What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
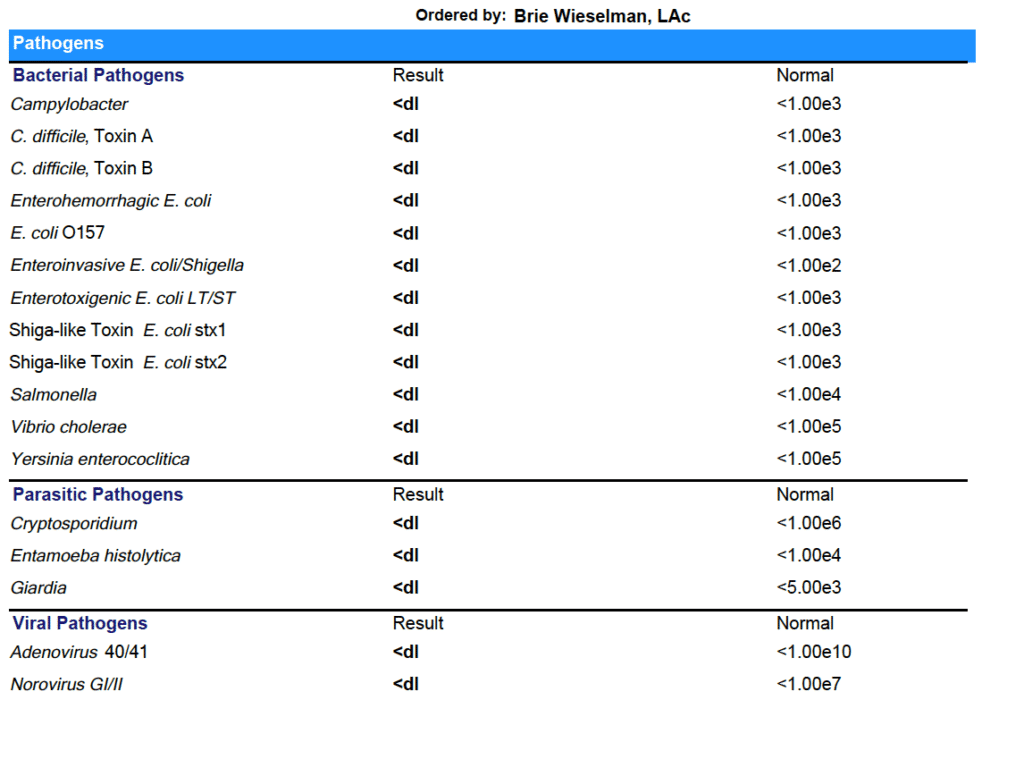
Marina agreed to the test, and a few weeks later, results were in:
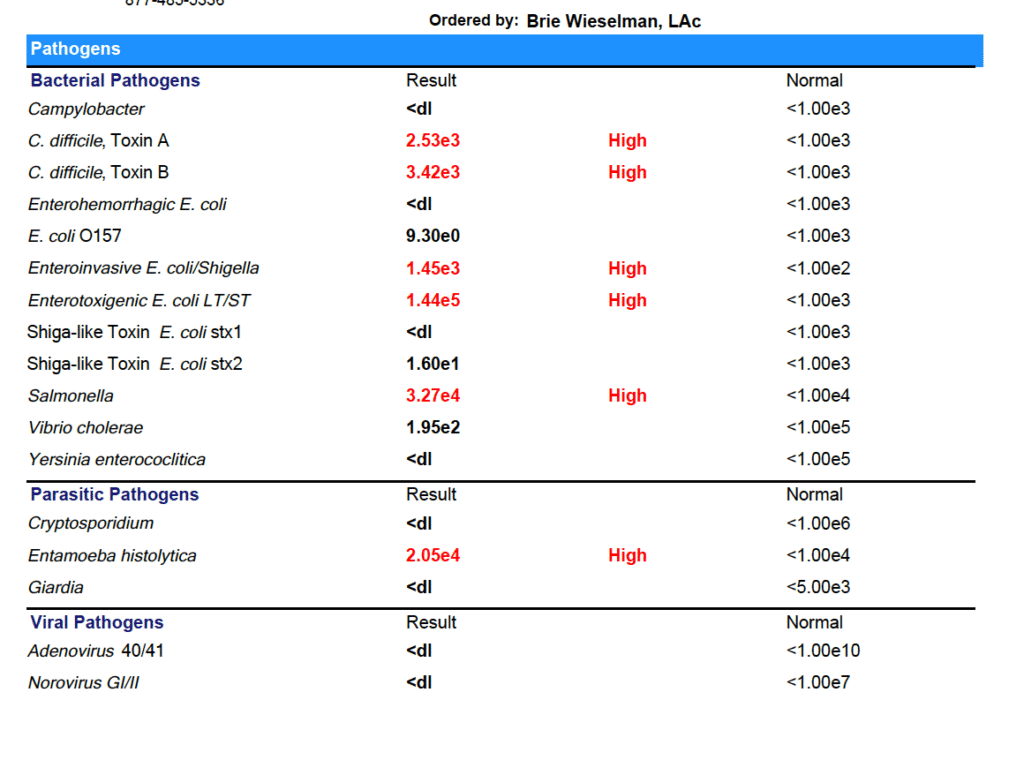
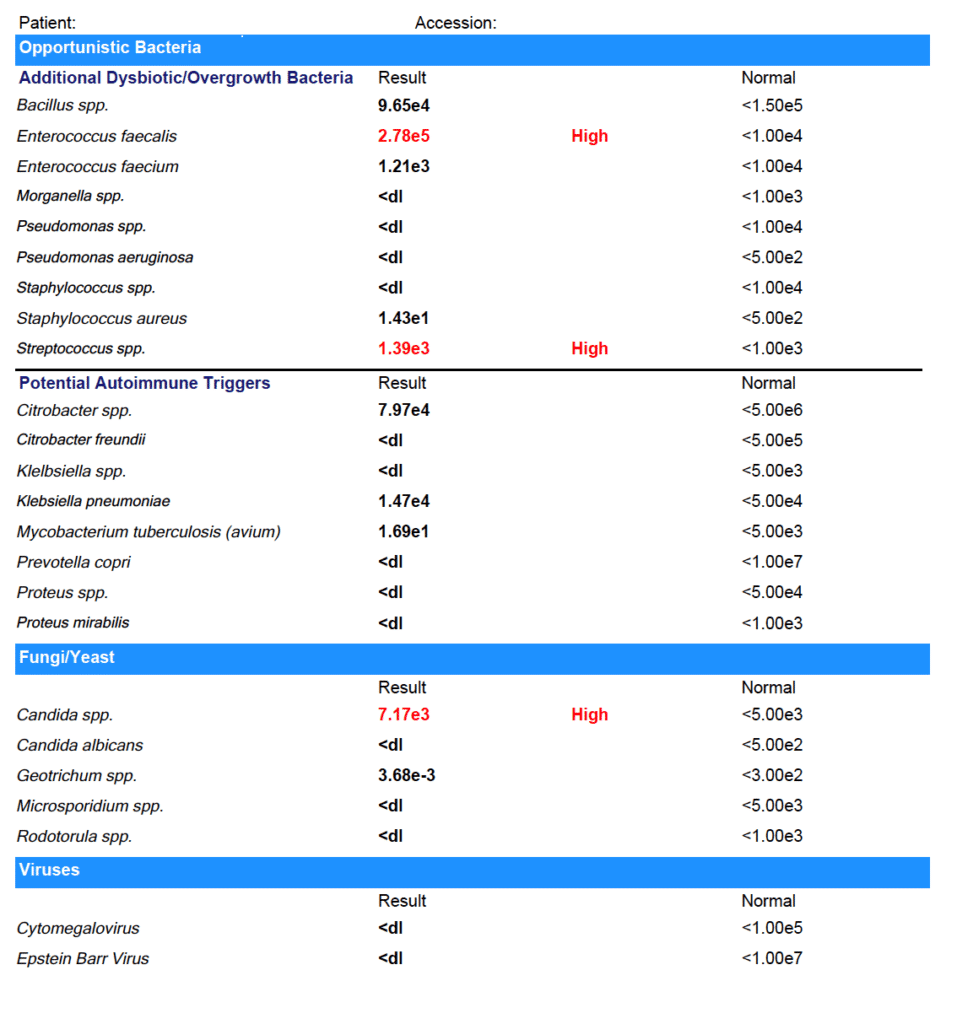
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
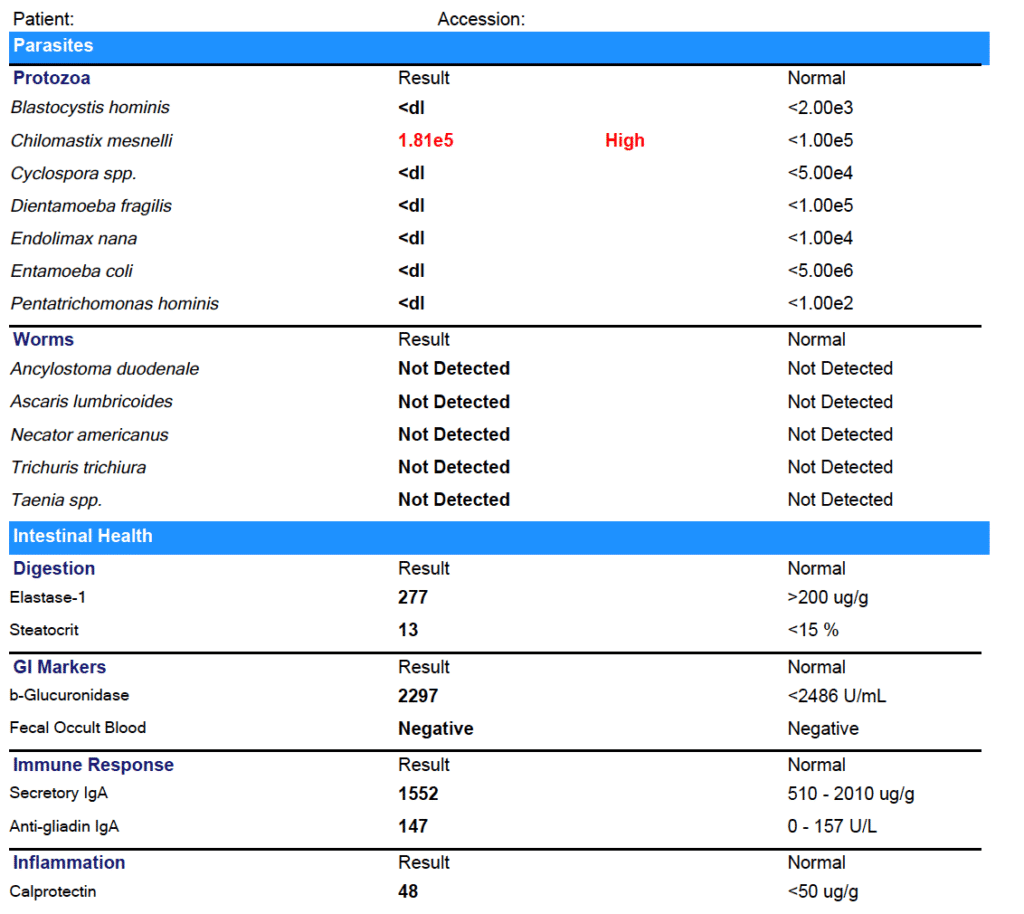
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
Step 3: The Second Test Results:
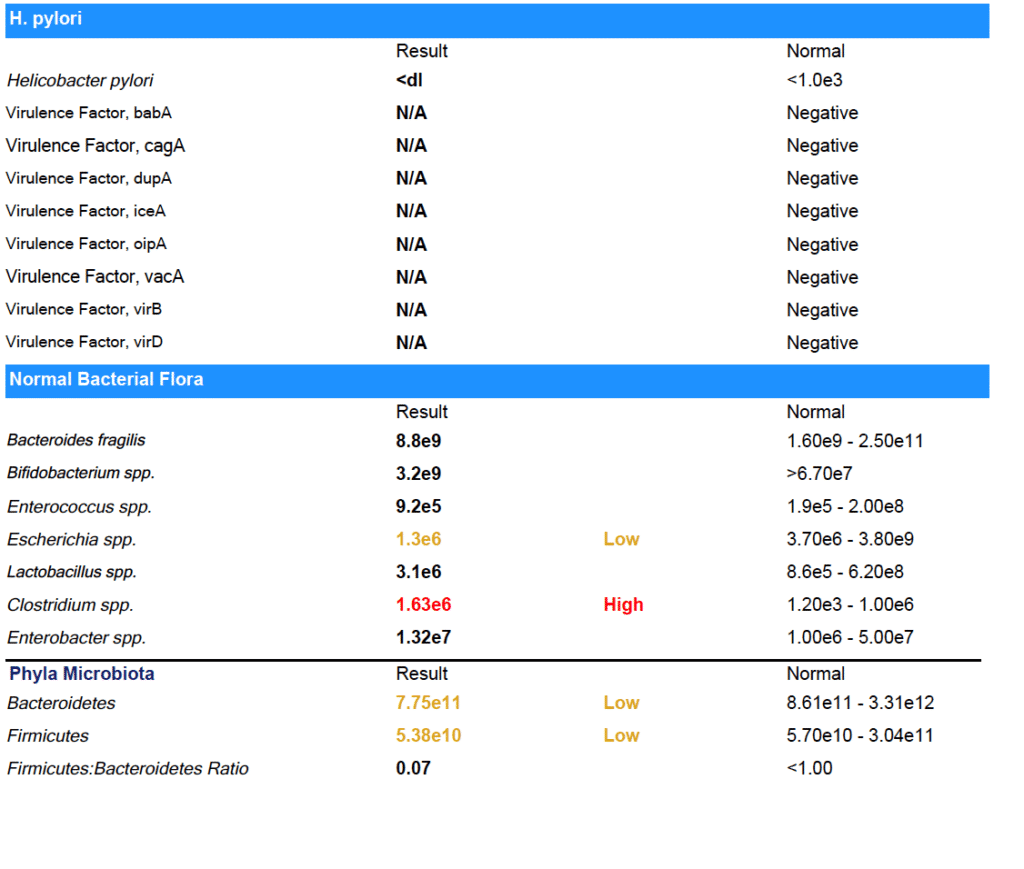
