What Causes Diarrhea in Adults and How to Stop It
Diarrhea can take control of your life. I’m not talking about the average tummy bug kind of diarrhea. I’m talking about the type of diarrhea that lasts for days, weeks, months, or even years…chronic diarrhea.
Diarrhea can disrupt the rhythm of your daily life, and take a real toll on your body. But, the good news is that you do not have to live with chronic diarrhea! Diarrhea is a treatable medical condition. Together, we can uncover what’s causing your diarrhea, help to treat your symptoms, and get you back on the road to good health.
Diarrhea Symptoms
Passing loose, watery stools three or more times per day is the primary symptom of diarrhea. Other symptoms can accompany diarrhea including:
- Belly bloating
- Cramping
- An urgent need to use the bathroom
- Nausea
- Abdominal pain
Some people can experience more severe symptoms including:
- Blood or mucus in your stools
- Fever or chills
- Vomiting
- Light-headedness or dizziness
What Causes Diarrhea?
There are a variety of factors that can cause diarrhea. Temporary diarrhea, lasting one to two days, can result from a viral infection, the food you ate or traveling.
On the other hand, chronic diarrhea can indicate a more serious problem. The most common causes of chronic diarrhea include inflammatory bowel disease (Crohn’s disease and ulcerative colitis), chronic infections, and malabsorption syndromes (cystic fibrosis, Celiac disease, lactose intolerance, etc.) in which food is not digested and absorbed.
Chronic diarrhea is a common complaint amongst our patients. Below are seven of the most common causes of chronic diarrhea that we treat including gallbladder removal, IBD, gut dysbiosis or pathogen imbalance, histamine intolerance, gluten intolerance or Celiac, dairy intolerance, and SIBO.
1. Gallstone or surgical removal of the gallbladder
Frequent loose, watery stools after having gallstones or having your gallbladder removed (cholecystectomy) is common. The gallbladder collects bile to release when you eat aiding in the digestion of fats. Removing the gallbladder takes away the main storage site for your bile acid. Instead, the bile acid is stored in the gut causing it to be less concentrated and drain into the intestines. Once in the intestines, it can have a laxative effect making stools looser.
GI transit times can also be altered after gallbladder surgery causing transit times to decrease in the small intestine and accelerate in the colon. This impairs the body’s ability to absorb water from your stool leading to looser, watery stools.
2. IBD
Inflammatory bowel diseases (IBD), including Crohn’s, Ulcerative Colitis, and other types of colitis (microscopic or lymphocytic colitis), are diseases of chronic inflammation. IBD causes tissue destruction and inflammation of the bowel walls limiting the body’s ability to absorb fluids. This results in loose, watery, or even completely liquid stools.
Patients with IBD may experience frequent and urgent bowel movements because fluid moves more rapidly through the intestine. You may also see blood in or on the stool and experience extreme weight loss, anemia, fever, and loss of appetite.
3. Gut Dysbiosis or Pathogen Imbalance
Gut dysbiosis is a generic term for an imbalance in gut flora. Our digestive tract contains a delicate balance of different kinds of bacteria. When one species becomes overgrown or gets wiped out, the balance is thrown off leading to diarrhea along with many other symptoms.
There are several pathogens known to cause gut dysbiosis including bacterial, yeast, parasites, and viral pathogens.
- Acute Bacterial Pathogens: The most common bacterial organisms to cause diarrhea include: e coli, shigella, Campylobacter Jejuni, Citrobacter, yersinia enterocolitica, salmonella, and Staphylococcus aureus. Chronic bacterial toxins like those secreted by C Difficile can also lead to diarrhea. Older adults in healthcare facilities, like hospitals or nursing homes, or who have recently been on antibiotics, are more at risk for contracting C Difficile.
- Yeast and Fungal Overgrowth: Rapid growth of Candida (a yeast) and cryptococcus (a yeast-like fungus) in the GI tract can lead to diarrhea, especially after antibiotic use.
- Parasites: Intestinal parasites including giardia, entamoeba histolytica, Cryptosporidium Parvum, and Protozoan parasites like blastocystis hominis, Cyclospora, Dientamoeba Fragilis, Entamoeba coli, and endolimax nana can cause diarrhea. Parasitic infections are often, but not always, marked by stomach cramps, bloating, nausea, and watery diarrhea.
4. Histamine Intolerance
Histamine is a chemical that notifies the brain when to release stomach acid for digestion. And, it is part of our response to injury or an allergic reaction. Histamine intolerance occurs when the body is unable to break down enough of it in the intestines, causing histamine levels in the blood to rise.
Histamine intolerance can result from a multitude of factors including a combination of genetics, and a leaky gut. This leads to decreased secretion of DAO enzyme (used to break down histamine), liver detox overburden, and dysbiosis.
5. Gluten Intolerance or Celiac
Gluten, a protein found in wheat, can cause inflammation in the gut and can change the structure of the gut wall. For people with gluten intolerance or Celiac disease, gluten can cause chronic diarrhea along with other GI symptoms.
6. Dairy
Dairy products contain three components that can cause diarrhea: lactose, whey, and casein.
Lactose intolerance is an inability to digest lactase, a sugar found in milk products. Lactose intolerance occurs when the small intestine does not make enough of the digestive enzyme lactase. This condition is common in adults with a genetic predisposition or after an injury, disease, or infection of the small intestine. Lactose intolerance causes diarrhea by increasing the volume of water in the colon, which in turn increases the volume and liquid content of the stool.
Casein and whey, the two proteins in milk products, can cause an allergic reaction when the body thinks the protein is harmful. Most people with an allergy to casein or whey have symptoms that appear as infants and outgrow them with age. However, patients with gut wall damage can experience dairy protein intolerance with diarrhea and other GI symptoms.
