Anxiety Disorder Symptoms, Hormonal Imbalance, and Histamine Intolerance: The Surprising Connection
Your brain is foggy. Making even small decisions feels overwhelming.
You’re worried about everything and it’s hard to sleep at night.
The fatigue that nearly overpowers you makes you want to go back to bed and pull the covers over your head and hide from everyone and everything.
You’re cranky, restless, and on edge. Panic attacks cause your heart to race and your palms to get sweaty.
Even if you only have only a couple of these problems, you may have generalized anxiety disorder. That’s the bad news.
The good news? You can feel at peace, happy, and calm again. The answer lies in balancing your hormones. But that’s not all. You’ll also need to get rid of problems like blood sugar imbalance that cause your hormones to get out of whack. Then there’s histamine intolerance, which is strongly linked to hormonal imbalances and anxiety.
Hormone Imbalance: The Victim Not the Villain
Imbalanced hormones are not the villains responsible for your anxiety disorder. They’re more like the victims of other problems happening in your body. That’s why as a functional medicine provider specializing in irritable bowel syndrome, inflammatory bowel disease, and women’s fertility issues I see a lot of patients who also suffer from anxiety and panic attacks.
In fact, 75% of my patients present to my clinic with anxiety along with other issues like acid reflux, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), digestive issues, endometriosis and many more.
Hormones are actually responders, the language the body uses to talk to itself. Hormones express what they’re seeing in the different tissues around your body and tell your body how best to respond.
In other words, when hormones break, it’s not typically the root cause of your problems. Rather, the hormones shift in response to the root cause or causes of your health problems.
That said, working to adjust and balance hormones can help you feel better. When your hormones are balanced, you will have more energy and bandwidth to work on the real root cause underlying your health problems.
In this article, I’m going to dive into one common factor that breaks hormonal balance. Then I’ll hone in on one of the most important hormones for people suffering from anxiety disorder and its link to histamine intolerance.
I’ll also shed light on some of the other reasons for anxiety and panic attacks and let you know what you can do to feel less anxious and more at peace.
First, though, let’s talk about what generalized anxiety disorder actually is and its symptoms.
What Is Generalized Anxiety Disorder?
Everyone gets anxious from time to time. Work deadlines, tests at school, dealing with relationship problems or other stressors can all lead to occasional anxiety.
People with generalized anxiety disorder, on the other hand, experience ongoing worry or fear much of the time.
Often, people with anxiety disorder feel anxious or get panic attacks even while trying to make simple decisions. Generalized anxiety disorder can cause problems at work, in school, and in your relationships.
Symptoms of generalized anxiety disorder include :
- Difficulty concentrating or brain fog
- Fatigue
- Insomnia (difficulty falling or staying asleep)
- Irritability
- Restlessness
- Worry
Generalized anxiety disorder and panic disorder are some of the most common mental disorders in the United States. These are different types of anxiety disorders. Technically, conventional medicine considers panic attacks to be a separate disorder. However, in my experience as a functional medicine provider, most people aren’t going to have panic attacks without already having generalized anxiety disorder.
Symptoms of panic attacks include:
- Feeling out of control
- Feelings of impending doom
- Pounding heartbeat or rapid heart rate
- Shortness of breath, smothering, or choking
- Sweating
- Trembling
Past trauma can trigger panic attacks. But they can also happen in people who have never experienced any trauma.
Blood Sugar Imbalances Wreak Havoc on Hormones
One of the most common reasons why hormones break is because your blood sugar isn’t balanced. I have seen many patients get 90% better just by balancing their blood sugar.
Low blood sugar mimics anxiety. When your blood sugar crashes, the body attempts to push up blood glucose levels. It does this by making epinephrine, otherwise known as adrenaline, which triggers glucose production in the liver.
Increased adrenaline leads to a “fight-or-flight” stress response in the body. This same biochemical process is also linked to anxiety.
If you tumble into a chronic, on-going low blood sugar state, your body may boost its production of the stress hormone cortisol. This helps tissues in the body be less reactive to insulin, which boosts glucose circulation in the bloodstream. But high levels of cortisol can cause problems, too.
Guess what higher cortisol levels are also linked to? Anxiety.
What’s more, in my work with thousands of patients, blood sugar swings have been the biggest driver of fatigue, anxiety, and mood swings!
A functional medicine provider can order the right tests for blood glucose and insulin sensitivity. These include LDH (lactate dehydrogenase), HbA1c (hemoglobin A1c), SHBG (sex hormone binding globulin), fasting glucose, fasting insulin, and sometimes glucose response testing.