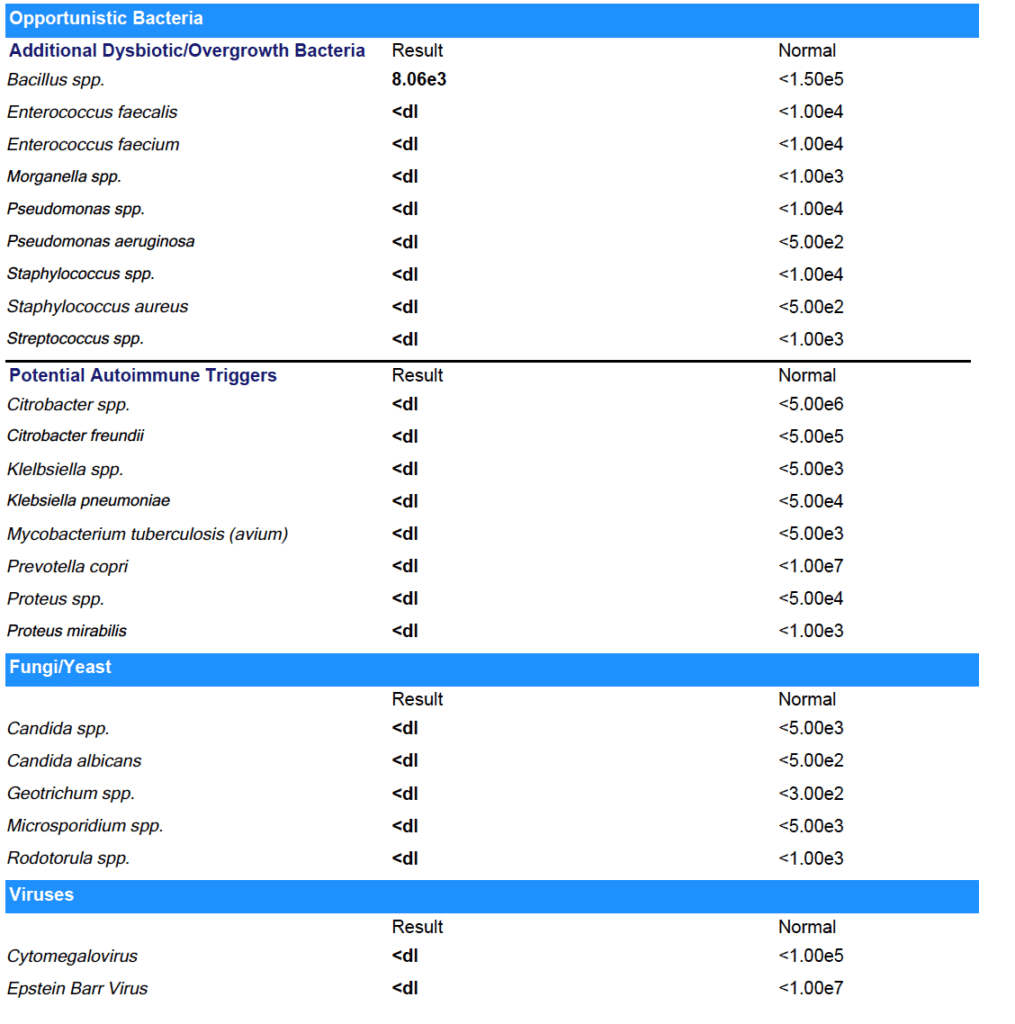
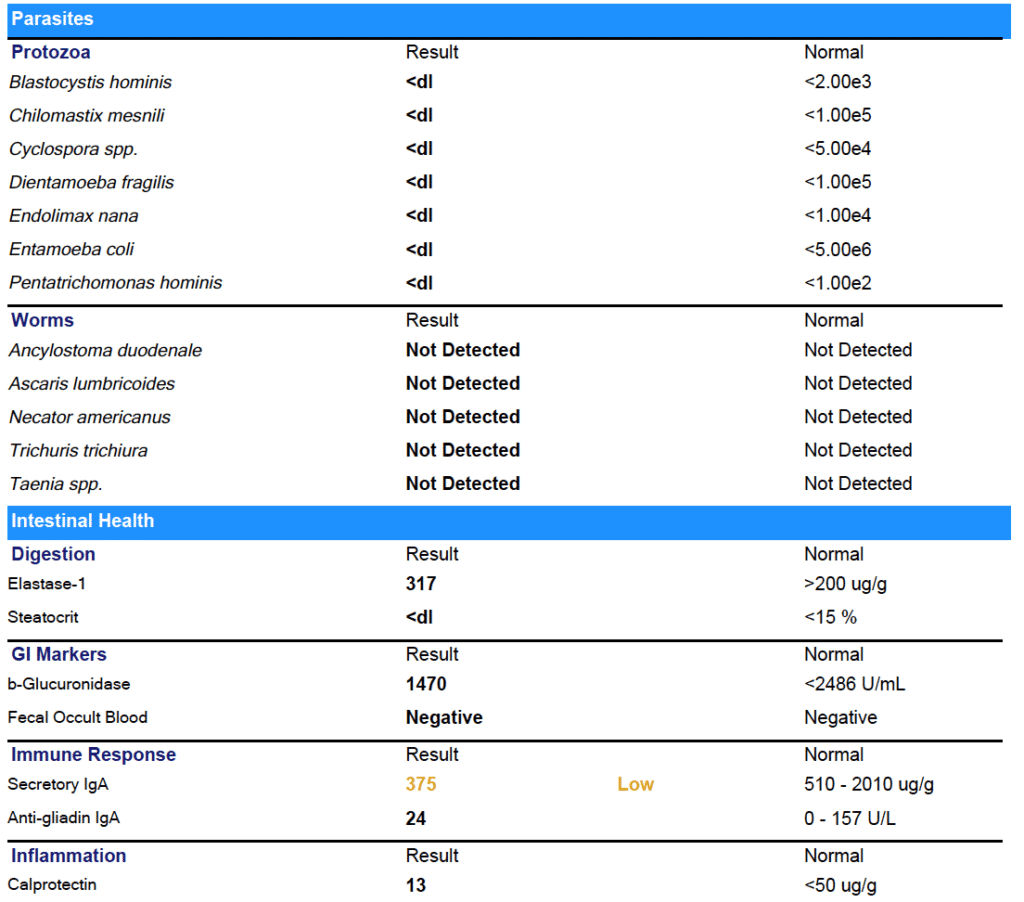
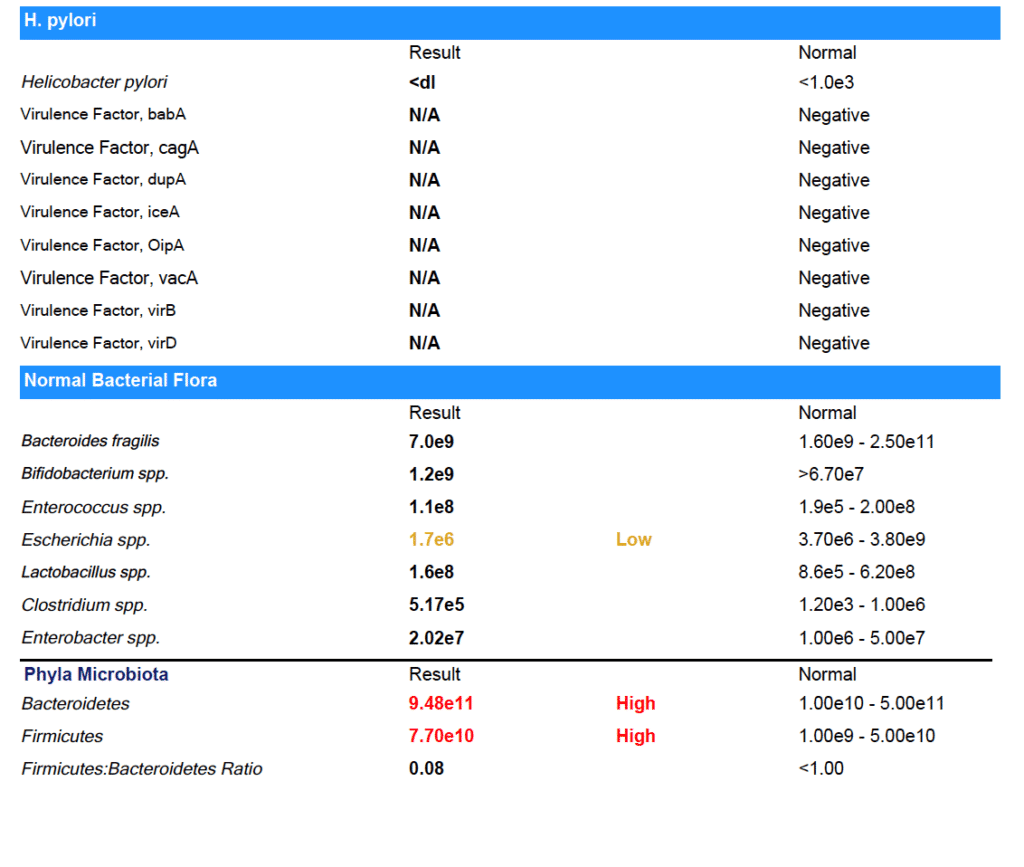
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
My Top Travel Tips for A Healthy Gut
Traveling is one of my biggest passions. When I got married, we chose to do a destination ceremony and reception with all of our friends and family in Sayulita, Mexico, instead of a traditional wedding (no regrets there!).
