled Eggs!
Ingredients:
- Any number of eggs
- Pot of boiling water
- Steaming basket
Directions:
- Add water to just reach the bottom of the steam basket.
- Bring to a rolling boil – not just tiny bubbles. It must be making steam.
- Add eggs to the basket in a single layer.
- This is the important part – Set your timer!
- Steam for 6 minutes for very soft boiled eggs, 7 minutes for somewhat soft boiled, or 10 minutes for hard boiled.
- When the timer goes off, run eggs under cold water, or plop them in an ice bath if you’re less lazy than I am. Even if you skip this step, the steam helps separate the shell from the egg, so the eggs will generally peel perfectly. They may just keep cooking a bit longer.
Voila! Fast, easy, nutritious, and delicious.
Eat What You Love Again This Holiday Season and Beyond
Everyone is gathered around the holiday table eating pumpkin pie. But not you. You know how you’ll feel after eating it.
Bloated.
Your tummy will hurt.
Lots of gas.
Maybe your skin will break out or start itching or you’ll be overwhelmed by fatigue.
Such a beautiful-looking pie and you can’t even have a bite. You sigh. It’s like the culinary equivalent of the Grinch Who Stole Christmas. You’re a mean one, Mr. Pie.
And the problem isn’t just the pumpkin pie. It’s all the carbs served with a traditional holiday dinner.
That’s how my patient, who I’ll call Jane, felt. When she first arrived in my office, she dreaded Thanksgiving and the holidays. She knew that if she touched any of the sweet treats or high-carb foods she’d pay the price.
That was until I pinpointed the root causes of her problem. Now, she actually looks forward to the holidays because she can indulge in the edible offerings of the season while still feeling healthy and well.
Yes, it’s possible. How did we do it? And how can you get rid of bloating, abdominal pain, gluten intolerance and more? You’ll discover the answers to these questions and more in this blog post.
A Frustrating Time in Jane’s Life
When Jane first arrived in my office in 2019, she was 12 weeks pregnant with her fourth child. She was having a super hard time and needed relief asap.
For starters, she was exhausted. She’d been pregnant or breastfeeding for the last seven years. She also homeschooled all of her children.
Her tummy hurt, she had near-constant gas, she was bloated and constipated. As if that wasn’t enough fun, she also had gnarly acne, painful canker sores, and regularly itchy ears, scalp, arms, and legs. Her eyes often crusted over in the morning.
She had been barely getting by eating a basic diet. She could only eat clean proteins with olive oil and salt along with above-ground veggies. If she ate anything else her symptoms flared. She couldn’t eat starches and only a little, if any, fruit. Eating nuts gave her canker sores.
As you can imagine, she dreaded Thanksgiving and the holidays. She couldn’t eat turkey if the brine had even a little sugar in it. She couldn’t have stuffing, even if it was gluten-free. And forget about anything high-carb.
No mashed potatoes and gravy. No grains. No dairy.
Can you relate?
Nothing Seemed To Work For Good
It had been six years since she felt “good.” Back then, she was on the Gut and Psychology Syndrome (GAPS) diet. This type of diet addresses the connection between the gut and brain and is often used to heal the gut. It includes meat, fish, eggs, fruit, non-starchy vegetables, and fermented foods.
But Jane had to stick with the GAPS diet religiously, and even then some of her symptoms lingered. After being on the diet, her digestion wasn’t painful anymore and she stopped catching every cold and flu that went around, but she still suffered from daily bloating and constipation.
Jane’s problems actually dated back to before the age of 10. Back then, she had frequent tummy pain. Her parents took her to the doctor a bunch of times, but no one could figure out what was wrong.
In college, doctors put Jane on the drug Accutane for her acne. If I had a dollar for every patient of mine who told me this was part of their history! Accutane devastates the gut microbiome and detoxification. The gut microbiome is the collection of bacteria, both good and bad, that live in your intestines and tune your metabolism, brain, gut health, and immune system.
Even worse, doctors make women take birth control while on Accutane because it can cause birth defects. The birth control sends women into a state of estrogen dominance, which only makes their problem worse.
Not surprisingly, Jane’s stomach pain got worse over the years. In her early 20s, Jane went on a gluten-free diet and the pain went away for a while. But it ultimately came back.
The First Red Flag
During our first appointment, Jane mentioned she had a front-loading washer. It smelled musty and she’d seen mold in it. Gross, right?
In her old house, the washer was in the basement and she could leave the door wide open to reduce the mold. Now the washer was on the main floor in her new house and there was foot traffic, so she had to keep the door closed. The musty smell grew worse.
Helpful hint: get rid of your front-loading washer, like yesterday!
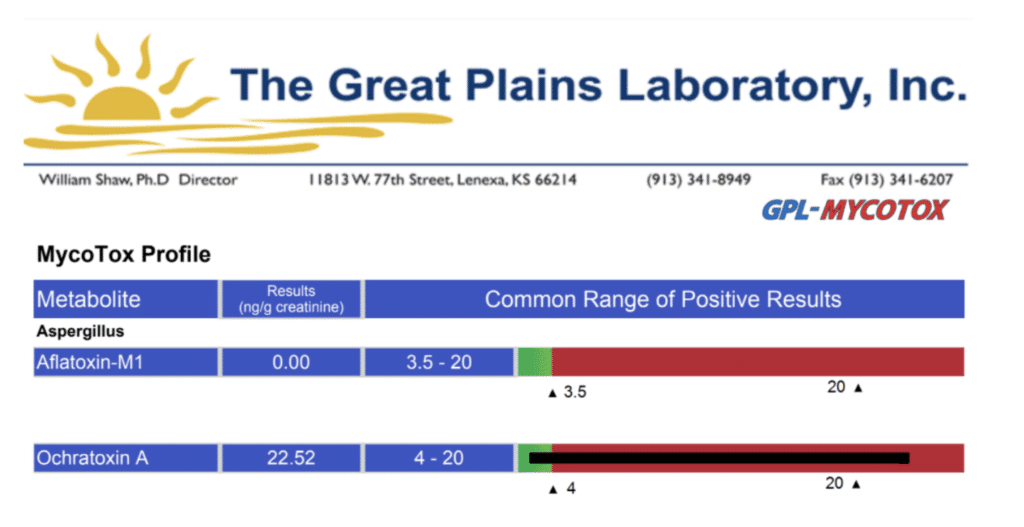
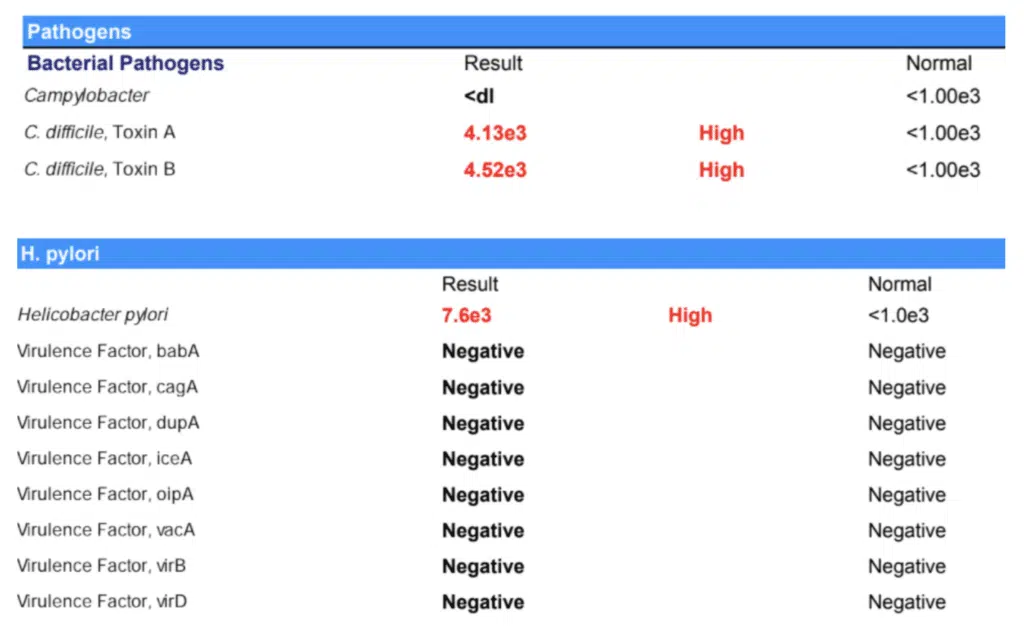
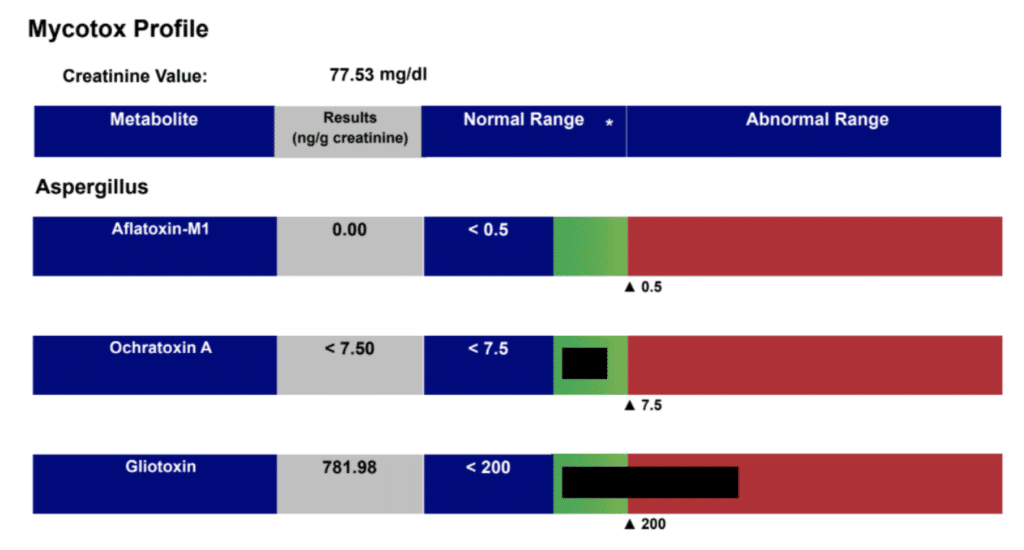
The presence of the moldy washer led me to order a mycotoxin test, which identifies toxins from mold. The result? Jane had HUGE amounts of a type of toxin known as ochratoxin, which are produced by some Aspergillus species of black mold.
Other tests I ordered were:
- GI-MAP stool panel, which detects parasites, bacterial and viral dysbiosis, and Candida
- Organix panel, which identifies nutrient deficiencies and metabolic imbalances
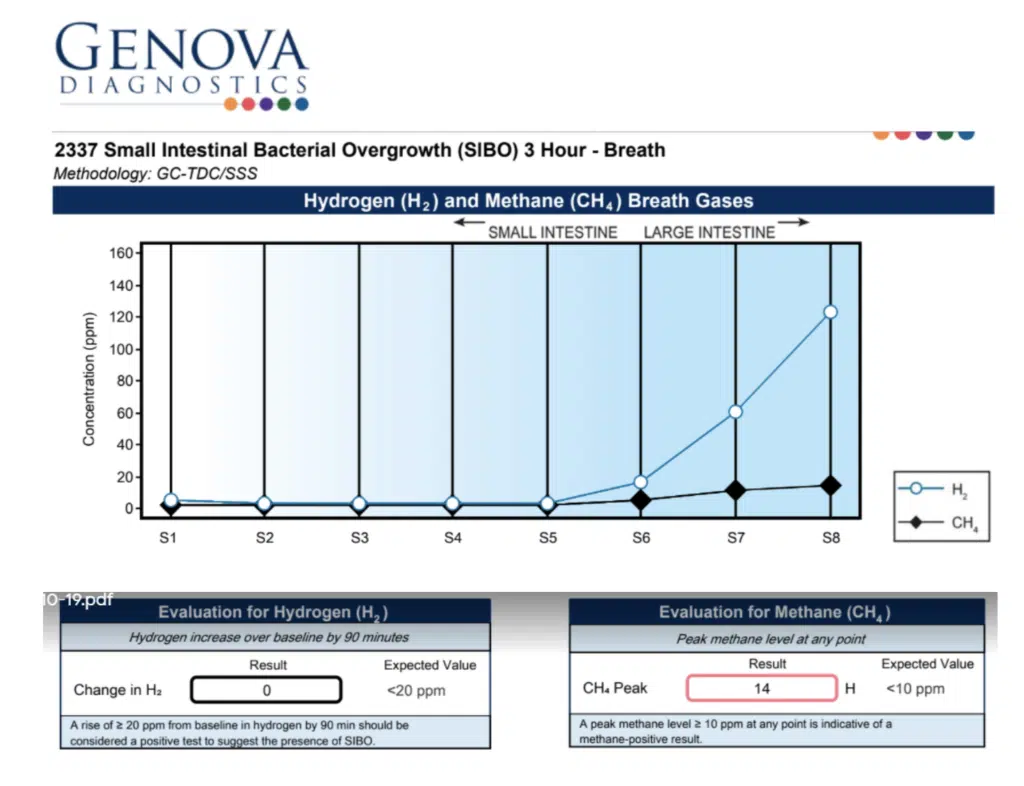
- Small-intestinal bacterial overgrowth (SIBO) breath test, to determine if she had SIBO, a condition where there is an abnormal increase in the bacteria population of the small intestine, which can cause diarrhea, weight loss, and malnutrition. Jane actually requested this test, after reading about SIBO symptoms in a blog post I had written.
A Trio of Test Results
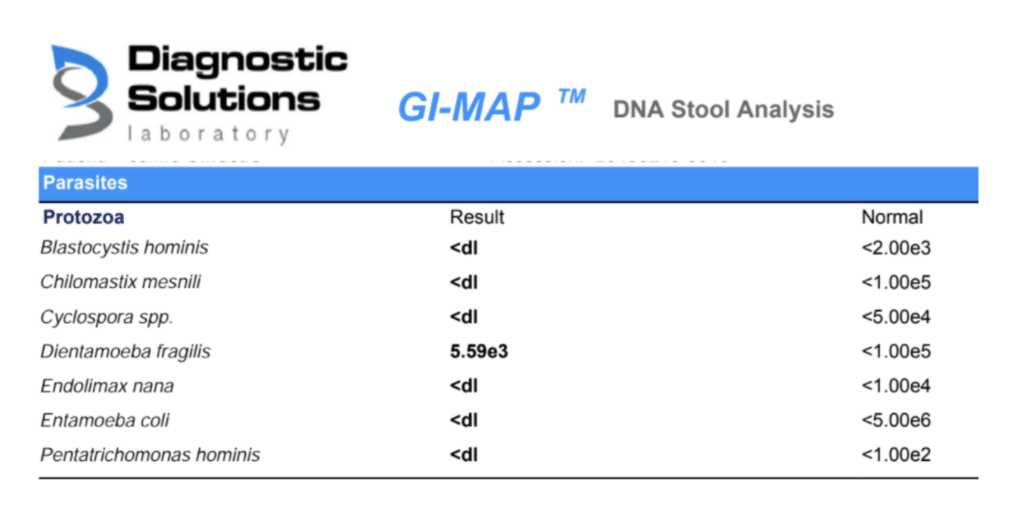
The GI-MAP stool test revealed Jane had an amoeba parasite called Dientamoeba fragilis, which can live in the large intestines of people. This little bug often causes no symptoms, but in some people it can lead to diarrhea and abdominal pain, as well as loss of appetite, nausea, and fatigue.
Jane’s Candida levels were through the roof. And her SIBO test came out positive. She had a type of SIBO known as methane dominant (IMO). This type of SIBO is caused by an overgrowth of single-celled organisms called archaea. It can cause constipation as well as bloating and gas.
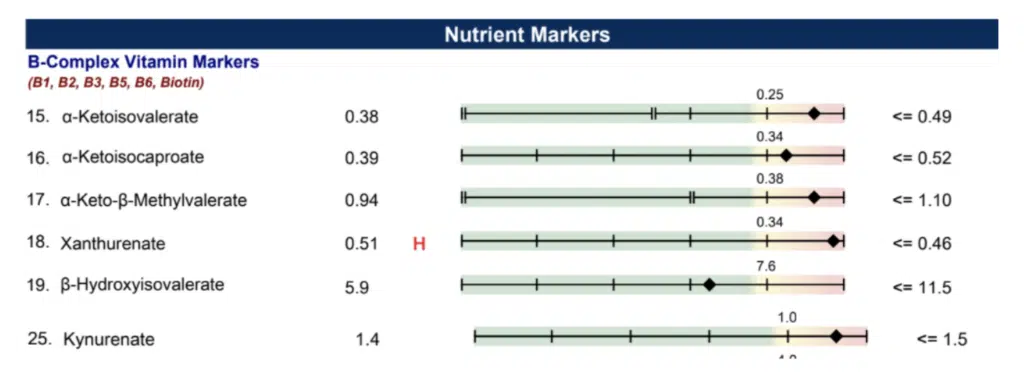
And what about Jane’s Organix test? That showed she was deficient in some nutrients. She needed B vitamins, especially vitamin B6.
Helping a Pregnant Jane Feel Better
In most patients I would have treated the mycotoxin right away, but because she was pregnant I had to put the brakes on that approach. Otherwise, the mold could end up in her breast milk as she was detoxifying.
Until she finished nursing, I decided to focus more on healing her gut and resolving her gut symptoms. Here’s what I did at first:
- I gave her enzymes and hydrochloric acid to improve her digestion. I gave her some nutrients and herbs to help her with constipation.
- I put her on a low-FODMAP diet for the short term, but only because she was in such extremely bad shape. If you’re pregnant, don’t try this type of diet at home! It’s hard to follow this diet and get all the nutrients you need for you and the baby. You need a trained practitioner to supervise. However, for Jane, it reduced her symptoms and it was only for a short period, so it was worth it!
- I had her take several supplements including L-glutamine to heal the gut and butyrate and probiotics to balance her gut microbiome. I also gave her gentle herbs to reduce gas and bloating and encourage more frequent and complete bowel movements. For example, she used stone root (Collinsonia), a safe and effective way to promote better BMs in pregnancy.
- Suggested she avoid electromagnetic fields (EMFs) for the health of her and her baby. She noted that this dramatically shifted her symptoms in a short time.
Taking the Next Step to Feeling Well Again
After Jane finished nursing we went after her parasite first. Jane started doing coffee enemas and taking anti-parasitic herbal supplements. At the same time, I wanted to make sure she was making healthy amounts of bile, so I gave her phosphatidylcholine and a liver-supporting supplement known as TUDCA.
Next, we went after the mold toxins. I had her take supplements to detoxify her body of the Aspergillus mycotoxin. These included liposomal glutathione, binders specific to the mycotoxins she showed on her tests, antioxidants, and Quinton liquid, which helps transport toxins out of cells. I also suggested she have mold remediation done on her home. And aha! As I suspected, the problem went beyond the front-loading washer: the remediator found mold in the home’s air ducts.
This wasn’t an overnight treatment. She needed two rounds of the anti-mold supplements, three months per round, with retesting in between.
At the same time, Jane continued to work on healing her gut. She took digestive enzymes, L-glutamine, and Tributyrin-X™, a postbiotic butyrate supplement that promotes gut health, heals the intestinal walls, and encourages regular bowel movements.
At this point, as treatment unfolded, she had less indigestion and gas.
Getting rid of the mold was HUGE!
Things were looking up—but they still weren’t perfect.
Digging Deeper to Heal the Gut
Jane began an anti-Candida protocol. But those stubborn little fungi refused to be beaten.
I decided to retest her gut. And guess what showed up to the party? She was infected with high levels of two critters: C. difficile and H. pylori.
She’d probably picked up these bacteria after taking antibiotics for persistent diarrhea and fever during an earlier pregnancy with her third child. The antibiotics made the diarrhea and fever go away but she developed bronchitis. And guess what? The doctor gave her more antibiotics and she developed a vaginal infection. This was probably because the antibiotics caused a flare-up of the Candida. She was given yet more antibiotics. All that during pregnancy!
H. pylori and Candida often go hand in hand. As I’ve written about before, they often work as a team, so getting rid of one helped get rid of the other. Likewise, I have seen that C. difficile always exists in tandem with Candida overgrowth.
In order to tackle the C. difficile and H. pylori, we put the mold treatment on intermission. Once we got rid of these two bacteria, her symptoms were better. And she could finally say goodbye to her Candida overgrowth.
To address the vitamin B6 deficiency showing up in her Organix panel, she started supplementing with this nutrient. Vitamin B6 is important for brain development and keeping the nervous system and immune system healthy. Vitamin B6 plays an important role in the immune system of the intestines. The friendly flora of the gut also need vitamin B6 and other B vitamins to do their job well.
Take a look at her follow-up results for ochratoxin A. So much better! More importantly, this was associated with her symptom reduction. I always look at lab results in the context of how the patient is feeling. This is as much- or more- important than what we see on lab results!
This whole process isn’t an overnight fix. It can take nine months or more. This is especially true for people like Jane who have had mycotoxins, bacteria, and other harmful organisms in their gut for a long time. Jane had symptoms almost her entire life. The longer you’ve been infected, the longer it may take to heal.
Be persistent!
Moving forward, we will focus on gut repair while nourishing and rebuilding Jane’s microbiome. We will support her detoxification processes for at least six months and maybe more.
Jane Doesn’t Have To Deprive Herself Anymore
Today, Jane is feeling amazing. She can tolerate a lot more foods. She no longer gets canker sores when she eats nuts. And what about her bloating, constipation, and abdominal pain? Virtually all gone!
Thanksgiving and the holiday season are now something Jane looks forward to for the first time in years. Her body can handle stuffing, potatoes, and pumpkin pie.
It’s the same on a daily basis. Within reason, Jane can tolerate less-than-perfect foods without going into a downward spiral.
Keep in mind that this journey is different for each person. Not everyone with food sensitivities can go back to eating a spectrum of allergenic foods in quick time. And some people may have to avoid a certain allergen for life because it harms their bodies. However, in general, when we improve gut health, people can resume eating foods (in moderation) that previously sent them into a tailspin.
Eat The Foods You Love Again
Do you have food sensitivities, gluten intolerance, or digestive symptoms like bloating, abdominal pain, and gas? You don’t have to live with these forever. Like Jane and I did, you and I can work together to unearth the root cause of your problem. I’ll help you eat your favorite foods again and feel healthier while you’re doing it. Your path to better gut health begins with a free 15-minute troubleshooting call.
Safe Effective Herbal Remedies for Common Childhood Illnesses
Table of Contents:
- An Ounce of Prevention is Worth a Pound of Cure
- Is It Really a Seasonal Illness—Or Something Else?
- Children’s Remedies for Colds, Flus, or Other Ear, Nose, and Throat Symptoms
- Children’s Remedies for Belly Aches and Poor Digestion
- Children’s Remedies for Skin Irritations, Rashes, and Skin Allergies
- Children’s Remedies for Emotional Upset, Agitation, and Poor Sleep
- Don’t Be Frightened of Fevers
- Safe, At-home Remedy for Fevers
- How To Improve Children’s Immunity
---------------------------------------------------------------------------------------------------------------------------------------
You roll over in bed and open your eyes to the sound of little feet padding across the bedroom floor.
“Mama, I don’t feel so good.” Cough, cough, sniffle.
Ugh. It’s inevitable. Kids get sick. And then, you get sick. And if you have had a little one in daycare or preschool, you may have wondered if your home was getting hit with every virus on the planet, a new one seemingly every 2 weeks.
The good news? Exposure to lots of germs will build your child’s immunity. The bad news? Hearing them cough all night or struggling to breathe through a stuffed-up nose will break your heart.
What’s more, you’re not going to get the sleep you need when you’re concerned about your child. And that will do a number on your immunity, too.
And these days, you’ll also worry whether it’s just a cold or flu or whether it’s COVID.
I have a little one of my own. So I know how heart wrenching it is when a child becomes ill. That’s why I always make sure to have some child-safe dietary supplements and nutrients on hand—just in case.
In this blog, we will cover the most common illnesses that plague our little tykes and the home remedies to turn them around. Beyond seasonal colds and flus (where we will start), I’ll also go over tummy complaints, skin irritations, and emotional upset and agitation. I want you to have these tools to help your child at the earliest signs of illness, when it really counts.
Here are some of the children’s supplements I keep in my own natural home medicine chest. But first…
An Ounce of Prevention is Worth a Pound of Cure
Of course, the best strategy is to keep your child from getting sick in the first place. Nutrition is your first and most powerful tool in keeping kids’ immune systems working right.
Many of us find ourselves wondering what to feed our previously milk or formula fed babies when 6 months roll around and our newly sitting little one, with teeth, shows interest in food. If you’re like me, this caused me more than a little anxiety!
One thing to know is that at least until 12 months, food is really about exploring, introducing, and experiencing. It’s much less about nutrient intake. So don’t stress if you only get a bit or so in (or mostly in….the rest will end up on their outfit, in your hair, or on the floor. If that’s happening, you’re doing it “right”! Solid or semi-solid food can be given every few days, initially. And, even in the toddler years, it’s completely normal for kids' appetites to ebb and flow dramatically. One pediatrician wisely expressed her advice as, “Think about what they consume over a week, rather than this or that meal.”
Without going into detail on what to feed your baby and when, I will link to my favorite book on this subject HERE.
For kids who are eating solid foods, avoid processed foods and grains (fun fact: we don’t really make the digestive enzymes needed to digest grains in adequate amounts until at least 2 years of age). Focus on grass-fed animal products, pasture-raised eggs, and raw dairy. Make stocks and soups from organ meats and bones.
Most importantly, avoid sugar and fruit juice, which weakens immune cells’ ability to fight off infections. One study showed that eating 100 grams of sugar doesn’t decrease the number of immune cells (neutrophils), but it decreases how well they respond to infection. Watch out for processed grains and flours such as fruit, crackers, puffs, and chips. We want to avoid those for our children, however hard that may be. Instead, choose fruit with fiber and starchy vegetables to complement the healthy meats and eggs. And for on the go snack options (yes, i know we all love a good puff ; )-- there are now nutrient dense grain-free options like these, which contain bone broth, cassava root, and whole veggies--toddler approved!
Their pouches are really amazing as well, and include wild caught or pasture raised animal foods, healthy fats, bone broth, and high mineral organic veggies.
Is It Really a Seasonal Illness—Or Something Else?
Before reaching for dietary supplements, be certain your child’s problem is really a cold or a flu and not an imposter. Congestion, fever, hacking cough with a greenish discharge from the nose or eyes can mean your child is actually teething. Teeth breaking through the gums can cause inflammation. This mirrors symptoms of a viral or bacterial infection.
Children’s Remedies for Colds, Flus, or Other Ear, Nose, and Throat Symptoms

Traditional Chinese Medicine (TCM) is a complete system of medicine that has been used to diagnose, treat, and prevent illnesses for more than 5,000 years. As a TCM practitioner, I have seen these safe, gentle Chinese herbal formulas work wonders for congestion of the ears, nose, throat, lungs, as well as coughs, and colds. Kan is a good brand. I know because I used to work as their herbalist, and I know they test for purity and accuracy of proper composition of herbs, heavy metals, pesticides, and microbial contamination. In general, I recommend using medical grade Chinese herbal formulas that you can buy through a healthcare practitioner.
Give the TCM herbal formulas I mention below to your child when you nurse or when the child eats. Mix them in water, juice, or mashed fruit or veggies. My daughter even loves the taste directly on her tongue and asks for them! Here are general doses to keep in mind:
0-4 years: 15-30 drops, 2-4 times daily.
In very tiny babies (under 6 months), consider 3-5 drops if at all.
4-8 years, 30-45 drops, 2-4 times daily.
8-12 years: 60-90 drops, 2-4 times daily.
1 full dropper = 30 drops
In very little ones, give the TCM formulas through breast milk. If you might need to give this treatment through breast milk to your nursing infant, please consult with a trained practitioner first. Dosing varies for mothers. In general, I recommend mothers take 2 milliliters per dose, 30-45 minutes before nursing for the highest concentration in breast milk.
Immune-Boosting Nutrients
It’s best to start with the basics. Defending your child against common childhood illnesses starts with making sure he or she is nourished with the most effective children’s immune vitamins.
Vitamin C and Zinc – Both of these are immune-boosting powerhouse nutrients that can stop viruses in their tracks. Vitamin C may stop your child from getting sick in the first place. And when your child is already ill, vitamin C and zinc can shorten the amount of time your little one is sick. They can also make the illness less severe.
The bad news? Deficiencies in these nutrients are really common. Zinc deficiency is an especially big problem. That’s because an anti-nutrient known as phytate found in many cereals blocks zinc absorption. If your child gets a lot of upper respiratory tract infections like colds or respiratory flus, you can probably blame it on zinc deficiency. Giving kids zinc reduces the risk of respiratory infections and their duration.
Signs of low zinc:
- Growth retardation
- Neuro-sensory disorders or cognitive impairment
- Rough skin (bumps on arms is need for omega-3 fats or vitamin A usually)
- Lowered immunity
- Signs of depression and ADHD correlation
Vitamin D – This is another nutrient important for immunity. And many people are deficient. We live in a sun-starved society where people stay indoors for fear of getting skin cancer or are simply too busy to step outside.