To resolve low blood sugar problems that show up on the tests, eat more healthy fats, which are easier to assimilate and digest.
High quality protein is also important. Back before I knew I had polycystic ovary syndrome – a condition linked to insulin resistance – I was eating vegan and vegetarian and chowing down on carbs. This was the wrong approach because anytime you have a problem with blood sugar or insulin, carbs are the bad guys.
The Soothing Effects of Progesterone
Your brain has receptors for sex hormones like progesterone. So it’s not surprising that progesterone can influence brain function and mood.
If you have anxiety, progesterone is one of your best friends.
Women with low progesterone levels are prone to anxiety. That’s why in conditions of low progesterone such as during PMS, post-childbirth, perimenopause, and menopause there’s an increase in anxiety and frequency of panic attacks.
Progesterone and its metabolite allopregnanolone act as a natural antidepressant, enhance mood, and relieve anxiety. Progesterone has a calming effect on the brain. It increases the actions of a feel-good, calming neurotransmitter known as GABA (gamma-aminobutyric acid).
By giving GABA a helping hand, progesterone acts like a hormonal lullaby, helping you fall asleep easier and stay asleep longer.
What’s Histamine Intolerance Got to Do With It?
Histamine is a chemical released by some cells of the body. If you’ve ever had an allergic reaction or seasonal allergies, you’re likely familiar with its effects such as runny rose, sneezing, or hives.
Histamine isn’t always the bad guy. We need some histamine to release stomach acid and to help move food through the gut. The important thing is for histamine to complete its life cycle by being broken down and cleared from the body.
When that doesn’t happen histamine intolerance occurs. This is when the body makes too much histamine and too little of the diamine oxidase (DAO) enzyme needed to break it down.
Anxiety is a symptom of histamine intolerance. Other symptoms include headaches, fatigue, nausea, irregular menstrual cycles, sinus issues, digestive problems, tissue swelling, and dizziness.
In my experience, people most likely to suffer from histamine intolerance are people who are perfectionists. These are often the same people who suffer from anxiety and panic attacks. They want things to be a certain way and hold high expectations.
Characteristics of people most likely to develop histamine intolerance include:
- Academic overachievers
- Highly motivated
- Inner anxiety with a calm exterior
- Being competitive – with themselves and/or others
- Having obsessive/compulsive or ritualistic behaviors, or a need for structure and strong routine, feeling of order and control over things.
The above characteristics can actually be positive and work in your favor. If you have those characteristics you’re highly intelligent, super productive, and probably are successful in work and life. When your hormones are in balance these traits can work for you.
However, if your histamine is too high and your hormones are out of balance then you might develop poor stress tolerance, feelings of anxiety, and insomnia.
Progesterone Guards Against Histamine Intolerance
Progesterone enhances DAO, the enzyme that breaks down histamine. So progesterone helps histamine meet its maker and clear it from the body.
Estrogen dominance, on the other hand, boosts the body’s production of histamine. Women whose histamine production is estrogen driven will see flares of their problems either right before ovulation or more likely right before their period, because that’s when they’re naturally estrogen dominant.
Does anything else cause histamine intolerance besides estrogen dominance? You bet. Genetics can play a role. My own histamine intolerance was partly caused by genetics. But the gut plays a huge role, too. For me, my high histamine and hormonal imbalance came down to the “bad” organisms in my digestive tract (Helicobacter pylori, Giardia, and Candida albicans)
Leaky gut leads to lower levels of DAO and in turn high histamine. This is because the place where your body makes DAO is mostly mucosal barriers like the intestines.
If your liver isn’t working its best, that will cause problems, too. The liver detoxifies histamine. If its detox abilities are weakened, histamine will build up in the body. It’s just one more thing to fill your bucket up to the point of overflowing.
Other Hormones to Watch in Anxiety and Panic
In my patients with anxiety, I always keep an eye on other hormones besides progesterone. These include:
- Thyroid – If thyroid hormone levels are up and down like in Hashimoto’s it can mimic bipolar disorder. Low thyroid hormones are also linked to low progesterone.
- DHEA (Dehydroepiandrosterone) – DHEA is the most abundant circulating hormone. Balancing levels of DHEA can lead to better mood and less anxiety.
- Serotonin/Estrogen – Serotonin makes you feel content, happy, calm, and ready for sleep. It reduces anxiety and the tendency to think about sad or dark thoughts over and over (cyclical thinking or ruminating). You need estrogen to convert amino acids into serotonin.