Traveling hasn’t always been fun for me, though. When I was younger, I felt like EVERY time I traveled, I got sick. And I’m not talking about a cold, folks - I’m talking about the nemesis of every globetrotter: traveler’s diarrhea.
Traveler’s diarrhea, Montezuma’s revenge, Delhi/Bali belly - it’s all caused by food poisoning. And while it will definitely ruin your trip, it also has a more sinister side - food poisoning can cause lasting damage to your digestive system leading to a lifetime of #gutproblems.
Want to know how food poisoning can cause long-term digestive issues - and what I do to avoid traveler’s diarrhea (even in the most exotic locales!)? Keep reading!
(Not interested in the science? Skip here for my travel tips).
How Food Poisoning Can Wreck Your Gut Long Term
I can’t tell you how many patient in my clinic can trace their digestive symptoms back to a case of food poisoning. And the science backs them up! Food poisoning is a known cause of irritable Bowel Syndrome (IBS). IBS after food poisoning is called “post-infectious IBS.”
But this gets a little complex, so bear with me here...
IBS isn’t a disease - it’s a syndrome. That means it’s just a name for a group of symptoms (fun stuff like gas, bloating, diarrhea, constipation, and food intolerances). IBS is a diagnosis of exclusion, meaning your doctor will call your symptoms IBS when they can’t find any other cause for them.
For many people - perhaps as much as 60% - the actual cause of IBS symptoms is something called Small Intestine Bacterial Overgrowth (SIBO). SIBO occurs when bacteria that should be confined to the large intestine migrates up and into the small intestine. A healthy small intestine should have very little bacteria in it!
So how does bacteria get from the large intestine to the small to cause SIBO?
It’s usually do to a problem with the Migrating Motor Complex (MMC). The MMC is what creates movement in your intestines - called peristalsis - and moves food from your stomach down through your intestines and eventually out of your body.
So what can harm your MMC? The most common causes are chronic viruses like Lyme disease, structural abnormalities, high stress levels, and… food poisoning!
Stay with me here - food poisoning can cause your Migrating Motor Complex to malfunction. When the MMC malfunctions, bacteria can move from the large to small intestine and overgrow, causing SIBO - and SIBO is the cause for as much as 60% of IBS!
As you can see, it’s a complex chain of events - and that’s why for years doctors have missed the connection between IBS, SIBO, and food poisoning. Luckily they are catching up now.
Toxins & Autoimmune Responses
So how exactly does the food poisoning cause damage to the Migrating Motor Complex?
Common food poisoning bacterias like E. coli, salmonella, Campylobacter jejuni, and Shigella all produce a toxin called cytolethal distending toxin B. It sounds bad, doesn’t it?
Your body will start producing antibodies against the cytolethal distending toxin B. For some people, they’re able to fight it off over in a few days and move on without long-term problems, but for about 10% of us (raising my hand!) we can’t fight it off as quickly - and therefore we keep producing more and more antibodies.
These antibodies don’t just fight the cytolethal distending toxin B - they also reduce a kind of protein in our intestine called vinculin.
Vinculin is very important in the health of Migrating Motor Complex - vinculin is crucial for proper function of nerve cells in the gut that cause peristalsis. When the MMC isn’t functioning and movement of food through the gut is slowed down, bacteria can overgrow and cause SIBO - plus other symptoms like bloating and gas.
The good news is that your gut can recover vinculin over time. First, you need to heal the SIBO. But it’s also critically important that you don’t get food poisoning again. So if you already have some gut issues, don’t stop reading now!
Here’s What I Do To Avoid Traveler’s Diarrhea
The key to avoiding traveler’s diarrhea is being proactive - think about where you’re going, research, and prepare! There are supplements I take to prevent illness, supplements I bring with me for defense in case I start feeling sick, and hygiene practices I follow, too.
Supplements I Use When Traveling To Keep My Gut Happy
When I’m travelling, I always take a probiotic. My favorites are Floramyces (which contains the yeast Saccharomyces boulardii) or UltraFlora Acute Care (this one blends S. boulardii with Bifidobacterium and Lactobacillus). I take 1 capsule of either, 1-2 times daily.
I also take Biocidin Advanced Formula Liquid to help boost my immunity. I start with 3 drops per day and work up to 5-10 drops twice daily.
Finally, I always take an Adaptogen blend. Adaptogens are herbs that help mitigate the stress of traveling. Yes, traveling is fun - but it is also hard on our bodies! Moving through time zones, awkward sleep schedules, and even just enjoying all the “newness” are all registered as stress to our bodies. I like blends that contain herbs like rhodiola for emotional and mental stress and eleuthero for physical stamina. NanoMojo Liquid and HPA Axis Homeostasis are my two go-tos.
Don’t Eat That!
Hygiene practices are so important for avoiding traveler’s diarrhea.
I always carry hand sanitizer with me - but not the conventional kind! Commercial hand sanitizers are full of BPA and other chemicals. Instead I make my own from aloe vera gel with lavender and tea tree essential oils, plus some Silvercillin. If you don’t want to make your own, this is good alternative. And of course - wash your hands with hot soap and water whenever you can.
Only drink bottled water - and never get ice! (Yes, even on the plane and in fancy restaurants!)
Avoid salad and uncooked veggies - especially lettuce. Cooked veggies (and cooked, hot food in general) are better when traveling. Worried about missing your greens? I bring a greens powder with me and mix it with bottled water. This one is my favorite.
Make sure you wash any produce you buy. As tempting as it is, don’t eat fruit straight from the farmer’s market cart. Wash it with a non-toxic fruit and veggie disinfectant first!
When eating out, look for food carts and restaurants with long line and plenty of locals.
Do This If You Feel Something Coming On
The minute I start to feel “off” - fatigued, grumbling stomach, or even a headache - I switch from my prevention to my treatment protocol.
I up the Biocidin Liquid to 10 drops, 3x per day.
I double up the probiotic.
I add in Oregano Oil Gelcaps for several days - 2 caps 3x daily.
And if diarrhea strikes? I go to a classic Chinese remedy called Huang Lian Su. It’s a blend of berberine-containing herbs that always works for me. I use 4-5 tablets, 3-4 times daily.
Happy Trails To You!
I hope these suggestions helps ease your fears about traveler’s diarrhea - and allow you to travel the world without getting sick!
And if you think food poisoning is at the root of your SIBO or gut problems, I hope you’ll consider working one-on-one with me to get it resolved. There is hope for overcoming gut problems - even one you’ve had for years! You can book a free consult with my team anytime. We’d love to help you!
4 Crucial Steps for Mealtime that can make-or-break your digestion
When it comes to healing digestive issues, it’s certainly true that we need to test to identify and then treat any infections or dysbiosis that may be contributing.
But just as importantly, we need to optimize the environment of the gut. In order to develop infections or overgrowths, the environment has to be right. Otherwise, our healthy gut terrain is inhospitable to the “bad guys”, and nurturing to the “good guys”.
This mainly involves things like optimal digestive secretions (like stomach acid and pancreatic digestive enzymes) that set the pH and fully digest our food. This ensures that we both assimilate the nutrients contained in what we eat, but also prevents other organisms, like bacteria and yeast, from eating it instead.
Other secretions, like bile from our liver/gall bladder, are also super essential. Bile digests fat, but also is a powerful antimicrobial, and regulates the motility of our intestines.
Of all the digestive secretions, Stomach Acid might be the most important when it comes to resilience against infections. Stomach acid (called Hydrochloric Acid, or HCL) is like your first line of defense.
You may know that stomach acid’s main role is to break down the proteins we eat, so that we can absorb the smaller amino acid building blocks to use as nutrition.
But stomach acid is also antibacterial to undesirable strains because of the low pH environment that it creates.
Keeping food in the stomach long enough is critical for the action of stomach acid to control the populations infused into lower regions with each pulsatile release of chyme. This is because food needs to be exposed to stomach acid (HCL) long enough to kill bad bacteria, preventing them from proceeding on into the small intestine.
So, if you have super-rapid motility (this is common in people who have chronic diarrhea), your food may pass too quickly through the stomach and into the intestines, and not have enough exposure to HCL. This equals increased risk of infections, in addition to not enough nutrient digestion.
Due to…
- Stress
- Nutrient deficiencies
- Modern diet and lifestyle
- And even just natural aging!
it’s unfortunately very common for people to produce less than optimal amounts of stomach acid to meet the demands of food intake.
And…..we need enough HCL present to keep the stomach pH below 4 for the entire time the food we are digesting in the stomach. If this doesn’t happen…pathogenic microbes pass unharmed into the intestines where they can take residence! (hello SIBO and parasites!)
Here’s the most important thing I want you to learn today:
HOW we eat our meals is one of the most important factors in optimizing gut environment.
