Harnessing the Power of Hormones: Menopause, Weight Management, and Beyond
As women navigate the winding path of perimenopause and enter the world of menopause, a whole gamut of changes start to occur within their bodies. These changes are mostly driven by shifts in hormone levels, most notably, the decline in estrogen. One area of our health that takes a significant hit during this time is weight management. It’s as if an internal switch has been flicked, and suddenly, maintaining a steady weight becomes a challenge. Who’s body is this? When did these jeans get too small?
But why does this happen? And is there anything we can do about it?
Estrogen, Appetite, and Weight
Estrogen, one of the primary female sex hormones, performs numerous functions beyond its role in reproductive health. It is intricately linked with our metabolic health, affecting how our cells convert glucose into energy.
During the perimenopausal transition, estrogen levels decline, leading to what we could call a "temporary energy crisis". Our cells find it harder to convert glucose into energy, which can trigger increased appetite, hot flashes, and night sweats. The latter can disrupt sleep, which can then further exacerbate these symptoms. This combination of physical discomfort and heightened appetite often leads to overeating or binge eating, contributing to weight gain.
The Glucose-Ketone Transition
As estrogen levels decrease, our bodies need to adapt to this new metabolic environment. The hormone estradiol, a form of estrogen, usually increases glucose sensitivity by enhancing the ability of mitochondria (the powerhouses of our cells) to turn glucose into energy.
With the decline in estrogen levels, our cells have to switch from burning glucose to burning ketones. This switch requires a certain degree of "metabolic flexibility". If the brain can adapt to a higher ketone state, the symptoms should be temporary. However, if the body cannot adapt due to whole-body insulin resistance, this can potentially lead to more serious conditions such as dementia.
What Are Ketones?
Ketones are produced in the liver from the breakdown of fats. This production occurs in the absence of glucose, which comes from sugars and carbohydrates. This process can occur overnight, during fasting, or when we eat meals that are primarily made up of proteins and fats, without adding more than 5 grams of carbohydrates.
Embracing Metabolic Flexibility for a Healthier Perimenopause
Metabolic flexibility is your body's ability to switch between using glucose or ketones as a fuel source. This flexibility is essential, especially during the perimenopause transition, as it allows your body to adapt to changing hormone levels and efficiently use available energy sources.
When your body can seamlessly shift from glucose to ketones, you can experience fewer menopausal symptoms, improved energy levels, and better weight management. Here are some strategies that can enhance your metabolic flexibility:
Dietary Approaches
The foods we consume play a crucial role in how our bodies metabolize energy. Specific types of diets can enhance metabolic flexibility by optimizing your body's ability to switch between glucose and ketones.
Low-Carbohydrate, High-Fat Diets (LCHF)
These diets, such as the ketogenic diet, are designed to shift your body's primary fuel source from glucose to ketones. By reducing carbohydrate intake and increasing healthy fats, you can stimulate your liver to produce ketones more efficiently, promoting metabolic flexibility.
Mediterranean Diet
This diet emphasizes fruits, vegetables, whole grains, legumes, and healthy fats, like olive oil and fatty fish. It's rich in nutrients that support metabolic health and can enhance insulin sensitivity, a crucial aspect of metabolic flexibility.
Fasting
Intermittent fasting, whether it's time-restricted eating or alternate-day fasting, gives your body a break from processing food. This pause allows your body to deplete its glucose stores and start producing and using ketones, increasing metabolic flexibility.
Resistance Training
Physical activity, especially resistance or strength training, can boost your metabolic flexibility by enhancing insulin sensitivity and promoting muscle growth. Having more muscle mass means your body can store more glucose, thus reducing the likelihood of insulin resistance.
Lifestyle Steps
Implementing simple lifestyle changes can also greatly enhance your metabolic flexibility.
Adequate Sleep
Sleep deprivation can lead to insulin resistance, impairing your metabolic flexibility. Aim for 7-9 hours of quality sleep per night.
Stress Management
Chronic stress can negatively impact your metabolic health, including your body's ability to switch between fuel sources. Regular mindfulness practices, like yoga or meditation, can help manage stress levels.
Empower your journey through perimenopause by improving your metabolic flexibility. Our group program integrates these dietary, physical activity, and lifestyle approaches, providing a comprehensive plan to help you navigate this transition with grace and strength.