I give my kid a sugar-free vitamin D gummy every day. Just be certain your child is old enough to chew, otherwise this type of vitamin D is a choking hazard. You can use vitamin D drops for very young kids who can’t chew and make sure you’re getting enough vitamin D yourself, especially if you’re breastfeeding.
Multivitamin – Still breastfeeding? Then make sure you’re taking a good prenatal vitamin. For children who are older and able to chew, I like Xymogen Kids Chewable Multi.
Anti-Viral Supplement
Monolaurin – This coconut-oil-derived supplement hits the virus where it counts: its protective lipid shield, which destroys the virus’ main defense. South Pacific islanders who ate a lot of coconuts had almost no colds or flus compared to other non-coconut-eating native peoples.
Monolaurin is one of my favorite children’s cold or flu remedies. You can give your child monolaurin proactively or at the first signs of a cold or stomach flu. This reduces their symptoms and speeds up their healing. The product I like is called Lauricidin. The mini pellets should be swallowed with water or juice or placed in apple sauce, pudding, or peanut butter.
Immune Support
Probiotics – These friendly flora do double duty. They can keep children healthy over the long-term and reduce symptoms when your little one is sick. They’re especially good at reducing symptoms of colds and flus and fending off the ear infection known as otitis. I’m particularly fond of Klaire Labs Ther-biotic for Infants powder and Klaire Labs Ther-Biotic Children’s Chewable. Garden of Life Gummy Probiotics is another good one for children who can chew, as is RAW Probiotics Kids.
Colostrum – This is a fluid released from the breasts of female humans, cows, and other mammals after they’ve given birth and before breast milk is released. It’s a powerful immune-booster packed with antibodies that fight infections. This is an important supplement for infants who aren’t breastfed, are under six months old, and who have GI issues. Keep in mind that taking too much colostrum can cause constipation and the non-spray form has dairy. My favorite product is PRP Spray.
Myco-Forte Liquid – This moisturizing supplement is a good choice to support immunity in kids with dry mucous membranes and respiratory tracts. Ideal for kids who tend to have dry skin or get a dry, barking cough when they get sick.
DHA – An omega-3 fatty acid, DHA fortifies kids’ immune and respiratory function in utero and during developmental stages in childhood. DHA also prevents asthma attacks. And we haven’t even touched on its stellar actions for brain development! Important for mom to take during pregnancy and for kids throughout childhood and beyond.
N-Acetyl Cysteine (NAC) – This amino acid breaks up thick gunky mucous in the nasal passages and respiratory tract. It boosts the production of glutathione, the body’s master antioxidant. One bonus: NAC may also make kids with autism less irritable and cut down on obsessive compulsive behavior like hair pulling, nail biting, and skin picking.
Bioray NDF Immune – Supports lungs, throat, and sinuses and reduces body aches during viral infections. It bolsters the immune system, calms irritability, and strengthens respiratory health. The formula contains chlorella, antioxidants from organic fruit, and naturally occurring vitamin C, zinc, copper, manganese, calcium, and potassium. Great to pair up with the two traditional Chinese medicine formulas Chest Relief and Pipe Cleaner (more on these below).
Windbreaker – A combination of Chinese cinnamon, chrysanthemum flower, Chinese mint, burdock seed, and honeysuckle flower, this formula fights an invasion of viruses and bacteria. It’s good for kids with symptoms like sneezing, coughing, runny nose, mild fever, aches, irritability, and itching or scratchy eyes, nose, and throat. Start this at the first sign of illness and continue it while your child is ill. Pair it with any of the below formulas for colds and flu.
Minor Bupleurum combined with Windbreaker – Antiviral and antibacterial, Minor B is used both to ward off colds and flus and to fight them after they’ve gotten into the body. It opens blockages, so I love this for ear infections.
Chest Relief – A combination of citrus peel, licorice, bamboo juice, and white mulberry leaf, Chest Relief formula gently clears phlegm and boosts immunity. It’s best for cough with sticky phlegm that’s hard to cough up and that’s made worse by drafts, temperature changes, or when your child is out in the wind or lying down. It’s not a good choice for severe wheezing.
Pipe Cleaner – This combination of schizandra, radish seed, and honeysuckle flower, normalizes mucous secretion and breaks up congestion and strained breathing. Best for children with symptoms like wheezing, coughing, dry throat, sticky phlegm (yellow or green), and feeling thirsty. This can be used together with Chest Relief.
Open Air – Apricot seed, tangerine peel, and Chinese cardamom team up to relax the chest, and open up air tubes in the lungs known as bronchioles. It’s good for wheezing, shallow breathing, and a cough with phlegm, as well as a dry mouth and throat. Open Air is used more for when cold or flu symptoms resemble asthma.
This Little Piggy and Other Tips
Acupressure of the feet – Massage your child’s sides of toes to open up and drain the sinuses. Gently roll each “little piggy” between your fingers.
Use a Humidifier with Eucalyptus Oil – Adding eucalyptus oil to a humidifier can fill the air with an antiviral scent.
Children’s Remedies for Belly Aches and Poor Digestion

Grow and Thrive – This is a gentle Chinese medicine formula that can help with loose stools, diarrhea, poor appetite, slow growth, indigestion, and more. It promotes digestion and assimilation of food for better nutrition and growth. It encourages food to pass smoothly through the intestines, training peristalsis (the muscular actions that squeeze food through the gastrointestinal tract). Grow and Thrive promotes a healthy gut microbiome. It contains lycii berry, Chinese hawthorn berry, tangerine peel, radish seed, fennel, magnolia bark, and toasted kudzu root.
Grow and Thrive is indicated for children with underdeveloped “spleen.”In Chinese medicine, spleen has many functions, but it somewhat correlates with our ability to digest and assimilate our food. When we can’t digest and assimilate properly, our bodies become starved for nutrients and our cells and organs malfunction. When the “spleen” is weak or underdeveloped, we will often see “dampness” in Chinese medicine. In Chinese medicine each organ system has a state of relative moisture and temperature in which it functions optimally; generally speaking, the Spleen operates better when dry and warm, and problems arise when it is cold and damp. A cold, damp spleen can show up as loose stool, drooling, poor appetite, and kids who tend to start solids later. That’s because spleen strength is required to be able to handle and use those solid foods!
When your child cuts teeth, it means that the “spleen” and “kidney” are developing well. Not to be taken literally. In Chinese medicine, “kidney” is related to the ability to develop and grow. In other words, digestion, assimilation, healthy growth, and development are underway!
This is a sign that your baby is ready for solid food introduction. What we feed them can support or hinder this development. Focus on nutrient-dense foods. For example, avoid rice cereal and opt instead for liver and egg yolk. Meat broths, veggie broths, and pureed veggies are great. Fruit in moderation.
Tummy Tamer- This formula helps move food through the intestines and counteracts indigestion, belching, gas, bloating, nausea, bad breath, or stinky poo. With cardamom, fennel, bitter orange, licorice, and water plantain, Tummy Tamer eases belly aches, slow digestion, and irregularity. It also helps relieve symptoms after eating such as nasal congestion, fatigue, or irritability. If your child has these or other food sensitivity symptoms, you will like this product. But dietary changes and addressing root causes of gut-immune imbalance are also necessary to send food sensitivities packing.
Easy Going- If your little one can’t go, this is a gentle and tasty option containing rhubarb root, flax seed, hyssop, and bitter orange fruit. It does many of the good things for digestion as Tummy Tamer but it is specifically designed for constipation. I tend to use this along with Liquid Magnesium (Douglas Laboratories) and sometimes combine it with NDF Pooper formula as well. This should be discussed with a trained practitioner if your child has ongoing constipation, but it is generally safe for occasional or short-term use.
Belly Binder- Much like Tummy Tamer above, Belly Binder moves food through the intestines and optimizes digestion, but it is specifically designed for children with diarrhea or loose stool. It contains lotus seed, Chinese yam, anemone root, and cardamom. Chronic loose stools or diarrhea aren’t normal so you may need to meet with a trained practitioner and run a stool panel to get to the root cause. But for occasional or short-term use, it is generally safe.
Any of the above 3 can be combined with NDF Tummy.
Children’s Remedies for Skin Irritations, Rashes, and Skin Allergies
Fire Fighter – This is a very energetically “cold” formula for rashes, swollen glands, or gooey leaky rashes. It’s great for infections of the eyes, ears, nose, or throat (think sinus infections or Strep throat). It clears and moves heat and toxins out of the blood using dandelion root and flower, Chinese mint, scrophularia root, and clove flower. It circulates healthy blood and oxygen to the skin and mucous membranes where it is needed. Fire Fighter can help with hives, boils, acne, or itchy insect bites or stings. It can help with mild allergic reactions and even food sensitivity symptoms. It is not for long-term use, but is very safe.
Children’s Remedies for Emotional Upset, Agitation, and Poor Sleep

NAC – Mentioned above for thinning mucus, NAC also helps to calm irritable children. It can help with hair pulling, nail biting, skin picking, children on the autism spectrum, or other signs of obsessive-compulsive disorder. It supports detoxification by making the master antioxidant, glutathione. I recommend 300 – 900 mg/day three times daily in kids over 5 years old.
NDF Focus – Improve your child’s cognitive function, focus, and his or her ability to handle stress. This is a perfect addition when your child also has a histamine response, such as seasonal allergies, runny nose, and/or itchiness. I like this in cases where ADD is a consideration. NDF Focus reduces environmental sensitivities, supports adrenal health (Eluethero, reishi mushrooms, Chinese licorice root, Schisandra berry), and liver health (milk thistle, Agaricus, Chinese licorice).
Quiet Calm - This formula clears heat from the mind and spirit, relaxes muscles and nerves, and stops spasms. It will help your little one with mood swings, crying spells, moodiness, pensiveness, anxiety, timidity, and/or tantrums. With jujube seed, Schisandra, lotus seed, mimosa tree bark, gardenia fruit, and red tangerine peel, it’s good for kids with difficulty falling asleep, staying asleep, or with nightmares. It is even more appropriate if there is mucus in the ears, throat, or sinuses.
NDF Sleepy- Good for restlessness and worry, it is similar to Quiet Calm and can help kids fall asleep more quickly. Similarly, it contains jujube seed, and albizzia bark (bigger happiness tree), which has been shown in studies to improve getting to sleep and staying asleep. It also contains dan Shen and reishi mushroom to soothe irritability and restlessness.
Quiet Calm and NDF Sleepy are very similar, some kids respond better to one over the other. I usually try one and then the other to see which is the best fit.
Nutrition plays a big part in children’s stress, anxiety, attention deficit, and mood. Check out The Better Brain, a book by premier researchers Dr.s Bonnie Kaplan and Julia Rucklidge, which explores the topic further.
Don’t Be Frightened of Fevers
Does your child spiking a fever send you into a panic? Even as a trained medical professional, the first time my child spiked a fever it was scary! We might even reach for the Tylenol (acetaminophen) to lower that fever. After all, it’s safe compared to aspirin, right? Nope. Tylenol (Acetaminophen) in excess is well known to harm the liver. Tylenol is tied to increased risk of asthma, eczema, allergies, and runny nose. All of these are symptoms of liver toxicity and leaky gut, indicating Tylenol could contribute to these two conditions.

Even worse, Tylenol is dangerous when mixed with other drugs. Every year there are 100,000 calls to poison control centers and 450 deaths from Tylenol-caused liver failure alone. Acetaminophen causes more cases of acute liver failure than all other medications combined.
Listen; I’m not saying don’t ever use Tylenol. Just think twice about whether your child really needs it. Consider leaning on the natural remedies mentioned earlier, first, when your child is feverish, coughing, or congested. Generally, fevers under 102 degrees are not something to worry about. Viruses like cold. They don’t like heat. A fever sends the virus on a one-way trip to the Sahara desert, where it heats and destroys the little bugs and stops them from thriving. The faster your child burns off the virus, the sooner they will be feeling good again!
That said, if you are confused or think you need to seek medical help for your child with a fever, then by all means do so. Your intuition is primary!
Here are some general rules of thumb about navigating your child’s fevers.
Seek medical attention for:
- Babies under 3 months with a fever of 100.4 or higher
- Babies between 3 and 6 months with a fever of 101°F (39°C) or higher
- Kids over age 3 with a fever over 102° F that lasts for 2 or more days
Seek medical attention right away if your feverish child has these symptoms:
- Trouble feeding (nursing)
- Trouble breathing
- Rashes
- Vomiting or diarrhea
- Inconsolable
- Lethargic and drowsy, less responsive, or trouble waking up
- Lowered urine output or not pooping (if very young)
- Rapid or strained breathing
- Rapid pulse
- Body or neck seem stiff
Herbs can help lower fever in children but you will need to discuss this with your trained healthcare provider.
Safe, At-home Remedy for Fevers
Here is an old Chinese medicine treatment, called the “Lemon Wrap,” to lower fever. It is safe to try at home, and especially when fevers are on the lower end and not accompanied by any of the symptoms mentioned above. I have used it with babies older than 6 months, and with toddlers, with fevers higher than that mentioned above.
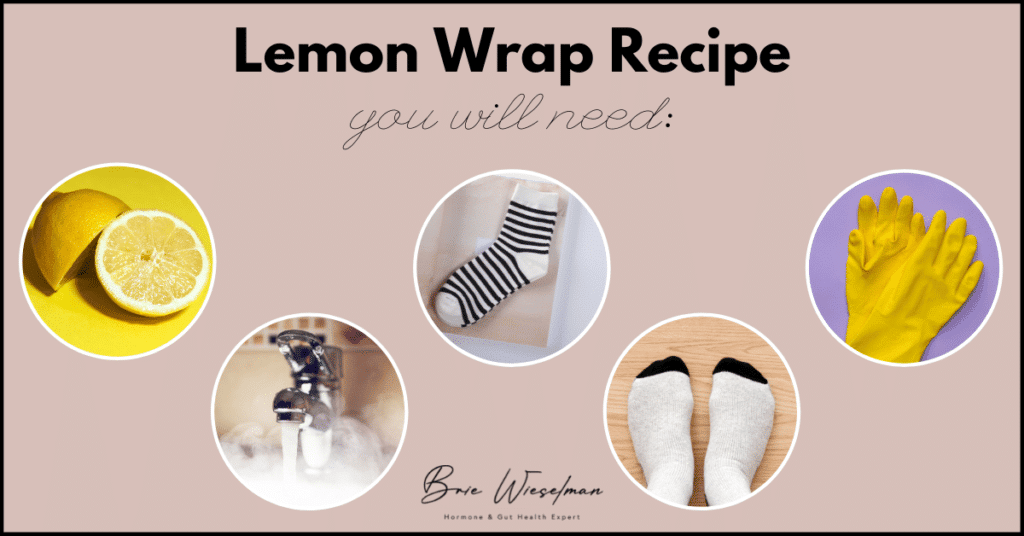
You will need:
- A lemon
- Hot water (2-3 cups) in a pan
- One pair of adult cotton socks
- One pair of adult wool socks
- Rubber dishwashing gloves
Directions
- Warm up your child’s feet with warm water or a warmed water bottle first.
- Squeeze the juice of a lemon in 2-3 cups of water.
- Heat in a pan until hot to the touch.
- Soak the cotton socks in the mix.
- Put on gloves and squeeze out the excess liquid from the socks. It may be hot on your hands. Let the sock cool until you can comfortably touch it, like to the safe but warm temperature of bathwater for your child.
- Pull on the cotton socks over your child's feet, all the way up the calves, or thighs if it reaches.
- Put the wool socks on over the cotton ones, and cover up your child with a blanket.
- Wait until the socks are completely cool to the touch, or dry. They will actually dry out pretty quickly,
- Then apply another round. Up to 3 times.
Your child will probably nap after this fever-lowering treatment. You should see the fever come down several degrees in a relatively short time, as few as 1-2 hours. If the fever persists, seek medical help.
How To Improve Children’s Immunity
Illnesses are part of daily life with children. But there are so many preventative, nutritional, and herbal tools at your disposal to ease their discomfort and get them well sooner. If you’d like to work with me to support your child’s immune health naturally, let’s meet for a free 15-minute troubleshooting call. During this chat, I’ll get to know more about your biggest concerns and where your child might be struggling. Then I’ll work with you to devise a customized plan to keep your little one healthy and strong and ready to face any immune challenges that come your way.
Effective Ways to Deal with Postpartum Depression and Anxiety
Feeling like a hot mess after having your baby?
Are you blitzed out in love but also feel like you want to crawl into a hole and disappear? Or are you awake at night worrying even though you need sleep more than anything? Are you having trouble wanting to hold your baby and then feeling guilty about it?
You’re not a bad mom. Your hormones are just scrambled.
While a few days of hormone crash or baby blues is common, anything beyond that is a sign of postpartum depression or anxiety. Having a baby should be one of the happiest times of your life, right?
Sadly, though, many of us feel unhappy after our baby is born and suffer from postpartum depression. The Centers for Disease Control (CDC) says one in eight new mothers have this condition.
In my experience, it’s more like one in three.
Motherhood turns our worlds upside down and there’s no getting around that. But postpartum depression or anxiety makes it so much harder. Keep reading to learn why you’re feeling blue and how to get back to normal as soon as possible after birth. It’s a wild ride and you deserve to feel good while you bond with your new baby and adjust to your new life.
What is Postpartum Depression?
Postpartum depression is a feeling of sadness that new mothers experience after giving birth. Symptoms of postpartum depression include:
- Feeling angry
- Crying more often
- Postpartum mood swings
- Not communicating, or withdrawing from others
- Feeling numb
- Worrying about harm coming to the baby
- Worrying you’ll harm the baby*
- Preoccupied with the sense that you’re not a good mom
- Feeling like you won’t do a good enough job caring for your baby
Sound familiar? Anyone? If so, raise your hand.
* If you feel concerned you might actually harm your baby, please speak with a professional. Generally, your OBGYN office is a really supportive place to start.
Is It Postpartum Depression or Baby Blues?
Postpartum depression isn’t the same as baby blues. Postpartum depression lasts longer than two weeks and can hang around for four years or longer.
Baby blues, on the other hand, usually appear soon after delivery and last only up to ten days after birth. Baby blues are related to the exhaustion from labor and giving birth, as well as the effects of the heroic hormonal shift that occurs during this time.
Baby blues are a normal part of giving birth. They happen in up to 85% of new mothers. Symptoms of this emotional condition may include crying for no reason, irritability, restlessness, and anxiety. These symptoms last a week or two and generally resolve on their own without treatment. Postpartum depression, on the other hand, can be a lot more severe.
Postpartum depression tends to show up within the first month after delivery—usually after the first ten days. Sometimes it can start as baby blues, which turns into a second wave of postpartum depression. You might even be able to tell when baby blues turns into something more.
When You Worry Too Much About Your Baby
Postpartum anxiety is also a real thing. In this condition, new mothers obsessively worry about the health and well-being about their child. Symptoms can include:
- Constant or near-constant worry
- Feelings of dread and fear about things that could happen
- Insomnia even when your baby is sleeping
- Thoughts that won’t calm down
You can also have physical symptoms of postpartum anxiety. These include fatigue, heart palpitations, sweating, nausea, shaking, and hyperventilating.
In modern times, we have so many apps and methods to track a baby’s health and progress. Postpartum anxiety might show up as excessively tracking baby’s metrics like feedings, liquid, wet or dirty diapers, etc. If it feels like you are over-focused on this and it is not medically necessary, or if it is adding to your anxiety, consider if tracking your baby’s metrics is best for you. If you are Googling about your baby’s well-being much more than what seems appropriate, it may be a sign of postpartum anxiety.
The Heroic Hormonal Shift
Can’t relate with those magazine-ad mommies who are wearing their new baby while going for hikes in the beautiful outdoors, gorgeous hair whipping in the wind? How about those well dressed and fully makeup’d Instagram influencers?
It’s easy to compare. We’re all guilty to some extent. And while I won’t tell you to stop (easier said than done), I do want to encourage you to try and stay true to yourself and the things you love about you.
This is NOT a moment of weakness. Hormonal changes, depression, and anxiety make this so much easier said than done. It’s cloudy. It’s dark. It’s confusing. It’s a roller coaster. Remember that every single journey is different. Everybody is different and every healing journey looks different, even from someone you may know really well.
When you’re giving birth, your progesterone levels take a nosedive. At the same time, estrogen levels increase. This hormonal shift is what causes the uterine contractions that lead to delivery of the baby.
That’s a good thing. The bad news, though, is that this puts you into a near-instant state of estrogen dominance.
This is a heroic amount of hormonal shift. And it happens in just this one moment of pregnancy.
This sudden dramatic drop off of both estrogen and progesterone essentially mimics menopause.
Interestingly, these changes depend as much on the hormones of the baby, as they do on the mother’s! This is why induced deliveries** are more likely to require hormonal interventions after to restore a mother’s good mood and well-being. When a birth is induced, the hormonal cascades that promote the stages of labor aren’t encouraged in the same way.
Induced labor triggers the release of higher levels of the stress hormone cortisol in the baby. This in turn leads to a drop in progesterone, just like you would experience before your period. Only it’s much more dramatic because progesterone levels are 20 times higher in pregnant women.
Whether labor is induced or occurs naturally, the resulting hormonal changes happen relatively quickly. But it can take a long time to restore them to a more balanced state.
The postpartum period is defined as six to twelve weeks after delivery. Yet, sometimes it takes up to four years for out-of-whack hormones to rebalance themselves. This usually depends upon the stage of your reproductive cycle when you give birth. By that I mean, are you 20-years-old when delivering your baby or 45-years-old and perimenopausal?
During and after birth, new mothers also produce high levels of a hormone known as oxytocin. This is sometimes called the bonding hormone or love molecule. This is because it leads to feelings of euphoria and connection. It makes you love and want to take care of this tiny, needy little animal you have created. Oxytocin is triggered at birth, by touch, and by breastfeeding. It helps take the sting out of the other hormones dropping so severely.
**Please note: Whether you chose or needed a certain intervention in your birth plan, there is no judgement or shaming intended here. We are just talking about the evidence related to these labor and delivery events. Many women dream of the “perfect birth,” and few of us get it.
Hormonal Causes of Postpartum Depression and Anxiety
One or more of four hormones tend to be out of whack in women who are depressed or anxious after giving birth.
Thyroid Hormones
The thyroid works extra hard in pregnancy. It generally returns to pre-pregnancy levels within six weeks after you’ve given birth. But if it’s not working properly this can create depression, anxiety, or fatigue. In this case, a women can have an overactive thyroid (hyperthyroid) or a sluggish thyroid (hypothyroid).
New mothers could also develop thyroid autoimmunity (Hashimoto’s or Graves’ disease). Or they can have a flare-up of a pre-existing thyroid autoimmune condition.
Women who have higher levels of antibodies known as thyroid peroxidase antibodies (TPO), which indicate Hashimoto’s disease, have higher risk for postpartum depression. The same is true for women with lower levels of the thyroid hormone known as free T4.
Cortisol
This is the stress response hormone. Your body produces it according to a circadian rhythm every day. During regular daily life, cortisol is high in the morning and lower at night before bed. That’s why you have energy in the morning and get tired at night. But throughout pregnancy it naturally increases in both mom and baby.
The placenta—an organ that grows in the uterus during pregnancy to provide oxygen and nutrients to your unborn child—is its own hormone manufacturing plant during pregnancy. It acts like this to ensure fetal development is happening like it’s supposed to do.
The placenta signals the baby and mom to make more cortisol. If cortisol levels don’t return to normal after delivery, there’s an increased risk of postpartum depression.
Ironically, though, the problem isn’t high cortisol after giving birth. It’s low cortisol.
Cortisol levels are high during pregnancy. After pregnancy, they drop. This can cause problems because for months the placenta has signaled the mother’s body to make cortisol. Sometimes, a new mom’s body has to relearn how to make cortisol. That’s why cortisol levels don’t always bounce back right away.
Serotonin
Serotonin is a hormone that makes you feel content, happy, calm, and ready for sleep. You need estrogen in order to convert amino acids into serotonin. When estrogen levels take a tumble after giving birth you may not have enough estrogen to encourage adequate serotonin production. This is especially true if you’re close to menopause.
Oxytocin
Trauma early in life is associated with low oxytocin later. High stress also is not a friend to your oxytocin levels.
What’s more, women who are given synthetic oxytocin (Pitocin) during labor might not make enough oxytocin on their own. Research shows these women have a higher risk of postpartum depression. Sadly, women aren’t often told this when deciding whether to use this drug during labor and delivery.
It Takes a Village but You Likely Don’t Have One
It’s not just hormonal issues that are causing your depression. To make matters worse, you’re also exhausted. Caring for a baby is 24-hours a day, non-stop.
You’re not getting together with your friends. You’re losing sleep. You’re often not eating balanced meals or at regular intervals and you’re not exercising like you used to do.
You might also be feeling a loss of sense of self.
We used to live in villages where aunts, uncles, grandparents, siblings, and cousins all helped with the care of a child. Today’s women are feeling the lack of overall support networks. This leads to feeling isolated. New mothers and fathers often have to do the work of a whole village. These feelings of isolation and overwhelm are even worse in women with postpartum depression and anxiety.
Sure, some couples have the support of grandparents that live nearby. But in many cases, grandparents live in distant cities or states and are only visiting for a short while after the birth.
Don’t hesitate to build your support network. Ask for help. Call on friends and family. Use Facebook mother/parent groups in your local area. Check out postpartum support groups through your OBGYN’s office or lactation support organizations. For those who have a religious or spiritual leaning, there are many community resources provided by synagogues, mosques, or churches. Gyms sometimes have childcare rooms to give you a break while you do self-care. Hire help for childcare or housework. Motherhood isn’t something we can do alone.
Other postpartum resources are:
Postpartum Progress is the world’s most widely-read blog dedicated to maternal mental illness. It gives a list of providers who specialize in PPD in your state.
Postpartum International is a nonprofit dedicated to raising awareness “among public and professional communities about the emotional changes that women experience during pregnancy and postpartum.”
La Leche League is a nonprofit that provides breastfeeding information and support to those who want to breastfeed their infants. In addition to groups that offer support to pregnant women and new moms, breastfeeding is thought to have a protective effect against postpartum depression.
Postpartum depression screening tool (or Edinburgh Postnatal Depression Scale) helps identify women who may have postpartum depression.
Birth trauma resources Stress caused by a traumatic pregnancy and delivery can often override the ability to emotionally cope, leading to psychiatric complications such as post-traumatic stress disorder (PTSD) and post-partum depression.
Risk Factors for Postpartum Depression and Anxiety
You’re more likely to suffer from postpartum depression if you:
- Had major depression prior to pregnancy
- Experienced high levels of stress before or during pregnancy
- Have a history of trauma
- Had a traumatic birth.***
- Struggled with anxiety disorder prior to pregnancy
- Have a history of insomnia or other disruption in your circadian rhythm
- Have high testosterone, which occurs more often in women with polycystic ovarian syndrome
- Are low in oxytocin
- Have low thyroid hormone levels
- Have a history of severe premenstrual syndrome (PMS)
- Your natural drop in estrogen and progesterone is particularly severe
- Fall into the category of low socioeconomic status
***Traumatic births are not often acknowledged by medical professionals and good options for healing and recovery aren’t well publicized. Many people don’t know where to start or that they could get help with this. There are therapists, counselors, and support programs available for women who experienced birth trauma.
Racial Differences in Postpartum Depression
There’s an important fact to bring to light. It’s that women of color who suffer from postpartum depression often don’t receive the right treatment. Postpartum depression care and awareness in all women is lacking. However, there are definite racial and ethnic differences in postpartum treatment.
For example, in one study, 9% of white women began postpartum mental health care, compared with only 4% of Black women and 5% of Latinas. Blacks and Latinas were significantly less likely to begin treatment for postpartum depression compared with whites. Among those who did begin treatment, Blacks and Latinas were less likely to receive follow-up treatment or continued care compared with white women.
Of the new mothers who started taking antidepressant medication, Black women and Latinas weren’t as likely as white women to refill a prescription.
Research shows that BIPOC women experience postpartum depression at a rate of nearly 38%. Meanwhile, the rate is much lower—only 13% to 19%—when statistics include all women with postpartum depression.
Promote Equal Postpartum Care for Mothers of Color
There are certain action steps we can take to make sure mothers receive healthy, safe, fair pregnancy and postpartum care. We recommend you read this Center for American Progress article, which offers a number of great suggestions on what policy-makers, health care providers, and you, can do to support mothers in underserved communities. Here are other steps you can take to bring about social change for this serious problem affecting mothers of color.
- Amplify and support women of color-led organizations.
- Support policies that improve work-family balance for women in the workplace.
- Support the Shades of Blue Project, an organization focusing on maternal mental health in underserved communities, before, during, and after childbirth.
- Donate to the National Birth Equality Collaborative (NBEC), an organization that provides training, research, and other assistance for the issue of black maternal mortality.
- Support the National Association to Advance Black Birth, an organization founded to help provide training and access to midwives and doulas of color and lower pregnancy-related deaths.
- Support the Black Mamas Matter Alliance, an organization that educates and advocates for better legislation to reduce black maternal mortality. They highlight needed research, and spread information about the social determinants of health that influence outcomes like traumatic birth or maternal and infant mortality.