Just becoming aware of HOW we eat, is one of the biggest things you can do to change what is happening with your digestive secretions, and therefore, with your microbiome.
Chewing: Why is chewing your food so important in regards to this?
Yes, chewing breaks your food down into smaller pieces, increasing the surface area, so that digestive secretions in the stomach and small intestines (like pancreatic enzymes, bile, and stomach acid) can further break them down.
But….there are other not so obvious reasons!
Chewing exposes foods to enzymes in the saliva that break down the cell walls of gram positive bacteria, causing them to die.
This means that chewing adequately is really our first weapon against pathogens that might be entering with our food!
Being relaxed while eating: Stress is a big factor that leaves us more prone to getting opportunistic gut infections, because stress shuts down our digestive secretions.
When our brain thinks we need to run from the proverbial tiger, it focuses our body’s energy and attention on surviving NOW, and diverts it from activities that are about long term survival, like digesting our nutrients.
Stress also spikes our cortisol, and this suppresses our gut’s immune system big-time--for much the same reason. And the hormone that our brain uses to signal the adrenal glands to make more cortisol, CRH, can promote leaky gut.
Healthy Meal Hygiene for Healthy Gut Environment:
1) Focus on creating a state of overall calm before, during and after eating to encourage stomach acid and digestive enzyme secretion.
2) Chew adequately—more than you think….keep chewing!-- to reduce particle size and mix enzymes in the saliva.
3) Include balanced fats, carbohydrates and proteins in each meal to encourage food to stay in the stomach long enough.
4) Planning enough time for meals—not eating on the run—is critical, to help allow for parasympathetic (rest-and-digest) nervous system activity. This allows for proper secretion of digestive fluids. Otherwise, if our body thinks we are running from the hypothetical tiger, there’s no digestion being emphasized, and no secretions being made—“Ain’t nobody got time for that”!
Have any questions or comments on this?
Pop on over to my facebook page and ask me anything!
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
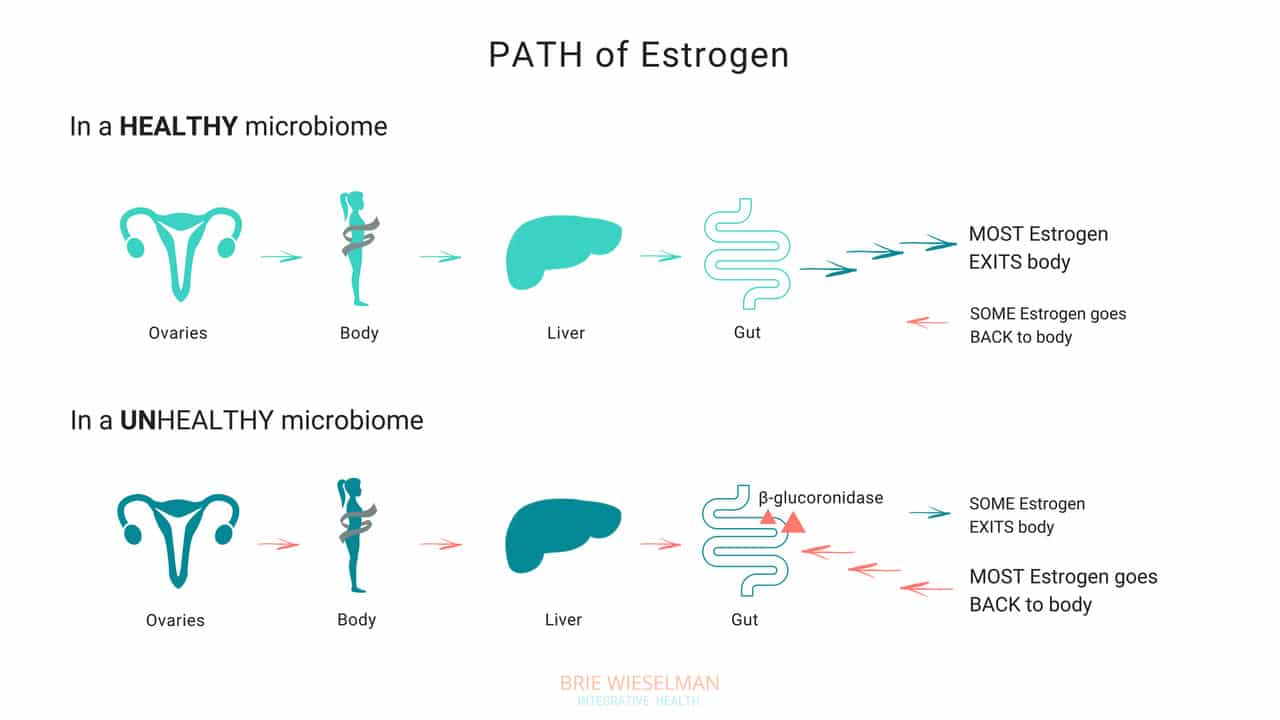
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
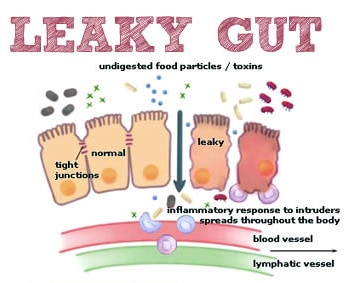
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.
Acid Reflux and Chronic Urinary Tract Infection; Totally 'Unrelated' Symptoms With the Same Root Cause?
One of the principles of Functional Medicine is finding and treating the “root cause.”
But sometimes, it isn’t as simple as finding one root cause and getting rid of it. Most of my clients have multiple health concerns - and multiple causes behind them. Helping them is about peeling back the layers and addressing each one as we go.
For my client Jane, peeling back the layers was exactly what we needed to do! She came in because she was experiencing tightness in her chest caused by acid reflux - and we wound up working through multiple gut infections, addressing vaginal dryness, and putting interstitial cystitis (a condition that causes chronic bladder pain like a urinary tract infection) into remission.
Every time we treated another “layer” Jane felt better than before.
Today, Jane wants to share her story in her own words. If you’re considering pursuing help with a Functional Medicine Practitioner like me, I hope this story helps you better understand the process of working with a practitioner.
Jane’s Story
About three years ago, I started dealing with some bloating. Then, I’d occasionally have constipation - not all the time, but enough that I noticed it. I had a colonoscopy and the results came back normal. I started taking a probiotic. The bloating and constipation just became kind of a general annoyance I was living with.
But then I started feeling tightness and pain in my chest. That was really scary. I went to the doctor right away, but the tightness and pain weren’t heart-related. That’s when I realized they were actually a digestive issue. I decided to go see a physician at my regular clinic, and they told me it was acid reflux, prescribed Prilosec, and referred me to a GI doctor.
Luckily I had read enough about Prilosec to know I didn’t want to take a proton-pump inhibitor. Instead, I decided to get a second opinion from a Functional Medicine Practitioner - that was Brie.
Working With Brie
From the start, Brie was very thorough. She took a really detailed history that helped me connect some dots about what had started all my digestive symptoms in the first place. The past summer, I’d had a urinary tract infection and taken a course of antibiotics. Then in the fall, I went traveled out of the country and had to take a course of the antibiotic Cipro for traveler’s diarrhea. That's when the bloating and constipation became worse and the other acid reflux symptoms started.
But she wasn’t just interested in the acid reflux - Brie asked questions about my overall health. When I told her I was experiencing vaginal dryness, urinary pain, and low libidio, she took me seriously. My doctor had diagnosed my with interstitial cystitis - basically pain in my reproductive organs for no reason.
Brie explained to me how the antibiotics had killed the good bacteria in my gut as well as the bad. She recommended stool testing and a breath test for Small Intestine Bacterial Overgrowth (SIBO), as well as hormone testing. She also recommended I cut out dairy and gluten temporarily to give my system a break, since those foods are common gut irritants. She also recommended some supplement that would soothe my gut and help with symptoms until we got the test results back. All this happened at our very first meeting!
The Test Results Came In
The test results came back a few weeks later - they showed low cortisol, low estrogen, H. pylori, low beneficial flora, and a few overgrown bacteria (citrobacter, pseudomonas). Plus, I had both methane and hydrogen type SIBO and was under-producing pancreatic enzymes.
It was a lot to take in and I was so glad I had Brie to help me understand what the results meant. She saw how everything was connected.
Brie explained that the H. pylori infection was likely causing the acid reflux, and that the SIBO was probably the cause of the constipation and the uti bloating. My hormone problems were tied in to all of it and causing the vaginal dryness, urinary pain, and low sex drive.
It was a relief to know there was a reason I was feeling the way I was feeling - especially because my symptoms had gone into a flare as we waited for the test results. I remember going to visit a friend for a few days and having to come home early because I was just so uncomfortable.
Brie started my on a supplement protocol for 6-8 weeks for both the H. pylori and the SIBO. I kept avoiding gluten & dairy, too.
After I finished the first supplement protocol, we re-tested. The H. pylori was gone! The SIBO levels had come down, but it wasn’t completely gone. On the second stool test, I also had positive results for some other common gut infections and parasites, including candida overgrowth. Brie explained that all of this was normal - the first protocol of supplements had helped destroy the “biofilm” - the protective cover the bad bacteria use to protect themselves and hide. With the biofilm gone now, we could see other parasites and better treat the SIBO, too.
By, then my acid reflux was totally gone and I was feeling pretty good gut-wise. But I was still struggling with the vaginal dryness and hormone symptoms. And, what I initially thought was a bladder infection turned out to be Interstitial Cystitis. The “UTI” pain didn’t respond to normal treatments, and the pain turned chronic. Can a UTI cause bloating and constipation?
Putting Interstitial Cystitis Into Remission
My hormone symptoms were slowly improving as my gut healed - but Brie also suggested using a plant-based bioidentical estrogen replacement. She also had me use vaginal DHEA, a vaginal probiotic, and some herbs. Those helped me feel better right away.
Brie also explained that two of the bad bacteria that the tests had shown were overgrown in my gut - proteus and citrobacter - were related to the Interstitial Cystitis, too. As we treated those, my symptoms disappeared completely.
Brie suggested I work with a pelvic floor therapist, too. That helped me relax some overly tight muscles that were contributing to the pain.
Changing My Diet
Brie suggested I follow a gluten and dairy-free, low-FODMAP diet. It helped me a lot in the beginning, but I was anxious to reintroduce more foods as soon as I could.
After a few months, I was able to reintroduce beans and some other legumes, which I hadn’t been able to tolerate for years, and I really missed. I am now back to eating all fruits and veggies, and I can even add in a little gluten here and there. That makes me feel good!
Where I Am Now
After working with Brie, I feel great for the first time in years.
I came to see her because of the acid reflux - but she opened my eyes to a lot of problems I had been writing off as “normal” or just “part of getting older.”
Gut-wise, I am feeling so much better now! After having given up gluten and dairy for years, I’m finally able to experiment with adding them back into my diet again now.