Why wait? Book a discovery call with us today. It’s time to take control of your health and embrace a brighter, leaner, and more energetic you during perimenopause and beyond.
Your Path to a Healthy Perimenopause
Understanding these complex processes is the first step towards taking control of your health during perimenopause and beyond. There are ways to navigate these changes and manage the symptoms effectively.
The transition into menopause should not equate to giving up on your health goals. This is a time for empowerment, for harnessing the change and using it to propel yourself into a phase of increased longevity, youthful skin, solid energy, a fiercely sharp brain, and a lean body.
Our group program is designed specifically for women in perimenopause who want to 'reverse-age'. Our scientifically-backed strategies will help you adapt to the hormonal changes, improve your metabolic flexibility, and help you avoid weight gain. Better yet, we understand that your body is not identical to the next woman’s body and metabolism, and we utilize state of the art lab testing to personalize your protocol for longevity optimization and reclaiming your body, energy, mind, and beautiful skin.
I encourage you to take this journey with us. Book a discovery call today, and let’s work together to not just weather the menopausal transition, but to thrive through it. Embrace this change as an opportunity to become the best version of yourself. Because you deserve nothing less.
Pros and Cons of Hormone Replacement Therapy
Mood swings, hot flashes, nigh sweats, weight gain, loss of libido: these are just some of the most common “symptoms” of menopause.
Is it any wonder most women dread this transition?
But what if there was a way to skirt menopauses negative side effects completely, and sail through this major change without sweating, screaming, or stress? According to some, the secret to making it through menopause is hormone replacement therapy (HRT).
But is hormone replacement therapy right for you? Today, let’s talk what happens in the body on the hormonal and chemical level during perimenopuase and menopause, how hormone replacement can and can’t help, and options you have to support this transition even if you’re not interested in HRT.
Menopause vs. Perimenopause: What’s The Difference?
Menopause is defined as going 12 or more months without a menstrual cycle. Perimenopause is the time period - usually several years - leading up to menopause. It’s a transition period sometimes thought of as “puberty in reverse.”
The average age of menopause in the Untied States is 51, and perimenopause usually stars 4-10 years before that. For some women, perimenopause symptoms begin as early as age 35. And if you need another reason to quit, research has shown smokers reach menopause at a younger age than non-smokers.
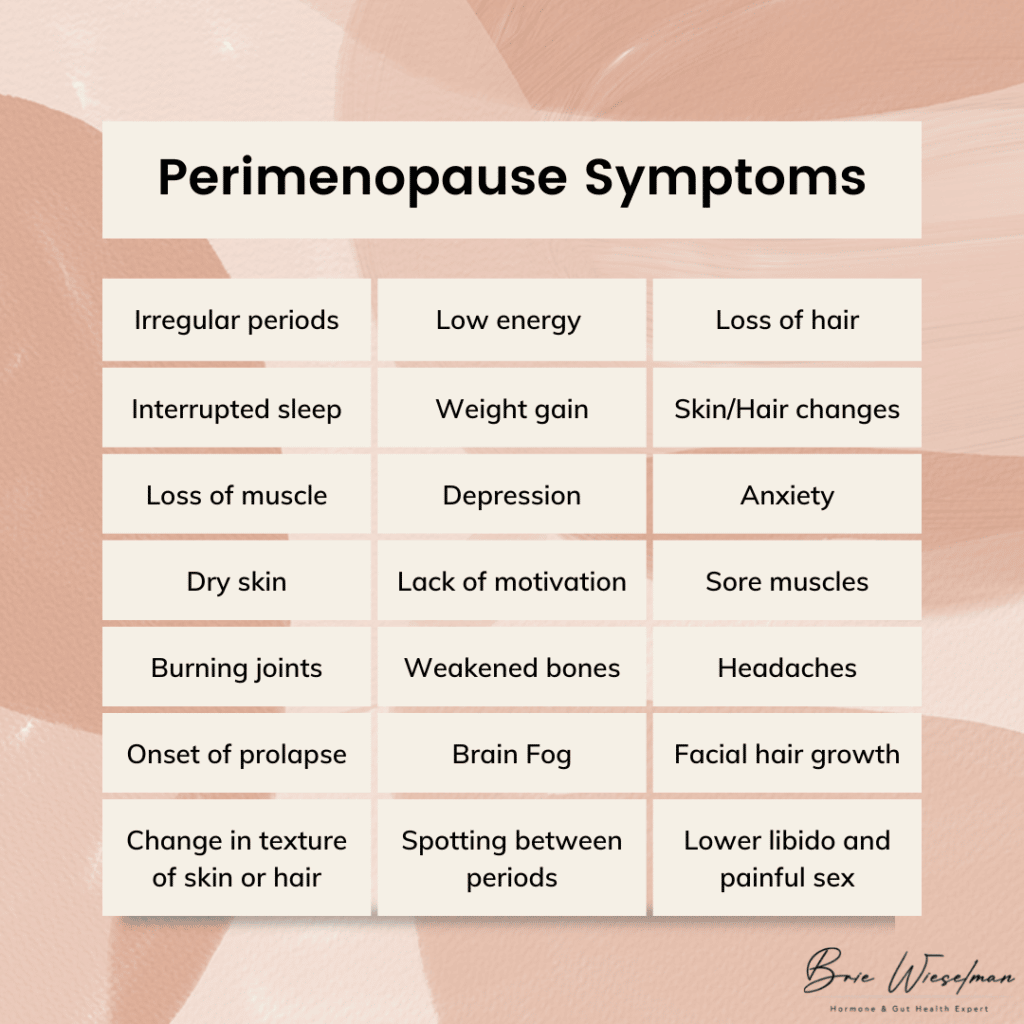 Perimenopause symptoms include:
Perimenopause symptoms include:
- More frequent or heavier periods or missing or less frequent periods