How to Get Rid of Postpartum Depression and Anxiety
If you have postpartum depression and/or anxiety, please know that you don’t have to suffer alone. Here is what I do with my patients who are feeling emotionally and physically debilitated after giving birth. I’ve had a great deal of success with each of these strategies.
Test hormone levels.
I test women’s sex hormones, adrenal, and thyroid markers. I usually use the dried urine test for comprehensive hormones (DUTCH) to look at adrenal hormones (cortisol and DHEA) and sex hormones. This involves collecting a small amount of urine on filtered paper four times per day. I also order blood tests to look at thyroid function.
Various types of therapy.
Here are some I recommend:
- In women who have suffered a trauma in the past or who had a traumatic birth, I recommend a type of therapy known as eye movement desensitization and reprocessing (EMDR).
- Hypnosis therapy and cognitive behavioral therapy also work really well.
- Meditation programs like Ziva can be a powerful tool.
- Apollo neuro wearable touch therapy is another interesting solution. You wear it on your ankle or wrist and it emits silent, soothing vibrations that work on your central nervous system.
- Body therapies like acupuncture and craniosacral therapy can help.
Hormonal Support and Dietary Supplements
It’s critical you work with a trained functional medicine healthcare practitioner when taking hormones or dietary supplements. He or she can help you use them appropriately for your specific health concerns. They will order testing to find out the root cause of your postpartum depression or anxiety in the first place. Everyone is unique. The problem could be imbalances in hormones like thyroid, cortisol, progesterone, and estrogen. Or the culprit could be nutrient deficiencies, problems with brain chemical imbalances, anemia, etc.
These are the areas I work on with my postpartum patients to kick anxiety and depression:
- Oral natural progesterone in appropriate cases
- Estrogen (estradiol) support in appropriate cases
- Serotonin support, when testing indicates it, and under supervision of a clinician. This involves supplementing with tryptophan or 5-HTP. If your serotonin levels are high, it can be a marker of inflammation and supplementing with tryptophan or 5-HTP can only make things worse.
- A prenatal supplement. The same one you used during pregnancy can work wonders on your mood and mental health outlook.
- Lactation-safe herbal formulas and nutraceuticals.
At the risk of repeating myself, it is best for you to work with a skilled practitioner on this journey. With that in mind, these products are safe across the board if you’re breastfeeding your baby:
- Herb Lore Anxiety Blend tincture. Reduces stress, calms anxiety, fear, and agitation.
- Herb Lore Happy Day tincture. For women feeling sorrow, sadness, or depression.
- Lavella. An oral lavender essential oil that reduces anxiety and helps with sleep.
- Rescue Remedy. For trauma, stress, anxiety, depression, panic attacks, accidents, or injuries. Safe for newborns, pets, siblings, spouses/partners, too!
We Can Help You Feel Happy Again
If you have postpartum depression or anxiety, you’re not alone. We can order the right testing to help you balance your hormones and other factors that can cause your sad mood. We’ll pinpoint the root causes, and design a customized protocol just for you.
Babe, you can get through this rough time. We’ll hold your hand every step of the way to show you exactly what you need to do to feel happiness and joy again.
Your path to a happier life begins with a free 15-minute troubleshooting call. During this chat, I’ll get to know more about what troubles you. If after the call you come on board as a patient, I’ll work with you to get rid of your postpartum depression and anxiety. Book your call today so you can start enjoying the precious moments of a new beginning- for you and your little one.
I Have PCOS – Should I Try The Keto Diet?
Is the Keto diet right for PCOS?
This is one of the most common questions I get as a Functional Medicine practitioner and person with PCOS myself…
And with good reason! The Keto Diet is often touted as a solution for two of the biggest issues people with PCOS face: blood sugar issues and weight gain.
But as with most things related to PCOS, using the Keto diet for PCOS is not a one-size-fits-all solution.
Today, let’s take a deeper look at this question - and hopefully, provide you with a customized answer.
What Is PCOS?
If you’re reading this, you probably either have been diagnosed with or suspect PCOS: polycystic ovarian syndrome.
But even though it's very common (affecting 1 out of very 10 women), this condition is hugely misunderstood, so I think it’s always good to start with a quick refresher on what exactly it is.
First of all, despite what the name implies, people with PCOS don’t necessarily have cysts on their ovaries. (And equally important - just having cysts on the ovaries doesn’t mean you have PCOS!) Instead, PCOS is about hormone imbalance - specifically, an excess level of androgens.
Androgens are hormones typically thought of as “male”: primarily testosterone and androstenedione, but also DHT, DHEA and DHEA-S. (But just to confuse things even further, some people with PCOS will never show high testosterone or DHEA levels.)
Along with androgen excess, people with PCOS generally have “ovulatory dysfunction” - meaning they don’t ovulate monthly. They may have irregular periods (long, short, heavy, or absent) - but they can also have normal-appearing periods (they might not even know they aren’t ovulating, or they may ovulate sometimes, and not others).
Lots of other symptoms go along with androgen excess and ovulatory dysfunction - but none of these HAVE to be present. Some people with PCOS have them all, and some have none:
- Insulin resistance (even if the person is not overweight)
- Cysts on the ovaries
- Excess hair growth on the body
- Weight gain and weight loss resistance
- Acne
- Thinning hair on the head
- Oily skin or hair
- Infertility
What Is The Keto Diet?
Now that we’ve brushed up on PCOS, let’s do the same for Keto.
Keto is shorthand for the ketogenic diet - this is a pattern of eating where carbs are kept low enough, and fat intake is increased, so that the body shifts from burning glucose (sugar, carbs) for fuel to manufacturing ketones, an alternative source of fuel for your body. The state in which you are using ketones for fuel is called “ketosis.”
It takes a few days of very low carb eating to switch into ketosis - and once you’re there, eating carbs again will bump you back out. That means keto is not a diet you can do halfway or dabble in easily - it's all or nothing.
It varies person to person, but usually carbs need to be kept below 20-50 grams per day to achieve ketosis. That is very low: one banana alone has 27 grams of carbs. This means all starchy foods are out: potatoes, most fruit, oatmeal, rice, bread, etc. Non-starchy foods that are high in sugar - like ice cream - are also out.
But it's not just about cutting carbs - you also have to significantly increase fat intake, with 70% or more of total calories coming from fat - and that’s where this can get a little tricky for some people (more on that to come).
But one REALLY important thing to note before we go any further: keto is not the same as just cutting carbs, and for people with PCOS, it should not involve under-eating. Under-eating calorically can further suppress ovulation, making PCOS symptoms worse.
How Does Keto Help PCOS?
Keto may help PCOS by addressing one of the biggest symptoms: insulin resistance. And for people with PCOS who have weight loss as a concern, the keto diet may help them shed unwanted weight.
Research has shown that in small groups of people with PCOS, a keto diet can:
- Lead to weight loss
- Normalize insulin levels and reverse insulin resistance
- And, most importantly: The LH/FSH ratio, LH total and free testosterone, and DHEAS blood levels were also significantly reduced
That suggests that the Keto diet isn’t just treating the symptoms - it may actually help to balance hormone levels.
It’s not completely understood yet how this happens, but the endocrine system is very complex, and interactions between hormones matter - and don’t forget that insulin is a hormone, too!
I know it sounds great, but before you dive into keto there is a big catch that we need to talk about.
The Keto Diet for PCOS is NOT One-Size-Fits-All
If you are considering trying a keto diet for PCOS - great! I support you 100%. For my own PCOS, reducing carbohydrate intake was one of the best things I did.
But before you go any further…. I want to give you a quick warning:
Depending on your genetics, you might need to do keto a specific way.
Most people with PCOS need to follow a “Mediterranean keto” diet - in fact, it was this specific diet that led to the amazing results in that 2020 research article I mentioned above.
Mediterranean keto focuses on poly and monounsaturated fats from foods like olive oil, avocados, fatty fish, and nuts and seeds.
Traditional keto focuses more on quantity than quality - it's all about lowering carbs and increasing fat in any way possible.
That often means LOTS of cheese and red meat - both of which are very high in saturated fat.
For some people, there is nothing wrong with saturated fat - they are genetically programmed to tolerate high levels of saturated fat well. But for many people - especially those with PCOS - saturated fat is problematic.
3 Things People with PCOS Need to Know Before Starting Keto
There are two gene variants to look for and one general rule to know about before starting keto.
First, for people with either the FTO or APOA2 SNP variant, saturated fat can be problematic. People with the FTO variant usually don’t tolerate simple sugars or saturated fats well. This variant also makes you more likely to burn fat slowly and struggle with feeling full.
The APOA2 gene variant also affects metabolic hormones. Research suggests that people with this variant do best if they eat under 22 grams of saturated fat a day. That’s very hard to do if you’re eating red meat, dairy, and bacon!
Finally, dairy in particular can be a problem for people with PCOS - whether or not they have the FTO or APOA2 variants. Milk (from cows, goats, sheep, and camels) contains the hormone insulin-like growth factor-1 (IGF-1), which mimics insulin in our body. IGF-1 is a growth hormone (which makes sense, as milk is for baby animals!). In most people, a little dairy here and there can be well-tolerated because humans have a binding protein for IGF-1 that inactivates it.
But for people with PCOS or hormonal imbalance, who already are likely to be insulin-resistant or have high insulin, the added burden of IGF-1 can be a problem. This is amplified because women with PCOS have LESS of the binding protein for IGF-1 and higher IGF-a levels than other people do, too. And the ovaries of women with PCOS are more sensitive to IGF-1 (and other growth hormones), too.
IGF-1 can also cause your ovaries to overproduce testosterone (an androgen) - which is something we’re trying to minimize.
That’s why I recommend most people with PCOS try cutting dairy - and if you’re considering Keto, get some basic genetic testing done to reveal how you tolerate saturated fat (I can help with that).
Your Genes Can Reveal So Much
Whatever your health struggles are - I think investing in genetic testing is one of the smartest choices you can make.
Your genes are like your body’s instruction manual. Your genetic variants can give you information about your diet, lifestyle, exercise needs - and even what nutrients you’re likely to struggle getting enough of.
That’s why I’m making genetic counseling a bigger part of my practice: it helps patients create a truly customized health plan, without wasting time on plans that would never work for you genetically.
Want to learn more? Book a free consult with my team today and we can talk through what we offer. We’d love to support you on the journey to better health.
Meet Your Gallbladder: The Essential Detox, Hormone, and Digestive Organ Most People Know Nothing About
More than 600,000 people have their gallbladder removed each year in the U.S.
That’s like if every single person in Las Vegas had their gallbladder removed!
Usually, the gallbladder is removed because of painful gallstones. It’s treated as a totally normal, safe procedure with no side effects.
But that’s just not true...
Your gallbladder is actually a crucial part of your digestive, detox, and hormonal systems.
And even if you haven’t had your gallbladder removed, gallbladder dysfunction is becoming more and more common, and can cause symptoms like:
- Digestive issues (pain, bloating, diarrhea)
- Fatigue
- Skin congestion (acne, rashes, eczema, etc.)
- Weight loss resistance
- Hormone imbalance (PCOS, estrogen dominance, etc)
- Fatty liver disease
- And more
Today, I want to explore the role of the gallbladder, common signs and symptoms of gallbladder dysfunction, and steps you can take to heal and optimize your gallbladder function. Learn about hormone imbalance after gallbladder removal.
What and Where Is The Gallbladder?
Your gallbladder is a small organ that sits underneath your liver. Your liver makes bile (the digestive liquid needed to break down and absorb fat) and the gallbladder stores it, concentrates it, and then releases it to the stomach on demand.
The gallbladder plays key roles not just in digestion, but also in detox and hormone balance, as bile is needed both for clearing toxins from the body and for the healthy production of hormones, as well as hormone removal and balance. For that reason, the gallbladder isn’t just a digestive organ - it’s also a hormone and detox organ.
In Chinese medicine, the gallbladder is also attributed with governing decision making and qualities like inspiration, action, and assertiveness (think of the saying “they have gall!”). A strong gallbladder is associated with a quick return to normal after a physical or emotional shock. On the other hand, a weak gallbladder is associated with timidity or hesitation, and problems making decisions or following through. Finally, the gallbladder is also seen as a pivot, a turning point for new decisions and stages of life.
What Bile Does
Although it’s not sexy, the bile created by the liver and then stored, concentrated, and secreted by the gallbladder is one of the most important secretions in your body. Bile consists of ~95% water, in which are dissolved bile salts, bilirubin phospholipid, and cholesterol, primarily.
Here are just some of the many roles of bile:
- Bile emulsifies fat, increasing fat absorption. Bile is an essential “degreaser” and “emulsifier” of dietary fats. Bile is also essential for the utilization of the fat-soluble vitamins A, D, E and K. Bile deficiency leads to vitamin deficiencies.
- Bile prepares nutrients for assimilation in the small intestine. Bile takes food that has been acidified in the stomach and alkalizes it, allowing it to be broken down and absorbed.
- Bile assists in detoxification. Bile contains the conjugated toxins - carcinogens, xenobiotic chemicals, pharmaceuticals, heavy metals like mercury, aluminium and lead, and deconjugated hormones - from the 2 phases of liver detoxification.
- Bile helps modulate the microbiome. It acts as an antimicrobial, keeping the balance of bacteria in check.
- Bile transports excess cholesterol out. In doing so, it prevents cholesterol levels from rising too high.
- Bile lubricates the intestines and plays a regulatory role in motility, allowing food to go through the digestive tract a lot easier and preventing constipation.
- Bile prevents the formation of gallstones by breaking down fats before crystallization, and also digests and dissolves gallstones, which are composed mostly of cholesterol and particles.
- Bile triggers the release of glutathione, which is considered the “master” antioxidant, and helps eliminate bilirubin.
- Bile breaks down fats, and as such, is essential for weight loss!
- Bile controls the rhythm of the gut - the circadian timing of your gut motility is controlled by the gallbladder. Changes in motility (the time it takes for food to move through the digestive system) can lead to issues like Small Intestine Bacterial Overgrowth (SIBO).
The Gallbladder, Bile, and PCOS
The gallbladder’s role in hormone balance deserves special attention, especially in relation to PCOS (Polycystic Ovarian Syndrome).
Dietary fat and bile (to absorb it) are both necessary for the production of hormones. Even more importantly - bile helps your body excrete excess and used hormones, like estrogen. In addition, estrogen dominance (either as a result of hormone imbalance or due to supplemental estrogen, like birth control pills) are known risk factors for sluggish bile (the precursor to gallstones) and gallstones themselves. This is believed to be because estrogen causes an increase in cholesterol levels in the bile, which can then thicken and form stones.
Interestingly, research has shown that in PCOS, bile acid levels are actually significantly elevated, and that high levels of bile acids correlated with higher levels of testosterone levels, meaning worse PCOS.
The exact mechanism is not yet known, but it is thought to be related to sluggish bile, which is more commonly seen in those with hormone imbalance and PCOS. The sluggish bile raises levels of bile acids in the blood. There, the bile acids act on the Farnesoid X receptor, which has hormonal actions throughout the body, and can lead to elevated testosterone.
In addition to increasing testosterone, high levels of bile acids can also contribute to insulin resistance, another major issue in PCOS.
Bile and Leaky Gut
Bile flow issues or lack of bile can also cause or worsen leaky gut (increased intestinal permeability).
While leaky gut is often attributed to toxins produced in the gut or pathogenic bacteria living there, insufficient bile is another major cause.
One role of bile is to bind with toxins and help them be safely excreted from the body. But if there is inadequate bile to bind with the toxins, they can damage the intestinal barrier, allowing toxins and undigested food into the bloodstream… creating “leaky gut.”
Leaky gut causes widespread, multi-system issues and may even be a major part of triggering autoimmune disease. It is common in IBS (Irritable Bowel Syndrome), ulcerative colitis, Crohn’s disease, Celiac disease, and more.
Signs of Gallbladder Dysfunction
The most common type of gallbladder dysfunction is the result of slow or sluggish bile. This can be a result of not enough water (remember, bile is 95% water!), but can also occur when bile is oversaturated with toxins. The sluggish bile is more like peanut butter than water, and is too thick to flow freely.
In addition, the removal of the gallbladder, as well as other conditions, can lead to reduced levels of bile salts in the bile and weakened bile.
Symptoms of sluggish or weak bile include:
- Abdominal tightness
- Bloating
- Difficulty digesting fats
- Diarrhea
- Constipation (fat can build up in the intestinal wall and cause slow movement in the digestive tract)
- Trapped gas
- Bad-smelling gas
- Stomach cramps
- Gallstones
- Fatigue and malaise
- Fatty stool that floats or is light in color or grayish white
- Increase in allergies, chemical sensitivities, or food intolerances
- worsening PMS/Estrogen dominance…
- Hormone imbalances like PCOS
- Heartburn
- Erratic bowel movements
- Weight loss
- Signs of Vitamin A deficiency: Dry eyes, night blindness, red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks), and dry skin
Why Are So Many Gallbladders Removed?
Typically, the gallbladder is removed due to gallstones. Gallstones are crystallized masses of bile and cholesterol. Around 20% of females over the age of 40 have gallstones.
When gallstones become stuck in the duct of the gallbladder, they can cause pain and inflammation called cholecystitis. The most common treatment for gallstones is simply having the gallbladder removed. The surgeon then ‘“reroutes” the bile to go straight from the liver to the stomach.
Risk factors for gallstones include:
- Alcohol
- Excess reproductive hormones from supplementation or steroids (most commonly estrogen dominance)
- Oral contraceptive pills (birth control pills)
- High Endotoxin load causing sludgy bile
- Hereditary disorders like Gilbert's syndrome
- Thyroid issues or thyroid supplementation with T4
- Hepatitis
- Pregnancy
However, without the gallbladder, bile isn’t concentrated and lacks adequate bile salts - leading to the problems discussed above. That’s why gallbladder removal isn’t something you should just jump into.
Testing For Gallbladder Issues
If you suspect gallbladder issues, various tests can help pinpoint the problem:
- Blood test for cholesterol levels - if a person’s cholesterol production is low, bile production is also likely to be low. I look for cholesterol levels lower than 170.
- Digestive stool analysis - can help identify undigested fat in stool, which is caused by low bile availability.
- Bloodwork - to look for changes in serum bilirubin, alkaline phosphatase, serum glutamic oxaloacetic transaminase (SGOT), lactate dehydrogenase (LDH), aspartate aminotransferase (AST) and alanine transaminase (ALT). In early stages of gallbladder dysfunction, these levels might not change. However, functional medicine practitioners like me also use a more narrow interpretation of what normal is.
- A HIDA scan - this imaging test uses a radioactive material to measure the emptying function of the gallbladder, and can help diagnose:
- Gallbladder inflammation (cholecystitis)
- Gallstones, which can’t be seen, but can contribute to reduced flow or blockage to less bile flow if blocking
- Bile duct obstruction
- Congenital abnormalities in the bile ducts, such as biliary atresia
With my own patients, I use the ION panel by Genova (Organic Acids section) to evaluate the various pathways of liver detox and glutathione/antioxidant capacity. These results often illuminate when the liver or gallbladder are overburdened long before we see markers of pathology like elevated liver enzymes in labs. They also give more detail about exactly how the liver or gallbladder are compromised and can best be supported, in each individual.
Support for a Healthy Gallbladder
If you’re having signs of any gallbladder issues, step one is to get tested and find out exactly what’s going on.
In addition, here are some of the steps I turn to again and again with my patients:
- Switching out hormonal birth control (pill, patch, ring, etc.) for non-hormonal to reduce estrogen levels
- Supplements that support healthy gallbladder function
- Digestive enzymes and bitters
- Dietary changes: avoid excessive fried, fatty and greasy food and increase leafy greens
- Cut out alcohol
- Exercise regularly
In addition, addressing the emotional side of gallbladder health can be important. Try to express your emotion freely (journaling is an easy way to get started), address your past traumas (get help from a professional), and forgive.
And if you’ve already had your gallbladder removed? I can help you with strategies to support your digestion and hormones, even without your GB!
Want to learn more? Book a free 15 minute consult with my team now. It’s a zero-obligation opportunity to get a functional medicine opinion on your gallbladder health (and even if removal is something you should consider!).
P.S. Gallbladder issues are more common in women and those on hormones (like HRT or birth control). But if you catch gallbladder issues early on, you can avoid ever developing painful stones. Book a free 15 minute consult now.
The Surprising Truth About Low Stomach Acid (And How To Solve It Naturally)
Do you burp after meals? How about get so bloated, you want to unbutton your pants? Does food feel like it just sits in your stomach?
These are all tell-tale signs you might be suffering from a really common but not-well-known condition: low stomach acid, also called hypochlorhydria.
Stomach acid has a bad rap - most people are familiar with antacid medication for heartburn or indigestion, and (understandably) assume that stomach acid is bad for you and must be decreased.
But surprise - the complete opposite is actually true. In fact, adequate stomach acid is a crucial part of the healthy digestive process. And, in my clinical experience, far more people have low stomach acid than high!
Today, let’s talk about why stomach acid is so key, what it feels like when yours is low, and how we can treat this common issue easily and naturally.
The Truth About Stomach Acid
Stomach acid - scientific name hydrochloric acid (HCL) - is one of the key steps in the digestive process.
During the gastric phase of digestion, food you chew and swallow travels down the esophagus and into the stomach. There, distention (literally the stretching of the stomach by the addition of food), triggers the production of acetylcholine (ACh), which then triggers parietal cells in the stomach to release stomach acid.
But even before you start eating, just the sight, smell, and thought of food can also jumpstart the secretion of stomach acid via activation of the vagus nerve. This is called the cephalic phase of digestion.
The stomach is specially designed to handle the incoming acid - the stomach is lined with lipoprotein rich membranes that protect it from being burned by the acid. (Other parts of your body don’t have this same protection - which is why when stomach acid gets into the esophagus, it causes a burning sensation.)
Once secreted by the parietal cells, stomach acid performs several key functions:
- It kills any pathogens that may have come in with food (i.e. the kind of bacteria that cause food poisoning) or hitched a ride on the saliva from the mouth, where tons of bacteria live.
- It activates pepsin to start protein digestion
- It stimulates bile production and release by the liver and gallbladder, so fats can be emulsified and digested
- And finally, it triggers the release of pancreatic enzymes in the small intestine, where the partially digested food from the stomach (called chyme), is broken down and absorbed into the bloodstream
What Happens When Stomach Acid Is Low
When stomach acid is low for any reason, it can impact all aspects of digestion.
Low stomach acid can slow and stall out the digestive process - leading to discomforts like burping, bloating, stomach pain, and even (surprisingly) cause heartburn and acid reflux symptoms.
And while these are the symptoms most people notice (and complain about) first, they are actually just the tip of the iceberg.
More troublingly, low stomach acid can have a huge impact on your body’s ability to absorb nutrients from the food you eat. Stomach acid is essential for breaking down protein into digestible amino acids, and for the absorption of certain key nutrients like iron and vitamin B12. Without these key nutrients, the body is unable to repair tissues, produce hormones, and create neurotransmitters - all things necessary to feeling happy and vital!
Finally, low stomach acid also is a common factor in the development of food sensitivities, because it is stomach acid that triggers the release of digestive enzymes in the small intestine. Lack of enzymes is often to blame for food reactions - the one most people are familiar with is lactose intolerance, where a lack of lactase enzymes cause digestive issues like gas, diarrhea, and pain.
If you’re eating a high-quality, nutrient-dense diet but still struggling with symptoms of nutrient deficiency like brittle hair and nails, poor skin quality, cravings, and fatigue - or you have ever-increasing food sensitivity - low stomach acid could be the reason why.
What Causes Low Stomach Acid?
Stomach acid gradually decreases with age, and levels can start to drop as soon as age 40.
In most people, environmental factors are the main cause of low stomach acid. These include:
- Stress - the big one that no one likes to talk about! Stress impacts all phases of digestion, and especially the production of stomach acid and other digestive fluids
- Low protein diet - this is often a “chicken and the egg” situation, since eating less protein is often a result of those with low stomach recognizing protein-rich foods don’t make them feel well, and consciously or subconsciously cutting back. On the other hand, eating low protein can cause the body to naturally downregulate acid production (since less is needed to digest protein).
- Low zinc status - zinc is an essential cofactor for stomach acid production, and the modern diet is fairly low in zinc-rich foods like oysters.
- Eating on the go - like stress, eating in a hurry or while distracted can prevent the body from shifting into the “rest and digest” parasympathetic state needed to complete all the phases of digestion adequately.
- And finally - using over-the-counter or prescription acid-reducing medications.
Are You Using Antacids?
Antacids include over-the-counter and prescription PPIs (proton-pump inhibitors) like Prilosec or Nexium, H2 blockers like Pepcid or Zantac, and antacids like Rolaids or Tums. They work by either blocking the production of stomach acid, or neutralizing acid in the stomach.
These are some of the most commonly used drugs in the world. And, when used the right way, they can be extremely beneficial. But, many people take these drugs daily for years without any idea of the potential side effects.
Research has shown that PPI use can lead to the development of Small Intestine Bacterial Overgrowth (SIBO), which causes bloating, diarrhea, constipation, food intolerances, and stomach pain. In one study, more than half of people on a PPI for 12 weeks developed SIBO. In addition, research has shown PPI use is a risk factor for candida overgrowth, as well. The connection between PPIs and both candida and SIBO is likely due to the reduced ability of the body to kill pathogens that come in on the food you eat or with your saliva.
The irony with antacids is that most people take them to address the symptoms of low stomach acid - bloating, gas, indigestion - without realizing that they are actually just compounding the problem by further reducing acid levels.
How Do I Know If I Have Low Stomach Acid?
Testing for stomach acid levels is possible with a test called the Heidelberg acid test. However, this test is extremely difficult to come by, and most doctors and practitioners don’t have access to it.
Instead, I use an advanced stool panel to look for several key specific bacterial indicators of low stomach acid. Specifically, I look for these bacteria:
- Pseudomonas - this bacteria grows on poorly digested proteins that may be present due to low stomach acid. It also commonly occurs with food sensitivities, as undigested proteins are a main driver for triggering an immune response to foods. If you have high pseudomonas, and especially with food sensitivities, think about raising your stomach acid levels!
- Streptococcus and enterococcus - these gram-positive, aerobic species naturally occur in the oral microbiome, gut microbiome (found in the large intestine), and upper respiratory tract. However, they can overgrow or become infectious. Streptococcus commonly causes strep throat and upper respiratory infection, and if stomach acid is low, can infect the stomach. Enterococcus strains are common in dental infections (and found in up to 90% of infected root canals), and if stomach acid is low, can also infect the stomach.
- C. difficile - I always work on raising stomach acid levels in those with chronic or recurrent infection with this organism. C. difficile infection can be life-threatening in some cases, causing bloody or profuse diarrhea requiring hospitalization, and is commonly seen in medical settings after the use of broad-spectrum antibiotics. But it also often shows up on stool panels with minor or moderate symptoms, not requiring hospitalization. In addition to raising stomach acid levels I use herbs and probiotics to treat this.
- H. Pylori - this common infection thrives in a low-acid environment and even deconjugates stomach acid in order to make its host more hospitable. Ironically, PPIs are often used as part of the treatment for the ulcers and gastritis H. pylori can cause, continuing the cycle. Importantly, however, H. pylori is not always a problem. If levels are high or symptoms like ulcers, gastritis, rosacea, upper GI gas and bloating are also present, it may need treatment. For low or normal amounts of H. pylori, raising stomach acid levels is often all that is needed!
- Klebsiella- this bacteria is common in the oral microbiome, but high levels are associated with inflammatory bowel disease like ulcerative colitis and Crohn's disease. Because klebsiella is common in the mouth, elevated levels are often a sign stomach acid isn’t doing it’s job of killing bacteria in the stomach.
(Interested in a stool test like this? Book a free 15-minute consult here to learn more about stool testing and get started!)
How to Support Healthy Stomach Acid Levels Naturally
Creating a customized plan to support your digestion is what I do best. Every person is unique, and needs a unique protocol for best results. But, in general, these are some of the strategies I turn to again and again:
- Supplemental HCL - supplemental betaine HCL paired with pepsin (a digestive enzyme that specifically helps with protein digestion into amino acids) can be extremely helpful. One 6-week study in 97 people with indigestion found that taking betaine HCL and pepsin significantly reduced symptoms like stomach pain and burning.
One word of caution: supplemental betaine HCL may not be right for those with ulcers or gastritis. If you have these conditions, try one of the other suggestions or book a free consult for one-on-one support.
- Adequate B vitamins - B vitamins have thousands of benefits, one of which may be better stomach acid levels. One study found that increased B vitamin intake lowered risk of acid esophagitis. In addition, low stomach acid levels can hinder B vitamin absorption, increasing your need.
- Apple Cider Vinegar - this is a long-time fix for low stomach acid. Try taking a shot of ACV or dilute it with water to drink with meals. Be sure to rinse your mouth with plain water after drinking ACV.
- Ginger - helps to stimulate the digestive system. Try ginger tea or ginger chews.
- Bitters - bitter flavors stimulate the vagus nerve and tell the body food is coming, promoting the release of HCL and other digestive secretions like enzymes and bile. Try taking a bitter tincture directly on the tongue before eating.
Put Low Stomach Acid in Perspective
If you suspect low stomach acid, taking these simple steps to raise it can help you feel a lot better.
But in my clinical experience, low stomach acid is very rarely the only problem!