The interstitial cystitis pain is gone now, too. I didn’t realize how much the pain held me back from enjoying life - I even cancelled an overseas trip because of it!
I’m so happy to be where I am now with my health. I’m following a maintenance protocol now and continuing to meet with Brie occasionally to make sure I’m doing the right things moving forward.
Working with Brie has made a huge difference for me, and I wish more people could have access to it! I hope my story helps to spread the word.
Do You Need Help, Too?
Jane had amazing success - she cleared multiple gut parasites, fixed her digestion, reversed interstitial cystitis, and was even able to reintroduce foods she hadn’t eaten in years.
Why was she so successful? Because she dedicated herself to working through the process of Functional Medicine. She didn’t give up even when it got complicated - and neither did I!
I hope reading Jane’s story has helped you understand better understand the process of working with a Functional Medicine Practitioner like me.
If you’re inspired and ready to start your own journey, you can book a free, no-obligation Prospective Patient Interview with my team. During this 20-minute appointment, we’ll learn about you and discover if you’re a good fit for working with us.
Recipe: The Best Waffles in the World! (Cassava Flour Waffles)
A large percentage of my patients have SIBO and are on Low Fodmap diets, are on a version of AIP (Autoimmune Paleo), or a paleo diet. So I’m always looking for safe starches to include to ensure proper carbohydrate intake and to act as food for their good gut bugs. Squashes, sweet potatoes, and root veggies make up a good amount of the carb sources in my diet as well as many of my clients.
But once in a while, I want something with that perfect amount of CRUNCH.
Something that you can slather with grass-fed butter when you need some comfort food from childhood....
Growing up, my house was a waffle house, at least on some weekends. Now, since we have (mostly) eliminated grains in our house, bread-like things happen less frequently, and waffles were unheard of.
But then I fell in love with Cassava.
Many of you know next to practicing Functional Medicine, my biggest passion is dancing, specifically dances of the African and afro-brazilian diaspora. On my last trip to Brazil, I realized how many things are made with cassava/tapioca, and also how absolutely delicious it is! Besides frying the chunked root, it is made into cakes, mashed, and (my personal favorite) miniature cheese-bread rolls called “pao de quiejo” (cheese bread).
Cassava (also known as yuca) is a starchy tuber, and is a staple for millions of people in South America, Asia, and parts of Africa. This plant can be processed into both tapioca starch as well as cassava flour (which maintains the fiber content), each of which have slightly different properties when it comes to using them in cooking and baking.
And, it can be used to make, hands down, the best waffles in the world.
I made these at a birthday breakfast for my extended family recently, and no one could believe they were grain-free. Even the pickiest eaters downed at least 2
Cassava is naturally gluten, grain, and nut-free, and is also low FODMAP. But somehow, it’s a pretty close replacement for wheat flour in terms of texture, and can be used as a replacement in most recipes 1:1.
One thing to note before going on a cassava binge: it is very high in carbohydrate per gram, compared to other roots like sweet potatoes or beets. This can lead to glucose/insulin spikes in those who are sensitive, or if you eat too much. If you’re on a low carb diet, or have diabetes or other blood-sugar issues, avoid cassava, or save it for the occasional treat.

The only brand I use is Ottos Naturals, as I’ve heard of other people having less-than-stellar results with other brands. There are tons of great recipes out there for tortillas, breads, naan and other treats out there in the inter-webs if you do a quick google search. But this waffle recipe takes the cake, IMHO! (Credit to Laura Franklin of Fresh & Frank)
Crispy Cassava Blender Waffles
Makes about 10 standard square waffles
Ingredients
1 cup Otto’s Cassava Flour
1/2 tsp Himalayan salt
2 tsp baking powder
1/2 tsp cinnamon
1 ripe banana
2 organic eggs
1-2 tsp real vanilla extract
2 Tbsp organic virgin unrefined coconut oil
1.5 cups coconut or almond milk
Directions
1. Preheat waffle iron.
2. Throw all ingreidnets into blender.
3. Blend all for about 30 seconds to 1 minute.
4. Check batter; if it seems too thick still, add a splash more almond/coconut milk or water. You want it thick but still able to pour.
5. Pour onto waffle iron. Depending on the integrity of your waffle iron, you may need to cook these twice to make sure the inside cooks through.
6. Remove when crispy and golden brown on the outside. (I know it’s hard to wait, but don’t remove too early!) Top with desired ingredients.
Waffles freeze well and can be thrown directly in the toaster to crisp up!
Recipe: Grandma Fleischer’s Chopped Liver
Liver.
You either love it or you hate it. Or you're too scared to find out.
If you ask someone who grew up in a family where you regularly ate liver, or other organ meats, they'll inevitably grin with deliciousness. But for those of us who didn't dish up liver and onions regularly, the idea can be a bit foreign.
Given the opportunity, most little kids that get introduced at an early age actually LOVE liver.
Personally, I grew up on the east coast, near lots of kosher delis, and ate my fair share of chopped liver. I remember being held in my grandfather's arms, at the fridge, eating it on a spoon out of a deli container and begging for more. Somewhere in my later childhood years, it stopped being something we had around, and by the time I was 23, (after a 15 year stint as a vegetarian), you couldn't pay me to touch the stuff.
A few years ago, with the bone-broth-slurping, organ-meat-eating trends that came with the advent of the Paleo movement, I started really looking at nutritional content of organ meats. Bite for bite, liver holds it's own against virtually anything you can call food, when it comes to nutrient content. Liver is particularly high in Vitamins A, C, Biotin, Folate, and B12, as compared to other foods that are considered to be good sources of these nutrients. In Chinese medical nutrition, liver has been touted for centuries as the best "blood builder" and fertility food-- and indeed, with high levels of iron, folate and b12, it's a sure fire way to help alleviate anemia.
Armed with this knowledge, I was determined to re-learn to eat liver.
If my 3-year-old self could do it, so could my 38-year old self!
Now I learn a lot from my patients. And on my mission to love liver, it was one of my long time patients, Adam, who came to my rescue. After a discussion about this in my office, about once a month or so, Adam brings me a little glass jar with his grandma's chopped liver, and some celery sticks or Mary's Crackers.
And as I sit and munch, it's like I'm 4 all over again....
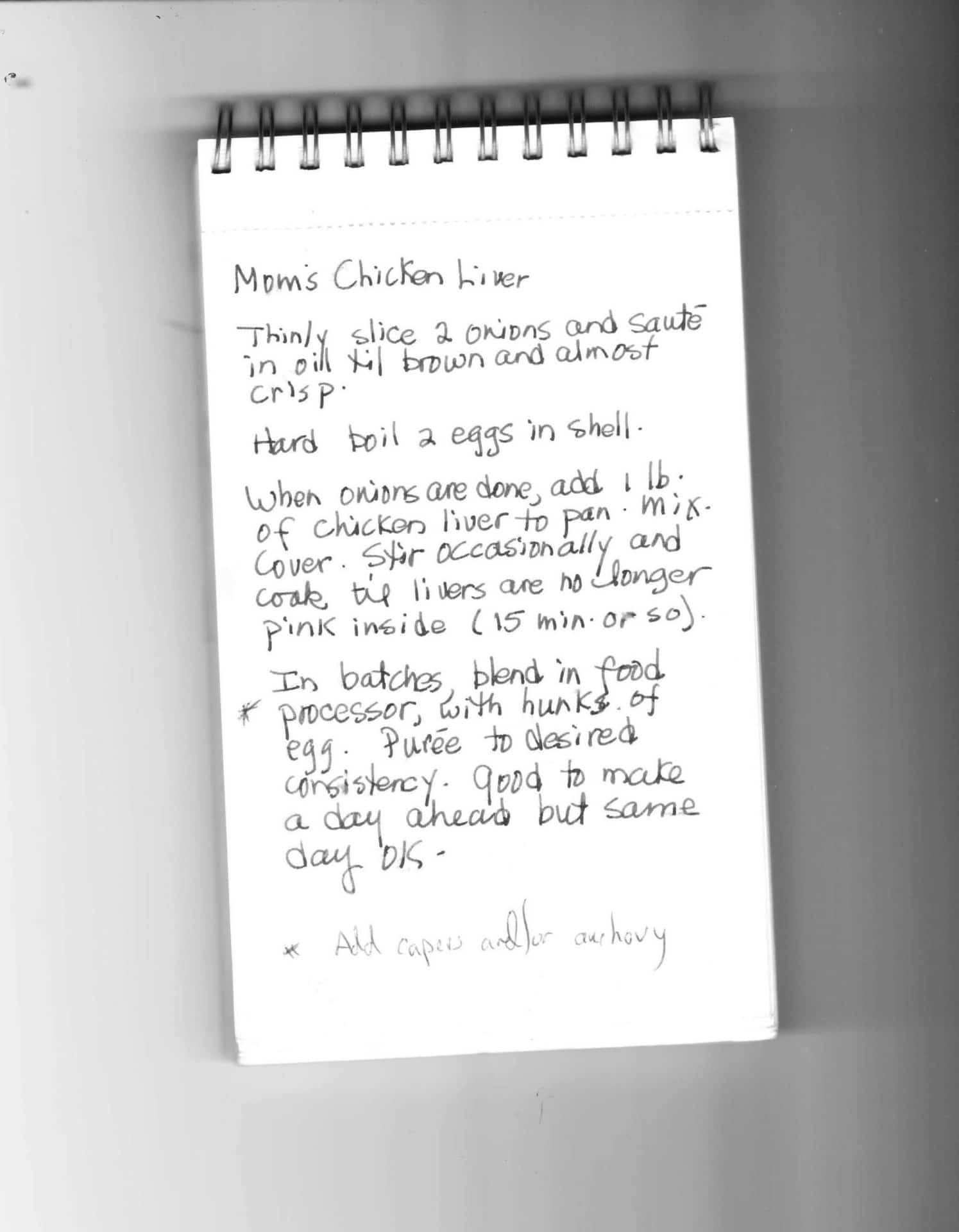
Grandma Fleischer’s Chopped Liver
(With huge gratitude to Adam F)
Ingredients
1 Lb Pasture Raised/Organic Chicken Livers
2 Yellow Onions
2 Eggs, hard boiled
Salt
Pepper
Optional: 2-4 slices of Bacon, Anchovies and/or Capers
- Thinly slice 2 onions and sautée in oil until caramelized brown and almost crisp. Be sure to salt and pepper liberally as you sautée. You can use avocado oil or grass-fed butter for sautéeing, or you can start with 2-4 chopped up pieces of bacon in the pan, and then use that fat to sautée the onions. Cooking time for the onions is 10-20-mins.
- When the onions are done, add 1 LB of chicken livers to the pan, salt and pepper again. Cook 8-12 minutes, on medium (not high) heat, turning or stirring every few minutes (but not too much stirring).