7. SIBO
SIBO is an overgrowth of bacteria in the small intestine. Normally, the small intestine contains fewer bacteria than the large intestine and is focused on food absorption. For many who have SIBO, diarrhea is a common symptom.
How is Chronic Diarrhea Diagnosed
The key to diagnosing chronic diarrhea is to uncover the underlying root causes so that we can address them and prevent future relapses. Common tests for patients with chronic diarrhea may include:
- Comprehensive Stool Microbiome Testing – A stool sample can be used to evaluate the root cause of digestive tract issues. Functional medicine stool tests provide information about absorption, digestion, yeast overgrowth, bacterial imbalance, parasite infection, inflammation, metabolic activity, and immune function.
- SIBO Breath Testing with both lactulose and fructose for best accuracy
- Blood Test – Specific blood tests can help identify celiac disease antibodies and yeast antibodies.
- Imaging – Imaging can include endoscopy, colonoscopy, or sigmoidoscopy and is generally used to diagnose or rule out Inflammatory Bowel Disease or structural issues as a driver for symptoms.
Natural Remedies and Treatments for Diarrhea
The challenging part of treating diarrhea is that there is not a one size fits all treatment plan. Many mild cases of diarrhea will resolve on their own. But, for more severe, chronic cases of diarrhea there are a variety of natural remedies and treatments available.
Diet
Specific Carbohydrate Diet (SCD):
The SCD diet is incredibly effective at stopping urgent, frequent bowel movements. This is for you if you run to the bathroom 10 to 20 times per day. The SCD diet focuses on removing carbohydrates that are not fully digested and remain in the gut leading to an overgrowth of harmful bacteria. It is particularly helpful for my patients who have Crohn’s disease, celiac, ulcerative colitis, and chronic diarrhea.
Download a free guide to properly starting the SCD diet from the team at Healthy Gut.
Starch and Meat Diet:
A starch and meat diet is an alternative to the SCD diet that works for some people. This whole-food diet is focused on eating foods like white rice, white potatoes, meat, fish, and poultry. Like the SCD diet, this diet limits all processed and canned foods.
Diet Considerations During Flare-Ups:
Curing the cause of chronic diarrhea can take time. And, flare-ups happen. During diarrhea flare-ups keep these diet considerations in mind.
- Be cautious with fruit, except for bananas
- Raw vegetables can be hard to digest and cause GI upset
- High amounts of fats and oils can be difficult for a sensitive digestive system. Limit high-fat foods like egg yolks, cream, oils, and bacon.
Many other diets (low FODMAP, Low Histamine, Low Salicylate, Low Oxalate, or Autoimmune Paleo) can be useful for the treatment of diarrhea depending on the underlying causes.
Stress Reduction
Have you ever had to run to the bathroom before a presentation or a big event? That’s your gut responding to stress! Increased levels of stress can cause changes to your gut motility, which means that your body can slow down or speed up food processing based on your levels of stress.
Active stress relief activities are a critical component of naturally treating diarrhea. Try watching a funny movie, taking an Epsom salt bath, meditating, or practicing moderate exercise daily.
Sleep
Many of your body’s metabolic processes occur during the night, including digestion. And, sleep provides your body the much-needed energy for digestion to happen.
A few nights of poor sleep might not have a major impact on your GI health. But, chronic insomnia or poor sleep can impact your GI and contribute to your chronic diarrhea.
Supplements
Depending on the cause of your diarrhea, a variety of supplements may be beneficial to you. I often incorporate the following supplements into my patient’s treatment plans.
Digestive Enzymes:
After eating, enzymes break down the food so that we can absorb the carbohydrates, fats, and proteins. Without enzymes, larger food pieces remain in our gut and begin to ferment, feeding the bacteria. This can either slow down digestion or speed it way up.
There has been significant research indicating the successful use of digestive enzymes to support patients with chronic diarrhea. The key to digestive enzymes is taking enough with the right balance of acidity for them to work. It may take some time, but my patients who use digestive enzymes report amazing results!
I recommend Holozyme by Healthy Gut.
High Dose Probiotics:
High-dose probiotics have been shown to balance the gut microbiome and improve intestinal permeability promoting intestinal barrier functions and alleviating many inflammatory responses.
Depending on the cause of your diarrhea, I recommend a variety of probiotics usually containing 250 (or more) organisms daily to help control diarrhea. Below are a few of my go-to probiotics:
- S. Boulardii, a probiotic yeast strain, is my number 1 go-to for helping alleviate diarrhea, especially if it was a result of antibiotic use. But, in my clinical experience, patients with IBD should proceed with caution with introducing S. boulardii because Anti-Saccharomyces cerevisiae antibodies (ASCA) have been associated with Crohn’s disease. Saccharomyces Cerevisiae (Brewer’s/Bakers yeast) is similar enough to S Boulardii that the immune systems of sensitive individuals can cross-react, potentially triggering a symptom flare.
- Bacillus Claussi, a spore-forming probiotic, is an effective probiotic for treating diarrhea, preventing antibiotic associated diarrhea, and may be viable as the only treatment in some cases of SIBO where tolerated.
- Bacillus Subtilis is a multifunctional probiotic ideal for preventing the growth of bacteria and enhancing nutrient digestion. HU58, a strain of bacillus subtilis, is used for the management of antibiotic-associated diarrhea in adults.
- Lactobacillus Rhamnosus GG (LGG) is one of the most widely used probiotic strains and it is ideal for patients with histamine driving their diarrhea. In addition, there are many well-documented studies showing that LGG is indicated for the prevention and treatment of gastro-intestinal infections and diarrhea.
- UltraFlora Intensive contains Lactobacillus plantarum 299v, a probiotic strain of lactic acid bacteria that is naturally occurring in the human gut. This probiotic is excellent at decreasing anti-inflammatory symptoms making it ideal for reducing diarrhea in patients with IBS, C. diff, spontaneous colitis, and high E coli levels.