It either comes on as a result of other issues - like poor nutrient status and stress - that need to be dealt with, or causes other issues, like SIBO or candida overgrowth that require separate treatment.
If you’re dealing with digestive issues of any sort, I would be honored to support you in healing. Having struggled with health issues myself, I know exactly how debilitating they can be, and what vibrant health feels like (it’s AMAZING!) - and I want that for you, too.
We have a variety of plans and approaches to fit your health needs, schedule, and budget - but Step 1 is always a free, no-obligation chat with my team to learn about you and your concerns.
When H. pylori Met Candida: How They Team Up To Weaken Your Gut
If you have any sort of digestive problem—for example gas, bloating, inflammatory bowel disease (IBD), acid reflux, ulcers etc.—you’re probably wondering, why me? What’s causing me to suffer with bad indigestion or abdominal pain?
Some healthcare providers oversimplify the answer to that question. They try to blame all your digestive problems on one organism. For example, if you have acid reflux or ulcers, then Helicobacter pylori (H. pylori) must be the only organism to blame, right?
Wrong.
First of all, organisms like H. pylori, despite what you may have heard, aren’t always bad. Sometimes, they can actually benefit your health.
It’s actually when H. pylori gets together with its friend Candida albicans that it causes the most trouble.
Organisms that team up like this with other organisms may be called synergists or co-infections.
What does that mean for your digestive health? It means that if you’ve got two different potential troublemakers (certain bacteria or fungi) living in your GI tract, it might spell more trouble than if you only had one.
But it’s more complicated than that. Remember, most of the organisms or “good bugs” living in your gut are helpful or harmless. Scientists call them commensal bacteria. On the other hand, there is a small percentage that can be harmful, or pathogens. We will call those “bad bugs.”
The kicker is that your gut health determines whether a bad bug can cause trouble or not. For example, if you have good gut health with plenty of healthy bacteria and their beneficial byproducts, even a few different bad bugs won’t cause trouble. An unhealthy gut, on the other hand, can make your GI tract more vulnerable to even one type of bad bacteria or fungi that makes its home there.
In this blog post, I’ll use H. pylori and Candida to paint a picture of an example of commensal organisms that can turn bad. I’ll also show you how the presence of these two organisms can make or break your digestive and overall health.
What Is H. Pylori Anyway?
H. pylori is a bacterium that colonizes the lining of the stomach. Its presence is linked to duodenal and peptic ulcers, gastritis (inflammation of the stomach lining), and gastric cancer. Stool tests have also detected it in people with ongoing indigestion and abdominal pain. That’s why a lot of doctors go after H. pylori as a standard peptic ulcer or stomach ulcer treatment.
H. pylori really gets around. In fact, as many as 50% of adults carry this bacterium at some point in their lives but most have no symptoms.
H. pylori isn’t always a nasty bug as I will explain why later. But it can be nasty sometimes. With my clients, I will use agents that fight back an H. pylori overgrowth when any of these conditions are present:
- H. pylori overgrowth on testing.
- The presence of virulence factors. These are harmful substances that H. pylori makes to set up a home in the gut, avoid the immune system, and cause disease. Virulence factors increase the risk that H. pylori will cause digestive upset, ulcers, or cancers.
- Classic H. pylori symptoms such as ulcers, gastritis, upper GI bloating, acid reflux, acne, and more. When H. pylori overgrows in the gut, it tells me there is an underlying weakness. And while I do treat certain patients for it, at the same time I am asking the question: “Why?” Why did H. pylori take root and grow out of control?
What Causes H. Pylori?
H. pylori gains a foothold in your GI tract when levels of stomach acid take a nosedive. This can be a problem because when H. pylori turns bad, it can harm cells, cause inflammation, and damage the stomach lining. Here are some of the things that can cause low stomach acid:
- Drinking alcohol
- Drugs used to treat acid reflux (proton pump inhibitors)
- H. pylori itself
- Smoking
- Stress
H. Pylori: Not Always The Bad Guy
But here’s the thing about H. pylori: sometimes it’s actually your friend rather than your enemy. It has been co-evolving with us for millennia. At normal levels, H. pylori can be a commensal or friendly bacteria. While it has the potential to be a pathogen, it doesn’t cause disease in many people. In fact, it can:
- Reduce allergies, asthma, and skin diseases like eczema, especially in children.
- Lead to a lower risk of developing IBD. It does this by making some beneficial changes to the gut microbiome, the collection of bacteria, both good and bad, that live in the intestinal tract. This is why I often don’t want to get rid of H. pylori when I’m treating patients with inflammatory bowel disease.
Really, with H. pylori, what it comes down to is how many of these little guys do you have in your GI tract? And how virulent are they (meaning how likely are they to do damage)?
It’s also important to treat any underlying causes that made it too easy for H. pylori to set up shop.
And then there’s the question of: are you also infected with Candida?
What Is Candida?
Candida is a fungus that hangs out in nearly everyone’s intestinal tract. It’s part of the microbiome and thus a commensal fungus. In fact, Candida species appear in 40% to 80% of normal stool specimens.
However, when Candida goes from Jekyll to Hyde it can cause vaginal yeast infections and oral thrush. What is oral thrush? That’s when Candida builds up in the mouth and causes white sores on your tongue, lining of your mouth, gums, and throat. And that’s just the beginning. In functional medicine practice, I have seen Candida cause brain fog, fatigue, skin rashes, diarrhea, constipation, gas, anal itching, and joint pain.
Just like H. pylori, Candida can be a harmless wallflower in the gut or it can be a deadly pathogen.
What causes Candida to turn from harmless to health-harming? Here are some common reasons for Candida gone bad:
- Eating lots of sugary and processed foods
- Hormonal imbalances and birth control
- Stress
- Taking antibiotics, which kill off the good bacteria in your intestines
- Untreated diabetes
- Weak immune system
When Candida Meets H. Pylori
Candida and H. pylori are good friends. In fact, H. pylori can make itself comfy and at home inside Candida. And once Candida teams up with H. pylori, things go south quickly. Research found that if you’re infected with both these organisms you’re more likely to develop gastric ulcers or have more severe gastric damage than if you had H. pylori alone. Pairing up Candida with H. pylori also leads to a higher risk of peptic ulcer disease, hence the name “synergists.”
A lot of people have both of these infections at the same time. For example, in one study, out of 27 people positive for Candida, 18 were also positive for H. pylori. This is why I test for the presence of both of these organisms in my patients with GI problems.
The partnership between Candida and H. pylori is just one example of how synergistic organisms can impact your health. Candida is a real social butterfly. It has a lot of friends besides H. Pylori. These include the bacterium Clostridioides difficile (aka Clostridium difficile, the microbe responsible for bloody diarrhea). I used the friendship between Candida and H. pylori because it’s one of the best ways to show you how organisms can pair up to make your health worse.
Is Your Gut Ready To Face the Bad Guys?
In regards to GI issues, it’s really not about the “bad guy.” It’s all about whether you can tolerate the organisms that live in your gut. Some people with H. pylori and Candida have no symptoms at all.
The most important factor in this equation is your gut health. If H. pylori and Candida are present in excess it means you’ve got an underlying weakness in your GI tract. And we have to get at the bottom of why the weakness is there.
The answers to four questions will let you know how well your body will deal with invasions by these organisms:
- Are the good bacteria in your gut balancing out the bad bacteria?
- How effective is your stomach acid and digestion?
- How strong is your gut lining?
- How well is your immune system working?
It’s not possible to answer these questions on your own. That’s why, if you have GI problems, it’s best to work with me or another functional medicine provider to order the right testing, pinpoint the root causes, and design a customized protocol just for you.
Your path to better gut health begins with a free 15-minute troubleshooting call. During this chat, I’ll get to know more about what troubles you. If after the call you come on board as a patient, I’ll work with you to get rid of diarrhea, constipation, abdominal pain, gas, indigestion, acid reflux, and more. Book your call today and you can say goodbye to those frustrating, painful, and embarrassing GI problems and hello to great gut health!
Recent Studies and Links
As a Functional Gut Health and Hormone Specialist, I'm always learning. There are new studies being released almost daily, and what we know is constantly changing. So a huge part of my job is keeping abreast of the latest developments in functional medicine.
I decided to put together this blog post with some of the most interesting research available to us. "The more you know", and all that!
May 2023
July 2022
Interesting new data on generational trauma → Adverse experiences can change future generations through epigenetic pathways.
May 2022
Is Bone Health at Risk for Adolescents on Birth Control? A new review suggests that benefits continue to outweigh risks when it comes to preventing teen pregnancies
March 2022:
30 Years of Research Shows Sauna Bathing is Game-Changer for Longevity and Heart Disease. I recommend HigherDose Sauna to supercharge your self-care and boost holistic recovery.
February 2022:
Evidence suggests that patients with irritable bowel syndrome (IBS) are hyper-responsive to environmental, physical and visceral stimuli. IBS patients also frequently report poor sleep quality.
66.7% of long haulers tested positive for reactivated EBV, as compared with 10% of controls. The study suggests that symptoms may be related to this reactivation, more so than the initial virus.
January 2022:
A new study published in Science Advances suggests that cannabidiol (CBD), a non-psychoactive compound in the cannabis and hemp plant, significantly reduces the risk of SARS-CoV-2 infection.
Many women have suspected it but finally there's confirmation that Covid-19 vaccines may cause some small changes to the length of their menstrual cycles. A study funded by the United States National Institutes of Health (NIH) found the length of a woman's cycle was impacted by nearly one day on average after each dose of a vaccine, but it did not seem to impact the number of days of bleeding.
December 2021:
According to new research, hormonal IUDs do not have a purely local effect on the uterus – but, instead, affect the entire body. In other words, the contraceptive drug released by the IUD (levonorgestrel) travels to the breasts, brain, and other tissues. And importantly, levonorgestrel is NOT progesterone so acts differently in those tissues compared to progesterone. At the same time, hormonal IUDs can dramatically lighten flow and are arguably the gentlest type of hormonal birth control.
- The Pros and Cons of Hormonal IUDs (Mirena, Kyleena, and Skyla)
- Breast MRI Shows IUDs Have Systemic Effects
September 2021:
Breastfeeding and COVID-19: From Nutrition to Immunity: The accumulated body of knowledge regarding the role of breast milk in the development of the neonatal immune system and protection against infection by other respiratory viruses is discussed, with a focus on the anti-inflammatory role of the antibodies, microbes, and viruses provided to the infant in breast milk and its relevance to the case of SARS-CoV-2.
Groundbreaking FDA-Approved Study: Mushrooms and Chinese Herbs for COVID-19 - Pacific College: Top researchers at the University of California have launched a groundbreaking FDA-approved clinical trial to study natural medicine to fight COVID-19.
August 2021:
The Chinese herbal formula Huoxiang Zhengqi for diarrhea-predominant irritable bowel syndrome (CHAIRS): a study protocol for a double-blinded randomized controlled trial: This study is on a common Chinese herbal formula that has been used for hundreds of years, for nausea, symptoms of food poisoning/travelers diarrhea, and for IBS-D. This trial aims to demonstrate the efficacy and safety of HXZQ for IBS-D, which is expected to be an effective IBS-D treatment.
July 2021:
Black Seed and DHT: Animal studies show that Black Seed might have the potential to block DHT
Reishi Mushroom and Testosterone: Study found that reishi mushrooms reduced 5-alpha reductase levels, thus preventing the conversion of testosterone into DHT
June 2021:
BPA and Crohn's Disease: Evaluating the relationship between endocrine disruptors and Crohn's Disease
Additional Reading:
Check out my Instagram for tips, tricks, and information about gut and hormone health.
What Is Estrogen Dominance and Why Should a Woman Care?
Is Your Birth Control Method Making You Estrogen Dominant?
Irritable? No Sex Drive? Sugar Cravings Driving You Crazy? Birth Control Side Effects May Be to Blame
You’re cranky and feel like snapping at everyone around you.
You’re bloated but can’t stop thinking about that slice of pie or cake you saw at the bakery. It’s screaming for your attention!
Every month, before your period your head feels like someone is pounding it with a hammer. When that time of the month rolls around, you’ve got menstrual cramps like you wouldn’t believe.
Your libido has ghosted you. Sleep sounds more enticing than sex.
These are just some of the symptoms of estrogen dominance. That’s when your estrogen levels are high in comparison to progesterone.
Getting rid of estrogen dominance can work wonders on your mental and physical health. Yet, treating estrogen dominance symptoms never works. You’ve got to dig down to the root cause. I’ve had a lot of success with this approach in many patients.
In a little while I’ll share with you the story of one patient I’ll call Jennifer. By getting at the root cause of estrogen dominance, Jennifer was able to kick estrogen dominance to the curb. The result? Jennifer’s symptoms disappeared. She was happier and more relaxed, lost weight, and her libido was back in action.
I’ll tell you Jennifer’s story in a little while. But first, let’s talk about what is estrogen dominance. That way you’ll know why Jennifer’s treatment worked so well. And why you might have the same stellar results.
Too Much of a Good Thing
Estrogen isn’t always the villain. In fact, women need estrogen for many different areas of health including happy moods, heart health, and fertility.
It’s only when estrogen levels become too high in relation to progesterone that hormonal balance gets thrown off. This is what’s known as estrogen dominance.
Estrogen dominance symptoms include:
- Acne
- Breast tenderness or lumps (aka fibrocystic breasts)
- Breast, ovarian, uterine, and cervical cancer
- Disrupted sleep
- Endometriosis
- Fatigue
- Fibroids
- Headaches or migraines
- Holding on to body fat, especially in hips, thighs, belly, and butt.
- Infertility or subfertility
- Intense sugar cravings
- Low libido
- Mood changes: intense irritability, anxiety, devastating depression
- Stress
- Water retention
- Weight gain
Estrogen dominance can be especially nasty if you’re in perimenopause, the time before entering full menopause. If you’re one of the unlucky ones to be going through both at the same time you might have bad mood swings, horrible PMS, weight gain, and depression. And your libido tanks. Not fun!
What Causes Estrogen To Get Out of Whack?
Remember, our number one goal is to reach a healthy balance of both estrogen and progesterone. In a healthy woman, estrogen and progesterone are balanced and work together in harmony. Progesterone is critical because it counteracts the bad effects of too much estrogen.
There are a number of reasons for too much estrogen or too little progesterone. But hormonal birth control is a very common culprit that most women have never heard about it. A woman might be taking the mini pill or have a hormonal IUD (aka Mirena) and she has no idea it could make her symptoms worse.
Don’t get me wrong. Hormonal birth control has its time and place, but if you’re going to use it you should know about the risks and limitations. You should especially know it won’t fix a hormone imbalance. The problem will still be there after you start taking the pill.
Ironically, birth control is often used to treat symptoms of estrogen dominance like heavy bleeding and painful periods. However, hormonal birth control only makes the estrogen dominance worse.
How does this happen? Hormonal IUDs block ovulation. Without ovulation, you don’t get a healthy rise in progesterone each month. That’s not good. But it gets worse. Just because ovulation stops, doesn’t mean estrogen production stops. You’re still making estrogens- and you’re getting less and less progesterone.
How does your hormonal IUD or mini-pill block ovulation, send progesterone into a nosedive, and allow estrogen to rage out of control? It’s all thanks to progestin, a synthetic form of progesterone.
Doesn’t synthetic progestin work just like natural progesterone? Not at all. In a nutshell, progestin is kind of like progesterone’s evil twin. Progestin doesn’t act like progesterone in the body - it acts more like testosterone, and with none of the benefits of natural progesterone! That’s why it doesn’t improve your PMS, mood, or sleep symptoms.
Progestin-based birth control spells trouble for your body’s hormonal balance. And it throws your progesterone and estrogen levels out of whack.
In fact, the whole reason you might have had heavy periods in the first place is because you suffer from progesterone deficiency!
A Double Whammy
What’s worse, perimenopausal women are often using hormonal IUDs. That’s because several birth control pills’ side effects including risk of stroke, heart attacks, and blood clots, go up after you turn 35. At that time, your doctor may recommend a hormonal IUD. And many women keep using this form of birth control right through the perimenopause period.
Not only are you in perimenopause, which already makes estrogen dominance worse—but you’re also using a birth control device that can cause progesterone levels to plummet. This causes you to go deeper into estrogen dominance. And your symptoms continue to get worse. How crazy is that?
Other Causes of Too Much Estrogen
It’s bad enough that hormonal birth control like IUDs cause estrogen dominance. But if you’ve got one or more other problems going on, everything just gets worse. It’s like a snowball rolling downhill getting bigger and bigger.
Things that worsen estrogen dominance include:
- An overgrowth of bad bacteria in the gut (aka dysbiosis). Bad gut bacteria put estrogen back into circulation where it doesn’t belong.
- Constipation.
- Sluggish liver detoxification, which slows the clearance of hormones from your body.
- Stress, which hampers your ability to make healthy progesterone levels.
- Too much body fat.
- Xenoestrogens accumulate in our bodies and act like estrogens. These chemicals come from plastics, fragrances, pesticides, and processed soy products, to name a few.
Many doctors go after the symptoms of estrogen dominance rather than tackle the root cause. But symptom relief isn’t the same as hormone balance. In fact, trying to relieve symptoms by inserting a hormonal IUD only leads to more hormonal imbalance.
Instead, I go after the underlying hormonal imbalance issues such as healing the gut, balancing hormones, relieving stress, detoxification, and nutrient deficiencies. If these aren’t addressed, your whole health will suffer.
You remember I mentioned my patient Jennifer? Now we’ll get down to the nitty gritty on how I helped her get rid of the root cause of her estrogen dominance. At the same time we switched her over to one of the safest and best birth control methods.
Jennifer’s Path to Hormone Balance and Better Health
Jennifer was a 34-year-old patient of mine frustrated she couldn’t lose weight. She also had digestive problems. She was constipated and only had a bowel movement every third day. She felt bloated, although this symptom improved after she stopped eating gluten, grains, and dairy. Eating too much fat at one time caused her GI symptoms to act up.
To make matters worse, Jennifer struggled with severe anxiety, carb cravings, and low libido.
Sound familiar?
A few years ago, her doctor installed a hormonal IUD. Her periods became light and only lasted three days. This is a common side effect of these devices. In fact, it’s the main reason doctors recommend an IUD, to lighten heavy periods. This is because the progestin in the IUD reduces the thickness of the uterine lining, which in turn leads to lighter bleeding or makes periods go away completely.
Testing revealed Jennifer was estrogen dominant. No surprise there! Her estrogen levels were actually ideal but her progesterone levels had nearly hit rock bottom.
She also had low bile flow. Bile is needed to lose weight and detoxify the body. Bile deficiency happens a lot in women with estrogen dominance.
In addition, lab results showed she had a parasite and the harmful bacteria in her gut were growing out of control.
I felt bad this lovely woman was suffering. I knew we could turn things around for her.
Address Estrogen Dominance and Gut Health to Feel Happier, Sexier, and Lose Extra Pounds
We started working on the root causes of Jennifer’s problems. First, upon my recommendation, she had the hormonal IUD removed and replaced it with a copper IUD. These aren’t as hard on hormonal health. However, the copper IUD can promote heavier periods and increased cramping, especially in the first several months for certain women. In women like Jennifer, I address heavy menstrual bleeding by using Slow Flow and Chinese herbal formulas for one to three months. I supported Jennifer’s natural ability to make progesterone using vitamin C and Vitex.
To her surprise, she lost eight pounds! And she did it without doing anything other than just getting the hormonal IUD removed and taking those few supplements.
At that point I started working on her imbalanced gut bacteria and her sluggish liver, the cause of her low bile flow. The low bile was also the culprit behind her inability to digest fat, which in turn led to bloating and gas, sluggish bowel movements, and low levels of essential fat soluble nutrients such as vitamins A, D, and K.
We addressed the gut dysbiosis and the sluggish liver and—Viola!—her constipation and GI symptoms went away.
Throughout the course of treatment, she also said sayonara to her anxiety, carb cravings, and low libido.
Find Serenity, Boost Your Libido, Cure Carb Cravings, and More
I know how frustrating estrogen dominance symptoms can be. My heart goes out to all women suffering from this condition. I can work with you to pinpoint what’s holding you back from optimum health and turn it around, just like I did with Jennifer.
Your path to peace, sanity, and your best life ever begins with a free 15-minute troubleshooting call. During this chat, I’ll get to know more about what troubles you. If after the call you come on board as a patient, I’ll work with you on estrogen dominance treatments and run the right tests that can put you on the path to vibrant good health. Book your call today and you can feel younger, happier, and more energetic tomorrow.
Dude, Where’s My Period?
Where's my period? To some women, it sounds like a dream…
And when it happens to you, at first you might think… “Hey, that's really not so bad.”
But as a functional medicine practitioner, I can assure you:
Your period going missing IS a problem.
(Or rather, it indicates a problem!)
Today, let’s dig into why your period is so important, and why it might have gone missing (AKA amenorrhea). Plus, how worried should you really be?
Why Your Period Is Really, Really Important
For women of reproductive age, there’s really no other health marker as important as your menstrual cycle.
A normal menstrual cycle is anywhere from 24-35 days long and includes 4 parts:
- Menstrual Phase - this is what we think of as your period, the part of your cycle when you bleed. Hormones are lower at this point.
- The Follicular Phase - this occurs after your period, and is really the start of a new cycle, when the body prepares for potential pregnancy. Hormone levels rise during this part of the cycle as the body prepares an egg to be released during ovulation.
- Ovulation - this is the day somewhere in the middle of your cycle when your body releases an egg in response to peaking LH (luteinizing hormone) levels. Ovulation causes progesterone levels to rise.
- The Luteal Phase - this is the phase after ovulation, when you either get pregnant (which must happen within a few days of ovulation), or don’t. If you don’t get pregnant, you move back to phase 1 and have your period again.
And while talk of the menstrual cycle is very procreation-focused, your menstrual cycle actually isn’t just about getting pregnant or not.
The hormones that are driven to rise and fall by your menstrual cycle play other important roles in your health - most importantly, progesterone, which keeps bones strong and healthy and lowers the risk of certain cancers.
Not only that, but your hormones are meant to exist in balance: each hormone is counterbalanced by another, and if you’re not moving through each phase of the cycle, you can become dominant in one hormone - most commonly estrogen, which should be balanced by adequate progesterone. Estrogen dominance can lead to symptoms like weight gain, mood swings, tender/swollen breasts, and loss of libido.
That’s why moving through each phase of your menstrual cycle is so important, even if you’re not looking to have a baby now (or ever).
If Your Period Is MIA, You Probably Aren’t Ovulating
When you ovulate, an egg is released from the follicle. That follicle becomes the corpus luteum. The corpus luteum produces progesterone, which tells the body to build up a thick lining in the uterus.
If you don’t become pregnant, the corpus luteum withers, and the uterine lining is shed as your period.
What this means is that having a period - where you shed blood - is entirely dependent on ovulating. If you don’t ovulate, there won’t be a follicle to turn into the corpus luteum, so your body won’t be told to build up the uterine lining, and there won’t be anything to shed.
What I’m getting at is that a missing period tells us you’re not ovulating. And that’s what really matters, because it is ovulation that produces estrogen-balancing, bone-protecting, cancer-risk-reducing progesterone.
Now there are a couple exceptions: some women who ovulate irregularly may have bleeding, even without ovulation. It is more likely that you won’t - but it can happen.
Secondly, women who are on hormonal contraceptives (the birth control pill), may bleed every month, but are not ovulating (because hormonal contraceptives suppress ovulation). The “period” that you have on a hormonal contraceptive shouldn’t be thought of as a true period. Instead, it is actually a “withdrawal bleed” because the bleeding is triggered by the withdrawal from the artificial hormones during the placebo week of your birth control pill.
Is Your Period Up and Gone, Or Just Flaky?
When I’m working with a patient who has missing periods, here are some of the questions I ask to help point me in the right direction toward the cause, and ultimately, the solution.
Did you ever have normal cycles?
If you used to have normal, predictable cycles - and then suddenly they stopped or became unpredictable, that suggests to me something has disrupted your otherwise healthy hormones. If you’ve never had a normal cycle, all’s not lost- it just points me in a different direction.
Has your period been gone for months (or years) straight, or is it just unpredictable?
A period that comes and goes can suggest oligoovulation - which means ovulation is unpredictable. Anovulation is the complete absence of ovulation. Again, neither one means all hope is lost: this can just help suggest what might be going on.
Did you have any major life changes around the time your period disappeared?
This is another important detective question. The menstrual cycle is delicate - and is designed to prevent pregnancy during times of extreme stress or upheaval (since having a baby in a famine or war wasn’t really ideal for our ancestors!). It’s a good idea to try and create a timeline of when your period went missing and what was going on in your life at that time.
Reasons Your Period Could Be Missing
Now that you know why it matters that your period is missing, let’s get into the good stuff: figuring out why your period is gone!
Here is a list of the most common causes of a missing period I see with my patients:
Pregnancy
Ok, this one is pretty obvious: if you’re pregnant, you won't have your period. Luckily, it’s also really easy to rule out: if there’s any chance you could be pregnant, take a pregnancy test and know for sure.
Perimenopause
On the opposite end of the spectrum from pregnancy is the possibility of perimenopause. Perimenopause is the years-long period before the onset of menopause, when your hormone levels start fluctuating and your periods can become suddenly abnormal. In perimenopause, you might have longer cycles (34+days), skip a few cycles, or have lighter or heavier periods. Other perimenopause symptoms include mood changes, hot flashes, and night sweats. Perimenopause begins for most women sometime in their 40s - if you think you’re experiencing perimenopause early, that is something we can address. Even if you’re the “right age” for perimenopause to have begun, it is a myth that perimenopause has to be a horrible time. There is so much we can to help stabilize hormones and provide symptom relief as your body goes through this big (normal) change.
Polycystic Ovarian Syndrome (PCOS)
PCOS is a hormonal disorder that affects millions of women (myself included). It is distinguished by elevated levels of androgens (male hormones) and the absence of regular ovulation. (Remember, no ovulation = no period.) PCOS is complex to both diagnose and treat - but it can be done. Click here to read my ultra in-depth blog post on all aspects of PCOS and learn more about treatments.
It should be noted that PCOS can occur alongside another cause of a missing period, commonly hypothalamic amenorrhea (HA).
Hypothalamic Amenorrhea (HA)
Hypothalamic amenorrhea (amenorrhea is the technical term for a MIA period) is a hormone imbalance that prevents ovulation caused by 1) over-exercise, 2) stress, 3) undereating, or 4) some combination of all 3. If you used to have normal cycles, and suddenly lost them, HA is one to consider. Your physiology is designed to prevent ovulation (and therefore, reproduction) when stress is high or nutrition levels are low, and HA is a result of this. Some women experience HA even when at a normal weight, or doing an amount of exercise that is deemed normal by society. Developing HA is all about crossing your body’s threshold, and that level is different for all women.
There is no definitive test for HA, and it is usually diagnosed by eliminating other causes of a missing period first. If you have HA, learning to manage stress, eating more, and exercising less can all lead to the restoration of normal cycles, though the process can take time.
HA can occur alongside PCOS, but doesn’t always.
Premature Ovarian Failure
This condition occurs when the ovaries stop functioning normally at an early age. This can cause irregular, come-and-go periods, rather than a complete stop.The exact cause of premature ovarian failure is unknown, though its thought genetics and autoimmunity may play a role. Unfortunately, premature ovarian failure usually causes infertility, but treatment with bioidentical hormones can help manage other symptoms.
High Prolactin
Prolactin is the hormone that causes the breasts to produce milk, and it also suppresses ovulation. If you’re breastfeeding exclusively, high levels of prolactin can keep your period at bay. But if you’re not breastfeeding, high prolactin indicates a serious issue. It can be a result of a tumor on the pituitary gland or thyroid issues. Besides a missing period, tell-tale signs to look for are a milky discharge from the breasts, vaginal dryness, and acne.
Hormonal Contraceptives
Hormonal contraceptives (AKA the birth control pill, patch, ring or hormonal IUD) work by suppressing your body’s natural production of hormones and replacing them with artificial counterparts. Most hormonal contraceptives suppress ovulation, and the only “period” you get is a withdrawal bleed during the placebo week of the pill. Some pills allow you to skip the placebo week - sometimes called continuous pills - and skip the withdrawal bleed altogether. One exception is the hormonal IUD (Mirena), which doesn’t always stop ovulation, but often still causes lighter or absent periods.
So, does this mean hormonal contraceptives are bad? It’s a little more complicated than that. Hormonal contraceptives have a time and place. However, there are other non-hormonal birth control options I prefer - check those out here. And I don’t like seeing hormonal contraceptives used as a “treatment” for hormone issues like PCOS or heavy periods, because all they can do is cover up these issues, not fix the root cause.
Post-Pill Amenorrhea or Post-Pill PCOS
Recently stopped using hormonal contraceptives? That could be a cause of a missing period. Post-pill amenorrhea is a condition where periods remain absent after going off the pill. When you’re using hormonal contraceptives, your body’s normal hormone production is shut off. When you quit the pill, it can take time for hormone production to normalize, and a missing period can be the result. This should resolve in a couple months - if it takes longer, seek help. With my clients, focusing on diet, lifestyle, and key supplements can help speed up this process. Post-pill PCOS is similar - when hormones come back online after using the pill, androgens (male hormones) may surge, causing a temporary state of PCOS. Jumping in right away to help normalize hormone levels can help prevent this imbalance from becoming permanent. See this post for more on PCOS.