- Very important! DO NOT OVERCOOK THE LIVER--The livers should still have a little pink in the centers when done.
- In batches, remove livers and onions from the pan and transfer to a food processor with chunks of the hard boiled egg. Puree until it reaches the desired consistency. For an added kick, toss in a handful or two of capers and/or some small anchovy fillets. It just takes a few pulses in the food processor, don’t overdo it.
Serve with celery sticks, crackers, or other veggies and enjoy. This is best prepared a day in advance and then served the next day, but is still delicious when made the day of!
Top 3 Uses for This Amazing Probiotic Yeast
In the world of natural health, yeasts get a bad rap. But one of my favorite probiotics, Saccharomyces boulardii, is actually a beneficial medicinal yeast!
Commonly referred to as S. Boulardii, it was originally found on lychee fruit in the 1920s. When taken as an oral supplement, it colonizes the gut within three days. But the colonization is temporary—S. Boulardii disappears from stool within five days of discontinuing supplementation. Interestingly, the health benefits that it provides last beyond the time of oral consumption—which means that, like most other probiotic supplements—the benefits are not due to the probiotic strains taking root and colonizing.
Used for prevention and treatment of diarrhea
Many types of diarrhea are caused by dysbiosis (bad organisms living in the gut). When this occurs, the healthy microbial population takes a significant nose dive--especially important species like Bacteriodies, Ruminococus and Prevotella.
At the same time, the gap formed by the notable decrease in these beneficial bacteria, creates a void-like vulnerability that allows for increases in opportunistic bacteria like Enterobacter and less desirable Clostridia strains—these are aptly referred to as “pioneer bacteria” because they migrate to an area when there is an opportunity!
In this situation, Saccharomyces Boulardii has been shown to help in several ways:
- S Boulardii actually helps to bind pathogenic bacteria and carry them out of the digestive tract, especially Staphylococcus aureus, Klebsiella, Candida, and Salmonella
- Several human studies have demonstrated that S boulardii supplementation leads to faster re-establishment of a healthy microbiome, when recovering from infectious diarrhea.
- It increases the population of specific types of bacteria that are known to produce short chain fatty acids (SCFAs) by fermenting dietary fibers (prebiotics) and resistant starch. SCFAs are the energy substrate of cells in the gut lining that allow it to constantly heal and regenerate, preventing Leaky Gut. They also directly support some of the commensal (or good) bacteria as well.
S Boulardii is most notably useful in infectious Clostridium difficile infection. Clostridium Difficile (also called “C Diff”) is the primary cause of acute diarrhea after antibiotics, and it not an infection to take lightly. In extreme cases, it can even be life threatening. When 124 patients on high dose vancomycin (an antibiotic) for C. difficile related colitis were given S. boulardii, rates of recurrence plummeted from 50% to 16.7%.
But bacteria are not the only micro-organisms that can cause diarrhea. Overgrowth of yeasts like Candida Albicans can also induce diarrhea by causing inflammation of the gut lining. S boulardii has been shown to decrease tissue inflammation in the gut caused by colitis from Candida overgrowth, alleviating diarrhea from this cause.
Disrupts candida colonization in vaginal and other tissues
Candida albicans is the most common opportunistic fungal pathogen found in the human body. It has many tools at its disposal that allow it to thrive and take root; the ability to adhere to tissues and even penetrate them, biofilm formation and the ability to transformation into different forms at various stages of its life cycle.
In order to get an overgrowth in the first place, adherence is the first necessary step. Candida albicans is capable of adhering to the inside of cheeks, labia, vaginal and intestinal epithelial cells, as well as catheters, dental implants or artificial joints.
Not only has it been shown to interrupt Candida’s adherence, but S. boulardii is uniquely able to stimulate Secretory IgA (SIgA), our first line of defense against invading microbes. SIgA is essential to maintaining intestinal mucosal integrity, preventing leaky gut, and ensuring a stable, diverse microbiome—which is key to bulletproofing your gut. This is the main immune agent found in mucous membranes, saliva, tears and vaginal secretions, as its main function is to help protect you against pathogens.
Prevention
Perhaps the best use of S Boulardii is prophylactically.
With Antibiotic use: Since it yeast are not killed by antibiotics (only bacteria are susceptible to antibiotic drugs) you can (and should) take S boulardii during antibiotic therapy to prevent Candida overgrowth and other diarrhea-inducing opportunistic pathogens. Several studies have demonstrated that in patients with known H. pylori infection, S Boulardii supplementation improved eradication rates and reduced treatment-related side effects.
You can also take it before, during, and after travelling—it helps prevent traveler’s diarrhea! Meta-analysis of probiotics used preventatively for travelers diarrhea all showed significant reduction in the risk of traveler’s diarrhea when probiotics are used—but two randomized control trials showed a significant reduction in traveler’s diarrhea in the S. boulardii group compared with other types of probiotics used as controls.
For this particular purpose, I suggest 1000 mg daily. Should you get sick while travelling, you can continue to take it during traveler’s diarrhea, or ongoing diarrhea, to shorten the duration and promote recovery.
A word of caution
S Boulardii has been shown in studies to be helpful helping improve symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome. For example, in a 6-month study of patients with Chrons Disease, the relapse rate was significantly lower in patients treated with mesalazine plus S. boulardii (6%) than in those treated with mesalazine alone (38%).
That said, in my clinical experience, people with Inflammatory bowel disease should proceed with caution, when initially introducing S boulardii. The reason for this Anti-Saccharomyces cerevisiae antibodies (ASCA) have been associated with Crohn's disease (CD). Saccharomyces Cervisiae (Brewer’s/Bakers yeast)—used in baking as well as in brewing beer and wine—is similar enough to Saccharomyces Boulardii that the immune systems of sensitive individuals can cross react, potentially triggering a symptom flare. If any flare in symptoms is noted with oral consumption, discontinue use. Like other probiotics, S boulardii is also not appropriate in severely immunocompromised individuals.
To buy Saccharomyces Boulardii, click here!
Have you ever used this probiotic yeast for your gut health? What was your experience?
All About Food Sensitivities - New Cutting Edge Test Available! (KMBO FIT Test)
One of the primary tenants of Functional Medicine is to identify triggers for inflammation and reduce exposure. Sometimes, this looks like parasites or yeast overgrowth, sometimes it looks like an imbalance in amounts of Omega 6 to Omega 3 in the diet. And other times, this has to do with otherwise healthy, everyday foods that we eat, that simply aren’t a good fit for us at the time.
In theory, this should be simple. But historically, identifying food sensitivities accurately has been a challenge. Hundreds of tests exist for evaluating your immune systems reactions to food. But it has been shown time and time again that many of these tests are inaccurate, either under diagnosing, or over-reporting sensitive foods.
This makes it really difficult to know what to eat and what to leave behind. When a client’s test comes back with 30 reactive foods, it just leads to overwhelm for both the patient and the practitioner.
If your immune system is our planet, then your gut is like the water. Everything that you feed or put into the water is going to circulate, universally, affecting everything else on that planet. The air, the soil, the vitality of anything that grows. Knowing the foods that trigger decay and disease on your planet is essential to the overall health and vibrancy of your body.
You have far greater quantities of gut immune molecules, than you do in the entire rest of your body. Your gut immunity “scans” more in one day than is scanned by the systemic immune system in a lifetime!! Gut issues are so important to overall health, for this reason.
The truth is that food sensitivities are an underlying problem for every condition that I see.
And I mean everything:
- Arthritis
- Weight Gain
- Insulin Resistance
- Eczema, acne, and other skin conditions
- Fatigue
- Reproductive Hormone imbalance (PMS, PCOS, Menopausal symptoms)
- Infertility or recurrent miscarriage
- Autoimmunity of any kind
- Thyroid imbalances
- Adrenal issues
- Migraines
- Digestive issues ranging from IBS to Chrons or Ulcerative Colitis
- Depression, anxiety, insomnia, and brain fog
- and even addiction
Basically, any health concern where having increased inflammation would worsen symptoms or the disease process, can be worsened by exposure to foods that trigger your immune system. And inflammation is the bottom line in the vast majority of illness!
Even without illness or symptoms, anyone looking to live a long healthy life should run this panel, to prevent the development health issues later! I’m so excited to announce that it’s never been an easier or more reliable process to learn which foods are triggers for YOU! The FIT (Food Inflammation Test) by KMBO Diagnostics is cutting-edge lab testing that provides anyone who wants to rid their body of inflammation the information they need to avoid the foods that cause it! (***cut here for email, “read more”)
So, if it’s not an “allergy” what exactly is Food Intolerance or Sensitivity?
Hold up—let’s break this down a bit.
A whopping 85-90{0ace9f30246476cbe34912402cc70dd667071e9efa13e47cc458477e17894418} of our total immunity resides in the gut. There are several potential ways that you can have an immune reaction to a food. When we talk about Food “Allergy” and Food “Intolerances” or “Sensitivities”, these are very different things.
Our immune system is our bodyguard, working to protect us from “invaders” (like viruses and bacteria) that can cause us harm, 24/7. It works by tagging identifying proteins on the surface of the “invader” to mark it as a “bad guy” that should be attacked and eliminated.
Most of the time, this helps us. However, our immune system can also tag pollens, mold, toxins or chemicals, and other things we are exposed to. In the case of food allergies and sensitivities, a specific type of immune compound overreacts to the presence of a protein marker on the surface of a food molecule. The type of reaction is determined ultimately by type of immune compound that is doing the attacking in each reaction.
In a true food allergy, an immune compound called Immunoglobulin E (IgE) over-reacts to a certain food and causes a reaction within minutes or seconds. You can think of immunoglobulins like soldiers enlisted in our own personal immune army. Substances like egg, corn, or apples are normally harmless or healthy, but if you have an allergy, your body sees the food as a threatening invader!
In mild reactions, we might get histamine-driven symptoms like sneezing, runny nose, or itching, like with seasonal allergies. In a more aggressive reaction, you can develop hives, swelling, and even go into anaphylactic shock, which can be life threatening.
IgG is another type of immunoglobulin. IgG is produced by cells in the gut, in response to protein markers on substances like foods and bacteria. While IgE causes reactions within minutes, IgG causes reactions in 2 hours to 4 days or more!
Unlike true food allergy (IgE), IgG reactions are responsible for most of the symptoms that we associate with being “intolerant” or “sensitive” to a food. While the symptoms from an IgG response typically won’t include risk of death, they can still be uncomfortable and dangerous. For this reason, food intolerances are often dismissed as less significant, but in truth they can have serious consequences, especially with regard to your long-term health!
Food Sensitivity, leaky gut, and symptoms outside of the gut:
Logically, food intolerances can cause digestive symptoms. But how do these reactions cause symptoms all over the body like headaches or acne? If you have some degree of Leaky Gut, your immune system can react to the given food protein, forming immune-antigen complexes. When food proteins get through the gut lining, (through structures known as “tight junctions” in the intestinal wall), the resulting inflammation and immune activation causes further break down of the gut barrier. This in turn causes more leaky gut, and allows more food proteins in, creating a vicious cycle or increasing gut permeability and worsening food intolerances.