- High-dose lactobacillus, found in TheraLac, promotes healthy, rapid growth of all beneficial bacteria that can boost immune health and promote regularity.
Immunoglobulins or Colostrum:
Immunoglobulins and colostrum help strengthen the body’s natural immune system. While also fighting bacteria and viruses that cause diarrhea. I recommend utilizing a bovine-derived serum that is lactose-free to repair and support healthy gut barrier functions.
Chinese Herbal Formulas:
This is far from an exhaustive list of Chinese herbal formulas for diarrhea, but these are three of my favorites to use with my patients.
- Shen Ling Bai Zhu San – Usee for poor nutrient absorption, bloating, and/or loose stools.
- Raise Qi – Helpful for poor digestion, bloating and gas pain, chronic diarrhea, and loose stools.
- Huo Xiang Zheng Qi San – Ideal for treatment of acute diarrhea or travelers' diarrhea.
Short-Term Support in a Pinch
When you're in a pinch, it’s always helpful to keep a few diarrhea treatments in your arsenal. I recommend keeping these on hand:
- Bismuth Subsalicylate: Also known as Pepto-Bismol, increases the amount of fluid your intestines can absorb while reducing inflammation and overactivity of your intestines. Note that both liquid and chewable Pepto-Bismol may contain fermentable sweeteners. Follow the label for dosage.
- Imodium: Imodium works to slow motility for sudden diarrhea. Follow the label for dosage.
I Can Help Identify the Cause of Your Diarrhea and Get You Back on the Path to Good Health
Are you ready to troubleshoot your chronic diarrhea? Get a better understanding of your digestive health and the natural approach to resolving diarrhea once and for all, by booking a free 15-minute call with me.
If after the call you come on board as a patient, your clinician will order the best tests for your specific situation, and develop a unique treatment plan so that you can get back on the road to good health.
References:
"Symptoms & Causes of Diarrhea | NIDDK." https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea/symptoms-causes. Accessed 31 Mar. 2022.
"GI-MAP® Interpretive Guide - Diagnostic Solutions Laboratory." https://www.diagnosticsolutionslab.com/sites/default/files/u16/GI-MAP-Interpretive-Guide.pdf. Accessed 6 Apr. 2022.
"Histamine: The Stuff Allergies are Made of - MedlinePlus." 1 Apr. 2019, https://medlineplus.gov/medlineplus-videos/histamine-the-stuff-allergies-are-made-of/. Accessed 6 Apr. 2022.