Stress, Illness, or Travel
One of the simple explanations of a missed cycle? Periods of intense stress - whether psychological or physical, which can result in missing or delayed periods. The “stress hormone” cortisol is to blame. When you experience stress, your body produces more cortisol to help you respond to the stress. However, cortisol also interferes with communication between your brain and ovaries, where hormones are produced, preventing ovulation and therefore, your period. One missed or late cycle after a period of stress is likely NBD - as long as things normalize again quickly. But if you are chronically stressed, there are steps we can take to support your body in managing cortisol to hopefully take the burden off your menstrual cycle.
Chronic Disease
This is one of the less common reasons I see for missing periods, but it does happen. Again, your body will shut down reproduction first thing if it senses you’re not well enough to successfully reproduce, as a protection mechanism. If you have a chronic disease that is constantly taxing your body, it makes sense that your cycle could be disrupted. Most commonly, I see this with women with undiagnosed or poorly managed Celiac disease, since Celiac prevents proper nutrient absorption and causes chronic inflammation. Treating the chronic condition (and getting it under control) can help restore normal cycles again.
Thyroid Issues
An overactive or underactive thyroid (Hypo or hyper hypothyroidism) can also be a cause of missing or skipped periods, among other symptoms like feeling hot/cold, weight gain or loss, and hair loss. If you’re missing your period, and don’t know why, a full thyroid panel is a great place to start to rule out the possibility of thyroid issues.
How Do I Know Why MY Period Is Missing?
Now that you know the most common reasons your period could be missing, the next step is to narrow it down to what the issue is for you.
Some of these potential issues are easy enough to rule out, but for the rest, testing is the next best step. With my own clients who are struggling with amenorrhea, I use a combination of blood, saliva, and urine tests to help narrow down the root cause. (And if you are working with me, I’ll help you figure out which tests you can ask your regular doc to order and bill through insurance, too!)
Once we know the root cause, we can create a customized treatment plan to help restore ovulation and normal, healthy cycles.
If you’re missing your period and need support finding the root cause and getting it back, book a free 15-minute consult to get started working with me. This no-obligation first call is like a coffee date where we can test the waters and see if working together might be a good fit.
>>> Book a no-obligation free consultation <<<
Whether you’re trying to get pregnant or just worried about what a missing period means for your ehealth, I’d be honored to help get your cycles back on schedule.
Brie
PS - If there's ONE thing you take from this article, let it be this: missing your period is NOT normal, and needs to be addressed! In fact, a missing period is a major red flag that something is not quite right with your health. Don’t ignore it!
Recipe: Nourishing Water Kefir Jello
Want a recipe that’s nourishing for your gut, skin, hair, and nails… but also really delicious and fun to eat?
(I’m talking so delicious and fun… my 2-year old daughter begs for it!)
Let me introduce you to one of my all-time favorite easy and healthy snacks: water kefir jello!
I “invented” this water kefir jello back when my daughter was just getting started eating solids. I wanted to give her something ultra-healthy, packed with nutrients, and low in sugar… but also easy to eat.
Then I tried it myself… and got hooked!
This water kefir jello is definitely NOT just for kids… and no matter what age you are, you’ll get all the health benefits.
What's In Water Kefir jello?
This recipe has just a few ingredient, but they’re all ultra nutrient-dense:
Water Kefir - This is a naturally probiotic-rich fermented drink that is similar to kombucha. You can get it in health food stores - although more and more traditional grocery stores carry it now, too. The benefits come from the naturally-occurring probiotics, which are great for maintaining a healthy and diverse gut microbiome.
Not all water kefirs are created equally: look for one that is low in sugar, and doesn’t contain any artificial flavors or colors. My favorite brand is Kevita Sparkling Probiotic Drink - and for this recipe, I almost always use the Pomegranate flavor!
Fresh Citrus Juice - Your choice of fresh citrus juice adds bright sweet-tart flavor to this recipe… and provides plenty of immune-boosting vitamin C. I usually use lemon or lime juice, but grapefruit juice is also great in this recipe.
Monk Fruit Extract - this is a no-calorie, all-natural sweetener made from extracts of monk fruit. It’s rich in antioxidants and my favorite alternative to sugar. A little goes a long way - monk fruit extract is about 200x sweeter than table sugar. My favorite brand is Emerson’s Liquid Monk Fruit.
Grass-Fed Gelatin - Gelatin is packed with collagen. Collagen is the most abundant protein in the human body, and is a major component of our hair, skin, nails, and joints. Supplementing with collagen not only helps your hair and nails grow faster, longer, and stronger, but it can also help repair the lining of the gut, an essential step in healing a leaky gut. Even if your gut is healthy now, collagen is one of my top foods for retaining a strong gut lining going forward.
Some of the many benefits of consuming collagen include:
- Healing leaky gut
- Improving joint pain in those who exercise
- Improving the look of cellulite (In women who are normal weight - usually one of the hardest populations to treat!)
- Prevent the loss of bone density (Which is a huge issue for women, who deal with osteoporosis far more commonly than men)
- Reduce the appearance of wrinkles
Choosing an organic, grass-fed gelatin is important, because conventional cattle are exposed to high levels of the glyphosate in their lives, since they eat a diet primarily of glyphosate-treated corn and soy. Glyphosate builds up in the collagen-rich tissues of animals… and winds up in high levels in gelatin and collagen powders.
The WHO has labeled glyphosate as a “probable human carcinogen” since 2015, and there have been numerous lawsuits attributing glyphosate exposure to the development of cancer. It’s also a known endocrine disruptor, which means it messes with normal hormone levels and function. Not good! To avoid this, choose an organic, grass-fed brand. My favorite is Vital Proteins (Make sure you choose the gelatin in the green tub!).
Gelatin vs. Collagen Peptides: What’s the Difference and Does It Matter?
This recipe calls for gelatin, not collagen peptides. So what’s the difference?
Collagen peptides and gelatin are really similar - they both have basically the same amino acid profile, the same nutrients, and are both naturally flavorless.
The big difference is that gelatin is a cooked form of collagen, and the cooking process changes the chemical structure a bit, resulting in some different qualities.
Collagen peptides dissolve instantly in hot or cold liquids. They don’t have any gelling properties: they won’t change the texture of whatever you mix them into. That makes them great for adding to coffee, smoothies, soup, and even yogurt.
Gelatin, on the other hand, must be dissolved in warm or hot liquids - and once it cools, it creates a thick gel. If you mix gelatin into your morning coffee, and then let it cool… you will have coffee gel! Gelatin can only be used in things that will stay hot, or that you don’t mind gelling - like water kefir jello.
Both collagen peptides and gelatin have many benefits and uses. I use both - just not interchangeably. If you want to get the most benefits from collagen, I recommend using a collagen peptides supplement in addition to recipes like this one, which contain gelatin.
For this recipe, you must use gelatin, not collagen peptides, or your water kefir jello won’t gel!
I hope you enjoy this recipe as much as my family does!
Nourishing Water Kefir Jello
Hands-On Time: 15 minutes
Cooling Time: 4 hours
Ingredients:
- 3 ½ cups of water kefir
- ½ cup lemon or lime juice*
- 5 tablespoons grass-fed gelatin**
- Liquid monk fruit extract, to taste
* You can substitute any other citrus juice for lemon or lime. If using a different citrus juice, increase the amount to 1 cup and decrease ½ cup from the amount of water kefir used in Step 1.
** Do not substitute collagen peptides for gelatin. Collagen peptides do not gel when cooled, and therefore can’t form jello! Gelatin must be used for this recipe to gel.
Directions:
- Combine 2 ½ cups of the water kefir with the citrus juice in a medium bowl
- Add monk fruit extract to water kefir and juice mixture to taste (Approx. 2 droppers)
- Add remaining cup of kefir water to a small saucepan and sprinkle gelatin powder on top.
- Heat water kefir and gelatin mixture over very low heat until just slightly warmed and gelatin begins to dissolve. Do not bring to a simmer or boil, as this will kill the probiotics!
- As soon as gelatin begins to dissolve, remove from heat and whisk thoroughly to dissolve all gelatin.
- Add water kefir and gelatin mixture to water kefir and juice and stir to combine.
- Pour the entire mixture into a glass baking dish or mold, such as silicone ice cube molds.
- Cool in the fridge for at least 4 hours. Enjoy!
PCOS 101: Everything You Need to Know About Polycystic Ovarian Syndrome
I’ve been where you are right now… Maybe your doctor just told you, “You have PCOS.” Maybe you’re questioning it yourself… Googling for answers.
Or maybe - and this might be the most frustrating situation of all - you’ve been told for YEARS you had PCOS, only to be told now, you somehow, suddenly don’t.
The fear, overwhelm, frustration, uncertainty - I get it! (I have PCOS, myself.)
Nothing about PCOS is straightforward. (Even the name doesn’t make sense!)
So let me hold your hand for a minute - today I want to explain everything you need to know about PCOS, start to finish.
What Is PCOS?
PCOS stands for Polycystic Ovarian Syndrome - and it’s an endocrine (AKA hormonal) disorder that affects women of reproductive age.
PCOS is the most common hormone dysfunction among women and affects 10-20% of all women of reproductive age.
(That means if you get a group of 10 of your friends together, it’s likely 1-2 of you will have PCOS!)
And despite the name, PCOS really has nothing to do with cysts on your ovaries. Instead, PCOS is a condition marked by elevated levels of androgens (commonly called male hormones.) This is often testosterone, but can include other androgens.
People with PCOS often also have elevated luteinizing hormone (LH), and prolactin and lower follicle stimulating hormone (FSH).
And while your doctor might not make a big deal out of it, the truth is that PCOS is a lifelong disease with big medical and emotional impacts, and potentially the additional burden of obesity.
What Are The Symptoms of PCOS?
Symptoms of PCOS include:
- Hirsutism
- Male pattern hair loss or thinning
- Acne
- Oligo or amenorrhea (chronic anovulation)
- Obesity
- Sub/ Infertility
- Low libido and sexual problems
- Skin tags or darkened skin in the folds (acanthosis nigricans)
- GI problems (IBS, leaky gut)
- Arthritis and tendonitis
- Depression, anxiety, stress, eating disorders, and body dysmorphia
- Increased vaginal infections
- Sleep dysfunction
- Increase in certain cancers (uterine and breast)
- Increased rates of other gyn conditions, like fibroids, endometriosis
PCOS can also lead to:
- Pregnancy complications
- High blood pressure
- Diabetes
- Dyslipidemia
- Fatty liver
- Higher risk of cardiovascular disease
PCOS can present very differently in different women, and there are at least 4 different types (more on that to come).
One big misconception? That all people with PCOS are overweight. Although overweight/obesity is common in PCOS, it is not a symptom for all people with the condition.
Another misconception is that PCOS causes painful periods or pain. That’s not true either. If you have pain or painful periods, it is likely caused by something else (though it’s possible you have PCOS, too - it just isn’t the cause of the pain!)
How Do I Know If I Have PCOS?
How PCOS is diagnosed has changed over the years, which is part of why there is so much confusion around who does and doesn’t have PCOS. If you’ve been told you did have PCOS, but don’t now - the changes in diagnostic criteria explain why.
In the past, PCOS was diagnosed primarily based on missing or irregular periods and the presence of multiple cysts on the ovaries, as seen via ultrasound.
But now we know that there are many reasons cysts can appear on the ovaries - and sometimes, those cysts are entirely normal and not indicative of any disease state.
That’s why, today, PCOS is diagnosed based on updated guidelines from 2018 for missing or irregular periods AND androgen excess, which is determined as:
1) high androgens (male hormones) measurable on a blood test,
and/or 2) significant facial hair or jawline acne.
PLUS other reasons for androgen excess have been ruled out.
Ultrasound is no longer required to diagnose PCOS, though many practitioners still do perform one.
Even if you are missing periods, or have them irregularly, or if you had an ultrasound that featured cysts on your ovaries, if you do not have androgen excess as defined by labs or symptoms mentioned above, then it’s not considered PCOS. (Missing your period, but no androgen excess? There are lots of other reasons for missing periods. Read more here.)
Other signs of PCOS include the following, but these all are not always present, even with PCOS:
- Bilateral polycystic ovaries
- Elevated LH and LH to FSH ratio
- Oligoovulation (irregular or infrequent ovulation)
- Elevated free testosterone and DHEAS
- Glucose intolerance and elevated insulin
When Hormone Levels Are “Normal” But You Still Have PCOS Symptoms
If you have key symptoms of androgen excess - such as severe jawline acne and facial hair growth - but your lab tests are normal, don’t rule PCOS out.
Some women are extremely sensitive to even “normal” amounts of androgens. This means that even with normal levels, they may have key symptoms like jawline acne and facial hair growth. That’s why the guidelines state that PCOS diagnosis can be based on either elevated androgen levels on a blood test or symptoms of high androgens.
But, there are also other conditions aside from PCOS that can cause the symptoms of androgen excess, including:
- Congenital adrenal hyperplasia (an inherited condition that impacts the adrenal glands and sex hormones)
- High prolactin secretion
- History of using an oral contraceptive pills that contain progestins, which behave more like testosterone than progesterone in the body
Is It PCOS… Or Something Else?
Other conditions can sometimes be mistaken for the more-common PCOS. These include:
#1 Non-Classic Adrenal Hyperplasia (NCAH)
This condition is similar to congenital adrenal hyperplasia, but comes on later in life (usually around the time of puberty) and is not as severe. For women, symptoms include delayed first period (menarche), male-pattern hair growth and loss, and infertility. It is hard to tell the difference between PCOS and NCAH, but if a person presents with PCOS symptoms and is not insulin resistant, it could be NCAH - though some people with NCAH do have insulin resistance. NCAH is more rare than PCOS. The only way to distinguish PCOS from NCAH with certainty is by measuring 17-hydroxyprogesterone levels.
#2 Functional Hypothalamic Amenorrhea
This is the loss of normal menstrual cycles due to overexercise/undereating, and it often occurs in both normal and underweight women. It can be really difficult to distinguish a woman with FHA from a woman with PCOS who is lean. Tell-tale signs that it is FHA include low to normal basal FSH and LH levels and low estrogen (vs. elevated serum LH levels and low to normal FSH levels in women with PCOS). Women with FHA don’t usually have the severe jawline acne or male-pattern hair growth seen in PCOS. On an ultrasound, both women with PCOS and FHA may have cysts, but the ovaries and uterus of a woman with FHA are small or normal, whereas a woman with PCOS typically has increased ovary size. To make it a little more complicated… it is possible to have both PCOS and FHA simultaneously.
What Causes PCOS?
The exact cause of PCOS is not known, but it is likely a combination of genetic predisposition and environmental effects. Some known risk factors are:
- Mother had gestational diabetes (it’s thought that the exposure to higher levels of insulin levels in utero could lead to PCOS in adulthood).
- Exposure to endocrine disrupting chemicals in utero or in life. So far the focus has been of BPA.
- Diabetes or metabolic syndrome in first degree relatives
- Gut inflammation, such as IBS, SIBO, or leaky gut (because they cause chronic inflammation)
- Higher levels of oxidative stress, beginning in utero and continuing through life
- Vegetarian diet, which may contribute to low levels of zinc and
- Autoimmunity
- Hypothyroidism
It’s also suspected that a genetic mutation of the CYP17 enzyme, which is responsible for forming androgens from DHEA-S, could play a role.
Beyond these risk factors, it isn’t known exactly why some women develop PCOS and others don’t.
While what starts the initial process of PCOS remains mostly unknown, we do know what happens in the body that leads to PCOS. It’s a hormonal cascade that starts with hypothalamic gonadotropin-releasing hormone (GnRH).
First up, in a woman without PCOS, here’s what happens: hypothalamic gonadotropin-releasing hormone (GnRH), stimulates the release of LH - luteinizing hormone. The LH tells special cells in the ovaries called theca cells to convert cholesterol (a type of fatty acid in the body) into two androgens: testosterone and androstenedione. The androgens then move into the granulosa cells, where the hormone FSH (follicle stimulating hormone) converts them into estrogen via a process called aromatization.
But in a woman with PCOS, the process gets stalled out before the androgens can be converted into estrogen. Here’s what happens...
Women with PCOS have increased pulsatile GnRH release, which results in higher levels of LH and lower levels of FSH in most individuals. These higher LH levels cause increased androgen production by follicular theca cells. That means a woman with PCOS has more androgens to convert to estrogen to start - plus a lower FSH level, which is the hormone needed to convert the androgens to estrogen.
All those extra androgens in the ovaries stop the normal growth and maturation of follicles, and prevent ovulation. As a result, the ovaries wind up with lots of small, antral follicles that become cysts on the ovaries. This enlarges the ovaries and can also create an elevated serum estrogen level.
But that’s not all! In addition, the cells of people with PCOS respond to normal levels of the “blood sugar hormone” insulin by making increased amounts of testosterone. In a woman without PCOS, these levels of insulin would not result in excess testosterone.
This is intensified by the fact that women with PCOS also are far more likely than people without PCOS to have insulin resistance and elevated insulin levels.
PCOS and Insulin Resistance
PCOS and insulin resistance have a complex relationship: insulin resistance is both a symptom and a potential cause of PCOS.
But before we dig any further, let’s do a quick refresher on what insulin and insulin resistance are.
Insulin is a hormone secreted by the pancreas in response to blood sugar. When you eat food, it is broken down and absorbed into the bloodstream in the small intestine. This causes a rise in blood sugar. In response to this rise in blood sugar, the body pumps out insulin from the pancreas. The insulin helps shuttle the sugar out of the bloodstream and into the cells, where it can be used as energy.
Insulin resistance is one way this system can break down. Essentially, the pancreas continues making insulin, but the body stops listening. That can lead to both high levels of insulin (because the pancreas keeps making more) AND high blood sugar levels, since the insulin isn’t doing its job of moving the sugar out of the bloodstream and into the cells.
Insulin resistance is often the first step on the road to developing Type 2 diabetes and gaining weight, which is harder to lose.
Insulin resistance is very common in PCOS: even in non-obese women with PCOS are far more likely than other women of the same weight without PCOS to wind up with insulin resistance.
And while we don’t know for sure if the PCOS causes the insulin resistance… or the insulin resistance causes the PCOS… what we do know is that high levels of insulin stimulate the ovaries to make more testosterone. At the same time, high testosterone levels in women lead to insulin resistance and weight gain.
Being overweight with PCOS only intensifies the metabolic problems. Excess fat cells lead to fatty acids spilling into the bloodstream. Combined with the low antioxidant and high oxidative stress seen in PCOS, this leads to increased oxidation of the fats, which damages tissues. This creates yet another cycle where oxidative stress increases testosterone production, which only increases insulin resistance. Once this cycle is set in motion, it’s really difficult to stop.
PCOS is also inflammatory, and this inflammation further increases insulin resistance and abdominal visceral fat. The inflammation also promotes abnormal adipose function with inappropriate adipokine release. Adipokines include the “hunger and fullness” hormones leptin and ghrelin.
PCOS and The Microbiome
PCOS doesn’t just affect your hormones, however. It can also have major, negative consequences for the microbiome.
The microbiome is the collective name for all the bacteria that live in your gut and perform vital roles in digestion, metabolism, hormone production, and communication between body systems.
Stool testing showed the microbiome of people with PCOS was less diverse and had an altered composition compared to healthy controls.
The dysbiosis in the microbiome that PCOS can cause promotes even more inflammation, as well as allergies and autoimmunity. Research has shown that women with PCOS (both those who were lean and those who were overweight) had significantly higher LPS levels, a marker of inflammation and leaky gut, compared to healthy controls.
And, in another example of the way PCOS symptoms can be self-perpetuating, a dysbiotic microbiome as a result of PCOS could contribute to further weight gain and insulin resistance, further fueling excess androgens. Studies have shown that changes in gut microbiome trigger mechanisms that promote obesity, Type 2 diabetes, and metabolic syndrome. And, it’s known that people with Type 2 diabetes also have an altered microbiome.
Both obesity and dysbiosis, two common results of PCOS, directly increase gut permeability (leaky gut), which promotes insulin resistance, which drives further testosterone production in the ovaries, creating PCOS, which impairs ovulation and promotes further androgen dominance.
Bottom line: if you’re struggling with weight loss and obesity, and have PCOS, a dysbiotic microbiome could be a reason why.
What Happens If PCOS Is Ignored
For most people with PCOS, symptoms like unwanted facial hair and jawline acne are enough to make them want to seek treatment. PCOS can really impact quality of life.
But even if PCOS symptoms aren’t bothersome, leaving this condition untreated long-term has serious consequences.
Of course, PCOS affects fertility: it is more difficult or impossible for those with PCOS to become pregnant due to their irregular/absent ovulation.
However, even if you never want to become pregnant, PCOS does far more than affect fertility.
The high androgens produced in the ovaries lead to insulin resistance and inhibited ovulation. The insulin resistance puts you at risk for Type 2 diabetes and weight gain. In addition, even if insulin resistance isn’t a feature of your PCOS, the high testosterone levels seen in PCOS also increase the risk of Type 2 diabetes.
The inhibited ovulation leads to low levels of progesterone (because progesterone rises when ovulation occurs). Progesterone should balance estrogen, but when progesterone is low estrogen can become chronically high, and over a lifetime this increases the risk of estrogen-driven cancers like ovarian and breast cancer. Both low progesterone and absence of ovulation have been linked with significantly higher risk of breast cancer.
And, because another role of progesterone is to block androgens, the absence of progesterone only adds fuel to the fire. In this way, PCOS becomes a self-perpetuating cycle. This means it’s very unlikely to just “go away” on its own.
Is There Hope for Healing PCOS?
I know that this blog post has been really heavy so far.
Lots of scary symptoms and confusing hormones… that might leave you feeling like “Is there any hope for healing PCOS??”
So let me reassure you right now: there IS hope for healing PCOS!
I speak from personal experience - I was diagnosed with PCOS in my twenties. In fact, it was this diagnosis that really lit a fire in my soul for natural healing.
Today, my PCOS is well managed. My weight is stable, I have hair on my head, not my face. I was able to get pregnant and give birth to a beautiful daughter. To be totally transparent, we did use IVF - but I had PCOS, was almost 40, and have only one ovary! With those factors in mind, it went as smoothly and easily as it possibly could have - due in large part to the work I had done to optimize my health and hormones.
Life is good… and I want these kinds of results for you, too!
The rest of this article will be dedicated to healing PCOS.
Step 1 to actually treating PCOS is determining what type of PCOS you have.
The 4 Types of PCOS
While PCOS is the umbrella term, clinically, I see people with PCOS fall into one of four categories based on their symptoms and presentation.
Knowing what type of PCOS you have is critical because it guides what treatment plan will be most effective for you.
Read through all four types and see which one you identify most with.
Type #1: Insulin Resistance PCOS
Insulin Resistance PCOS is the most common type, and accounts for about 70-75% of all PCOS cases. The defining criteria? If a patient has insulin resistance of any degree and PCOS, they have Insulin Resistance PCOS. In addition, if you have pre-diabetes, you likely also are in the Insulin Resistance PCOS category.
High insulin levels promote high androgens, creating PCOS.
What years of working with PCOS patients has taught me is that, usually, there is some level of insulin resistance present in people with PCOS, even if it’s subtle. One tell-tale sign I look for are changes in energy levels after eating. In a healthy person, eating should only make you feel less hungry. If eating makes you feel tired and sluggish, or conversely, clears your head and gives you a major boost of energy, that’s a red flag.
To know if you have insulin resistance, your blood can be tested for high insulin levels using a fasting insulin test. Fasting glucose and hemoglobin A1c blood tests can also help provide a snapshot of your body’s response to insulin. However, sometimes a person has a normal fasting insulin, but still has a poor glycemic response to carbs. This means their blood sugar spikes above 140 or that their insulin resistance is more exaggerated than it should be. To assess this, an oral glucose tolerance test is used. Glucose tolerance tests are preferred because they can catch insulin resistance at lower levels and in earlier stages.
Another option is at-home glucose monitoring with a glucometer or continuous glucose monitor. I love this option because no doctor’s orders are needed (you can get a glucometer and test strips over the counter) and it can provide a bigger picture of what’s happening to your body when you eat real food over a longer period of time. If you want an exact, step-by-step guide to tracking your glucose measurements over the course of 3 days, click here to download my free At Home Blood Sugar Testing Guide.
Type #2: Inflammatory PCOS
All types of PCOS feature some inflammation, but in Inflammatory PCOS, inflammation is the hallmark symptom, and insulin resistance isn’t present.
People with Inflammatory PCOS often have known causes of chronic inflammation or other inflammatory symptoms and conditions, like:
- Autoimmune disease
- IBS or SIBO
- Joint pain or body aches
- Chronic headaches
- Chronic fatigue
- Depression
- Skin issues like eczema or psoriasis
Sometimes, Inflammatory PCOS is best diagnosed by ruling out the 3 other types. If you’re feeling uncertain if this type describes you, keep reading about the other types.
Type #3: Post-Pill PCOS
For some people, stopping hormonal birth control pills can lead to the development of PCOS. Stopping the artificial progesterone in the pill (called progestins) can cause a temporary surge in androgens that creates PCOS. This is most common with Yasmin, Yaz, and the Mirena IUD, although it can happen with other pills
People with this type of PCOS usually report that their periods were normal before starting the pill, and symptoms only began once they stopped. The good news is that, if treated, this type of PCOS is usually more temporary. Detox support and herbs that lower androgens can often reverse this type. (More on treatments to come.)
Type #4: Adrenal PCOS
Adrenal PCOS is largely genetic, but can also be triggered by extreme stress, weight loss diets, overexercise, and lack of sleep, all of which further tax the adrenal system.
Adrenal PCOS often looks a lot like congenital adrenal hyperplasia (CAH), which was discussed above. However, unlike with CAH, with Adrenal PCOS, 17-OH progesterone won’t be elevated. In addition, women with adrenal PCOS often only have elevated DHEAS, not testosterone or androstenedione.
For this type of PCOS, the best approach is supporting adrenal hormone function and managing stress, alone with nutrients and botanicals that help normalize androgens.
My Treatment Goals for PCOS
When you have any goal - but especially a big health goal like treating PCOS, it’s important to break it down into smaller, trackable, manageable goalposts.
PCOS treatment isn’t a one-pill-and-you’re-done kind of thing… it can take months of consistent work to see changes. Having clear-cut goals in mind helps power you through the process.
(And we also have health coaches on staff who are specially trained in helping you break down goals and achieve them step-by-step!)
My PCOS treatment goals include:
- Regulating hormone levels (increasing progesterone secretion, LH:FSH, decreasing prolactin)
- Improving the stress response and HPA (hypothalamus-pituitary-adrenal) function
- Optimizing the microbiome
- Optimizing detox pathways and function
What About Standard Treatments?
Two of the most common standard treatments for PCOS are hormonal contraceptives and the drug metformin.
Metformin is an insulin sensitizing drug that can help with insulin resistance. However, it doesn’t enhance ovulation for many patients. As far as drugs go, I don’t think metformin is a bad one, and it may have some benefit for you. Talk to your doctor about it. But, because metformin tends to displace vitamin B12, be sure to supplement or monitor your levels while using it.
Hormonal contraceptives (aka the birth control pill) are one of the most common “treatments” for PCOS, but aren't one I recommend. That’s because all the pill cna do is further suppress ovulation and hormone production - it does nothing to address the root cause of the imbalance. When you inevitably stop the pill (and all women have to stop the pill at some point, even if only because increased age has made the risk of blood clots too high), PCOS symptoms come roaring back.
Birth control pills also contain artificial progestins, which actually behave more like testosterone in the body than they do real progesterone. For women with PCOS, this can exacerbate symptoms.
Furthermore, one of the biggest issues with PCOS is that it suppresses ovulation, and ovulation is necessary for healthy hormone balance, preventing cancer, and maintaining bone integrity. The birth control pill also suppresses ovulation… which means it does nothing to fix the problem.
Step #1: Testing
Testing is an essential step for my work as a practitioner. But I’m not just talking about the run-of-the-mill tests you’ve likely had before… I use advanced, in-depth testing to get a deep look at what is happening throughout your body.
Here’s some of the tests I commonly use with PCOS patients:
- Testosterone
- SHBG
- DHEA
- Epi-Testosterone
- 5a-Androstanediol
- 5b-Androstanediol
- DHT
- Androsterone
- Etiocholanolone
- Estradiol
- Prolactin
- AMH
- LH
- FSH
- C-RP
I prefer to use the DUTCH Complete test for most of these hormones and metabolites, but they can also be tested via blood serum, as well. Some are only available via serum testing.
In addition to these, I also run some tests to rule out other conditions and assess overall health:
- 17-OH progesterone, to rule out CAH
- Thyroid panel, to rule out amenorrhea due to thyroid issues, and because thyroid issues often co-occur with PCOS
- Lipid panel, to assess metabolic syndrome and cardiovascular risk
I also sometimes use a month-long cycling panel to assess ovulation, and to look at overall progesterone levels/exposure over the month/cycle, because you can’t assess this with a one day snapshot. To do this, I use the Menstrual Cycle Mapping test from ZRT Labs or the Oova. Oova catches LH surges and can confirm ovulation, even in women with PCOS. This is HUGE because standard ovulation tests can’t detect the LH surge, since LH is already high in women with PCOS. For more on the Oova, read this. The Menstrual Cycle Mapping measures progesterone, LH, and estradiol, which can be really useful in some cases.