The over-activated immune system attacks local sites in the gut, but can also circulate in your bloodstream to tissues in distant locations around the body, such as joints, skin, your thyroid, or neurological tissue. Virtually any tissue in the body can be effected.
IgG-mediated symptoms can show up from 4 hours to 4 days after exposure to the reactive food. Clearly, this makes it difficult to identify what food caused what symptom!
Enter the FIT test!
The KBMO Fit Test is a revolution in food sensitivity testing. Like its ancestors, it still tests for IgG reactions to 132 different foods.

So, what’s so different and great about this test?
The main advantage that the FIT test offers, is that it screens for IgG types 1-4 (most IgG testing only looks at 1-2 types), and more importantly, screens for something called “complement”. When it comes to generating inflammation, complement is even more important than the level of IgG response to a food.
Let’s say that the initial IgG reaction is like the fire alarm going off at the fire station, and the first responders showing up at the scene. Compliment is like the rest of the squad showing up to help handle the situation…..they show up a bit later, but often create much larger hubbub at the scene of the accident or fire. The alarm (IgG) had to sound in the first place, to trigger the chain of events, but the responding teams (complement) were really what caused the biggest stir in the end. Foods that activate compliment can cause both local and systemic destruction of tissue by increasing inflammation.
In other words, you might have 10 or more foods with a significant IgG reaction, but the ones with complement are the ones that are significant in terms of boosting your inflammatory response. Knowing this information confirms which foods are most important to eliminate, instead of having a list of 40 foods to avoid! No other food sensitivity test currently available screens for IgG 1-4 and complement levels.
But there’s more…how the FIT Test can confirm if you have leaky gut
The FIT test is also a test for leaky gut, so you don’t need second test! If you show up as having a positive Candida antibody, it doesn’t mean that you have candida overgrowth. Candida is present in everyone’s gut, in low levels. A positive reaction to candida means that it is getting through the gut barrier, where it can present to your immune system. This confirms the presence of a leaky gut. The higher the reaction level, generally the worse the leaky gut. Having a high number of food reactions show positive (20 or more) also suggests leaky gut.
The best part is that this test is a blood spot panel. This means that we can mail it to you to do in the comfort of your own home– no blood draw needed! Based on your results, we design a 6-12 week elimination of your trigger foods, and then a systematic reintroduction to check for reactions. In most cases, antibody production in response to a given food will decrease or be eliminated within that time. When that happens, you may be able to reintroduce the food again without symptoms.
8 Reasons Your SIBO Isn't Clearing
If you’re like most people, you probably felt a mixed sense of frustration and relief when you found out that you have Small Intestinal Bacterial Overgrowth (SIBO). Relief, because all of your symptoms finally made sense. Frustration, because you’d heard how difficult treating SIBO could be; diet changes, herbs, antibiotics, pro-kinetics. It’s a lot to learn about, let alone put into action!
You ran a breath test. You changed to a low FODMAP diet. You found a practitioner and took a protocol of herbs or supplements. All of this felt empowering, and, at first, your symptoms started to get noticeably better. In fact they may have even resolved for the first time in years! But, then things changed and those old familiar symptoms started to return….
When things don’t go as planned…
What is even more frustrating than finding out that you have SIBO, is when you complete the protocol…..and the bloating, discomfort, diarrhea, or constipation, come right back, despite your best efforts. It’s just not fair, right?
What is even more frustrating than finding out that you have SIBO, is when you complete the protocol…..and the bloating, discomfort, diarrhea, or constipation, come right back, despite your best efforts. It’s just not fair, right?
I’m doing everything right….so why won’t my SIBO go away?
There are a few main reasons why people repeatedly fail to resolve their SIBO, despite using appropriate treatment strategies:
-
Using the wrong cocktail of herbs and supplements
A quick Google search will produce dozens of herbs that have been used to treat SIBO. But knowing which herbs or supplements to use for which type of SIBO (methane or hydrogen dominant, or mixed), or what dosage is necessary, is not always obvious.
-
Not treating for long enough
Duration of treatment should be based on several factors. Most important is what levels of hydrogen and methane gasses were found on your lactulose breath test, prior to the 120-minute mark. Many practitioners will recommend a standard treatment length of 2-4 weeks. While this is adequate for some cases, more progressed cases may require 8-12 weeks of continuous treatment with antimicrobials.
-
Not including probiotics during treatment
Many people hesitate to include probiotics during treatment, thinking that they might make SIBO worse. This is especially understandable if you took a certain probiotic formula and immediately felt symptomatic. Yes, some strains (especially d-lactate forming ones like acidophilus), can aggravate pre-existing SIBO. But some strains of antibiotics are shown to be more effective at treating SIBO than prescription antibiotics! Stick to soil based organisms, spore based probiotics, or Bifidus strains to be safe.
-
Not considering prescription antibiotics
I get it. I’m a trained herbalist first, always. And that means that I am just as reluctant for you to use prescription drugs as you are. However, we learn in pharmacology training in medical school that everything is a toxin, taken in the right dose. That’s right; even water can be toxic if you drink too much of it. Every medical practitioner eventually thinks about something called the cost to benefit ratio– “does the benefit given by this treatment, in this situation, outweigh the risk of using (or not using) it?”. In the case of antibiotics used for SIBO–specifically Rifaxamin– the benefit almost always outweighs the cost.
Rifaxamin is an antibiotic with several unique properties. It is not absorbed into systemic circulation– meaning that it stays in the gut. You can’t, for example, use Rifaxamin, to treat an ear infection, because it would never get to the inner ear. Rifaxamin is largely inactive by the time it makes it through the small intestine and into the colon. This means that it doesn’t upset the beneficial flora in the large intestine, leaving our good bacteria intact.
In other words, Rifaxamin isn’t associated with many of the negative actions that are associated with antibiotics in general. It is only used for one thing, and it does that thing very well. Dr Mark Pimentel, associate professor of medicine at Cedars-Sinai Medical Center, and a leading researcher in the area of IBS and SIBO diagnosis and treatment, says that he sees Rifaxamin be effective in at least 70% of patients SIBO.
While it’s certainly not a magic bullet, it’s worth a second look, if you’ve written it off as a potential treatment option!
-
Underlying structural abnormalities
While this isn’t the most common reason, it does exist, and won’t show up on breath testing. Changes in the intestine (like strictures, a blind-loop resulting from a GI tract surgery, problems with the ileocecal valve, or other structural issues) provide an ideal environment for bacterial colonization and overgrowth. These cannot be detected by physical examination or on a breath test, and can only be seen on imaging studies like x-rays and MRIs.
-
Co-infections
“Hey, who invited that guy to the party?” Some people with SIBO either haven’t had their stool tested for parasites, or, have used panels that weren’t good enough to catch them. If you have one or more parasites living in your gut, you will generally not get a full response to your SIBO treatments until you have properly diagnosed and treated the parasitic infections.
Another common scenario is having a mixed pattern of candida or other fungal overgrowth alongside of SIBO. Some SIBO may in fact really be “SIFO”– small intestine fungal overgrowth. Although there is some overlap, fungal/yeast overgrowth tends to respond to different herbs and supplements than are used to treat bacterial overgrowth. Sometimes, people need to adjust the treatment approach to target both bacteria and yeast, in order to get full results.
-
The wrong diet at the wrong time
Eating low FODMAP can be a helpful way to manage symptoms. But eating low FODMAP, or too low-carb whiletreating with anti-microbial agents can actually be counter-productive!
Studies show that using Rifaxamin plus Partially Hydrolyzed Guar Gum (PHGG) is more effective at clearing SIBO than Rifaxamin used alone. PHGG is a pre-biotic, which means that it feeds bacteria. So you would think that it would worsen SIBO by feeding the bacteria in the small intestine. In fact, it does exactly this, except that feeding the bacteria while using an agent that targets them while they are reproducing, yields exactly the opposite effect– it kills them off in higher numbers.
In this way, prebiotics make the treatment work better. Feeding the bacteria (either with a prebiotic like PHGG, or with FODMAP foods, as tolerated) is generally a good idea while taking herbs or prescriptions to treat SIBO.
Cops & Robbers: Clearing SIBO isn’t all about “killing the bad guys”
Reason number 8 is its whole own section, because it is probably the most significant driving cause in your stubborn or recurrent SIBO. Many people, in fact many practitioners, are treating SIBO as if it’s a parasite. If your SIBO treatment only consists of using things to “kill the bad guys”, you’re missing the boat.
To see why this is true, we have to recognize that SIBO isn’t an infection that we “pick up” from somewhere out in the world, but rather a situation that arises because the terrain of the gut has changed so that it is now hospitable to bacteria. While we are supposed to house trillions of bacteria in the large intestine, the small intestine is supposed to be relatively sterile. There are several aspects of the “terrain” that need to be considered.
-
Digestive secretions
Pancreatic enzyme insufficiency, or inadequate stomach acid or bile production all set the stage for less-digested proteins, carbohydrates, and fats. This means less nutrition for you, but also means more fermentable matter for the bacteria causing the problem!
-
Motility and the MMC
People with SIBO have altered digestive motility. This can be either a cause or an effect of SIBO, depending on the individual case. Although most people with SIBO will have symptoms of diarrhea or constipation, the kind of motility that is most important when it comes to getting rid of SIBO, and keeping it gone, is the Migrating Motor Complex. The migrating motor complex is responsible for cleaning the small intestine, specifically between meals. It functions like house keeping, in order to sweep bacteria, and undigested carbohydrates and fibers that might feed bacteria, out of the small intestine and into the colon.
Re-establishing proper motility and MMC activity is critical to your recovery from SIBO, as well as for future prevention. There are many ways to encourage proper patterning of gut motility. Using prokinetic herbs or drugs is standard, but many therapies (like abdominal massage, acupuncture, and neurological chiropractic) can enhance the benefits.
The vagus nerve is the main player here, and we know that vagal tone can be disrupted by trauma and ongoing stress. While physiologic approaches (like probiotics, prokinetics, abdominal massage, acupuncture, gargling, or chanting) are helpful, sometimes it is more important to find ways to gently face into the underlying mind-body issue. Therapy, hypnosis, and MBSR can prove to be indispensable in these situations. Often times the experience of having SIBO can facilitate an opportunity for deeper exploration of what is living in our hearts, minds, and spirit that is unresolved.
-
Dysregulated cortisol levels and the Immune system
One of the main reasons SIBO can arise is if your digestive immunity is compromised. Around 86% of your total body immunity is located in the GI tract.
Anything that suppresses or alters this immune activity can leave you more vulnerable to fostering bacterial growth where it shouldn’t be–in your small intestine!