- Cortisol – Cortisol is primarily produced by the adrenal glands. Adrenal fatigue can make you less likely to cope with stress. If you have a poor stress response, cortisol can be too high or too low. If cortisol goes up due to stress, your progesterone levels can take a tumble.
Strategies to Reduce Anxiety and Panic Attacks
Here are some simple changes you can make to feel calmer and less anxious:
- Reset your inner clock. First thing in the morning, immerse yourself in bright outdoor sunlight without wearing sunglasses. After sundown, expose yourself to dim light. If you’re not doing these things, neither dietary supplements nor hormone replacement therapy will work.
- Let go of toxic people, habits, and behaviors
- Seek professional therapy
- Practice stress management techniques like transcendental meditation, hypnotherapy, somatic therapy, nature immersion, the Gupta Program, and psychedelic journeying.
Natural Hormone Replacement and Dietary Supplements for Stress
Natural Progesterone - Please email office to discuss
A functional medicine provider can prescribe personalized, low-dose bioidentical progesterone. This can relieve symptoms of histamine intolerance and estrogen dominance.
Vitamin B6 supplements can help with histamine balance including PMS related to histamine. Vitamin B6 can:
- Help produce progesterone.
- Promote GABA synthesis.
- Convert L-tyrosine and 5-hydroxytryptophan (5-HTP) to dopamine and serotonin, respectively.
- Enhance DAO production and lower histamine.
Start with 50 mg of vitamin B6 in the form of P5P. You can take more under the guidance of a functional medicine provider.
Magnesium is a natural stress reliever. I prefer the chelated form of glycinate and the product Neuro-Mag.
L-theanine, a substance found naturally in green tea, produces calming brain waves. Passionflower (Passiflora incarnata) also has soothing effects.
Taurine is an amino acid that promotes formation and release of GABA, which quiets down excitatory signals in the brain. A typical dose is 250 mg – 1,000 mg/day.
Best for acute panic attacks rather than chronic anxiety, glycine is an amino acid that interferes with the release of the neurotransmitter norepinephrine. At the first sign of a panic attack, place two grams of glycine powder under the tongue and let it slowly dissolve. This process can be repeated every few minutes if necessary and, in most cases, the problem will resolve within 10 to 15 minutes.
Cannabidiol (CBD)
This phytocannabinoid has calming, soothing effects. In human studies, CBD reduced anxiety caused by a public speaking test in subjects with social anxiety disorder.
This lavender-derived substance (also known as Silexan™) promotes relaxation and calms nervousness.
I Can Help Balance Hormones and Relieve Anxiety
To find out whether the root cause of your anxiety disorder and panic attacks is blood sugar issues, low progesterone, or problems with other hormones, you’re going to need an experienced functional medicine practitioner. The first step is to book a free 15-minute troubleshooting call with me.
If after the call you come on board as a patient, I’ll order the best tests for you and develop a treatment plan based on your unique biochemistry. You will find out the steps you need to take to feel calmer and happier. I know anxiety isn’t easy but together we’ll find a solution to make your life easier.
Endometriosis 101 Part 1: What Is this Condition & Why Is it Happening to Me?
Check out "Endometriosis 101 Part 2: How I Help My Patients Dealing with Endometriosis" HERE.
You might have heard me say this before: Your period is not a curse.
The truth is that your period is actually a sign of amazing things happening inside your body (regardless of if you ever even want kids!).
But…for some women, your period can feel like a curse from hell - all due to a condition called endometriosis.
Listen up ladies: If your periods are painful, long, heavy, and something you downright dread, please read this article.
If your doctor has told you they suspect endometriosis, please read this article.
If you’ve been suffering for YEARS without relief, please read this article.
One in 10 women in the U.S. is estimated to have endometriosis. (And it takes an average of 8-12 years to be diagnosed).
I won’t pretend I have a magic cure for endo (I wish I did!). But what I can do is share what I know, and assure you: You aren’t crazy. It does hurt. But it doesn’t have to be this bad forever.
This is a big topic, so I’m going to be covering it in two posts. Today, in Part 1, we’ll learn what endometriosis is, its symptoms, and what we (think) causes it. Part 2 will be all about actionable solutions you can put into practice right away.
What Is Endometriosis?
Have you ever wondered what your period is actually made of? It’s not just the same blood you see when you cut your finger - it’s actually endometrial tissue. Over the course of the month, women grow endometrial tissue in the lining of the uterus. When you have your period, that tissue is shed. (If you get pregnant, that endometrial tissue is important for supporting the fetus).