Step #2: Add Lifestyle Changes
The lifestyle changes I have patients implement vary based on their unique case, but there are some general principles that help most people with PCOS.
First, and maybe most importantly: prioritize sleeping 8 hours per night.
And while I know everyone says this… you also have to find a way to manage stress that works for you. Research has shown people with PCOS actually have a greater stress response than women without PCOS, even when the stressor is the same. It makes women with PCOS more inflamed, and more likely to experience anxiety and depression, too.
Some of my favorite tools for managing stress:
- EMDR therapy (with a trained practitioner)
- The ApolloNeuro wearable - this uses specialized touch therapy against your skin to promote feeling of calm and well-being. There is nothing else like it available!
- Inaura.com - a new platform that provides a wide array of therapies to help deal with stress and trauma
In addition, improving diet can help, too. I recommend eating 2-3 meals per day of an organic, plant-heavy diet avoiding gluten, most dairy, artificial sweeteners, trans fat, and alcohol. Eat plenty of healthy fats - like olive, coconut, and avocado oils, plus high quality animal fats, but avoid trans-fats. And if your diet is lower in carbs, be sure you’re including lots of variety of veggies to get the plant fibers your gut microbiome needs to thrive. And, if you’re not overly sensitive to caffeine, add 2-3 cups of green tea daily.
Step #3: Supplement Smart
Most people want to start with supplements, but it’s really the third step, after testing and diet and lifestyle changes. Remember that supplement regimens need to be customized to your needs - so while the ideas here are a great place to start, they can’t replace working one-on-one with a trained practitioner.
With my own patients, I use the results of their lab testing and the lifestyle changes to create custom, one-of-a-kind supplement protocols, with their specific type of PCOS and symptoms in mind.
One last thing, more isn’t always better. While all of these supplements have benefits, I usually use no more than 3-5 at any given time.
Here are some of my go-to supplements:
Magnesium
Magnesium is an essential cofactor for thousands of processes in the body and is especially key for insulin sensitivity. Research has shown people with Type 2 diabetes (which is common with PCOS) may excrete higher-than-normal amounts of magnesium in their urine, and that magnesium deficiency may be associated with the development of insulin resistance - which is another key component of PCOS.
In addition, magnesium absorption is interfered with by birth control pills, which many women with PCOS have taken or are taking for long periods of time. A good place to start is with this magnesium, 300 mg, twice daily.
Pre and Probiotics
Pre and probiotics promote “good” flora in the gut - prebiotics by acting as food for the gut bacteria, and probiotics by introducing new, beneficial strains. This leads to a greater production of anti-inflammatory Short Chain Fatty Acids (SFCAs), which are a byproduct of bacterial fermentation. SFCAs help improve tight junction function, reducing LPS passing into the bloodstream, which can overstimulate the immune system.
In an animal study, those with PCOS even showed reversal of PCOS with a microbiome transplant and lactobacillus (a type of beneficial bacteria). In another study, supplementing with probiotics and the mineral selenium reduced excess androgen levels and improved hirsutism.
My recommended probiotic is MegaSporeBiotic. Be sure to eat plenty of fruits and veggies for pre-biotic plant fibers, or add a prebiotic supplement like MegaPreBiotic.
Zinc
The mineral zinc has been shown to improve ovarian function, lower androgens, raise progesterone, and promote ovulation. My recommended brand is Designs for Health and the recommended dose is 30 mg daily.
Vitex
Vitex is an indirectly progesteronic herb that has been found in some research to benefit PCOS. Vitex can decrease prolactin by stimulating dopamine. Prolactin is often elevated in women with PCOS, and elevated prolactin promotes higher androgen levels.
While clinically, vitex seems to help many women with PCOS (including me), in theory, it could make PCOS worse. This is because vitex may stimulate LH, and in women with PCOS, LH levels are already too high. However, it is a game-changer for many women with PCOS. If you decide to try it, keep a close eye on your symptoms for signs of improvement or backslide. Especially consider it if you’ve been diagnosed with elevated levels of prolactin.
This product is my favorite blend with clinically meaningful levels of Vitex.
Inositol
Inositol is a plant compound (often thought of as one of the B-vitamins, but technically a sugar) that has been proven beneficial in those with PCOS. One potential mechanism could be that inositol contains the phosphoglycan that helps mediate insulin, and this phosphoglycan is often deficient in people with PCOS.
Research has shown inositol:
- Improves insulin sensitivity
- Improves ovulatory function
- Decreases serum androgens
- Decreases elevated blood pressure
- Decreases elevated plasma triglycerides
- Improves oocyte quality in women with PCOS
There are several forms of inositol: most commonly myo-inositol and d-chiro inositol. Both forms were shown effective in improving ovarian function and metabolism in patients with PCOS, although myo-inositol showed the most marked effect on the metabolic profile (i.e. insulin resistance), whereas d-chiro-inositol was better able to reduce hyperandrogenism. Myo-inositol may also protect against gestational diabetes in women with PCOS.
Most commonly, myo-inositol and d-chiro inositol are used in combination, as there is evidence they balance each other and provide the most benefits together. A standard dose is 4 grams daily. This is my recommended brand.
Licorice & Peony
Licorice and peony are often used together in traditional chinese medicine formulas, such as Shao Yao Gan Cao Tang. Research has shown they block the production of testosterone and promote aromatization, which converts testosterone to estrogen. Licorice in particular can help lower testosterone and block androgen receptors. They may also improve low progesterone, and modulate estrogen and prolactin.
N-Acetyl-Cysteine
N-Acetyl Cysteine (NAC) is a powerful antioxidant that works to reduce inflammation and oxidative stress in the body, both of which may be higher in women with PCOS. NAC promotes antioxidant activity by increasing the production of glutathione, which studies have shown women with PCOS have 50% less of than normal.
NAC can help lower testosterone and improve insulin resistance. One study even showed NAC was more effective at reducing insulin than the drug Metformin (more on this to come).
For women with PCOS looking to become pregnant, NAC may be especially important. Women with PCOS who took NAC were 3.5 times more likely to become pregnant, had a greater likelihood of a live birth, and reduced risk of preterm delivery.
In women using the drug Clomid to promote fertility, adding NAC improved ovulation rate, cervical mucus, mature follicles, endometrial thickness, follicular E2 levels, and luteal progesterone levels.
My recommended brand is Designs for Health, 900 mg, 3 times daily.
Berberine
Berberine is an herb that can benefit women with PCOS in many ways. First, berberine can improve insulin resistance in theca cells. It has been shown to be particularly effective against obesity and visceral adipose tissues (hormonally active fat). It also improved ovulation and increased fertility. Berberine was shown to reduce testosterone and improve LH:FSH rations compared to placebo.
Berberine may also benefit the gut microbiome of women with PCOS by increasing production of Short Chain Fatty Acids (SFCAS - for more on this, see Pre and Probiotics, above).
I like this brand of berberine.
Reishi
The mushroom reishi blocks 5-alpha reductase, which is the enzyme that converts testosterone into its stronger metabolite, DHT. This can help reduce overall androgen excess in women with PCOS. Reishi is also beneficial for the hypothalamic-pituitary-adrenal axis, as well.
My favorite reishi supplement is Mushroom Science Reishi, dose is 2 capsules, twice daily.
Gymnema
Gymnema is an herb that has insulin-modulating activity in those with PCOS, and can reduce elevated triglycerides, which are often also associated with PCOS.
**Important-- Gymnema is not for use during pregnancy or lactation.
Chromium
Chromium picolinate is an essential trace element that is particularly beneficial for insulin-resistant types of PCOS. Research has shown chromium had effects comparable with the drug metformin on ovulation and pregnancy rates, and was better tolerated.
I recommend Thorne Chromium Picolinate, 1000 mcg a day.
Saw Palmetto
Saw palmetto is an herb that can block prolactin receptors on ovarian cells, helping to reduce excess androgens.
Designs for Health Prostate Supreme 2 capsules twice daily.
Bioidentical Progesterone
Using bioidentical progesterone can lower androgens and LH, leading to less ovarian testosterone production. It also blocks 5-alpha reductase, the metabolite that converts testosterone into the more potent DHT, which is often elevated in PCOS. Bioidentical progesterone also slows the and GnRH pulses that are too rapid in people with PCOS, helping to treat the actual root of PCOS.
This is one of my top choices for every woman with PCOS - but be sure to work with a practitioner on this one, as bioidentical progesterone requires specific dosing to be effective and safe.
One thing to note is that adding bioidentical progesterone is not the same as starting a hormonal contraceptive (birth control pills). Birth control pills do not contain bioidentical progesterone - instead they contain artificial progestins, which actually behave more like testosterone in the body.
PCOS Is Complicated, But There Is Hope!
As you can tell by the length of this article, PCOS is incredibly complex. (And I could have written so much more!)
But if you take away only one thing, I hope it’s this: there is hope for effectively treating PCOS.
You don’t just have to suffer through and try to cover up the symptoms. With the right care, you can find and address the root cause.
If you’re ready to start treating your PCOS from the root cause on up, I’d be honored to help guide you there. Having struggled with PCOS myself, helping other women with the condition isn't just my job. It is my passion!
Just click here to book a FREE, no-obligation 15-minute consultation with my team. We use these short calls to get to know you, your health concerns, and see if working together would be a good fit. Think of it like a first date.
Brie
PS - Overwhelmed with all the info on PCOS? I know how that feels, and I’d love to help you find a customized plan (diet, lifestyle, supplements) to help manage PCOS and achieve your health goals. Book a free consultation here so we can chat about a plan for you. (No obligation!)
Dealing with Postpartum Hair Loss
I’ll never forget the moment after my daughter was born…
She was finally fed and content in her dad’s arms, so I snuck away for a shower…
And as I massaged my shampoo, enjoying a moment of peace…
I pulled my hands away to find a hamster-sized clump of hair in my hands!
Any postpartum mama knows what I’m talking about. Postpartum hair loss is no joke!
I knew that hair loss was a normal part of the postpartum period, but even with my super-thick and curly hair, the loss was really noticeable.
And at a time when women are often already feeling more fragile and vulnerable than usual, the sudden hair loss can be like adding insult to injury.
But is there anything we can do about it?
Let’s talk about it today.
What Causes Postpartum Hair Loss?
During pregnancy, estrogen levels are high. This prolongs the hair growth phase, leading to less normal hair loss and longer, thicker feeling hair.
But after pregnancy, estrogen levels drop really dramatically - from 5--100x the normal level during pregnancy to less than normal in breastfeeding. With estrogen suddenly so low, control of the hair follicles goes to testosterone, and specifically, a derivative of testosterone called DHT. With DHT in control, the hair growth phase shortens, and the result is significant hair loss.
In addition, the hormone prolactin plays a role as well. Prolactin is the hormone that rises to induce lactation after birth. But, prolactin also further suppresses estrogen and increases the expression of testosterone and DHT. More DHT expression may result in more hair loss.
And if you already have experienced androgen-driven hair loss, like that caused by Polycystic Ovarian Syndrome (PCOS), you may be even MORE sensitive to this shift after pregnancy.
I think of the postpartum period as a mini version of what can happen during menopause - that’s how big the hormonal shifts are. Women can become androgen-dominant in the postpartum period, causing hair loss and symptoms like vaginal dryness, low libido, and even vaginal atrophy—all of which can make sex less pleasurable or even downright painful. (If you’re wondering just how long your sex drive will be MIA for, it’s totally normal and common for it to be gone until you stop breastfeeding!)
Lactation-Safe Postpartum Hair Loss Solutions
First, remember that postpartum hair loss is 100% normal. And I pinky-promise, it is way more noticeable to you than to anyone else. I say this having gone through it recently myself!
But if trying to disguise it using ponytails isn’t enough, there are some evidence-based things you can try.
There are plenty of herbs that can help block DHT, and many of them can be safely used during lactation, without impacting milk supply.
However, not all DHT blocking herbs can be safely used during lactation: one to avoid until you’ve weaned your baby is saw palmetto. Saw palmetto is reported to block the response of prostate cells to prolactin, which are likely also upregulated by high prolactin in breastfeeding. It can work well for any remaining hair loss concerns after breastfeeding, but skip it until you’re done breastfeeding.
Now, let’s talk about the herbs that are safe in lactation!
- Stinging nettle
- Gingko
- 1-3 cups of green tea daily
In addition to these, there are a few more that deserve special mention.
#1 Fenugreek
In addition to blocking DHT, fenugreek also supports milk supply in some women. It may be especially helpful if you also experience any insulin resistance, such as that in PCOS. Those with PCOS often have high DHT and greater hair loss.
#2 Nigella Sativa (Black Seed)
This herb has been taken for centuries as a therapeutic medicine and for maintaining health, and animal studies show it also has the potential to block DHT. For mothers who are breastfeeding, black seed has been known to boost the breast refill rate. I especially recommend this to moms who have a low breastmilk supply issue due to insulin resistance.
#3 Reishi Mushroom
In a research study exploring the anti-androgenic effects of 20 species of mushrooms, reishi mushrooms had the strongest action in inhibiting testosterone. That same study found that reishi mushrooms significantly reduced levels of 5-alpha reductase, preventing conversion of testosterone into the more potent DHT. In addition, reishi has an extremely low toxicity profile and is a good adaptogen and immune support in new moms. This is another go-to for my PCOS patients.
Bioidentical Progesterone for Postpartum Hair Loss
Another treatment option during lactation is adding cyclical bioidentical progesterone. Biodientical progesterone helps because progesterone reduces 5-alpha reductase activity, which converts testosterone to its active metabolite dihydrotestosterone (DHT).
And if you’re wondering, is that safe? It is indeed. Think about it this way: many women get pregnant with their second (or third….or…. fourth) while still breastfeeding an infant. When we are pregnant, progesterone skyrockets, going up by a factor of ten. This shift - which is known to be safe - is much, much more dramatic than the increase in progesterone from adding cyclical bioidentical progesterone therapeutically. Some progesterone will pass into breast milk, but, again, it’s much lower than what would pass through milk if a woman were pregnant.
And, cyclical bioidentical progesterone is an FDA-approved treatment for postpartum depression. That’s why I often use it with breastfeeding moms, even when hair loss is not a top concern. It can help normalize the menstrual cycle after baby, improving mood and PMS-symptoms.
Nutrient Support for Postpartum Hair Loss
But before herbs or cyclical bioidentical progesterone, I like to start all women with simple nutrient support.
First up, make sure you’re still taking a great prenatal vitamin. Nutrient needs while breastfeeding are even higher than when pregnant. This Is Needed and Designs For Health are my two favorites.
Next, I recommend getting iron and vitamin D levels checked with a quick blood test. Low levels of vitamin D drive hair loss, and supplementing is so easy if needed. Optimal vitamin D levels are between 50 and 80 ng/mL.
Low iron is also really common postpartum, and low iron is associated with increased rate of hair shedding. Blood loss = iron loss, and childbirth often involves a significant amount of blood loss. Anemia is also very common in pregnancy, and not everyone has iron stores that just bounce back. If a serum ferritin level shows your iron levels are low (anything below 30, but optimal is above 50 and within range), supplement with a high-quality supplement. This is my recommended iron supplement.
Finally, don’t forget minerals! Your body will prioritize providing minerals in your breastmilk over meeting your own body’s needs. That means baby might be stealing all our minerals, through no fault of their own!
#1 Zinc is essential for supporting hair and skin health, plus zinc acts as a DHT blocker by reducing 5-Alpha-reductase. Zinc levels can easily get low in pregnancy and postpartum. If you’re going to supplement with more than what is included in your prenatal, I recommend testing along with copper. If taking zinc, you’ll also need to take copper to keep the two from becoming imbalanced. Serum Zinc should be 64-126, and copper should be 81-157, and the ratio between zinc/copper should be between .85-1.2. I use this product the most, in clinic.
#2 Magnesium is something every nursing or postpartum mama should be on. I suggest 300 mg per day minimum, but some women need more. This one is great!
#3 Copper and Selenium are also important, but should be part of any postpartum vitamin worth it’s merit. Check your prenatal and be sure these are included.
Hang In There, Mama!
Becoming a new mom is tough for so many reasons. I hope this information can help ease that transition a bit.
And if you’re looking for more natural but no-nonsense, judgement-free support from another woman who has been there - look no further! Whether you’re looking for support with hormone issues, fertility, or postpartum life, myself and my team of clinicians would be honored to help.
>>> Click here to book a no-obligation free consult at a time that works for you
- Brie
PS - Struggling with wild hormones, the baby blues, milk supply, or anything else postpartum? Yes, hormone shifts are a normal part of the postpartum period… but NO they do not have to make you miserable. Let me help.
Healing HPV with Functional Medicine Part 2
In Part 1 of this series, I explained the western vs. functional medicine approach to HPV. Read Part 1 here.
Even though HPV is a very common infection, treating it requires a completely individualized approach.
Quick recap: For the vast majority of people, the immune system is able to clear HPV on it’s own.
For the people who get HPV and can’t clear it, there can be numerous factors at play. As your functional medicine practitioner, my job is to not only identify these factors, but help you implement an affordable, manageable plan to address them.
In real life, I break this into two steps. Let’s look at them both.
Step 1: The Foundation
It sounds too simple… but for the majority of people who struggle with HPV, it is changing the basics that makes the biggest impact.
Getting good sleep - 7-9 hours per night, in a dark room, with the same sleep and wake time on average every day.
Healthy diet - removing foods that are troublesome for you, increasing whole foods, decreasing processed and inflammatory foods.
Exercise you enjoy - adding in exercise if you’re sedentary, and cutting back if you’re overdoing it at the gym, since over-exercise can suppress immune function.
Stress management - this varies person to person. It can be as simple as adding a meditation practice or as life-changing as quitting your job or moving.
Finding happiness and joy - not just reducing stress, but actively adding in things that you love and fill you with joy.
Spending time outside - camping, hiking, even a walk in the park. It’s all about re-connecting with nature.
Many people find that just making these changes not only ramps up their immune function (helping them clear HPV) but that it transforms their entire life.
To give proper attention to how important this step of the healing process is, I’ve teamed up with 2 health coaches who specialize in helping people make enjoyable, sustainable lifestyle changes for better health.
>>> Learn more about our health coaches here
Step 2: Specific Immune Support
Step 2 is the part where my specialty comes in - creating customized supplement protocols. While every client’s treatment plan is unique, here are some of my go-tos for HPV treatment:
Green Tea - Epigallocatechin gallate, a compound in green tea, has been evaluated on the cells of the cervix and has been shown to inhibit HPV and induce cell death of abnormal cells. In a case study of patients with CIN-2, those treated with green tea had a greater response than those given other treatments.
Coriolus versicolor - Also known as turkey tail, research has shown that in women with abnormal pap smear results, using a vaginal cream containing this mushroom led to significantly higher numbers of normal pap smears 3 and 6 months later.
Indole-3-carbinol - This substance is found in cruciferous veggies. A case study looked at the effects of indole-3-carbinol on high-grade lesions. Subjects were given 400mg of indole-3-carbinol per day. None of the placebo group showed complete regression, but 4 of the 9 who took the indole-3-carbinol showed complete regression after 12 weeks.
Beta glucan - This well-known immune modulator has been shown to have anti-cervical cancer properties.
In addition to these supplements, I like to use green tea, curcumin, probiotic and vitamin E suppositories. I also use a Chinese herbal liquid extract based on formula used in women’s gynecology for thousands of years, “Yin Care,” applied as a vaginal rinse in the morning.
Finally, I find that there is almost always a lack of adequate folate in my clients with HPV concerns. This can be due to poor absorption, a lack of folate in the diet, folate-depleting medications (commonly the birth control pill), or genetic SNPs that make keeping an adequate folate status more difficult. Rather than just prescribe a folate supplement, I recommend testing first. Not everyone needs more folate, and there is such a thing as overmethylation.
Case Study: A Real Life HPV Success Story
Now that you know what my treatment basics are, let’s look at how this works in real life. I want to tell you about a patient of mine who recently cleared her HPV and reversed her abnormal cells.
My client went in for a routine pap smear only to be told her results were abnormal and she was positive for HPV. A follow-up colposcopy showed she had CIN-1 and CIN-2-3 cells.
Her doctor recommended a LEEP, but my client was hesitant due to the potential side effects. Instead, she decided to turn to me. We had already had great results working together on her adrenal function, chronic Epstein-Barr virus, and food sensitivities.
Because she had already addressed the majority of foundations discussed above, the only lifestyle change we made was eliminating sugar. From there, we went straight into step 2, treating her immune system and the infection systemically.
We started with a 60-day customized plan that included:
- Coriolus extract
- DIM
- Methyl-b-complex
- Vitamin A
- Vitamin D
- Antiviral herbs (both western and Chinese)
- Green tea suppositories
- Probiotics both orally and vaginally
After 60 days on this protocol, she went for a repeat colposcopy… and the abnormal cells were gone! This was a huge success.
There were still signs of cervicitis (inflammation of cervix), but with reparative change, meaning things were getting better.
But even with these good results, her doctor still recommended a LEEP. We didn’t let that deter us, though, and continued with the 2nd phase of treatment. We added:
- High dose vitamin C
- Zinc
- Switched up the antiviral herbs
- Added the Chinese herbal formula Xiao Fu Zhu Yu Tang which has been shown to reduce cervicitis
- Added curcumin extract caps vaginally and Vitamin E suppositories
- Added a Chinese herbal liquid extract as a vaginal rinse, based on the “Yin Care” formula used in women’s gynecology for thousands of years
After 6 weeks on this protocol, she then had a repeat pap smear and… (drum roll please….)
She was negative for all dysplasia and negative for HPV!
We then moved into the final phase of her treatment: ongoing antiviral support and new suppositories to focus on repairing any remaining cervicitis: calendula, vitamin E, vitamin A, and DHEA.
Become An HPV Success Story Yourself
This client’s experience isn’t an unusual one - with the right support, it is to be expected that your body can heal HPV and the abnormal cells it causes long before it ever progresses to cancer.
If you’re dealing with HPV or abnormal cells, I’d love to chat with you about a customized protocol that could help you have similarly fantastic results.
The first step is to book a free intro call with my team. These calls are totally free and no-obligation. It’s like a first coffee date: low stakes, but it could lead to something amazing!
If you like what you hear, we’ll help you build a customized treatment plan tailored to your needs, lifestyle, and budget.
>>> Book a free intro call here
PS - Already had a LEEP? Just found out you have HPV? Wherever you are on the journey - and no matter what treatment choices you’ve already made - I would be honored to help you find the path forward toward healing. Book a free call to learn how.
Addressing HPV with Functional Medicine Part 1
HPV is a scary diagnosis… you can’t see it, you probably can’t feel it… and suddenly you’re hearing the big “C” word: Cancer.
It’s overwhelming and scary… and sadly, many western practitioners don’t do much reassuring, explaining, or even provide all the options for treatment and management.
And they definitely don’t want to talk about natural treatments for HPV…
But the truth is that you DO have options when it comes to treating HPV and the abnormal cells it can cause.
Today, I’m writing for anyone facing an HPV diagnosis. I know it is frightening and overwhelming - and I want to help. Let's talk about HPV, and I'll share a case study of one of my real-life patients who took a more natural route to treating HPV, with amazing results.
What Is HPV?
HPV stands for human papillomavirus. HPV is the most common sexually transmitted infection.
In 2018 alone, the CDC reported 43 million HPV infections. The bottom line is that most sexually active people have HPV at some point in their life.
Why is HPV so common?
Unlike other STIs, HPV can be spread even without any symptoms. In general, men are not routinely screened and have no symptoms, so they are often unknowingly spreading it. And, like men, women with HPV often have no outward symptoms. Because symptoms aren’t noticeable, it could be years after you contract HPV that you find out you have it during a routine pap smear or STI test. That makes tracking back to where you got it, and who you might have spread it to, nearly impossible.
But the most important thing to know about HPV is that in the vast majority of cases it is no big deal. Most people contract HPV and clear the virus on their own. Think of getting over a cold: your immune system does the work and takes care of it.
But for the people who aren’t able to clear HPV on their own, it can cause problems. That’s what we’re going to discuss today.
When HPV Doesn’t Resolve On Its Own
When HPV doesn’t resolve on its own, it can cause the development of abnormal cells on the cervix that can eventually lead to cervical cancer.
HPV doesn’t typically cause noticeable symptoms, and this is one of the reasons women need routine pap smears. We can’t see or feel the start of cervical cancer without an exam, but if caught early and addressed, it can be stopped before it evolves into full-blown cancer.
Even if you’re working with an alternative practitioner, don’t skip your GYN exam. It’s really important.
Pap Smear
So you did it, you went in for your pap smear or gynecological exam… only to get bad news: either your pap smear or your HPV test was abnormal.
Depending on your doctor, you might have been tested for HPV and gotten a positive result, and then come back for a pap smear… or your doctor might have started with a pap smear, and found abnormal cells on your cervix - also called cervical dysplasia.
Once cervical dysplasia has been found, the next step is usually a procedure called a colposcopy. This procedure takes tiny biopsies of the cervix for a closer look (compared to just scraping the top layer of the cervix in a pap smear).
The colposcopy shows what level of abnormal cells you have: low, moderate, or high, called CIN-1, CIN-2, or CIN-3.
In most cases, if your results show just CIN-1 or 2, your doctor will recommend a “watch and wait” approach. The hope is that your body will fight off the HPV and reverse the abnormal cells on its own.
If you have CIN-3 or CIN-2-3 (which means it's unclear if cells are CIN-2 or CIN-3), the next step is typically a loop electrosurgical excision procedure, better known as a LEEP. The LEEP takes a larger biopsy piece to get a better diagnosis and hopefully removes all the abnormal cells, too.
Doctors also often hope that as the body heals the cervix after the LEEP procedure, it will also recognize the HPV virus and fight it off.
After the LEEP procedure, you’ll follow up with another pap smear, with the hope that the abnormal cells are gone. You can also expect more frequent pap smears over the next few years.
If your follow-up pap smear isn’t clear, the next step could be another LEEP… or even a hysterectomy, depending on the circumstances.
What Western Medicine Gets Right (And Sometimes Wrong)
As a functional medicine practitioner, what I like about the western medicine approach is that it involves being proactive.
But here’s what I find frustrating…
It is estimated that only 5% of CIN-2 and 12% of CIN-3 cervical dysplasia cases will progress to invasive cancer if untreated.
And, in general, it takes 10 to 20 years for abnormal cells to progress to cancer, and that progression requires persistent HPV infection to occur.
That means that even if you have abnormal cells, you have a LOT of time to address it before cancer becomes a serious concern.
Secondly, the LEEP procedure is not without risk. While some have only minor bleeding and no other side effects, all of the following have been reported after one or more LEEP procedures:
- Miscarriages - Per one study from 2015, in 116 women studied, an 18% increased risk of miscarriage was reported among those previously treated with LEEP. A different study cited a positive association with second trimester miscarriage.
- Depression
- Cervical stenosis - narrowing of the cervix, which can make getting pregnant difficult or cause problems with passage of fluids like menstrual blood.
- Chronic pelvic pain
- Pain during sex
- Inability to orgasm, low libido, loss of sensation in vagina, cervix, or clitoris
- PTSD - a form of sexual trauma experienced that stays traumatizing when thinking or talking about the procedure.
And while there is a *hope* that the LEEP procedure will help your body identify and fight the HPV as a side effect… western treatment does nothing to address the root cause of the abnormal cells: the HPV infection!
And that’s where the functional medicine approach really shines.
The Functional Medicine Approach to HPV Treatment
No matter what stage of HPV you’re dealing with - from just a positive test result to CIN-3 cells - the very first step should be taking proactive steps to support your immune system in fighting HPV itself.
Remember that most people are able to clear the HPV virus without intervention. If you’re not, here are the red flags I look for:
- Low nutrient status
- Poor sleep
- Stress or poor stress management
- Genetic predisposition
- Other chronic infections
Together, all these factors can lead to low immune expression and a susceptibility to chronic viral infections of all types.
But the good news is that the majority of these factors are modifiable.
That means, with the right support, you might be able to shift from someone who isn’t able to clear HPV on your own, to someone who is.
And on top of this, we can also use antiviral protocols to give your body a leg up in fighting the infection.
A healthy immune system should be able to handle HPV all on its own - so the approach that makes the most sense is to treat your immune system, and then let your body get rid of the HPV and heal the abnormal cells.
No matter where you are in the process - from just finding out to having already completed one or more LEEPs - this approach can help.
In Part 2 of this post, I’ll share my HPV treatment plan and a case study of one of my real patients who reversed abnormal cells and HPV using this approach. Read Part 2 here.
- Brie
PS - ready for help with HPV? You don’t have to wait for Part 2. Book a free intro consultation with my team today to get started on your customized treatment plan. Book your intro call here.
The Real Cause of Premature Aging and Dull Skin
I’m not afraid to admit... I'm obsessed with good skin. After my work is done for the day and my daughter is asleep, going through my skin care ritual is how I wind down and relax.
And I know I'm not the only one… Skin care sales have skyrocketed in the last year.
But the truth is that there is a lot more to beautiful skin than expensive creams (or even an acupuncture facial… which I love).