- Interrupted sleep
- Low energy
- Night sweats/hot flashes
- Weight gain
- Change in texture of skin or hair
- Loss of muscle
- Irritability and depression
- Anxiety
- Lack of motivation
- Dry skin
- Sore muscles
- Burning joints
- Weakened bones
- Lower libido and painful sex
- Headaches
- Onset or worsening of prolapse
- Spotting between periods
- Facial hair growth (especially on the chin)
- Loss of hair (on the head)
- Brain fog
Of course, not every woman has every symptom, and it’s not an overnight onslaught. Usually, the first signs of perimenopause are a slightly shortened cycle (think 21-24 days instead of 28) and an increase in PMS symptoms and irritability.
The Hormonal Changes That Cause Menopause
So what is actually happening in the body to cause everything from weight gain to hair loss?
To start, let’s talk about the normal hormone cycle that occurs each month. It all starts in the brain when the hypothalamus signals the pituitary gland via gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In turn, LH and FSH tell the ovaries it’s time to ovulate and release an egg from the follicle. Ovulation triggers the release of estrogen and progesterone. The release of estrogen and progesterone communicate back to the brain that the system has worked, creating a feedback loop.
During the reproductive years, GnRH is produced in a rhythmic cycle, leading to regular cycles. But as we age and enter perimenopause, the release of GnRH becomes more unpredictable. In addition, as we age the ovaries stop responding to LH, leading to erratic ovulation. Because ovulation is what triggers estrogen and progesterone, when ovulation becomes erratic, levels of these hormones drop.
This doesn't happen all at once, though: the changes are often up and down. At first, estrogen levels may shoot up high, then drop back down. Progesterone is only made via ovulation, so it may be irregular in the early stages of perimenopause before beginning a gradual decline. The decline of progesterone often occurs faster than estrogen, leading to temporary estrogen dominance in perimenopause, as well.
The loss of progesterone affects the brain, GABA system, and HPA axis. Allopregnanolone, one type of progesterone, has a calming effect on the brain. Without adequate levels of it, sleep disturbances and reduced ability to cope with stress can occur. The loss of progesterone can also contribute to autoimmunity, especially Hashimoto's thyroiditis. And without the anti-androgenic effect of progesterone, excess androgens can stimulate insulin, contributing to insulin resistance.
In addition to these changes, testosterone, which is produced in the ovaries and adrenal gland, continues to be produced after menopause (though it peaks in the 20s). It is common to go through a phase in perimenopause where testosterone is high relative to estrogen and progesterone, causing symptoms like hair loss, central abdominal weight gain/body shape change, and the onset or worsening of insulin resistance.