"Enzyme therapy for functional bowel disease-like post-prandial ...." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6910206/. Accessed 12 Apr. 2022.
"Probiotics for infectious diarrhea - PMC - NCBI." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1773578/. Accessed 19 Apr. 2022.
"Bacillus clausii - The Probiotic of Choice in the Treatment of Diarrhoea." https://www.longdom.org/open-access/bacillus-clausii--the-probiotic-of-choice-in-the-treatment-of-diarrhoea-2157-7595-1000211.pdf. Accessed 12 Apr. 2022.
"Bacillus subtilis HU58 and Bacillus coagulans SC208 Probiotics ...." 11 Jul. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7409217/. Accessed 12 Apr. 2022.
"Towards a better understanding of Lactobacillus rhamnosus GG - PMC." 29 Aug. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155824/. Accessed 12 Apr. 2022.
The role of Lactobacillus plantarum 299v in supporting treatment of ...." 25 Jan. 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7882405/. Accessed 12 Apr. 2022.
What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
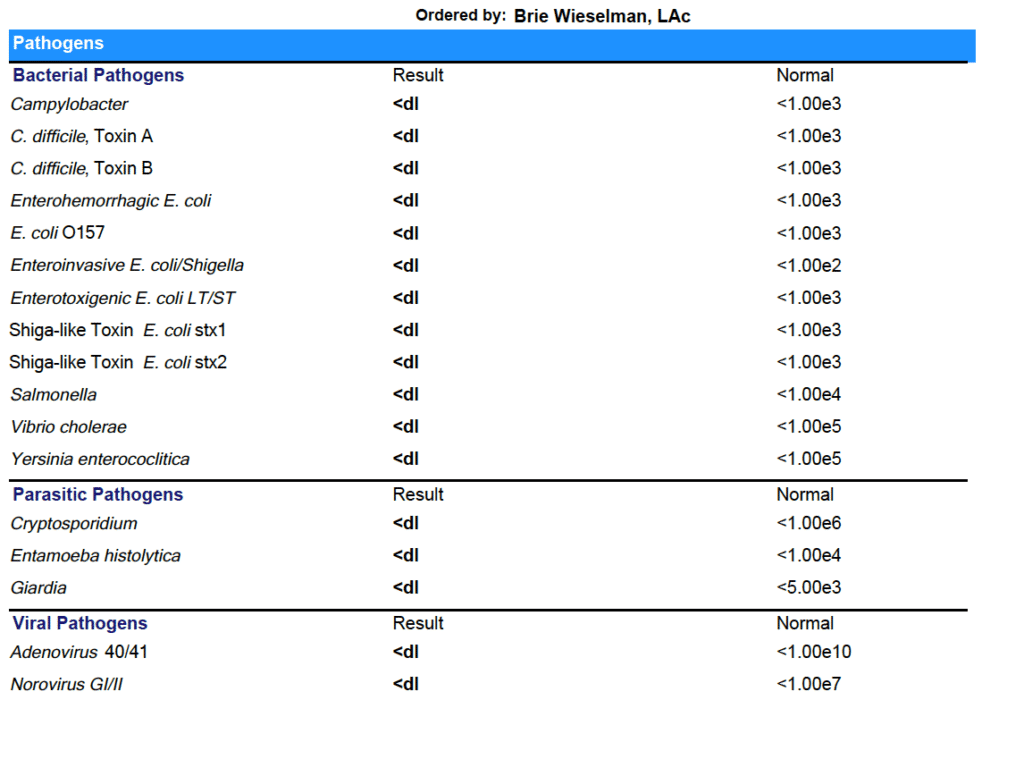