Good skin starts inside… and if you’re having skin issues like dryness, sagging and premature aging… as a practitioner, that puts up major red flags. Today, I want to explore the internal causes of common skin issues.
Good Skin Starts Within
You’ve heard this before I’m sure, but in our current skin-care obsessed world, it bears repeating: the foundation of beautiful, radiant skin is your internal health and well-being.
Your skin care regimen can help, but if something is amiss internally, you’re going to see it on your skin and no amount of products can fix it.
There's actually a lot of good info on the internal link to acne. It seems like there is finally (!) some acceptance and understanding that acne is an internal issue, and usually related to hormones. (More on that here.)
But what most people don't know is that issues like premature aging, wrinkles, sagging skin, dryness, fine lines, discoloration etc… They all have an internal cause, too.
You’re not just getting old or overdue for a facial… there are real issues that could be causing these symptoms, and one of them is thyroid issues.
The Thyroid-Skin Connection
The thyroid is a butterfly-shaped gland at the base of the neck that produces key hormones for the healthy functioning of the body: triiodothyronine (T3) and thyroxine (T4).
Women are 8x more likely than men to develop a thyroid issue… and a key symptom of thyroid issues is changes in skin.
Thyroid dysfunction may present on the skin as:
- Dryness and dullness
- Rashes
- Premature aging (sagging, wrinkles, fine lines, loss of elasticity)
- Cyclical acne
- Facial puffiness
- Slow healing
- Hyperpigmentation
That’s because the hormones produced by the thyroid are responsible for growth, energy, and repair of cells of the body.
On top of these skin issues, thyroid dysfunction has tons of other subtle symptoms that you may have no idea are connected, like:
- Feeling cold, or having cold hands/feet
- Hair loss
- Sudden weight loss OR weight loss resistance
- Fatigue
- Constipation
- Trouble sleeping
- And more
How Your Thyroid Messes With Your Skin
Thyroid dysfunction can either present as an overproduction of thyroid hormones or an underproduction.
Hyperthyroidism is an overproduction of thyroid hormones and is less common. It is caused by the autoimmune condition Graves’ disease, in which the body attacks the thyroid gland. Symptoms include weight loss, sensitivity to heat, and higher heart rate. In the skin, hyperthyroidism can cause:
- Hyperpigmentation, like melasma, which is darkened patches of skin. This is caused by increased pituitary ACTH in compensation for cortisol being degraded and processed at an upregulated rate.
Hypothyroidism is the underproduction of thyroid hormones, and it is more common than hyperthyroidism. It can have many causes, including autoimmunity, which causes Hashimoto’s. Symptoms include weight gain, cold sensitivity, constipation, hair loss, fatigue, and these skin symptoms:
- Slow cell turnover: if your thyroid hormone levels are low, you will have a lower rate of repair of cells all over your body - but it is especially noticeable in the skin cells, which should have a fast turnover rate. This might present as skin taking longer to heal, dullness (as the old layer of skin hangs out too long), or dry and flaky skin
- Increased wrinkles and sagging: In those with hypothyroidism, a decrease was observed in type-IV collagen and hydroxyproline during the proliferative phase of wound healing. But collagen isn’t just for wound healing - it’s also what stops aging and sagging skin.
- Puffiness: less thyroid hormones cause increased polysaccharides, which causes more water to be held in the skin, and also lowers mitochondrial respiration efficiency, causing poor blood circulation. All this = puffiness.
- Hyperpigmentation: the exact mechanism isn’t well understood, but hyperpigmentation (dark marks and melasma) is also associated with hypothyroidism, probably due to reduced blood flow and slower cell turnover.
In addition to these, conditions like vitiligo and alopecia are also warning signs that the thyroid may be struggling.
Save Your Skin!
If any of what I just described sounds like it could be affecting you… here’s what to do next:
Step 1: Get Your Thyroid Tested
A specialized practitioner like myself or your general doc can order blood work to check for thyroid issues. But be sure to get a FULL thyroid panel: many docs only test T3 or T4, and exclude TSH (thyroid stimulating hormone).
I also recommend cortisol testing. Cortisol is the “stress hormone”and it is closely linked to thyroid function.
If you have mild thyroid dysfunction, just making some key lifestyle changes may be all you need.
For more severe thyroid issues, I highly recommend working with a trained practitioner (book a free consult with my team here.) Treating thyroid issues is multifaceted, and you likely don’t need to be on thyroid meds the rest of your life.
At-Home Ways To Support a Healthy Thyroid
- Switch to natural products, many of the chemicals - PCBs, Phthalates, BPA, flame retardants and more - used in conventional beauty and home products can actually harm thyroid health. Switch them out for natural alternatives. (There are so many great, clean skin care brands now!)
- Remove processed foods both to lower your toxin exposure and to give your body the nutrients it needs for healing
- Prioritize good sleep
- Detox if needed - especially consider your exposure to heavy metals, mold, parasites, and chemicals. Some of my favorite detox-supporters are saunas!
- Exercise to promote healthy cortisol levels
- Find healthy stress outlets
- Try ashwagandha - this herb can help manage cortisol levels
And if you have any signs of autoimmune-related thyroid issues, like Graves’s disease, or a coexisting condition like rosacea, alopecia, vitiligo, or eczema - you might need more specialized support and guidance. Consider booking a free consult with my team here.
Thyroid Tests Normal?
Thyroid issues are one potential cause of premature aging and other skin issues, but they aren’t the only potential underlying cause. If your thyroid function is normal, here are some other potential causes I would want to investigate:
- Leaky gut
- Oxidative stress
- Toxicity
- Genetic (but don’t worry -this doesn’t mean you’re doomed, just what you need to work with your genetic predispositions)
- Poor nutrition and lifestyle habits
And you might have several of these factors happening at the same time - that’s when working with an experienced practitioner who can tease it all apart and help you manage each piece becomes so valuable.
Get Help With Your Skin Health
If you’ve tried all the serums and moisturizers… and you’re still not happy with the way your skin looks, it might be time to dig a little deeper.
My practice specializes in working with women with gut, hormone, and fertility issues, and we’d love to support you, too!
>>>> Click here to schedule a no-obligation, free consult
How To Know If You Have Hydrogen Sulfide SIBO - aka “Hidden SIBO”
Identifying and diagnosing SIBO (Small Intestine Bacterial Overgrowth) is tricky.
When it was first discovered, doctors thought SIBO was a rare disease…but now we know it’s actually incredibly common, with as much of 80% of people diagnosed with IBS (Irritable Bowel Syndrome) actually having SIBO.
But even with the knowledge that SIBO is actually super common, problems with reliable testing for SIBO mean it is STILL underdiagnosed.
But don’t worry - I’m not just here to complain. I have good news:
A new breath test for SIBO is now available that identifies all 3 main types of SIBO!
If you have “mystery” gut symptoms — and even if you’ve been tested for SIBO in the past and gotten a negative result — this information is very important for you!
The 3 Types of SIBO
SIBO is a condition where bacteria overgrow in the small intestine — as the name implies. The overgrown bacteria eat undigested food in the small intestine and produce gas as a by-product.
Different types of overgrown bacteria produce different types of gas: either methane, hydrogen, or hydrogen sulfide.
It’s the gas produced by the bacteria that causes SIBO’s hallmark symptoms: bloating and constipation or diarrhea.
Many practitioners classify SIBO into one of 3 types based on the type of gas:
Hydrogen SIBO - is associated with diarrhea
Methane SIBO - now also called “Intestinal Methanogen Overgrowth” or IMO, is associated methane SIBO symptoms of constipation
Hydrogen Sulfide SIBO - is the least well-understood and associated with diarrhea, but can also be present with constipation
Making it even more tricky, people can have more than one type of gas present, causing a mix of symptoms.
What Does Hydrogen Sulfide SIBO Feel Like?
People with Hydrogen Sulfide SIBO typically have some or all of the traditional SIBO symptoms:
- Bloating
- Gas
- Diarrhea
- Constipation
- Abdominal pain or discomfort
But I also look for these tell-tale signs of hydrogen sulfide:
- Bladder pain, frequency, or urgency
- Body or muscle pain
- Tingling or numbness in the hands and feed
- Sensitivity to noise and/or light
- Histamine sensitivity
- Sulfur-smelling gas (like rotten eggs)
- Whole body pain and overall feeling of unwellness
- Sulfur intolerance
Sulfur intolerance may be a condition you’re not familiar with. It’s symptoms are very similar to histamine intolerance: asthma, shortness of breath, hives/itchy skin, headaches, nausea, diarrhea, flushing, high or low blood pressure, brain fog, chronic stress (via elevation of cortisol and glutamate) and fatigue.
Sulfur is necessary to repair cells and carry out detox, but some people struggle with it for two reasons:
- Genetic mutations (like CBS or SOUX) that make it hard for them to process
- An abundance of sulfur-producing bacteria (like in hydrogen sulfide SIBO)
And some people have BOTH.
If you have a sulfur intolerance, you might find that high-sulfur foods — like kale, eggs, red meat, and garlic — make you feel worse, as do Epsom salt baths.
And if you’re a SIBO “tough case” or have chronic digestive issues, that’s another red flag for hydrogen sulfide SIBO.
Any of these signs are a great hint…but there’s only one way to know for sure. Let’s talk about that now.
How Do I Know Which Type of SIBO I Have?
The only way to know what type of SIBO you have is with a special test called a “breath test.”
To have a breath test, you’ll follow a special diet for 24 hours, then fast overnight. Then you’ll drink a sugar solution (made of either glucose or lactulose), and breath into a special collection device.
The idea is that the overgrown bacteria in your small intestine consume the sugar solution, ferment it, and produce gas. That gas can be measured in your breath sample. A practitioner trained in SIBO can interpret test results and prescribe treatment based on your gas type and level.
But the catch is that until now, only levels of hydrogen and methane could be detected in a breath sample.
That left many people who had the clinical symptoms of SIBO scratching their heads when their test results came back negative!
How could they have all the symptoms, but none of the methane or hydrogen gas? In many cases, the answer is hydrogen sulfide SIBO.
Hidden SIBO: Hydrogen Sulfide
Smart SIBO practitioners have found workarounds to help identify hydrogen sulfide SIBO even without a proper test - specifically looking for a test result pattern called a “flat line.”
But a flat line test result can only suggest hydrogen sulfide — not confirm it. Even more complicated, hydrogen sulfide may just be one of the gases present, and can explain why treatment for hydrogen or methane SIBO falls short of resolving all symptoms.
But all that is changing now!
New technology has created the first breath test for all three gases: hydrogen, methane, and hydrogen sulfide.
It’s called TrioSmart, and I’m really excited to have this as a tool in my kit for patients. While no test is 100% perfect, this can reveal some important information no other test can.
If you are tested and DO have SIBO of any type, we can use your gas levels and types to create a customized treatment plan.
Should I Get A SIBO Test?
Wondering if this new test might be for you?
Here are some of the indicators I look for:
- History of IBS or other “unexplained” digestive symptoms like bloating, constipation, or diarrhea
- History of restless leg syndrome or rosacea (both are commonly associated with SIBO)
- Past SIBO test was negative, but you still have symptoms
But you don’t need to figure this out…that’s MY job.
As your health guide, here’s what I do:
#1 Listen to you - your health history, your concerns, your questions.
#2 Create a customized plan - based on your health needs, your budget, and your schedule. Nothing one-size-fits-all.
#3 Support you along the way - answering questions, tweaking and updating your plan as needed, and anything else you need.
Sounds like what you need? It all starts with a no-cost, no-obligation 15 minute intro call with my team.
>>> Book a Free 15-Minute Consult
- Brie
PS - If you’ve been told you have IBS, and there is no solution, this test could change everything for you. I’d love to walk you through it, help you prep and order it, and most importantly: interpret the results and create a treatment plan! Step 1 is a free consult - book yours today.
What Your Gut Is Trying To Tell You About Your Thyroid (+ Tests That Can Reveal The Truth!)
Everything is connected.
It’s one of my key beliefs in medicine, and when it comes to your gut health and thyroid problems, it holds true.
If you’re struggling with thyroid symptoms OR gut issues, I want to take a look at both… because where we find one, we often find the other! And if you only try to fix one issue, you’ll wind up spinning your wheels, unable to fully heal.
And if you’re facing a thyroid issue, this is ESPECIALLY true.
Today, I want to explain exactly how gut infections and thyroid health are linked - and what you can do to find and address gut infections to achieve better thyroid health.
You - Yes, YOU - Could Have A Gut Infection
No one wants to think they could have any sort of gut infection or parasite. First of all, there is the “ick” factor associated with parasites and infections. Just talking about it might make your skin crawl!
Plus, most people think that gut infections only happen if they are drinking “dirty” water or travelling to far-flung countries.
But that just isn’t true! Even in North America, Europe, and Australia, gut infections happen all the time! Even very clean and careful people can become infected when doing everyday activities - like swimming, gardening, or eating out. If you have pets, kids, like to hike or spend any time outdoors, and eat or drink ANYTHING… you’re at risk of a gut infection.
So don’t panic… we’re exposed to potential pathogens all the time! You can likely think of one you know you’ve had… food poisoning.
Plus, one of the most common infections is actually overgrowth of commensal bacteria or fungi - which just means bacteria that belongs in the gut naturally either overgrows or grows where it doesn’t belong.
That’s why I bring up the topic of gut infections and parasites with all my patients.
Gut Red Flags To Beware Of
If you come to see me as a patient, I look for these warning signs that could indicate some sort of gut infection could be a factor:
- Diarrhea
- Constipation
- Abdominal pain
- Vomiting
- Gas and bloating
- Ulcers
- Weak immune system
- Autoimmunity
- Extreme fatigue
- Nutritional deficiencies
- Brain fog
- Sugar cravings
- Depression
- Anxiety
- Joint pain
- Obesity
- Food intolerances – especially developing new sensitivities
- Skin conditions – such as psoriasis, rosacea, and eczema
Or, any of these conditions, either diagnosed or suspected:
- Intestinal Permeability (leaky gut)
- Chronic and Acute Gastroenteritis
- Inflammatory Bowel Disease (IBD - Crohn’s or ulcerative colitis)
- Irritable Bowel Syndrome (IBS)
- Autoimmune Disease
- Small Intestine Bacterial Overgrowth (SIBO)
And of course, anyone with any type of hormonal issues - but especially thyroid or sex hormones - gets a closer look, since gut infections and hormones are so closely linked.
These Are The Tests I Order...
Have some red flags? It’s time to test!
First up are stool tests. This is where I start for almost all patients.
My personal favorite stool test is the GI Map.
Why do I like it? Compared to a regular stool test, the GI Map uses qPCR (quantitative) Technology, which is a more accurate way to detect and quantify organisms compared to more common culture, regular PCR, microscopy or DNA sequencing. qPCR works by amplifying and detecting DNA and RNA sequences, which is key because for results to be clinically meaningful, you need to know how much DNA is in the stool.
The GI Map test is also reproducible, which means that if you run it twice in a row, you get the same results - this is a key quality to look for in any diagnostic test. It’s used in research settings and it is the first pathogen assay that is FDA approved.
Other tests I like and sometimes use are:
- BiomeFx - this is a newer test that uses Whole Genome Sequencing to analyze over 25 pathogens measures their relative abundance as a percentage of your entire microbiome. This is different from traditional stool tests, which only look for any detectable number of pathogens present. While it isn’t uncommon to have a small number of pathogens present in your microbiome, the relative abundance in proportion to your other bacteria is what’s important.
- GI360 by Doctors Data
If you have constipation, diarrhea, gas, significant bloating or a history of food poisoning, I’ll also ask for a SIBO Breath Test.
If you have candida overgrowth symptoms like a history of antibiotic use, yeast infections, urinary tract infections or interstitial cystitis, chronic itching in groin, fungal toe nails, you’re reactive to yeast in foods, have been diagnosed with methane SIBO, have sugar or carb cravings, or stubborn weight issues, but the stool test doesn’t show candida, I will order Organic Acids, and/or Serum Antibodies to further suggest candida overgrowth treatment would be beneficial for you.
What Your Gut Test Results Can Reveal
Once I’ve got your test results back, the real fun can begin: interpretation and treatment!
But I don’t just glance at your results: I comb through all the details, connecting dots to put together a comprehensive picture of what’s happening with your health.
Here’s a peek at what I’m looking for in your test results:
Inflammation/Immune Markers
-
- Calprotectin - this is key for differentiating between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) (some tests also have lactoferrin). If below 120, it suggests infection, chronic NSAID use, or could be polyps, colorectal cancer or IBD. If above 120, it’s a sign of significant inflammation--which may be caused by an infection, but also generally receives a recommendation for referral to a GI doc if you’re working with me, as it can be suggestive of Celiac, or Inflammatory Bowel Disease such as Chrons’ or Ulcerative Colitis. (Gastroenterologists may suggest colonoscopy to rule these out when calprotectin levels cross a particular threshold). Each lab has a different range and sensitivity for calprotectin, so practitioners should use that lab's range. Should be rechecked at 4-6 weeks or after treatment.
-
- Zonulin - this is a keymarker of leaky gut.
-
- SIgA - this is a marker of gut secretory immunity and barrier function and can show loss of resilience and tolerance. I look at this for signs of chronic infection, immune suppression, and/or adrenal hormone dysfunction.
Digestion and Absorption
-
- Pancreatic Elastase-1 - this marker reflects levels of pancreatic digestive enzymes present. There are many reasons why someone might have sub-optimal digestive enzymes, but regardless of the cause, we will want to supplement with enzymes at least in the short term.
-
- Fecal Fat - this is a marker of fat breakdown and absorption. If really low, it’s a sign a patient is not eating enough fat (<5%). If high, it indicates fat malabsorption/digestion. I’ll want to consider bile flow/production issues, enzyme deficiency, or SIBO.
-
- Short-Chain Fatty Acids and Beta-Glucuronidase - these are functions of the bacteria in the microbiome that reflects if good bacteria are present in adequate numbers or if less desirable bacteria are overpopulated. SCFA are the main fuel for cellular repair of the barrier membrane. High beta-glucuronidase can be a cause of estrogen dominance, and can also signal overall issues with not just the gut, but liver detox, depending on the level.
Microbiome
-
- Commensal bacteria - these are your “good bacteria” - and this also shows which bacteria are in low number, and which are missing altogether
-
- Parasitology - looking for infections like campylobacter, giardia, Blastocystis hominis, entamoeba histolytica, etc are present.
-
- Mycology - this clues me in to what fungi and yeast are present.
-
- Pathogenic bacteria - aka bad bacteria, or bacteria that can be either bad or good (like H Pylori)
-
- Worms - Yes it is gross, but it’s not the end of the world!
What Does All This Have to Do with Your Thyroid?
Let’s bring this all back around to your main concern: your thyroid!
Research has actually linked multiple gut infections to thyroid issues. Here’s a breakdown of some of the most common ones:
Blastocystis hominis
This common gut infection (often called Blasto for short), which is spread via contaminated food or stool, can cause symptoms including bloating, diarrhea, nausea, flatulence, variable bowel habits, abdominal pain, hives, and fatigue. Additionally, this pathogen is notorious for causing multiple food sensitivities.
It’s also linked to Hashimotot’s thyroiditis: people with Hashimoto’s are more likely to develop the skin condition chronic spontaneous urticaria (also known as chronic hives), as well as irritable bowel syndrome (IBS). And a study of 54 people in Egypt with chronic urticaria (hives) revealed that Blastocystis hominis was found in 61 percent of them, while only eight percent of the healthy controls had the parasite, suggesting that Blasto could be linked to hives, IBS, and Hashimoto’s.
Epstein-Barr Virus
Epstein-Barr Virus is a common virus best known for causing the disease mononucleosis.
Research out of Poland supports my informed hunch that it’s also linked to Hashimoto’s. A 2015 study done there found the virus in the thyroid cells of 80 percent of people with Hashimoto’s, while controls did not have the Epstein-Barr virus in their thyroid gland.
Yersinia Enterocolitica
This infection is often caused by consuming undercooked meat or drinking contaminated water. There is some evidence that Y. enterocolitica is associated with autoimmune thyroid disorders including Graves’s disease and Hashimoto’s thyroiditis in genetically susceptible individuals because higher antibodies to Y. enterocolitica are often found in these patients.
Helicobacter Pylori
This ultra-common infection/overgrowth, best known as a cause of ulcers, is also linked to autoimmune thyroid disorders. In a Korean study, those who were positive for H. pylori were significantly more likely to also have anti-thyroid peroxidase antibodies present.
Small Intestine Bacterial or Fungal Overgrowth (SIBO or SIFO)
Both bacterial and fungal overgrowth in the small intestine is linked to hypothyroidism - research has shown as much as 54% of people with hypothyroidism also have SIBO or SIFO.
These overgrowths can also deplete iron, which is involved in thyroid hormone synthesis.
In my own clinical experience, many of those with Hashimoto’s often have a high degree of yeast overgrowth and symptoms to go with it: gas, bloating, brain fog, sinus congestion, GI distress, itchy skin or scalp, eczema, vaginal yeast infections, and intestinal permeability.
Giardia
Giardia is another common parasite most commonly caused by drinking contaminated water. Some research has shown it can prevent the absorption of thyroid hormones in the gut, leading to hypothyroidism. (While I don’t have studies to support it-- just my own observation with my clients-- I suspect this could be true for any parasite or overgrowth causing inflammation in the gut, and not just Giardia.) But the good news is clearing the infection reverses hypothyroidism!
Connecting the Dots & Creating Your Treatment
With the right testing, you might finally be able to “see” what caused your thyroid issues - or is exacerbating them: a gut infection.
All the testing and interpretation brings us to the most exciting point: treating your gut issues, And with that information in hand, we can co-create a 100% unique treatment plan for you.
For my clients, I always create a custom protocol based not only on their test results, but also with their budget and lifestyle in mind. I don’t believe in a one-size-fits-all approach to medicine, which means if you have a strict supplement budget to stick with, or really, really, REALLY don’t want to give up a particular food, we try our best to find a way to work with it so that you get the results you want, within your parameters.
If you want to learn more about what it’s like to work with me as a practitioner, sign up for a no-obligation 15-minute Intro Session here.
This is your chance to share your story with my team and get a realistic look at what working with us is like.
>>> Book an Intro Session Here
I hope this information was helpful to you - and you can find tons more over at my blog: https://briewieselman.com/
- Brie Wieseleman, L.Ac
Recurrent UTIs: Why They Happen & How To Make Them Stop
If you’ve felt it… you know that burn.
The dread washes over you…it’s back again.
You know what’s in store: the burning, of course…constantly feeling like you need to find a bathroom… another trip to the doctor for a urine sample...And probably another round of antibiotics.
That’s life when you’re struggling with recurrent urinary tract infections (UTIs).
And based on the number of women I see with this issue…recurrent UTIs are a major issue that gets very little attention from mainstream medicine.
(In fact, your doctor might not even want to admit it’s happening.)
But if it is happening to you…I’m not being dramatic when I say it’s like a recurrent nightmare.
Today I want to shine a big, bright light on this common issue: explaining not just WHY it happens, but steps you can take to treat existing UTIs and keep them from coming back.
Why Did I Get The First UTI?
If not normal, UTIs are actually very common in women. It’s simply a matter of anatomy: women have shorter urethra, and with the proximity of various openings (you know what I mean), bacteria transfer is inevitable.
Other factors that increase the risk of UTI include:
- Sex (especially with a new partner, who is introducing new bacteria)
- Exercise (especially in tight-fitting pants)
- Holding urine
- Hormone fluctuations
- Pregnancy
- Menopause
Most UTIs are caused by naturally occurring E. coli bacteria that hangs out in the gut. If you have more of that bacteria in your gut, it’s also more likely some of it will migrate down to the urinary tract and cause issues.
My main point here is that there shouldn’t be any shame around getting a UTI - it happens! But if they’re happening over and over again - you don’t have to live that way. So why does it happen?
What Causes Recurrent UTIs
First, I have to tell you an unfortunate truth: The more UTIs you have, the more likely you are to get another.
I know - it’s not fair. But here’s why: the most common treatment for UTIs is antibiotics. Antibiotics wipe out good AND bad bacteria. They don’t discriminate. That can lead to an imbalance of bacteria, weakened immunity, and an easy way for any bacteria that escaped the antibiotic treatment to build back up very quickly. That leaves you at increased risk not just for more UTIs, but bacterial vaginosis and yeast infections, too.
Candida overgrowth can also be a root cause of UTIs. (It’s sort of a chicken-or-the-egg situation, where it’s hard to say if candida came first, or candida was able to flourish because of repeat antibiotic use. Either way, candida has to be treated.)
Recurrent UTIs are also often associated with hormonal contraceptive (the Pill) and long term antibiotic use, such as for acne treatment.
Hormone changes - such as premenstrual - as well as flares of gut conditions (IBS, SIBO, etc.) both also often set off UTIs in my patients.
Recurrent UTIs can also be a sign of an autoimmune-type condition called Interstitial cystitis (IC) that causes chronic pelvic pain.
Depending what the root cause of your recurrent UTIs is, treatment will need to be tailored - but it’s usually some combination of gut microbiome rehab and hormone balancing (more on that to come).
Negative Test Nancy
Remember how I said some doctors don’t even want to admit recurrent UTis are an issue? Part of that has to do with a major testing issue.
The standard UTI test (urinalysis), which looks for white blood cells in the urine to confirm bacterial infection of the urinary tract or kidneys, is not 100% accurate - in fact research has suggested it may be accurate only as much as 30% of the time!
(Because it was designed to detect kidney infections, it uses a threshold for white blood cells that is much higher than many UTIs cause.)
Even worse - the next most commonly used test - a bacteria culture - is based on the now disproven idea that urine is sterile. We actually know urine is teeming with tons of bacteria that should be there…. So a positive bacterial culture doesn’t mean much, either.
And finally, we know that bacteria produce biofilms - I think of them like protective layers of goo on the outside of bacteria - that help them prevent shedding in urine and evade testing.
If you have the symptoms of a UTI, know what it feels like because you’ve had it before, go to the trouble of getting tested, and then get a false negative? It’s incredibly frustrating.
Even if your test is technically negative, you could be dealing with a UTI. There could be multiple causes. There could be multiple solutions. And working with an expert is the best way to suss all this info out.
How To Treat Recurrent UTIs
As I mentioned before, treating recurrent UTIs depends on what the root cause is.
Got crazy PMS that gives you a UTI every month like clockwork? Hormone balancing and healing may be your answer.
Have a wicked case of IBS that comes with a side of UTIs? Gut healing will be key for you.
Been using antibiotics 4x/year for the last 5 years? We’ll need to come up with a customized plan to heal your microbiome and get it thriving again.
Interstitial cystitis at play? I’ve seen patients make major improvements with diet and gut healing work.
But no matter your root cause, if you’ve got a current UTI, we need to take care of it first. (No antibiotics required.)
My method involves:
- Supporting the vaginal microbiome (with both oral and vaginal probiotics)
- Using a biofilm breaker
- Using herbs and supplements to address the infection (more effective and less likely to cause resistance compared to antibiotics, in my opinion)
- Following up with probiotics for preventing recurrent UTIs (this is backed by research)
Normally, I only share my tested UTI protocol with clients…but if you’ve made it this far, I want you to have it, too!
>>>> Download my day-by-day UTI protocol HERE <<<<
Think of it as a sneak-peek into what working with me as a practitioner is like. I hope it helps.
- Brie
PS - If my UTI protocol helps you, leave a comment and let me know! And if you’d like some guidance on your unique situation, don’t forget you can schedule a no-obligation free consult anytime here.
The SIBO Testing Mistake I See All The Time (And How To Test For This Common Condition The Right Way)
Last week I had a consultation with a new patient who had the gut symptoms I see all the time: bloating, food intolerances, and bowel disturbances (yes, I’m talking constipation and diarrhea!).
After hearing her entire health history, I asked if she had ever been tested for SIBO (Small Intestine Bacterial Overgrowth).
“No, that’s not it” - she told me - “I had a stool test that was negative for SIBO.”
Major. Red. Flag.
This is a HUGE misconception - but stool tests cannot diagnose OR rule out SIBO.
I don’t blame this woman or her doctor for being confused. Even great practitioners are often unsure what tests can and can’t diagnose SIBO.
This is really important because with the right testing... SIBO can be treated and resolved, most of the time.
That means you can say goodbye to the bloating and gas (for good) and get back to enjoying life.
If you’ve got digestive complaints - even (and especially) if you’ve been told you don’t have SIBO before - this blog post is for you. Let’s clear up all the misconceptions about SIBO testing so you can get on the road to healing.
What Is SIBO?
Small Intestine Bacterial Overgrowth (SIBO) occurs when bacteria overgrow in the small intestine. Normally, there should be very few bacteria in the small intestine - instead, bacteria should live in the large intestine.
When bacteria overgrow in the small intestine, those bacteria can feast on undigested food as it leaves the stomach and enters the small intestine. As the bacteria eat, they produce gas (hydrogen, methane, and hydrogen sulfide) and that gas causes symptoms like diarrhea, constipation, and bloating.