Some types of estrogen are produced outside the ovaries. Half of the body’s estrone (one type of estrogen) is made in the fat tissue and adrenal glands, and estrone becomes the predominant estrogen after menopause. This is good for bone density, brain tissue maintenance, and cardiovascular health - we need that estrone! This is why supporting adrenal health is so important for making it through menopause with optimal hormone levels (more on that to come).
The 4 Stages of Perimenopause
From a hormonal standpoint, I like to break perimenopause into 4 stages.
Stage 1: In this stage, estrogen is high, but progesterone levels have started to drop due to an increase in anovulatory cycles (when bleeding occurs and you have a “period” but your body doesn’t ovulate). The luteal phase is often shorter here, but periods might stay regular.
Stage 2: In this phase, estrogen levels are still high but start to fluctuate, causing symptoms associated with estrogen withdrawal, such as hot flashes, migraines, and night sweats. Cycle lengths may vary by as much as 7 days.
Stage 3: Stage 3 is marked by a significant increase in cycle length, going two or more months between cycles. The hormonal changes of Stage 2 remain and/or intensify, and estrogen remains high or rises and drops.
Stage 4: This final stage is often a waiting game: will you get your period again, or are you officially in menopause for good? Estrogen levels are low, unless you get a surprise period, which can raise levels back up temporarily.
Does Menopause Have to Be Miserable?
I could shout it from the rooftops: menopause is not a bad thing, and it doesn’t have to make you feel bad! If there is a menopause problem it’s simply that menopause and modern life are an evolutionary mismatch.
In comparison, the women of the remote Hadza tribe in Tanzania, who still practice hunting and gatherng as a subsistence pattern, don’t experience menopause the way American women do - in fact they report no symptoms associated with menopause, and don’t even have a name for this change.
How can that be? Some of the most important factors might be that Hadza women:
- Have robust gut microbiomes
- Have a strong sense of community and purpose
- Pre-menopausal women rest during their period
- Post-menopausal women eat less and walk more than pre-menopuasal women
- Spend more time pregnant and breastfeeding (and often transition directly from pregnancy/breastfeeding to perimenopause, softening the transition)
- Eat a foraged, high fiber diet without aunty farmed or processed foods
Fortunately, we don’t have to move off the grid to adapt some of these practices to our own lifestyles and reap the benefits. More on my suggestions for how to do this to come.
Understanding Hormone Replacement Therapy for Menopause and Perimenopause Symptoms
Hormone replacement therapy is the use of topical or oral estrogen, progesterone, and sometimes testosterone to temporarily increase hormone levels, treat the symptoms of perimenopause, and improve overall well-being.
Bioidentical hormone replacement therapy (B-HRT) is the use of replacement hormones that are identical to what the body produces. This is in contrast to the use of synthetic hormones, like those found in birth control pills.
As early as the 1930s, women were given placenta as a form of estrogen replacement therapy. In the 1940s, Premarin, a drug made from the urine of pregnant horses, was developed as a HRT. In the 1970s, studies linked estrogen therapy to endometrial cancer, revealing the importance of including progesterone to prevent estrogen-driven cancers.
From the 1960s to the 1990s, hormone replacement therapy grew in popularity. It was marketed as a way to stay youthful and feminine, and was widely used. But then, in the early 2000s, research showed HRT caused a slight increase in the risk of breast cancer, heart disease, stroke and blood clots.
Is Hormone Replacement Therapy Safe?
In 2002, a HRT trial was stopped early because of risks including a small increased risk of breast cancer, heart disease, stroke and blood clots, but fewer cases of hip fractures and colon cancer. This was followed by a 2003 report in the Lancet claiming the use of HRT increased the incidence of breast cancer, even though the data was not strong enough to document a clear harm.
This incomplete information created a change in public opinion that remains today: many women are hesitant to use HRT, even though we now know how to use it safely.
What we now know is that the most important factor for HRT safety is the age at which it is started. HRT is best started as young as possible, while in the perimenopausal window, and ideally continued for no more than 2 years beyond the last period. Starting HRT when older, or after the last period has occurred, increases the risk.
That’s why I’m glad you’re here reading this: if you want to start HRT, starting sooner is safer. But if you feel like you already missed your chance at HRT, and have now “aged out” - don’t give up hope. I have more suggestions for you at the end of this post.