Adrenal fatigue (HPA-axis dysregulation) leads to imbalanced stress-hormone levels (cortisol). And having cortisol levels that are chronically either too high or too low can lead to reduced levels of immune secretions in the gut. They can also slow down repair of the tissues that make up our stomach and intestinal lining, leading to leaky gut.
You need to test, to know.
-
Sympathetic Dominance
If you are constantly in “fight-or-flight” (also known as sympathetic dominance), your gut is at a disadvantage. Chronic stress overstimulates the sympathetic branch of our nervous system (like the gas pedal), and suppresses the parasympathetic branch (like the breaks). We need both, in balance.
Sympathetic dominance is known to slow motility; digesting the nutrients you’ll need tomorrow simply isn’t a priority if you’re running to save your butt, NOW!, if you’re running from a wild boar. It also shuts down digestive secretions, and suppresses immune activity, while up-regulating inflammatory compounds. Not a good look.
Digestive-focused hypnosis, Heart-rate Variability training, and meditation techniques such as Mindfullness Based Stress Reduction are a great way to give input to the nervous system and retrain it to kick off it’s shoes and relax a little.
The factors leading to your SIBO were really the perfect storm. Addressing these issues can make or break the success of your treatment. To learn more about how to get rid of SIBO, please schedule an appointment, or, contact my office to set up a FREE 15-minute consultation.
I Had To Take Antibiotics...How Can I Protect My Gut?
Many of my patients are surprised to hear that I, too, grew up with the ubiquitous bottle of pink bubblegum flavored prescription syrup in the fridge each winter. Amoxicillin—it’s the go-to antibiotic of choice for everything from ear infections to strep throat or pneumonia in children everywhere. Trust me; I had my fair share! Back when I was growing up, we just didn’t understand the ramifications of repeat antibiotic use, so it seemed that one could rarely leave the pediatrician’s office without a prescription for one.
Antibiotics are only effective for bacterial infections, and won’t have any impact on viral infections such as the common cold. With the rise of antibiotic resistant infections, or so called “superbugs”, even the doctors prescribing these drugs have taken a muchmore judicious approach to using them. We now know that the risks of repeat antibiotic use during childhood are long-lasting and have been linked to increased risk of allergies, autoimmune diseases, diabetes, obesity and even ADHD later in life.
There are many situations where antibiotic use can be avoided. For instance, most urinary tract infections, ear infections, sore throats, and the weepiest of oozing red eyes can be treated safely and effectively by aggressively using the right herbs or natural treatments. —In fact, I’ve treated hundreds of these types of ailments in my own clinic with only natural medicines and have seen great success. . Even the dreaded diagnosis of “strep throat” can be treated with appropriate herbs by a trained professional. The overwhelming benefit of using a natural approach to these ailments is that the “good” bacteria in your gut stays protected. Additionally, you avoid the side effects that often come with antibiotic use, like bloating, diarrhea, constipation, fatigue, and loss of appetite.
Certainly, there are situations where antibiotics can be lifesaving–I personally owe my life to IV antibiotics used for a bad case of sepsis I experienced several years ago. And while ear infections and urinary tract infections almost never need to be treated with antibiotics, if you’re in pain, or have been up every night for a week with a sick, crying kid, and are at your wit’s end, you may wind up gladly accepting that prescription.
In cases of bacterial infection, antibiotics will do the job, but not without massive casualties among the beneficial flora in the gut that form our defense system.
Our digestive tract houses around 500 species and up to five pounds of bacteria that help preserve our health every day. We have trillions of bacteria populating our large intestines—in fact, their cells out-number our human cells; one could say that we are “more bacterial” than human. These tiny organisms are so critical to our survival, it’s like having another essential organ that you couldn’t live without! Beneficial (or probiotic) bacteria in our guts play a host of vital roles for our health:
Nutrition:
Intestinal bacteria actually synthesize essential nutrients like B12 and K2, or convert them from the food we eat into active forms. In fact, while we get some of our vitamin K2 from eating dark leafy veggies, up to 75% of it is made in the gut.
Studies have recently shown that some gut bacteria are able to produce the active methylated form of Folate (5-MTHF), a key component in things like brain function and mental health, cell division and DNA replication, and normal fetal development during pregnancy. Having adequate amounts of the right type of good bacteria can be a game changer for individuals with MTHFR mutations, who are notoriously at a disadvantage in producing adequate quantities of this essential nutrient.
Hormone Balance:
A healthy microbiome is an indispensable part of the process by which we maintain hormone balance. Specific bacteria produce enzymes that help us break down and metabolize our estrogen. Essentially, these bacteria work to flush hormones that have been used, and are ready for elimination, out of the body, making way for fresh new hormones to take their place.
If you have the wrong types of bacteria in your gut, then estrogens get reabsorbed and recirculated, setting the stage for estrogen dominance and associated symptoms such as infertility, PMS, low libido, cramps, heavy menstrual bleeding , and PCOS. This also makes us more susceptible to estrogen related cancers like breast and uterine cancer.
Without enough of the good guys, we are setting ourselves up for a toxic build-up of hormones that can lead to PMS, menopausal symptoms, or worse.
What is living in our gut strongly influences almost every conceivable aspect of our health. In fact, most people don’t know that symptoms like allergies, acne, depression, fatigue and autoimmune diseases often have digestive problems at their root.
Immunity and Respiratory Illness:
Our microbiome also supports our overall immunity. Approximately 70% of your immune system is located in your gut and the good bacteria are informing this at all times. Studies show that gut microbiota influences our immune system, both in the intestines, but also systemically.
The use of broad spectrum antibiotics, (and other factors like chemical exposure, diet, and environmental exposure) alter the makeup of our microbiome. Multiple studies report that this alteration can negatively influence the immune response in your airways leading to greater susceptibility to many allergic airway diseases, including seasonal rhinitis and asthma, as well as viral infections of the respiratory tract.
Acute respiratory tract infections are the leading cause of death in infants and young children worldwide, and while these can be bacterial in origin, the majority of them are caused by viral infections. Researchers believe that that the composition of the microbiome may affect the severity of viral infection in children.
Digestive Disorders:
Locally, in the gut, disruption of the balance in the microbiota (dysbiosis) has been associated with inflammation-linked disorders, like inflammatory bowel disease.
Metabolic Syndrome and Weight Gain:
A Danish study with 169 obese and 123 non-obese participants confirmed that people with lower amounts of good bacteria had higher body fat percentage, increased insulin resistance, higher markers of inflammation, and poor cholesterol balance. They also gained more weight over time.
Several days to a week of antibiotics will wipe out majority of the bacteria, both good and bad–decreased diversity and altered composition can be seen within 3-4 days. Even a single dose of Clindamycin (commonly prescribed for things like bacterial vaginosis or sinus infections) causes an enduring loss of 90% of normal microbial diversity.
Our intestines are somewhat like an apartment building—there is only space for so many tenants. You want to have primarily good tenants, who pay the rent on time, take care of the place, and like to keep tidy. But wiping out the majority of the tenants, both good and bad, leaves it as a toss-up in terms of who will take residency after you stop taking the antibiotic.
So, while bacterial counts in the gut start to recover within a week, studies show that the composition of the microbiome is significantly altered from what was present prior to treatment. And because antibiotics only work against bacteria, this leaves room for pathogenic yeast or fungal strains to gain a running head-start while you are taking the prescription. While yeast like Candida are a normal part of our healthy microbiome, they should only comprise a small percentage of a diverse population. When they start to overgrow, and run the show, a myriad of problems and increased production of toxins can disrupt our digestive health and also impact other body systems outside of the gut.
The good news is that we have a lot of influence over who we promote when it comes to rebuilding the good guys! If you must take antibiotics, here are a few things you can do to help protect your gut and immunity while taking them:
Foods
Avoid sugar, alcohol, dairy (except fermented), and gluten: These foods either contain proteins that are harder to digest across the board, or tend to feed yeast.
Eat probiotic fermented foods: sauerkraut, kim chi, any other fermented veggies such as beets or carrots, coconut kefir, kombucha, yogurt (preferably homemade and 24-hour).
Drink bone broth: collagen heals the gut and is also prebiotic (feeds the beneficial flora).
Eat Prebiotic foods: Prebiotics are fibers found in specific foods that are food for the beneficial flora. Jerusalem artichokes (sunchokes), raw dandelion greens, garlic, leeks, onions, jicama, Chicory root (which you can find in Dandy Blend beverage), asparagus, green bananas and plantains, cacao, burdock root, or foods high in resistant starch (such as cooked and cooled rice, legumes, or potatoes) are all foods with high prebiotic content. You can also take a prebiotic supplement, like Mega PreBiotic—start slow! Interestingly, these types of starches onlyfeed the beneficial flora, and not the “bad guys”.
Supplements
Butyrate: Part of the reason why prebiotics are so helpful is that they provide raw material for the good bacteria to ferment, producing short chain fatty acids.
Butyrate, one of the SCFA’s produced in this process, is the energy source of choice for the cells lining the colon and helps regenerate colonic mucosal membrane. It has several different actions that are cancer-preventative. Butyrate also fights inflammation in the gut. In fact, not having enough Butyrate can trigger or worsen ulcerative colitis, chron’s Crohn’s disease or colon cancer.
While most of our butyrate is produced by our healthy flora, grass-fed butter is also a great source of dietary butyrate, and, it is also available in supplement form. Generally, I recommend taking it for 2-4 weeks following antibiotic use.
Probiotics: The most important probiotic you can take during and after a round of antibiotics is actually a strain of yeast. Saccharomyces boulardii is a beneficial, non-pathogenic yeast that was first identified on lychee and mangosteen fruits in the tropics. While it may sound strange to intentionally put yeast into your digestive tract, S. Boulardii is a completely different species from the pathogenic candida species that are associated with digestive and other health problems. Besides increasing short-chain fatty acids (remember those from above? We want those!) that soothe the mucosal cells in the gut, these yeast are also stellar at treating and preventing diarrhea, and also boost secretion of IgA (immune agents) in the gut. They are helpful for treating C. Difficile infection, reducing inflammation in IBD, and help to prevent the formation of food-allergies. I recommend Designs For Health Floramyces, or Saccromycin DF by Xymogen. The dosage that I recommend in this case is 5-10 billion CFUs 3-4 times daily. It is important to start taking Saccharomyces Boulardii as soon as possible, as it can (and should) be taken during course of antibiotics to help prevent yeast overgrowth and calm inflammation. Since they only work on bacteria, antibiotics won’t kill the yeast. Keep taking it for 2-3 weeks after completing the antibiotic.
Generally, after the antibiotic is completed, I recommend adding in an additional Acidphilus/Bifidus containing probiotic blend for several weeks, such as Klaire Labs Therbiotic Complete.
Have you taken antibiotics and noticed health changes after taking them? Or, have you taken preventative measures like the ones above that you felt safeguarded your health? If so, what differences did you notice?