Endometrial tissue is “hormonally responsive” which means it reacts to normal hormone changes that come with your monthly cycle. Blood flow is controlled by inflammatory compounds called prostaglandins.
A normal woman grows endometrial tissue in the uterus and then sheds it during her period. It’s all relatively painless.
But in a woman with endometriosis, the endometrial tissue grows outside the uterus. Most commonly it grows around the fallopian tubes and ovaries, but it can extend into the digestive system and really start growing anywhere in the body.
Endometrial tissue is hormonally responsive no matter where it is in the body - when hormone levels fluctuate (as they should to create your monthly cycle), all endometrial tissue (even that which has overgrown) will respond.
That means more inflammatory prostaglandins leading to pain, inflammation, and even scar tissue (adhesions) where endometrial tissue is located.
This can cause extreme pain during your period, from ovulation through your period, mid-cycle, and, for some women, all month long.
Pain can range from mild to excruciating, and frustratingly, the extent of the endometriosis does not correlate with how severe symptoms are. A little endometriosis can cause a LOT of pain.
Aside from pain, endometriosis regularly causes digestive issues and can impact fertility. It also increases PMS.
It’s estimated, however, that 20-25% of women with endometriosis have no symptoms. They may only be diagnosed when they have fertility issues.
If you do have extremely painful periods, heavy bleeding, and even symptoms like IBS that haven’t responded to treatment, please know that it is not normal and can be a sign of endometriosis. It takes the average woman 8-12 years to be diagnosed with endo. That's 8-12 years of suffering you shouldn’t have to endure!
What Causes Endometriosis?
The sad truth is that we don’t know for sure what causes endometriosis. Both traditional and functional medicine practitioners agree on certain things - but there’s no one proven cause.
While not currently classified as an autoimmune disease, endometriosis is known to have autoimmune features. It is also known to be related to hormone imbalance.
One other theory is about retrograde blood flow - basically when blood flow washes back up into the uterus and fallopian tubes. But, not all women who have some degree of retrograde blood flow develop endo - which means retrograde blood flow is just one of the mechanisms of endometriosis.
Because there isn’t a good understanding of what causes endometriosis in traditional medicine, most traditional solutions are focused on pain and symptom management...
Traditional Endometriosis Treatments (The Good, Bad & Ugly)
In traditional medicine, typical endometriosis treatments include:
- Oral contraceptives or the hormonal IUD (to block ovulation)
- Pain management (Ibuprofen, etc.)
- Surgery (ablation to remove endometriosis and even complete hysterectomy)
I will never shame a woman for using any of these treatments, and I think (at times) they have merit.
The biggest “red flag” is using oral contraceptives to block ovulation. Like with other conditions, oral contraceptives just work as a “band-aid” and do not address underlying causes. When you stop the pill, symptoms will resume. And because the artificial progestins in birth control can exacerbate estrogen dominance, long-term oral contraceptives can make endometriosis worse.
Not to mention that oral contraceptives can be just as damaging to the gut as antibiotics, and that can exacerbate leaky gut!
Are you using oral contraceptives to manage endometriosis? I’d love to explore what other treatment options are available to you. Book a free 15-minute consult with my team today.
Ablation surgery, on the other hand, can be transformative for women who have progressed endometriosis - and can even restore fertility in some cases! However, I think surgery should always be accompanied by other approaches to address underlying causes and inflammation.
I think a total hysterectomy is unfortunate…and I hope that most women with endometriosis don’t get to the point where such an extreme surgery seems like the only answer. In Chinese medicine, the uterus is considered the second heart, and a recent study showed women who had hysterectomies had higher rates of depression.
And while there is nothing wrong with pain management, functional practitioners like myself tend to focus more on suspected root causes of endo so that we can move beyond just pain management and toward resolution of symptoms.
Let’s talk about that now...
A Functional Perspective On What Causes Endometriosis
I often call endometriosis a disease of hormone imbalance. Specifically, endometriosis is associated with estrogen dominance due to low progesterone (where estrogen becomes high relative to low progesterone).
Low progesterone can have many causes. The most common I see are genetic, due to extended use of hormonal contraceptives (which tend to increase estrogen and decrease progesterone), and as a result of chronic stress. If you have adrenal dysfunction or HPA axis dysfunction, your body may downregulate progesterone to prevent conception during stress.
What you might not know is that estrogen dominance is a component of many autoimmune conditions. (And that may be why autoimmunity is more common in men than women). This might be because high estrogen levels are inflammatory.