In July 2017, the North American Menopause Society (NAMS) relased thier positon after reviewing the data amassed from millions of women usign HRT over several decades, and concluded the benefits of HRT outweigh the risk for healthy women, when HRT is started at the proper age. They found that being obese or having 4 or more alcohlic drinks per week actually increased the risk of breast cancer more than the proper use of HRT. Women using HRT had a 4 in 1000 chance of breast cancers vs a 3 in 1000 chance in women not using HRT.
In addition, they found there was no increased risk of heart attacks in women using HRT as long as they started taking HRT within 10 years of their last period or started between the age of 50 and 59.
In particular, bioidentical hormones are safer than synthetic hormones. Bioidentical progesterone likely decreases the risk of breast cancer, whereas synthetic progestins increase the risk. If started early in perimenopause, bioidentical hormones are actually heart protective as opposed to a risk factor for heart disease.
Pros and Cons of Hormone Replacement Therapy
When used correctly, the benefits of hormone replacement therapy include:
- Fewer hot flashes
- Improved insomnia & sleep disturbances
- Improved anxiety & depression
- Less brain fog
- Fewer menopausal symtoms in general
The primary cons are the potential slightly increased risk of breast cancer and heart disease.
When deciding to start hormone replacement therapy, there’s a lot to consider. Here’s some of what I go over with patients while developing a treatment plan:
- Age and proximity to menopause (starting earlier is generally better)
- History of breast cancer (self and family)
- Genetic predisposition to hormonal cancers
- Risk of cardiovascular disease (I screen for factor V and prothrombin in all patients before starting HRT)
The type of hormone therapy used matters, too. Options include pills, gels, creams, patches, troche, and liquids. While gels, creams, and patches are common , I actually prefer oral micronized progesterone, or, nanoliposomal topical serum. Most topical progesterones aren’t able to deliver a high enough dose to protect the uterine lining. In addition, there’s no “regular” rate of absorption for creams, gels, or patches. Each woman’s unique physiology determines how much and how fast she will absorb topical hormones. Topical progesterone can also be stored in the fat, then “dumped” by the body, leading to irregular levels in the blood, damaging the sensitive feedback loop in the brain. When used for longer periods of time, I’ve also seen fat-based topical progesterone build up to higher than physiologically normal levels, eventually causing progesterone receptor resistance, much like insulin resistance. When a woman has been using topical progesterone, has normal or even high levels when tested, but still has the symptoms of low progesterone, this is usually the reason.
Whatever form you choose, careful monitoring before, during and after use is an absolute must. After initial testing, hormones should be retested within 3 months of starting HRT to assess if levels need adjusting, as well as how estrogens are metabolized. Women often assume they need estrogen, but actually just need progesterone to start, as progesterone is often low relative to estrogen in early menopause. Progesterone can help with symptoms like night sweats and hot flashes just as much (if not more) than estrogen. When estrogen is needed, estradiol and estriol are both very safe when used in combination with progesterone.