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
Marina agreed to the test, and a few weeks later, results were in:
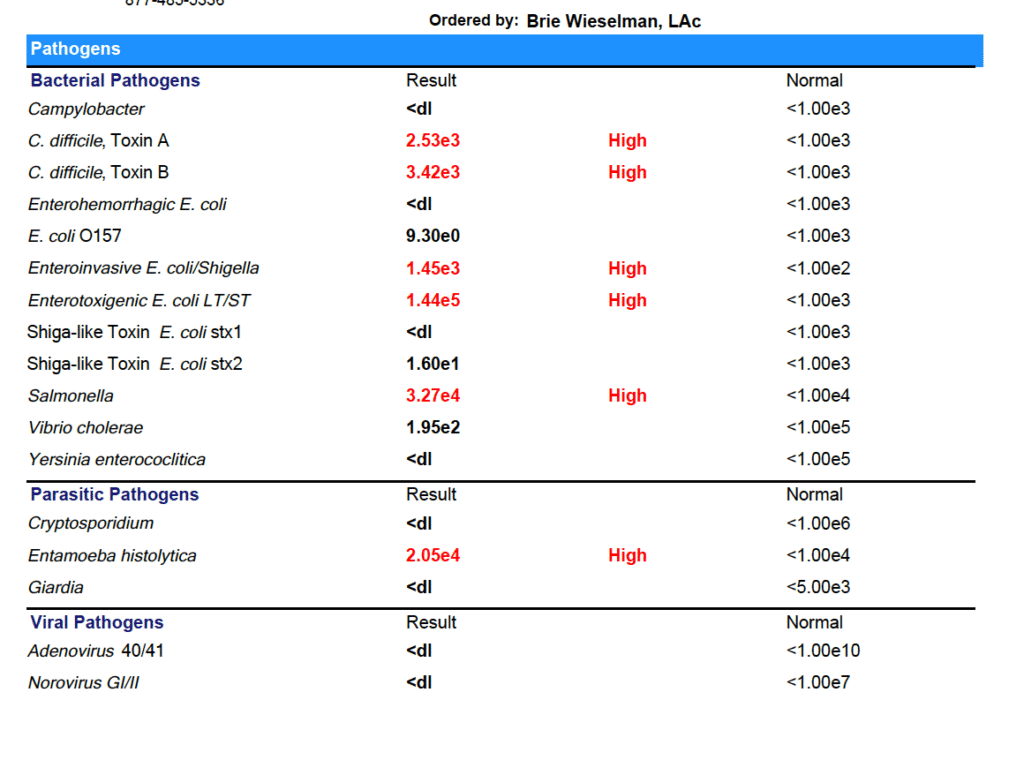
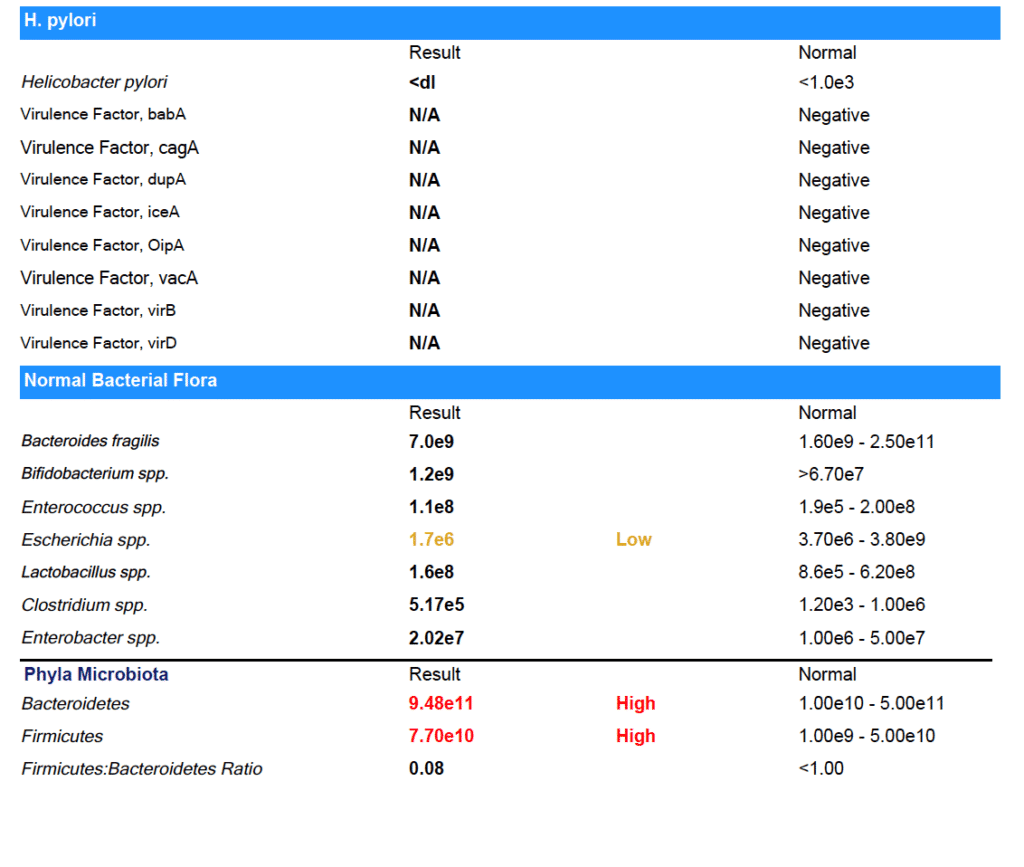
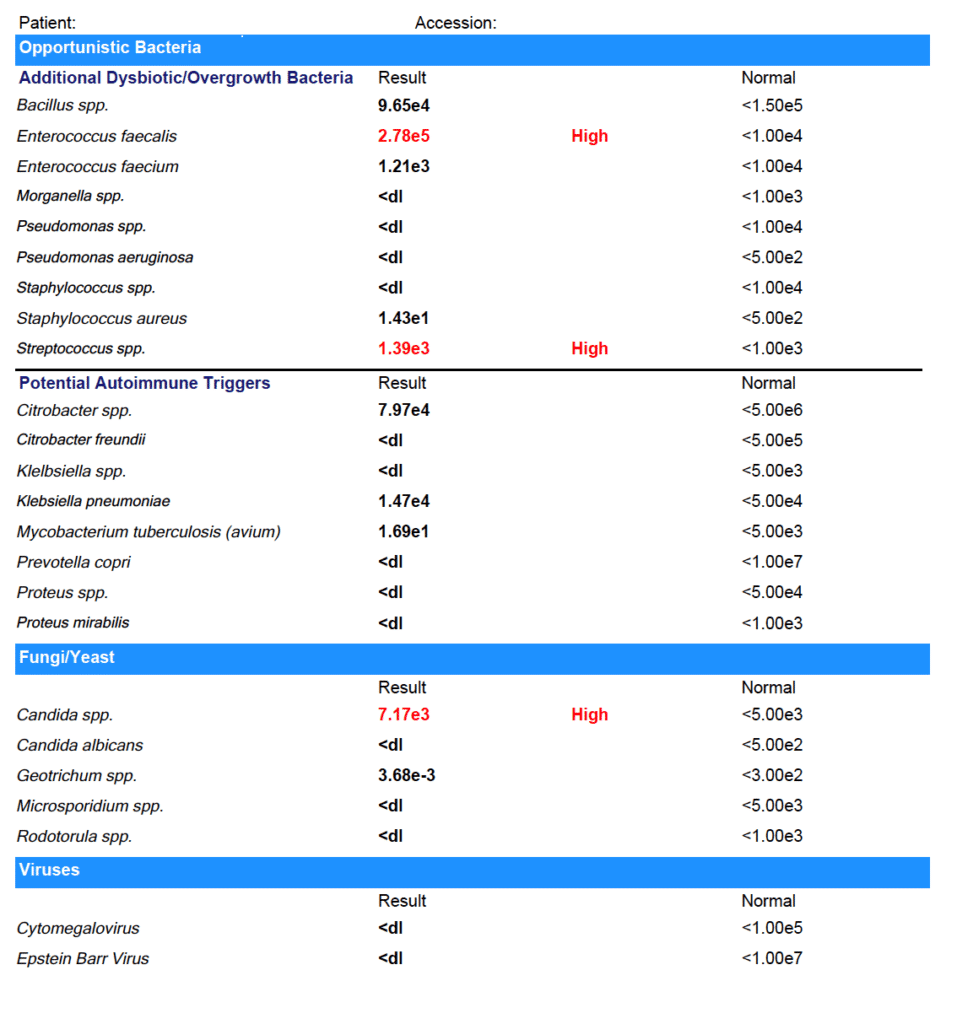
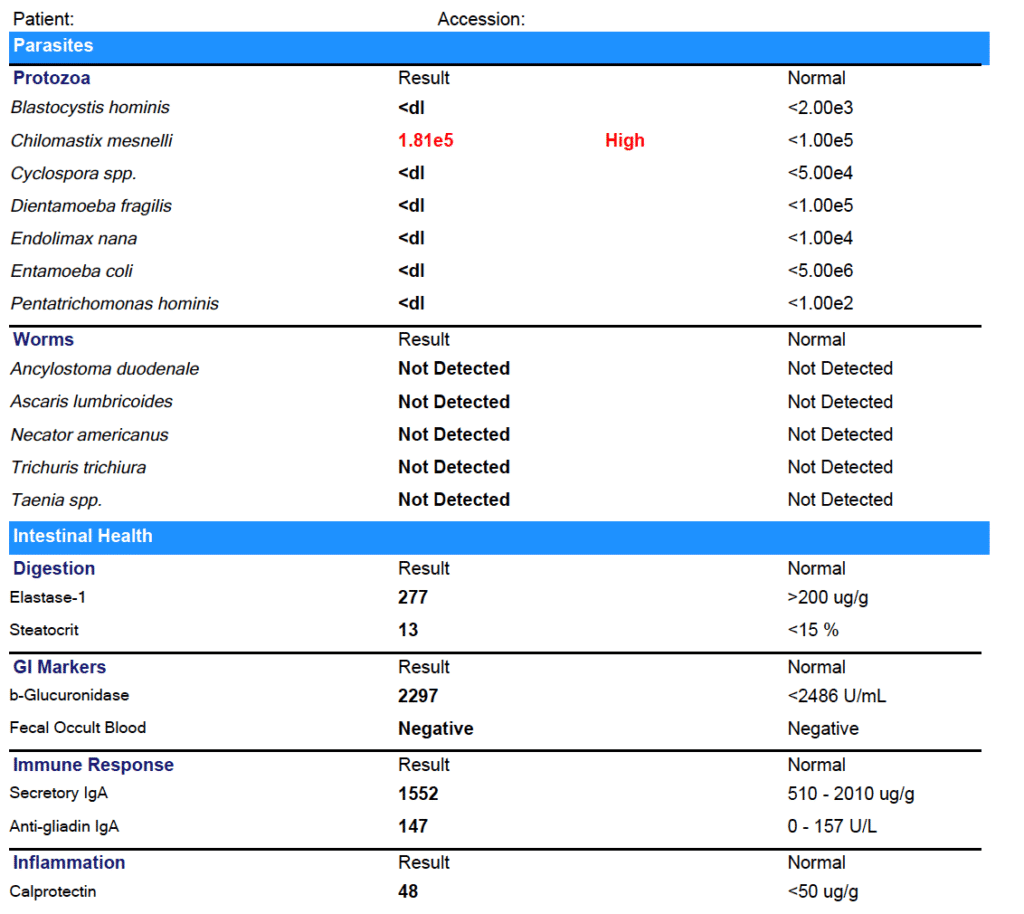
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
Step 3: The Second Test Results:
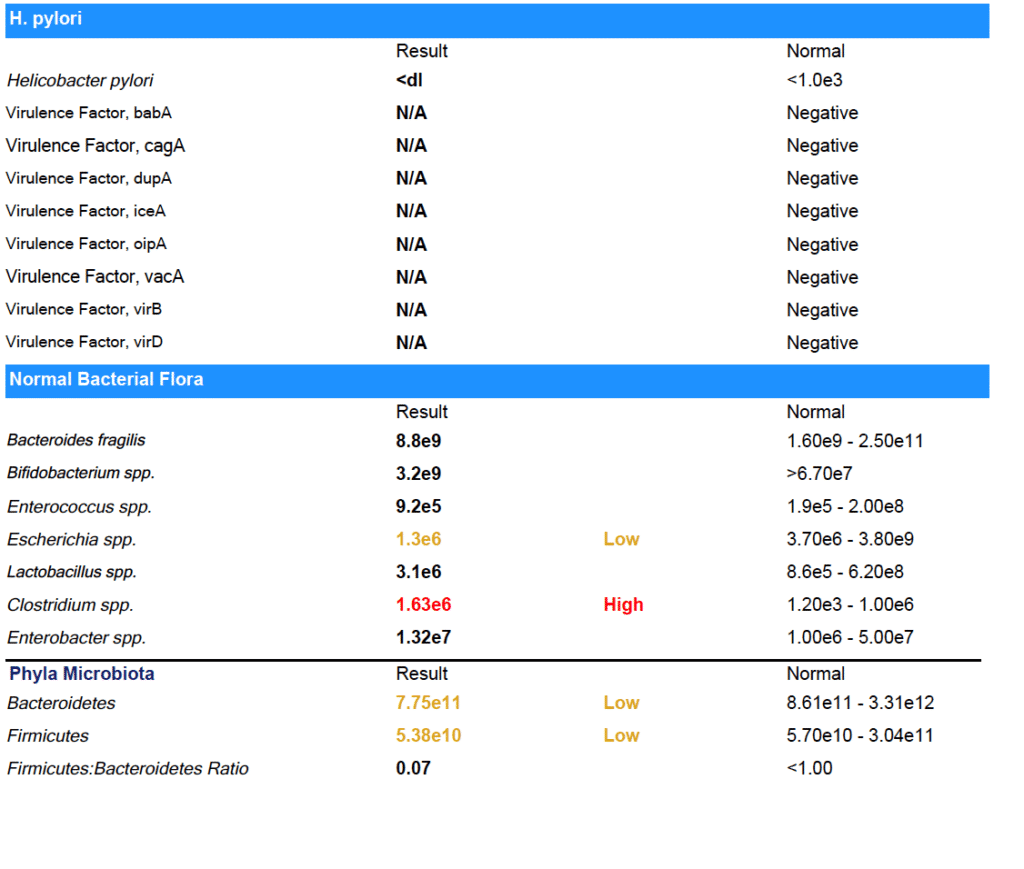
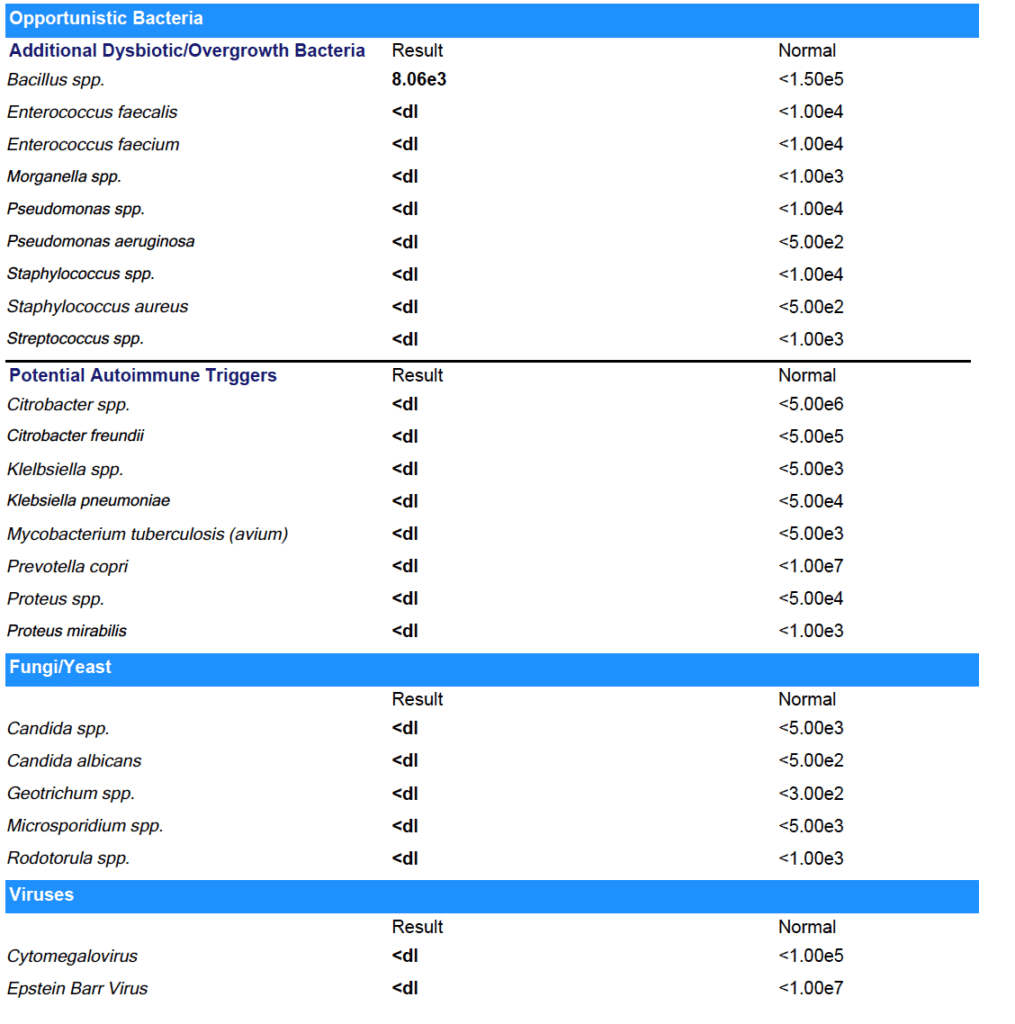
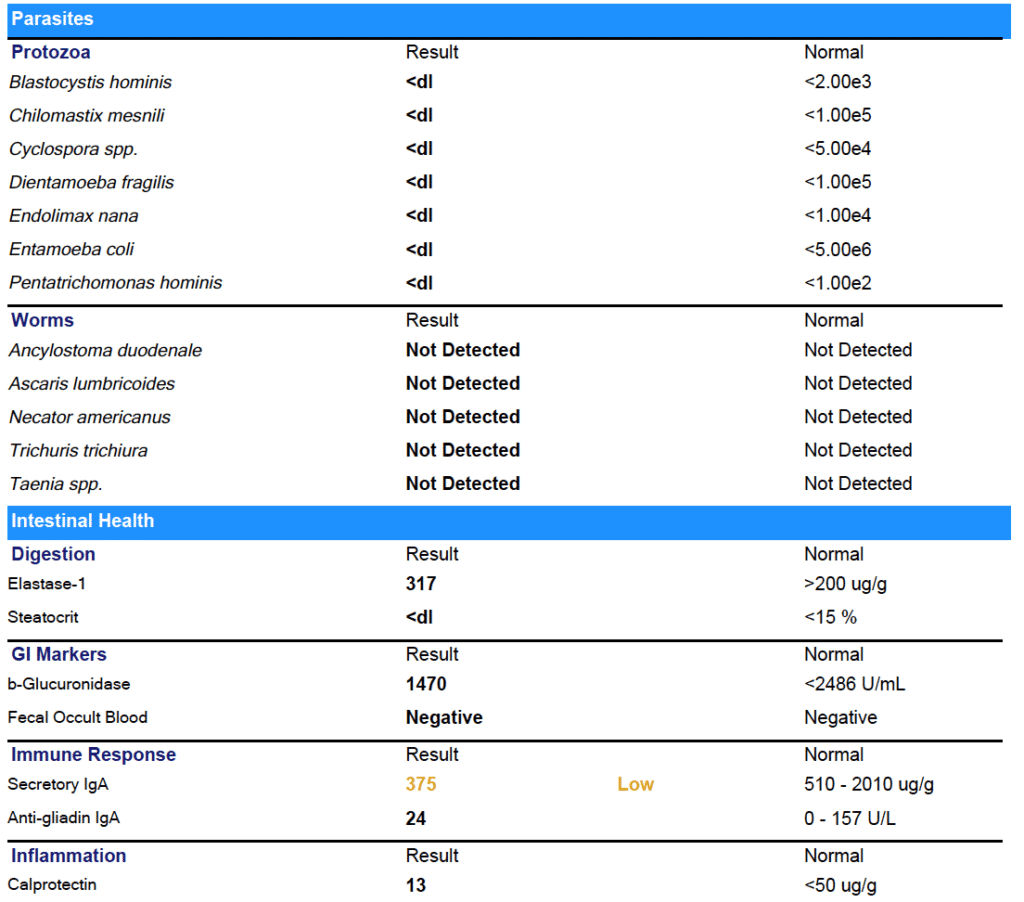
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
4 Crucial Steps for Mealtime that can make-or-break your digestion
When it comes to healing digestive issues, it’s certainly true that we need to test to identify and then treat any infections or dysbiosis that may be contributing.
But just as importantly, we need to optimize the environment of the gut. In order to develop infections or overgrowths, the environment has to be right. Otherwise, our healthy gut terrain is inhospitable to the “bad guys”, and nurturing to the “good guys”.
This mainly involves things like optimal digestive secretions (like stomach acid and pancreatic digestive enzymes) that set the pH and fully digest our food. This ensures that we both assimilate the nutrients contained in what we eat, but also prevents other organisms, like bacteria and yeast, from eating it instead.
Other secretions, like bile from our liver/gall bladder, are also super essential. Bile digests fat, but also is a powerful antimicrobial, and regulates the motility of our intestines.
Of all the digestive secretions, Stomach Acid might be the most important when it comes to resilience against infections. Stomach acid (called Hydrochloric Acid, or HCL) is like your first line of defense.
You may know that stomach acid’s main role is to break down the proteins we eat, so that we can absorb the smaller amino acid building blocks to use as nutrition.
But stomach acid is also antibacterial to undesirable strains because of the low pH environment that it creates.
Keeping food in the stomach long enough is critical for the action of stomach acid to control the populations infused into lower regions with each pulsatile release of chyme. This is because food needs to be exposed to stomach acid (HCL) long enough to kill bad bacteria, preventing them from proceeding on into the small intestine.