Like I mentioned earlier, endometriosis isn’t considered an autoimmune disease (yet). But it definitely has the “hallmarks” of autoimmunity: inflammation and immune dysregulation.
With endometriosis specifically, there is both a localized, chronic inflammation and the presence of self-antibodies. What we don’t yet know is if this is a response to endometriosis or the actual cause of endometriosis.
But we do know that there is also an increased number cytokines, an inflammatory component, and lower levels of apoptosis, which means cells aren’t dying at a normal rate.
All of this points to autoimmune - as does the fact that endometriosis also frequently occurs alongside other autoimmune diseases like MS, Hashimoto’s, lupus, and Inflammatory Bowel Diseases like Crohn’s and Ulcerative Colitis.
Research at the University of Tennessee has also shown that 100% of women with endometriosis also have leaky gut. (This doesn’t mean 100% of women in the world have leaky gut if they endometriosis - just women in the study - but it is a compelling number!)
That makes sense, since functional practitioners have long seen a strong link between leaky gut and the development of all kinds of autoimmune conditions.
I Have Endometriosis…Now What?
I never want to see another woman with endometriosis given a prescription for the Pill and a suggestion for a heating pad as a “solution” ever again.
As a functional medicine practitioner, my mission is to help you address endometriosis holistically.
Make sure you check out part 2 of this article for more information on exactly how I support my patients with endometriosis.
P.S. Also be sure to listen to my guest podcast appearance where I spoke with Tawnee Gibson of Endurance Planet all about endometriosis! Listen here.
How To Treat Depression & Anxiety Holistically - Part Two
In Part One of this series, I delved into the fact that depression and anxiety are not problems of JUST the brain or JUST the body. There is a definite mind-body connection, and the best treatments (and prevention) for depression and anxiety treat both. I also started going into the root causes – everything from childhood trauma to candida – and the solutions that might be able to help you. If you haven't read Part One yet, click here to go back and check it out!
Lots of people think “holistic” = “natural” or “alternative.”
But that’s not actually what holistic means!
A “holistic” approach looks at a person as a whole. Rather than seeing each part of the person - say their digestive system, or hormones, or mental health - as separate entities, holistic medicine views them all as interconnected.
(Sometimes, that does mean we use natural and alternative approaches to healing.)
But it always means that we’re looking at YOU as a whole person and not just a set of symptoms or a diagnosis.
I think that’s so important to make clear as I dive into the 2nd part of my series on treating depression and anxiety holistically.
Today, I’m going to explore how environmental exposure to toxins and hormone imbalances can play a role in depression and anxiety. It might seem crazy to think your detox pathways or PCOS could be related to depression or anxiety - but they can! Today I’ll explain exactly how and what you can do about it.
If you haven’t read Part 1 of my series, go HERE and read it first! Then come back and dig into Part 2!
What Toxins Are (And Aren’t)
Toxins is one of those words that gets thrown around a lot. But what does it really mean?
A toxin is any chemical or compound that has noxious or harmful effects on living organisms.
Toxins can come from outside us (our environment) but they can also be generated internally. For example, our hormones can become toxins if they stick around too long. They must all be “detoxified” - broken down and cleared from the body in order to make room for new fresh hormones to be produced. We also produce toxins in the gut.
But, the major source of toxins is the outside environment.
We have THOUSANDS of toxin exposures every single day. Here are just some of the most common ones:
- Smog in the air we breathe
- Touching receipts coated with chemicals
- Pesticide residue on food
- Prescription medicine contamination in drinking water
- Hair & beauty products made with dangerous chemicals
The EPA estimates that in 2014, 4 billion pounds of toxic chemical waste was released into the air, water or placed in some type of land disposal in the U.S.
(And they consider this an IMPROVEMENT over the 4.7 billion pounds released in 2002!)
It’s likely that at least 25% of the United States population is dealing with heavy metal poisoning, too.
And while our body is equipped to deal with toxins (that’s what our liver is for!) the amount of toxic exposure humans have today is overwhelming. That’s why so many people's detox systems are overburdened. We can’t detox at a rate fast enough to keep up with all the toxins coming in!
This leads to fatigue, allergies, skin reactions, accelerated aging, autoimmunity, brain fog, yeast and bacterial overgrowths, and… increased depression and anxiety.
How Toxins Mess With Our Brains
The brain is a powerful and vulnerable organ.
The brain is made of nearly 60% fat. And that’s a problem - because many chemicals and toxins are fat soluble (including the nefarious heavy metals!).
The brain is so susceptible to toxin damage that there’s a specific name for toxins that negatively impact the brain neurons’ function: neurotoxins.