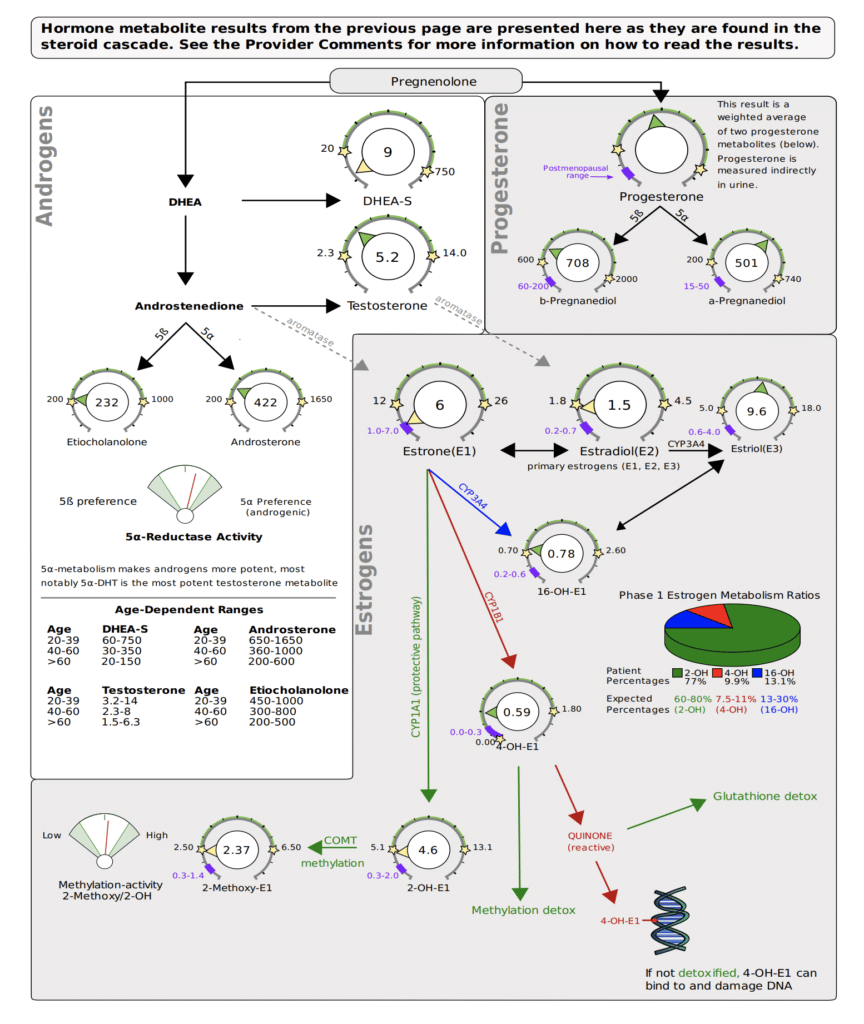
I use the DUTCH Complete Estrogen metabolism test, and look to make 2-OH as high or higher than all types of estrogen and other metabolites, for optimal, safe metabolism.
I also want 4-OH to be moderate to lower, at least not higher than 2-OH.
Alternatives & Complements to Hormone Replacement Therapy
Ready to start hormone replacement therapy? You’ll get the best results when also addressing your glucose, gut, and adrenal health in check, while paying attention to your diet, exercise, social life, and life purpose.
But even if you decide against HRT, addressing these other aspects of your health can have a radical impact on how you feel during perimenopause and menopause.
Eat For Balanced Blood Sugar
Research has linked hot flashes to insulin resistance, finding that glucose levels and the degree of insulin resistance rose as the frequency of hot flashes rose. Glucose levels were 33% higher in women who reported hot flashes 1 to 5 days per week than in those who reported no hot flashes. In another study of 6,000 menopausal women, diets high in fat and sugar led to a 20-percent increase in hot flashes and night sweats. After working with hundreds of women in my clinic, I’ve found that the more stable we keep their glucose levels, the fewer menopause symptoms they have.
Ditch Caffeine
There may be a link between caffeine use and certain menopause symptoms — namely, hot flashes and other symptoms related to the body's regulation of the diameter of blood vessels (vasomotor symptoms).
Avoid Spicy Foods
Like alcoholic beverages, spicy food causes vasodilation of the blood vessels, triggering hot flashes.
Eliminate or Reduce Alcohol
Cut back on drinks to 2 or less per week. When you do drink, expect to see menopause symptms return that night. (And surprisingly, wine is usually worse than clear spirits in this case - so maybe go with the vodka soda!) Cutting alcohol and sugar completely eliminates or minimizes night sweats and hot flashes in most women I see.
Exercise Regularly
Movement is always great, but it's most effective if you’ve been moving regularly in the time leading up to perimenopause, and then keep moving. Too much exercise or high intensity can actually trigger hot flashes because of the influence on blood flow to brain and skin and how the brain regulates body temperature.
Do Active Stress Management Daily
This can look like meditation, relaxation tracks, or hypnosis. CBT has also been shown to be very effective, especially in women who can’t use HRT due to breast cancer.
Support Gut Health
The gut plays a major role in the production and clearance of hormones. I always recommend a comprehensive gut health test and gut health practices like using a probiotic.
Try Phytoestrogen Foods
In some cases, phytoestrogen-rich foods like soy and legumes can be helpful.