So why do they overgrow? There are tons of reasons - but some of the most common reasons I see are:
- Endometriosis (which can cause sticky scars, called adhesions, inside that prevent the normal flow of bacteria)
- Certain medications that slow down the digestive system (opioids are a common culprit)
- Past food poisoning (which can trigger an autoimmune reaction that impacts motility)
If you’ve never heard of SIBO, you might think it sounds really rare or unusual… but it is very common. About one billion people worldwide have “Irritable Bowel Syndrome” - and of those, 60% are believed to actually have SIBO as a result of post-infectious IBS - which puts the estimate at about 600 Million people with SIBO!
Why Having SIBO Can Be Good News
The truth is I LOVE seeing a positive result on a SIBO breath test… not only does it explain why a patient has been dealing with symptoms (often for years)... but it is also a problem we can usually fix.
Depending on the type and severity of SIBO, it can be resolved in as little as one treatment cycle.
But successful treatment is wholly dependent on testing, since different types of SIBO require different treatments.
That’s why SIBO really requires not just an accurate test - but a practitioner who can interpret the results and create a customized treatment plan based on them.
Why Stool Tests Can’t Diagnose SIBO
To put it simply, stool tests are looking at the wrong part of the body. Stool tests tell us mostly what is happening in the large intestine - not the small!
So while it is possible that some of the organisms we see in stool testing are living in the small intestine, the results we get are more reflective of the large intestine.
Furthermore, while there can be some indicators that SIBO is likely from stool testing results, it's impossible to differentiate small vs. large intestine.
Stool tests can be really useful for diagnosing many other conditions - parasites, enzyme deficiency, and more - but they are not able to determine if bacteria is overgrown in the small intestine.
I love stool tests - and if you’re coming to me with gut issues, I almost always order a stool test - but it won’t tell you if you have SIBO!
Urine Organic Acids Tests Don’t Work Either
The urine organic acids test is another popular and really useful test - unless you want to diagnose SIBO.
The organic acids test can indicate if a bacterial overgrowth is present, but the problem is it can’t differentiate between the small and large intestine.
(Yes, Large Intestine Bacterial Overgrowth (LIBO) is a thing too!)
If you don’t know where the overgrowth is, you don’t know which treatment to use.
Again, this is a really useful test (and one I often use for other conditions) but it can’t diagnose SIBO.
The Right Way To Test For SIBO
There are 2 ways to test for SIBO properly:
- Endoscopy with culture (not commonly used anymore)
- Breath test (the gold standard and what I use)
(There is also a blood test for post-infectious IBS (which is a form of autoimmune IBS caused by food poisoning) that can be used, since most people with post-infectious IBS have SIBO. I use this if a breath test was inconclusive.)
The breath test is far and away the most simple, accurate, and useful of these tests, and it’s what I alway use with my clients.
That being said... Even though the breath test is the best, it doesn’t mean it’s perfect.
The breath test works by measuring hydrogen and methane gas in your breath after a special 24-hour prep diet and consuming a sugar solution (aka the test substrate). There are two options: glucose or lactulose.
The glucose test is only able to diagnose SIBO in the beginning of the small intestine (the small intestine can be over 20 feet long!). Because glucose is rapidly absorbed in the intestine, it isn’t good for finding SIBO that is farther down the small intestine.
The lactulose breath test can diagnose SIBO in any part of the small intestine, but it does have a higher rate of false positives.
Glucose is more likely to miss some cases of SIBO, but the ones it does identify are more likely to be true positive diagnoses.
Therefore, I sometimes run glucose and lactulose tests side by side to get a more complete picture.
Why The Right Test Matters So Much
I’ve said it before, but it’s so important that I will repeat it now: in SIBO, testing guides the treatment.
Depending on which gases are detected in your breath, and at what levels, treatment will differ.
That’s why it’s also really key to have help interpreting a test from a skilled practitioner. SIBO breath test results aren’t a simple “positive” or “negative” - you’ll get a graph that shows different gas levels at different points in the test.
If you’ve never seen them before, these graphs are confusing and overwhelming. But to someone who knows what they’re looking at, your breath tests results are like a map to healing your SIBO and resolving your symptoms.
Bottom line: if you suspect SIBO, get a breath test!
Get Help With SIBO
SIBO is a really complex condition (let’s not sugar coat it!). But it’s not incurable… and if you DO have it, resolving SIBO might be the answer to years of uncomfortable gut symptoms.
Every case of SIBO requires personalized treatment, but that’s part of why I love my job - helping you put the pieces of your health puzzle together and achieve your goals is my purpose in life!
I’ve helped hundreds of people diagnose and resolve SIBO… and I’d love to help you, too! There’s no need to make a commitment right now - book a free 15-minute consultation with my team to learn about how we could help you and what options you have here ---> Book a Free 15-Minute Consult
What We Know (& Can Do) About Coronavirus So Far
There’s only one topic on everyone's minds and hearts right now: coronavirus.
And as a health practitioner, I can’t ignore it!
Unfortunately, there is so much bad information out there right now… and even worse, some of it is coming from the alternative health space.
I don’t want anyone to feel panicked, but we do need to take this very seriously.
Today, I’m sharing exactly what we know about treating coronavirus (aka covid-19) so far.
#1 Social Distancing Is The Best Tool We Have
Other than washing hands and covering your face when you sneeze or cough, (please do these things!) the best tool we have to slow the spread of coronavirus is social distancing.
Social distancing is like “herd immunity” in that it only works if people who are and aren’t sick (and are and aren’t at high risk) all participate.
Even if you are not personally worried about coronavirus, you help protect the health of those at risk by staying home as much as you can. Cancel appointments. Don’t have people over to your house. Don’t go to the gym.
It's OK to go on walks and spend time outside - just keep your distance from others as much as you can.
When you DO go out (like to stock up on essential groceries), wash your hands, change clothes, and wipe down anything you took out with you (yes, I’m talking about your dirtier-than-a-toilet phone!). And if you are anyone in your household have symptoms that are vaguely viral, I would encourage you to use a service like Instantcart, and have someone shop for you for a very small fee and leave the groceries on your doorstep.
I recommend checking THIS website for accurate, up-to-date information on the virus. However, even medical professionals can’t get access to tests for covid-19 (because there are not enough tests!). You should assume the numbers in your community are MUCH higher than we see reported.
#2 Antioxidants Have Potential To Help
Research has shown that certain antioxidants (lipoic acid, ferulic acid, and sulforaphane specifically) have potential for boosting the type 1 interferon response to RNA viruses (including influenza and coronavirus).
That’s a science-y way of saying, they help your body fight off viruses more effectively.
Even better, there is some evidence that certain antioxidants could help fight off inflammation in the lungs caused by viral infections. This is important, because coronavirus primarily impacts the lungs, and, the part of the illness that can ultimately kill people is called ARDS (Acute Respiratory Distress Syndrome). ARDS occurs when an influx of inflammatory cells from your own immune system infiltrates the endothelial tissue in the lung, causing massive levels of oxidative stress in an attempt to fight the virus.
Other nutrients to consider:
Selenium: Selenium-deficient mice are more likely to get the flu, and selenium deficiency also promotes virus replication. Selenium deficiency also increases the rate at which viruses can mutate, potentially creating more virulent strains that may be better at avoiding detection. Selenium deficiency is known to be wide spread across certain regions of China where the virus has more readily spread.
Spirulina: Has been shown to decrease influenza mortality in mice. (Yes, mice, but the mechanism by which it works functions the same way in humans)
High dose glucosamine: Dampens inflammatory reactions (and therefore may help protect the lungs in case of infection)
N-Acetylcysteine (NAC): promotes glutathione production, the “master antioxidant.” It’s also mucolytic, which means it can clear up mucus and help get rid of gunk in your chest and nose. This has shown to be particularly helpful in the elderly, perhaps because plasma cysteine levels and cellular glutathione levels tend to decline with advancing age.
I’ll also be sharing my own personal supplement regimen at the end of this post.
#3 Vitamin C Is Being Studied Right Now
At the time of this post, there are already 3 clinical trials underway in China right now where patients with coronavirus are being treated with high dose vitamin C.
It’s obviously too early to make any conclusions but…. I like what I’m seeing!
Vitamin C helps in multiple ways. It can help prevent the onset of sepsis-related lung damage (a major concern for anyone who is hospitalized). It helps shorten the duration of the common cold and some studies have shown that low vitamin C levels are related to increased flu risk. And it is known to play a role in killing viruses and preventing their replication.
Just know: taking a vitamin C supplement every morning is not going to be the same as the high-dose IV treatments being studied in hospitals right now. If you are sick, taking vitamin C will not replace getting medical care! That being said, I’m still using vitamin C supplements right now., and if you do get sick, I recommend oral Vitamin C hourly, or administered via an IV by a licensed professional if you have access to one.
#4 TCM Can Aid Western Medicine
Most people don’t know that during the SARS epidemic, healthcare workers were treated with Traditional Chinese Medicine (TCM) to help prevent them from getting sick.
Today, the formula being used with coronavirus is adapted from Qing Fei Tang (clear the ling decoction). It is being used in combination with Western medicine to help people recover more quickly.
(FYI: This formulation isn’t for prevention - it’s for those who are already ill.)
In south Korea, public health officials are doing trials with Fah Talai Jone herb (Andrographis paniculata, also known as Chuan Xin Lian in Chinese Herbal Medicine) which contains Andrographolide (an extract from the herb). Tests in China indicated that Andrographalide could help prevent viruses in humans.
My hope is that anyone who is sick will be offered both Western and TCM treatments. The more we can do, the better!
→ Brie’s Supplement Regimen
I’ve amped up my supplement regimen in wake of the coronavirus. I don’t believe any of this will prevent me from getting sick… but I do know that it will help me recover should I become ill.
Even with supplementation, I’m still relying on washing my hands religiously and staying home as much as possible.
Luckily, I work with all my patients remotely, so it hasn’t had to impact the flow of our practice.
OK, here’s what I’m doing:
Multivitamin (this is the one I use)
Probiotics (Rotating Megaspore, Therbiotic Complete and floramyces)
Selenium 200 mcg
Zinc 20 mg
Host Defense Mushroom blend
Vitamin C 1000 mg 3 x day (it’s key to take vitamin C multiple times per day, as it is depleted and excreted very quickly)
Cold away by Health Concerns and/or Olivirex --1-2 times daily
Vitamin D 2000-5000 IUs
Magnesium 400 mg
NAC 600 2 x day
Spirulina 15 g
Jade Wind Screen (There are many brands with different names for this product. It is a chinese herbal formula called Yu Ping Feng San, and contains high dosages of astragalus in combination with other chinese herbs, and is intended to be used long term during cold and flu season to avoid illness. Do not use if you have known, active autoimmune disease. Some of the brands I like are Health Concerns AstraC or Astra Essence and Kan Herbs Initial Defense).
I may add some sulforophane. I am certainly keeping andrographis stocked and on hand. I have some Biocidin throat spray around as a first layer of defense for when I’ve been out and about.
I'm avoiding Elderberry because with PCOS, I'm on the autoimmune spectrum. Elderberry can flare existing autoimmune conditions, but it can also promote a “cytokine storm” - an overproduction of immune cells. If you're prone to autoimmunity and you contract a virus, the resulting cytokine storm can trigger the development of autoimmune conditions.
And I'm giving my baby Windbreaker by Kan herbs in low dose, with Vitamin D 400 daily and some Vitamin C.
What if you get sick? I would increase oral Vitamin C to hourly. High doses of vitamin C can cause loose stool, but this is less likely during times of sickness when your body has a higher demand of C.
I keep on hand any brand of the Early stage "Wind attack" chinese medicine formulas, as variations on these are what is being used in China both for sick patients and preventatively for health care providers. Some of the formulas that can be used are:
These are taken if you are exposed, and/or if you start to have symptoms like sore throat, or fever and are continued for as long as the symptoms stay in the throat, sinus, or upper lung.
Combining any of these, or similar, with Andrographis, one of the main chinese anti-viral herbs, (which I mentioned above is being used and studied for this virus). Some forms of this are Chuan Xin Lian, Antiphlogistic Formula, or Clear Heat)
There are other chinese herbal formulas being used for symptoms, but these should be prescribed and adapted by a chinese herbalist. I'm available for consultations should you or someone you love need support beyond the first stage of symptoms.
And equally importantly: don’t forget to consider your mental health and stress levels. Take a break from the news when you need to, and even with social distancing, stay connected via phone with the people you love.
I hope this information has given you some practical advice, as well as hope.
Do you have questions about the coronavirus? I’d love to help clear up confusion where I can. Click here to contact my office.
More Information (And Works Cited In This Article)
https://www.domo.com/coronavirus-tracking
https://www.thaipbsworld.com/59-returnees-from-s-korea-isolated-as-two-new-covid-19-confirmed/
https://www.ncbi.nlm.nih.gov/pubmed/32061635
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5295174/
https://clinicaltrials.gov/ct2/show/NCT04264533
http://orthomolecular.org/resources/omns/v16n12.shtml
Endometriosis 101 Part 2: How I Help My Patients Dealing with Endometriosis
Check out "Endometriosis 101 Part 1: What Is this Condition & Why Is it Happening to Me?" HERE
While functional medicine practitioners don’t know with certainty the root cause of endometriosis either (we’re still waiting on the science), we focus on what we do know about the condition by working to reduce inflammation and support the immune system.
Pain management and even surgery might be part of our treatment plan - but I would never see a woman in endometriosis pain and just throw the birth control pill at her! I am not interested in band-aids. I want real solutions for my patients.
Here’s how we address endometriosis (but remember that every treatment plan needs to be customized for your unique needs):
These steps can happen in any order or all at once, depending on your situation.
#1 Heal The Gut
Addressing gut health should always be high on your list for really any health concern, but especially for anything autoimmune.
I often see bacterial infections like SIBO (Small Intestine Bacterial Overgrowth), parasites, viruses, mold and toxin exposure, and food sensitivities. In studies, 80% of women with endometriosis also had SIBO.
These can all be signs and triggers for leaky gut, so addressing them and then working to heal the gut is key to recovery.
I like to start with a comprehensive stool test like the GI Map to find any gut health issues. Then we’ll work to clear any infections and implement dietary changes to support the gut (this could be an elimination diet, but that is not always the answer!).
One dietary change I do recommend? Cutting dairy and soy. There is a lot of research to support the idea that dairy and endometriosis are not good together. Dairy is hormonal, it’s a really common allergen, and it’s also pro-inflammatory. (As is soy.)
Do you have to quit them both forever? Absolutely not. Once you have endometriosis under control, you can probably enjoy them again in moderation. And of course, quality and quantity matter a lot. Go for grass-fed and organic, minimally-processed dairy when you do have it.
Another thing I look for on stool tests is high beta-glucuronidase. Beta-glucuronidase is an enzyme produced by gut bacteria and can be elevated by parasites and other gut infections. When beta-glucuronidase is high, it can lead to estrogen buildup. If you have high beta-glucuronidase, I’ll use calcium d-glucarate and Lactobacillus to help lower this and reduce the estrogen recirculation.
#2 Reduce Inflammation
Next, we’ll take a look at your lifestyle and see what could be leading to increased inflammation. It could be late nights at the office, too many meals out, drinking too much, or even “healthy” habits like over-exercise or a really restrictive diet.
Overtraining isn’t an issue for all women - but you might be surprised how easy it is to become “overtrained” with even a moderate exercise regimen. Remember, overtraining isn’t necessarily about too much exercise… it’s about too much exercise relative to too little recovery. That’s why Olympic athletes can exercise so much without overtraining - they spend all the rest of their time recovering! But for women who have to work, commute, get dinner on the table, do laundry, etc. etc. etc. there is rarely enough recovery time!
Stress in any form is incredibly inflammatory, but it’s not the only inflammatory element to look out for. The modern world is pretty rife with chemicals… and no one wants to think about the cumulative effect of the pollution we breathe (drink and eat, too!), the chemicals in all the products we use (from cleaning to personal care), or the added ingredients in most of our food (including unwanted pesticides and other chemicals). But - it all adds up to a lot of potential inflammation.
But, you don’t have to start living like a monk and throw away everything plastic in your home. I’ll help you choose where you can make a few key changes to reduce overall inflammation.
#3 Stabilize Blood Sugar
One big myth is that weight loss can help with endo symptoms. If you’re carrying a lot of excess weight, losing weight can potentially help with symptoms (since hormones are produced in fat cells) - but that doesn’t mean weight loss is a “cure.”
If you’re already lean, the extra stress on the body of trying to lose more weight can make your symptoms worse. And even if weight loss is one part of your healing plan, it’s definitely not the whole story.
Rather than emphasize weight loss, I like to focus on stabilizing blood sugar with a whole-foods based diet.
This is really important because higher blood sugar levels lead to increased insulin, which stimulates the conversion of testosterone into estrogen. This is just another contributor to the high estrogen levels that are linked to endometriosis.
#4 Balance Hormones
You can’t diagnose hormone imbalance based on symptoms, so I never start a hormone protocol without testing. I use the DUTCH Hormone Panel with my patients.
Once we’ve identified your imbalance, we’ll come up with a plan to correct it - everything from herbals and supplements to acupuncture, exercise, diet, and stress management can come into play.
Some of the herbs and supplements I use most often are:
Melatonin
Melatonin is an antioxidant that has been shown to be able to reduce pelvic pain associated with endometriosis. Now, I don’t want to give out a dose because it’s not the typical low dose that people use to help them sleep. It’s actually a pretty high dose. And it can definitely make people groggy. As a practitioner, I want to make sure it’s appropriate for you. But in the right dosage, melatonin can reduce endometriosis pain by as much as 40%. And it’s safer than the pharmaceutical options by far!
Before supplementing, you can also do things to naturally increase your own melatonin levels like have good sleep hygiene, avoid caffeine, avoid blue light after three in the afternoon, and sleep in a dark room.
Vaginal Probiotics
This is one of my favorite tools - and yes, it is what it sounds like: just take probiotics, and stick them up there! This is really safe and one of the easiest ways to shift the vaginal microbiome.
(If you have chronic yeast or bladder infections, or bacterial vaginosis, this can also help with those conditions in many cases!)
The brands I recommend are Jarrow’s Fem-Dophilus and FloraFemme.
Pycnogenol
Pycnogenol is another really well-known antioxidant that’s very specific to lowering pain and lesions in endometriosis. It’s safe and effective for many women.
Bioidentical Progesterone
This really depends on the woman and proper hormone testing. Please don’t go buy some natural progesterone cream and start self-supplementing! Getting the dose right and monitoring while you use it is so important.
But this works because proper progesterone levels balance and oppose estrogen. Think of it like a teeter totter. But in women with endometriosis, there is evidence that they may have progesterone resistance and therefore need slightly higher progesterone levels than the average woman to achieve that balance.
DIM
Diindolylmethane (DIM, in short) is a phytochemical found is cruciferous veggies (think broccoli, cauliflower, brussels sprouts etc.) and it’s one of my favorite tools for estrogen dominance. It helps balance levels of different types of estrogen and block androgen receptors. Get it from eating lots of veggies, or try a supplement.
#5 Support Better Detox
Your body knows how to detox itself (thanks to your liver, kidneys & more) - and you don’t need a 10-day juice fast to “cleanse.” But that doesn’t mean we can’t support detox.
Your detox symptoms can easily become overburdened when you consider the amount of toxins you’re exposed to (pollution, chemicals in cosmetics, pesticides on food to name a few). Your liver can get “jammed” trying to detox as much as possible - which can then burn through your glutathione stores and leave you feeling totally burnt out.
And remember - your liver also plays a major role in detoxing excess estrogen, so if it’s jammed up, you’re setting yourself up for estrogen dominance.
I’ll have you take a look at where you’re being exposed to toxins as well as teach you some easy tricks for supporting the body’s detox processes.
These are some of the supplements I love for supporting better detox:
Calcium D-Glucarate
Calcium d-glucarate is one I mentioned before for gut health. It is a supplement that’s pretty safe to play with if you have endometriosis because you can assume that you have some level of estrogen dominance. But again, I like to use it based on stool testing so we can be certain that excess beta-glucuronidase enzyme is in fact a part of your issue. Because why take excessive supplements that are not doing for you what you need? That’s a waste of time and money.
N-Acetylcysteine
I always say this is the supplement I would take if I was trapped on a deserted island… it’s just awesome. It has many uses and it supports the production of or master antioxidant, glutathione (which we all need more of!)
In a double-blind study, 92 women with endometriosis were either given NAC or no treatment. And during the NAC treatment, they saw a distinct reduction in the number of cysts or tissue implants, as well as size. In the women using NAC, lesions stayed the same or actually shrunk.
In the no treatment group, lesions tended to grow! The NAC was more effective than hormonal treatments.
And the crazy part is that 24 women in the NAC treatment group who had scheduled laparoscopy actually cancelled their surgery because they had such a great reduction in pain. One woman even got pregnant!
I can’t recommend NAC highly enough. But quality does matter - I usually use physicians-grade from brands like Pure Encapsulations, Thorne, or Designs for Health. I like to use 500 mg, 2-3 times daily.
One caveat: if you have acute gastritis (inflammation of the gut lining) NAC can thin the gut wall slightly, so it might not be right for you.
Don’t Just Accept Endometriosis or Painful Periods
I would never lie and tell you that I have a magical cure for endometriosis. I don’t (and no one does).
What I do have is a holistic approach to healing that takes into account not just symptom management - but also addressing the root causes so that you can experience true relief.
Because there are multiple layers to healing endometriosis, I recommend you get support from an experienced practitioner. A practitioner can help you assess your gut health, hormones, and detox symptoms and strategize healing. Working with an experienced practitioner can turn and a long and frustrating process into a much shorter one. (The majority of my clients see major, lasting improvements in just 3-6 months.)
It’s very possible to be symptom-free, even with endometriosis. It’s very possible to see heavy bleeding, painful periods, and PMS go away. I’d love to help you.
You can book a free 15-minute consult with my team right now. During the call, we’ll listen to you and explore how we could guide your health forward (no obligation!).
Periods shouldn’t be painful or something to dread! I’d be honored to help you take back control and feel better.
P.S. Do you feel like you’re already eating well, managing stress, and STILL struggling with endometriosis? I’d love to learn more and see if we can’t get you feeling better. Book a free 15-minute consult today.
Endometriosis 101 Part 1: What Is this Condition & Why Is it Happening to Me?
Check out "Endometriosis 101 Part 2: How I Help My Patients Dealing with Endometriosis" HERE.
You might have heard me say this before: Your period is not a curse.
The truth is that your period is actually a sign of amazing things happening inside your body (regardless of if you ever even want kids!).
But…for some women, your period can feel like a curse from hell - all due to a condition called endometriosis.
Listen up ladies: If your periods are painful, long, heavy, and something you downright dread, please read this article.
If your doctor has told you they suspect endometriosis, please read this article.
If you’ve been suffering for YEARS without relief, please read this article.
One in 10 women in the U.S. is estimated to have endometriosis. (And it takes an average of 8-12 years to be diagnosed).
I won’t pretend I have a magic cure for endo (I wish I did!). But what I can do is share what I know, and assure you: You aren’t crazy. It does hurt. But it doesn’t have to be this bad forever.
This is a big topic, so I’m going to be covering it in two posts. Today, in Part 1, we’ll learn what endometriosis is, its symptoms, and what we (think) causes it. Part 2 will be all about actionable solutions you can put into practice right away.
What Is Endometriosis?
Have you ever wondered what your period is actually made of? It’s not just the same blood you see when you cut your finger - it’s actually endometrial tissue. Over the course of the month, women grow endometrial tissue in the lining of the uterus. When you have your period, that tissue is shed. (If you get pregnant, that endometrial tissue is important for supporting the fetus).
Endometrial tissue is “hormonally responsive” which means it reacts to normal hormone changes that come with your monthly cycle. Blood flow is controlled by inflammatory compounds called prostaglandins.
A normal woman grows endometrial tissue in the uterus and then sheds it during her period. It’s all relatively painless.
But in a woman with endometriosis, the endometrial tissue grows outside the uterus. Most commonly it grows around the fallopian tubes and ovaries, but it can extend into the digestive system and really start growing anywhere in the body.
Endometrial tissue is hormonally responsive no matter where it is in the body - when hormone levels fluctuate (as they should to create your monthly cycle), all endometrial tissue (even that which has overgrown) will respond.
That means more inflammatory prostaglandins leading to pain, inflammation, and even scar tissue (adhesions) where endometrial tissue is located.
This can cause extreme pain during your period, from ovulation through your period, mid-cycle, and, for some women, all month long.
Pain can range from mild to excruciating, and frustratingly, the extent of the endometriosis does not correlate with how severe symptoms are. A little endometriosis can cause a LOT of pain.
Aside from pain, endometriosis regularly causes digestive issues and can impact fertility. It also increases PMS.
It’s estimated, however, that 20-25% of women with endometriosis have no symptoms. They may only be diagnosed when they have fertility issues.
If you do have extremely painful periods, heavy bleeding, and even symptoms like IBS that haven’t responded to treatment, please know that it is not normal and can be a sign of endometriosis. It takes the average woman 8-12 years to be diagnosed with endo. That's 8-12 years of suffering you shouldn’t have to endure!
What Causes Endometriosis?
The sad truth is that we don’t know for sure what causes endometriosis. Both traditional and functional medicine practitioners agree on certain things - but there’s no one proven cause.
While not currently classified as an autoimmune disease, endometriosis is known to have autoimmune features. It is also known to be related to hormone imbalance.
One other theory is about retrograde blood flow - basically when blood flow washes back up into the uterus and fallopian tubes. But, not all women who have some degree of retrograde blood flow develop endo - which means retrograde blood flow is just one of the mechanisms of endometriosis.
Because there isn’t a good understanding of what causes endometriosis in traditional medicine, most traditional solutions are focused on pain and symptom management...
Traditional Endometriosis Treatments (The Good, Bad & Ugly)
In traditional medicine, typical endometriosis treatments include:
- Oral contraceptives or the hormonal IUD (to block ovulation)
- Pain management (Ibuprofen, etc.)
- Surgery (ablation to remove endometriosis and even complete hysterectomy)
I will never shame a woman for using any of these treatments, and I think (at times) they have merit.
The biggest “red flag” is using oral contraceptives to block ovulation. Like with other conditions, oral contraceptives just work as a “band-aid” and do not address underlying causes. When you stop the pill, symptoms will resume. And because the artificial progestins in birth control can exacerbate estrogen dominance, long-term oral contraceptives can make endometriosis worse.
Not to mention that oral contraceptives can be just as damaging to the gut as antibiotics, and that can exacerbate leaky gut!
Are you using oral contraceptives to manage endometriosis? I’d love to explore what other treatment options are available to you. Book a free 15-minute consult with my team today.
Ablation surgery, on the other hand, can be transformative for women who have progressed endometriosis - and can even restore fertility in some cases! However, I think surgery should always be accompanied by other approaches to address underlying causes and inflammation.
I think a total hysterectomy is unfortunate…and I hope that most women with endometriosis don’t get to the point where such an extreme surgery seems like the only answer. In Chinese medicine, the uterus is considered the second heart, and a recent study showed women who had hysterectomies had higher rates of depression.
And while there is nothing wrong with pain management, functional practitioners like myself tend to focus more on suspected root causes of endo so that we can move beyond just pain management and toward resolution of symptoms.
Let’s talk about that now...
A Functional Perspective On What Causes Endometriosis
I often call endometriosis a disease of hormone imbalance. Specifically, endometriosis is associated with estrogen dominance due to low progesterone (where estrogen becomes high relative to low progesterone).
Low progesterone can have many causes. The most common I see are genetic, due to extended use of hormonal contraceptives (which tend to increase estrogen and decrease progesterone), and as a result of chronic stress. If you have adrenal dysfunction or HPA axis dysfunction, your body may downregulate progesterone to prevent conception during stress.
What you might not know is that estrogen dominance is a component of many autoimmune conditions. (And that may be why autoimmunity is more common in men than women). This might be because high estrogen levels are inflammatory.
Like I mentioned earlier, endometriosis isn’t considered an autoimmune disease (yet). But it definitely has the “hallmarks” of autoimmunity: inflammation and immune dysregulation.
With endometriosis specifically, there is both a localized, chronic inflammation and the presence of self-antibodies. What we don’t yet know is if this is a response to endometriosis or the actual cause of endometriosis.
But we do know that there is also an increased number cytokines, an inflammatory component, and lower levels of apoptosis, which means cells aren’t dying at a normal rate.
All of this points to autoimmune - as does the fact that endometriosis also frequently occurs alongside other autoimmune diseases like MS, Hashimoto’s, lupus, and Inflammatory Bowel Diseases like Crohn’s and Ulcerative Colitis.
Research at the University of Tennessee has also shown that 100% of women with endometriosis also have leaky gut. (This doesn’t mean 100% of women in the world have leaky gut if they endometriosis - just women in the study - but it is a compelling number!)
That makes sense, since functional practitioners have long seen a strong link between leaky gut and the development of all kinds of autoimmune conditions.
I Have Endometriosis…Now What?
I never want to see another woman with endometriosis given a prescription for the Pill and a suggestion for a heating pad as a “solution” ever again.
As a functional medicine practitioner, my mission is to help you address endometriosis holistically.
Make sure you check out part 2 of this article for more information on exactly how I support my patients with endometriosis.
P.S. Also be sure to listen to my guest podcast appearance where I spoke with Tawnee Gibson of Endurance Planet all about endometriosis! Listen here.
