Neurotoxin exposure is a direct cause of depression and anxiety because they cause neurotransmitter dysfunction and inflame the brain.
This creates problems with brain signaling.
Neurons work by secreting specific brain chemicals (primarily serotonin and dopamine) out of the end of one neuron (called vesicle) into the space between the neurons (called the synapse).
Ideally, these chemicals are taken up by the receptor sites on the next neuron meant to receive the message. When that happens, a response signal is stimulated, and it continues on down the line to next neuron. If too much of any one brain chemical is released, it should be reabsorbed into the storage vesicles. This is called reuptake.
It’s sort of like your neurons are all playing a game of telephone.
But when toxins get in the way, the game gets messed up. The next neuron can’t hear the message clearly and passes it on wrong - or maybe not at all.
The toxins (and the inflammation caused by them) block the receptor sites on the neurons from taking up the chemicals - aka “hearing the message.” Your neurons don’t get the signal.
And that means you don’t feel the effects of serotonin or dopamine, because they aren’t able to do their job.
Then, the serotonin and dopamine that should have been taken up start building up in the synapse.
Your body goes into action: it knows it can’t let too much of these chemicals accumulate. It starts creating enzymes to break down the serotonin and dopamine that are stuck in synapse.
The end result? Your reserves of serotonin and dopamine are lowered.
Depression and anxiety are both a result of the receptor sites in your brain being “shut down” and the lowered serotonin and dopamine this ultimately causes.
Signs Your Detox System is Overburdened and Needs Help
If you’re dealing with symptoms of depression or anxiety, it’s a sign your detox systems could be overburdened - along with these other signs:
- Memory, concentration, and focus problems
- ADD or ADHD
- Skin problems (acne, eczema, psoriasis, hives, rashes)
- Fatigue
- Overeating & food cravings
- Autoimmune conditions
- Feeling chronically flu-like
- Yeast overgrowth (Candida)
- Bacterial overgrowth (SIBO)
- Food intolerances
But - all of these symptoms can be related to OTHER problems as well - which is why it’s so important to get accurate lab testing, and not just guess at a diagnosis based on symptoms.
Here’s what I commonly see with my patients:
A patient with depression or anxiety will also have digestive tract infections or dysbiosis, yeast overgrowth, or food intolerances.
These promote inflammation in the gut, and the inflammatory cytokines circulate in the blood and travel into the brain across the blood brain barrier, impacting brain function.
(What do I do to help? Glad you asked! After testing, I use specific amino acids like 5-HTP, tyrosine, and GABA, plus nutrient cofactors to deal with shut-down receptor sites and neurotransmitter deficiency. At the same time, I’m addressing underlying root causes of the gut infections.)
How To Address Depression & Anxiety Related To Toxin Exposure
The solution to depression and anxiety caused by toxin exposure is to address the cause of the inflammation: those toxins!
That means limiting exposure as much as you can: get a water filter, air purifier, buy organic, switch to natural beauty products, etc.
From there, I start by enhancing detoxification pathways with nutrient protocols, hydration, herbs, saunas, skin brushing, and lymphatic system support so the toxins can be broken down and excreted from the body.
Next, I use lab testing to identify where in the detox pathway things are getting gummed up. Is your Phase 1 or Phase 2 liver detox malfunctioning? Proper testing can tell us!
I also use Organic Acids Testing and Heavy Metals testing to see exactly what toxins you’re dealing with.
I have to give a warning here: you MUST be careful when doing detox work. It can be dangerous to stimulate detox and have the body suddenly dump toxins from storage into circulation.
It’s never good to detox someone who still has a leaky gut or gut issues - and it can make your gut issues get worse.
You shouldn’t feel sick when detoxing - this usually indicates pulling toxins out of storage faster than your body can clear them.
An experienced practitioner can help you detox safely.
Depression, Anxiety & Hormones
I’ve saved the best (worst?) for last: hormones!
On some level, almost all depression & anxiety is related to hormone imbalances.
Neuroscientists at the National Institute of Mental Health have even stated that most depression in the United States is caused or contributed to by HPA-axis dysregulation (also called adrenal fatigue) and hormone imbalances.
The most important players for depression and anxiety are cortisol, DHEA, testosterone, estrogen, and progesterone. Together they can trigger a biochemically-induced depression.
Cortisol Dysfunction
Cortisol is a stress hormone that’s has to be just right. Too high or too low, and you can have lots of problems. But it’s tricky because your cortisol levels shouldn’t be steady throughout the day: they should follow a predictable arc of rising quickly in the morning when you’re exposed to light and slowly lowering throughout the day.