Rehab Your Adrenals
Your adrenals are responsible for synthesizing appropriate levels of testosterone, progesterone, and estrogen in the perimenopause transition and beyond. Test your hormones with a DUTCH Complete panel and work with a practitioner who can create a customized protocol to rehab your adrenal hormone function.
Get Personalized Help with Hormone Replacement Therapy & Menopause
If you’re entering perimenopause (or already in the thick of it), hormone replacement therapy can help ease the transition. But even if you’re not ready (or not interested in) HRT, using diet, lifestyle, and herbs can help significantly. Either way, you don’t have to just accept the night sweats, hot flashes, weight gain, and mood swings - we can help!
If you’re looking for support in menopause, perimenopause, HRT, or natural alternatives to HRT, click here to book a free consult with our team.
We’ve helped hundreds of women in this life transition, and we’d be honored to help you, too.
Natural Treatment of PMS and PMDD
Raise your hand if you struggle with menstrual cramps, painful periods, irritability, mood swings, depression, and more the days and weeks leading up to your period.
If you raised your hand, you are not alone!
Nearly 90% of all menstruating women in the United States experience premenstrual syndrome (PMS) in their lifetime. And approximately 3% of those women experience such severe symptoms that they can be categorized as having premenstrual dysphoric disorder (PMDD).
Contrary to what some people may think, PMS and PMDD are real conditions. They can cause significant physical discomfort, impact your mental and emotional health, and disrupt your daily life.
Below, we’ll review the symptoms, causes of PMS and PMDD and how to naturally treat them.
What are PMS and PMDD?
PMS is a group of symptoms that many women experience during the luteal phase of their menstrual cycle. Typically starting around ovulation and ending the first day of their period.
PMDD, on the other hand, is a type of PMS but the symptoms are much more severe. Women who suffer from PMDD experience a decreased response to the body’s inhibitory molecule, GABA, which helps to limit activity associated with stress and anxiety. Causing women to experience five or more common PMS symptoms for seven or more days.
PMS and PMDD Symptoms
PMS can begin a few days or up to two weeks before the start of a woman’s period with mild to moderate symptoms. These symptoms only occur within those two weeks and are not present during the rest of the month.
PMS can present with a variety of physical, emotional, and cognitive symptoms including:
- Bloating
- Headache
- Fatigue
- Acne flare-ups
- Breast tenderness
- Mood swings
- Depression or anxiety
- Changes in appetite
- Insomnia
- Constipation or diarrhea
PMDD shares many of the same symptoms as PMS, but these symptoms are much more severe. These symptoms can be so severe that they disrupt tasks of daily living. And, many women experience very little relief from common over-the-counter medications.
What Causes PMS and PMDD?
Scientific research hasn’t conclusively identified the cause of PMS or PMDD. Nor has it determined why some women experience it more severely than others. But, research has suggested several different theories as to what causes PMS and PMDD.
Hormonal changes that occur during the menstrual cycle:
Many believe that PMS occurs in response to the changing levels of the hormones estrogen and progesterone. Also referred to as the sex hormones.
These hormonal fluctuations are thought to increase anxiety, irritability, and other mood changes experienced before your period.
Interaction between sex hormones and neurotransmitters:
The fluctuating levels of the sex hormones can impact the brain chemicals serotonin, dopamine, and GABA. Estrogen is required to synthesize serotonin and increases the number of serotonin receptors in the brain. Whereas progesterone helps stimulate dopamine release and increase GABA function.
Because both estrogen and progesterone levels drop before your period, the production and the effect of these “feel-good” chemicals are impacted. Leading to increased anxiety, changes in mood, and insomnia.
In women who struggle with PMDD, progesterone alters the shape of their GABA receptors making it harder for GABA to bind to them and improve mood, depression, or anxiety.
Other contributing factors:
There are other contributing factors that could lead to both PMS and PMDD including:
- Genetics – There are hundreds of genes that help eliminate toxins from our bodies. One example is the COMT gene which helps to eliminate estrogen from your body. Those with the slow COMT gene mutation struggle to eliminate excess estrogen and can experience endometriosis, strong PMS, and fibroids to name a few.
- Weight – No matter the cause for being overweight, an increase in fatty tissue equals an increase in hormones. Increased production of estrogen can cause inflammatory responses in the body and promote many PMS symptoms.