So, if you have super-rapid motility (this is common in people who have chronic diarrhea), your food may pass too quickly through the stomach and into the intestines, and not have enough exposure to HCL. This equals increased risk of infections, in addition to not enough nutrient digestion.
Due to…
- Stress
- Nutrient deficiencies
- Modern diet and lifestyle
- And even just natural aging!
it’s unfortunately very common for people to produce less than optimal amounts of stomach acid to meet the demands of food intake.
And…..we need enough HCL present to keep the stomach pH below 4 for the entire time the food we are digesting in the stomach. If this doesn’t happen…pathogenic microbes pass unharmed into the intestines where they can take residence! (hello SIBO and parasites!)
Here’s the most important thing I want you to learn today:
HOW we eat our meals is one of the most important factors in optimizing gut environment.
Just becoming aware of HOW we eat, is one of the biggest things you can do to change what is happening with your digestive secretions, and therefore, with your microbiome.
Chewing: Why is chewing your food so important in regards to this?
Yes, chewing breaks your food down into smaller pieces, increasing the surface area, so that digestive secretions in the stomach and small intestines (like pancreatic enzymes, bile, and stomach acid) can further break them down.
But….there are other not so obvious reasons!
Chewing exposes foods to enzymes in the saliva that break down the cell walls of gram positive bacteria, causing them to die.
This means that chewing adequately is really our first weapon against pathogens that might be entering with our food!
Being relaxed while eating: Stress is a big factor that leaves us more prone to getting opportunistic gut infections, because stress shuts down our digestive secretions.
When our brain thinks we need to run from the proverbial tiger, it focuses our body’s energy and attention on surviving NOW, and diverts it from activities that are about long term survival, like digesting our nutrients.
Stress also spikes our cortisol, and this suppresses our gut’s immune system big-time--for much the same reason. And the hormone that our brain uses to signal the adrenal glands to make more cortisol, CRH, can promote leaky gut.
Healthy Meal Hygiene for Healthy Gut Environment:
1) Focus on creating a state of overall calm before, during and after eating to encourage stomach acid and digestive enzyme secretion.
2) Chew adequately—more than you think….keep chewing!-- to reduce particle size and mix enzymes in the saliva.
3) Include balanced fats, carbohydrates and proteins in each meal to encourage food to stay in the stomach long enough.
4) Planning enough time for meals—not eating on the run—is critical, to help allow for parasympathetic (rest-and-digest) nervous system activity. This allows for proper secretion of digestive fluids. Otherwise, if our body thinks we are running from the hypothetical tiger, there’s no digestion being emphasized, and no secretions being made—“Ain’t nobody got time for that”!
Have any questions or comments on this?
Pop on over to my facebook page and ask me anything!
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
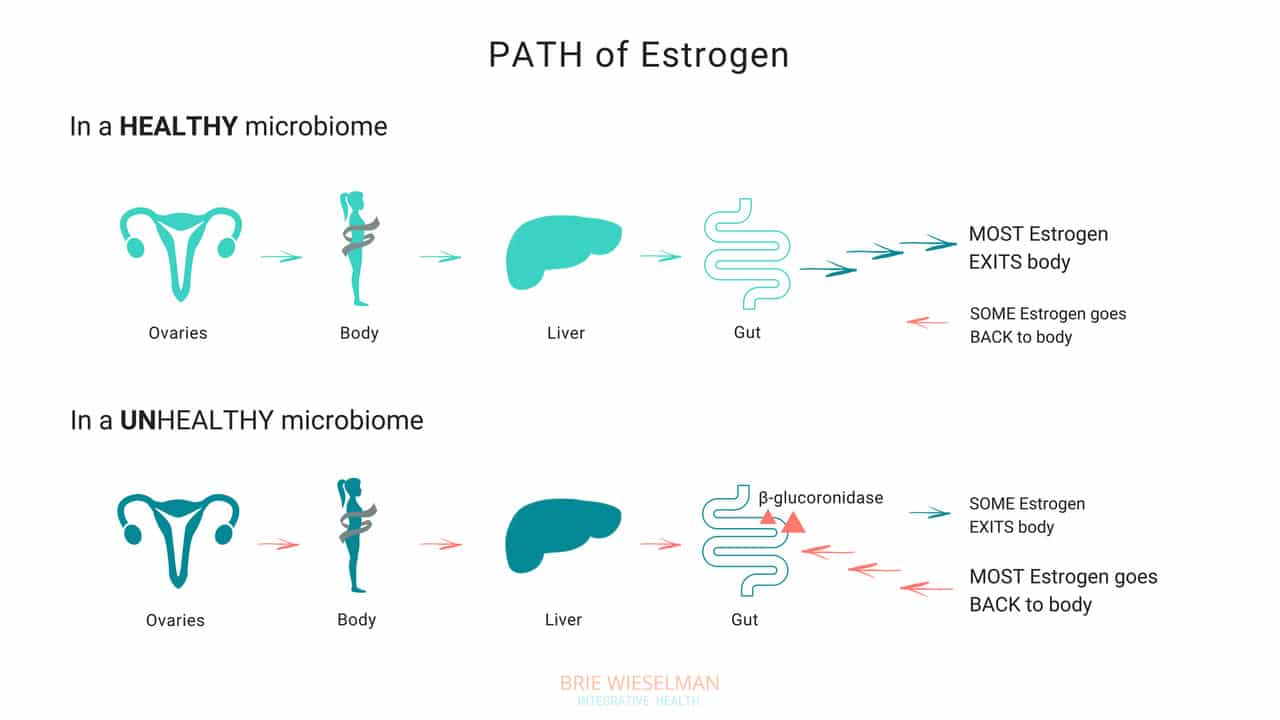
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.