(That’s why cortisol problems can be easily overlooked! You can’t just look at one reading - you need to look at both levels throughout the day, and the rate at which they rise and fall to get the complete picture of cortisol health.)
Low cortisol levels are related to depression - and in particular, are linked to postpartum depression. Low CAR response (the rise of cortisol first thing in the morning) can also be related to depression.
But - high cortisol (especially high at nighttime) is also related to depression - both high and low levels can cause similar symptoms. Again - that’s why you must have accurate testing!
What messes up cortisol levels?
The big triggers for cortisol imbalances are are sustained and chronic stress! It can be mental OR physical stress - anything from a stressful job, being a super-busy new mom, or over-exercising can wreak havoc on cortisol levels.
Sex Hormones Imbalances
Progesterone, estrogen, and testosterone are the primary sex hormones - but they can also have a huge impact on mental health and depression and anxiety in particular.
Here are just a few of the many ways sex hormones can directly impact mental health:
Progesterone helps balance blood sugar levels. Remember - the brain is dependent on adequate glucose to function. Low progesterone levels can lower the supply of glucose available to the brain. This decrease in "brain fuel" contributes to the most common psychological and emotional symptoms of PMS like:
- Irritability
- Rage
- Depression
- Tension
- Anxiety
- Confusion
- Fatigue
- Memory lapses and loss
- Inability to concentrate
- Decreased stress tolerance
Estrogen and progesterone also have a strong effect on the neurotransmitters involved in mood regulation:
- Progesterone binds GABA receptors (which decreases anxiety and depression)
- Progesterone raises serotonin hormone levels in brain
- Estrogen increases dopamine activity in the brain
That means, any change in hormone levels (even subtle ones!) can contribute to psychological symptoms.
Unfortunately, the treatment given to many women who do experience mood symptoms with their monthly cycle is the hormonal birth control pill.
This drives me crazy as it only compounds the problem!
Birth control pills deplete the body of essential vitamins and minerals like folate, b vitamins, and magnesium - all of which are involved in the synthesis of chemicals for brain health (among other things!).
This can result in intensified depression, anxiety and PMS! A number of studies have linked depression with the use of oral contraception.
Studies have also indicated that using the Pill for extended periods of time can alter the gut microbiome, especially predisposing users to candida overgrowth and other bacterial and fungal issues.
The nutrient deficiencies that are induced by the Pill are largely due to the influence on the gut microbes, where many of these nutrients are synthesized. (So again, many of these issues point back to the gut - make sure you read Part 1 of this series!)
But that’s not all…
Thyroid Problems
Every cell in your body has receptors for thyroid hormone - including the brain!
(That should give you a clue to how essential a healthy thyroid is for overall well-being!)
Thyroid hormone makes progesterone receptors more sensitive. This means that low thyroid hormone can mimic the symptoms of low progesterone. (Remember the fun PMS stuff we talked about in the previous section??)
Low thyroid hormone can also directly impact neurotransmitter levels. It can cause low dopamine levels - which translates to lack of motivation, drive, and willpower.
Taking Control Of Anxiety & Depression
No matter what root cause (or causes) of depression and anxiety you’re dealing with, there are certain steps you take with your diet and lifestyle to help alleviate symptoms.
For some of my clients, just making lifestyle and diet changes is enough to completely alleviate symptoms of depression and anxiety! Here are some things to try in all the major categories:
Eat:
- Eat plenty of healthy fats (like avocado, coconut, and olive oil)
- Avoid processed foods and excessive sugar
- Some people can benefit from removing dairy & gluten
- Choose organic foods (especially the Dirty Dozen)
- Aim for 10 servings of fruits & veggies per day
- Focus on eating for balanced blood sugar (avoiding processed carbs!)
Move:
- Exercise has been shown to be as effective in most cases as antidepressant drugs for alleviating depression
- Find what works for you and what you ENJOY doing
- If you haven’t been exercising regularly, just start with 20-30 minute walks daily
Sleep:
- Turn off screens 1 hour before bedtime
- Schedule enough time for enough hours (8 hours or more)
- Sleep in a dark room, with the temperature slightly cooler
Stress:
- Active stress management is something I recommend for ALL my clients (no matter what health concern they have)
- Meditation, yoga, tai chi or qi gong, making art, dance, journaling are some of my favorite options for managing stress
- Making a conscious decision to “switch” from fight-or-flight mode to rest-and-digest mode
- Consider working with a counselor or therapist - especially if unresolved emotional issues are a factor for you
Next Steps For Treating Anxiety & Depression
After reading Part 1 and Part 2 of this series, you might be feeling a little overwhelmed.
It seems like you could have hormone issues, toxin exposure, gut issues, and maybe yeast overgrowth, too! (Plus there’s definitely some past trauma lurking that needs to be dealt with….)
As one of my mentors in Chinese medical school used to say: “You are entitled to more than one problem at the same time!”
The truth is that while some people have one primary cause, the majority of depression or anxiety cases is due to a “perfect storm” of factors.
Everything we’ve discussed in this series can be interrelated:
- Having dysregulated cortisol levels can not only contribute to changes in the brain and brain chemistry, but can alter the way the immune system operates, leaving us more prone to inflammation and more vulnerable to infections in the gut
- Having a leaky gut from food intolerances or infections will affect the brain directly, but will also be a major contributor to detox system overwhelm
- Having low thyroid function can cause symptoms of low progesterone
The complex way all these systems interacts means one thing: you don’t want to go this alone!
I really believe everyone should have a trusted practitioner by their side, guiding them through the process of healing.
The right practitioner (trained in a holistic approach like Functional Medicine) can untangle the strings of depression and anxiety and get back to feeling like yourself!
If this resonates with you, I’d be honored to have you book a 20-minute consult with my team. These consults are totally free and a chance for us to share how we are trained to help you!
→ Learn more and book a free consult with my team here.
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
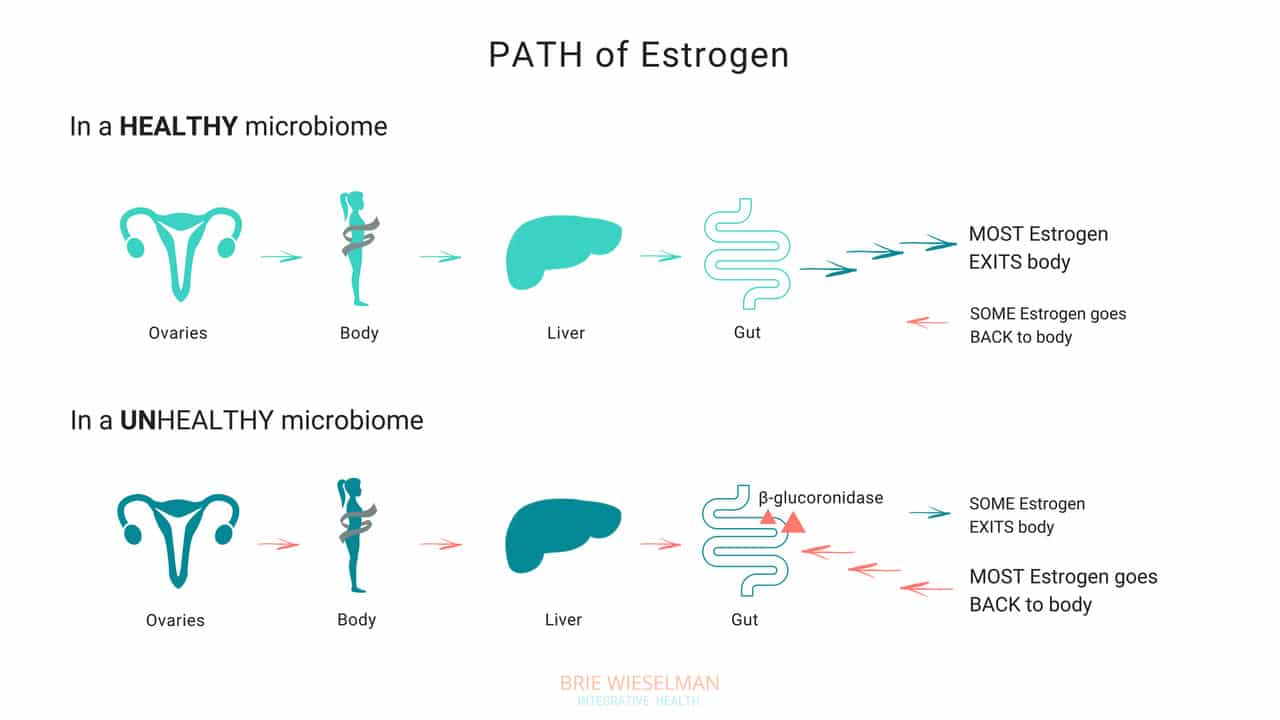
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.