- Estrogen Dominance – If the gut is not processing estrogen or the liver is unable to detox estrogen, the body will have an increased level of estrogen relative to progesterone.
- Detox Issues – If the liver is unable to detox excess estrogen it may be too stressed and require you to decrease your toxin load in other ways.
- Gut Health – Our intestines are filled with trillions of bacterial cells (known as the microbiome) that work together to regulate the production, metabolism, and detoxification of hormones. When the microbiome is disturbed and the bacteria is damaged, dysbiosis can occur. Learn more about the importance of gut health and hormones here.
- Histamine Intolerance – How your body reacts to the foods you eat can be driven by hormone fluctuations. Estrogen dominance can increase histamine and adequate progesterone can help balance it out.
Diagnosing PMS and PMDD
There is no definitive test to diagnose PMS or PMDD. However, there are several screening tools I used when diagnosing PMS and PMDD.
- Estrogen and Progesterone – DUTCH test or a serum blood test done seven days post ovulation to evaluate your estrogen and progesterone levels.
- Adrenal Testing – DUTCH test to evaluate your adrenal health and confirm you are not experiencing an HPA axis dysregulation.
- Thyroid – You need adequate amounts of thyroid hormones for your ovaries to make progesterone. Progesterone also helps the thyroid function well. Research has reported that a high percentage of women with PMS also have hypothyroidism.
- Blood Glucose and Insulin Sensitivity – High blood sugar levels lead to high insulin levels which decreases the sex hormone-binding globulin (SHBG). If your insulin is always high there won’t be much SHBG causing estrogen and testosterone to rise relative to progesterone.
Natural Treatment of PMS and PMDD
If you have PMS or PMDD, there are several natural treatments that I use to relieve symptoms. These can include strategies such as diet modifications, exercise, and supplements. All focused on improving your overall well-being, stress relief, and symptom management.
Here are some of my more commonly used natural treatments for PMS and PMDD.
Diet
Eating healthy is critical to managing PMS and PMDD. Some foods can increase the likelihood of some symptoms like bloating, blood sugar fluctuations, fatigue, and mood swings. I recommend:
- Omit refined sugar, carbs, caffeine, and alcohol.
- Choose grass-fed, wild, and organic foods when possible.
- Boost your veggie intake! Load up on cruciferous veggies and fruits high in antioxidants like broccoli, cauliflower, brussels, kale, and arugula.
- Increase your fiber during the luteal phase of your cycle.
- Add 2 TBSP of ground flaxseed to your diet daily
Exercise
Move your body daily! Several research studies have shown that moderate cardio exercise everyday can help improve PMS and PMDD symptoms in four to eight weeks!
Aim for 30 to 40 minutes per day of cardio exercise or yoga.
Supplements
Getting the required dietary supplements each day has been shown to improve PMS and PMDD symptoms. Depending upon your symptoms and dietary requirements I recommend the following supplements:
- Magnesium: Migraine headaches, anxiety, adrenal concerns, blood pressure issues…your magnesium is likely lacking. Think of it as a calming agent that you can use just about anytime.
- Vitamin B6: Helps to produce progesterone and promote GABA synthesis which can ease fatigue, irritability, and insomnia. I recommend beginning with 50 mg.
- Vitamin E and good fats. Vitamin E supplements and essential fatty acids help combat the effects of PMS by reducing the effects of the hormone prolactin. I suggest starting with 800 iu Vitamin E Tocotrienols, 2 caps of omegaMonoPure 1300 [email office for more information on this product], or 2 caps of EPO (bonus: EPO is great for glowing skin!).
- Calcium: Adding additional calcium support has shown to be a simple and effective treatment for the luteal phase symptoms of PMS. I recommend adding 1200 mg of calcium per day.
- Saffron: In women with mild to moderate depression, saffron has shown to have an antidepressant-like effect. And, it can be used throughout the luteal phase of your cycle. I used the product MoodStasis beginning with 15 mg twice a day.
- Progesterone Drops. Augmenting your progesterone with natural progesterone drops based on your labs can help mimic your body’s progesterone production. This cyclic taper allows us to taper up or down based on your personal need. (email our office for help with this product)
- Hormone-balancing herbal blends. A hormone-balancing herbal blend can help promote progesterone production and estrogen clearance. I often use Vitex, DIM, or CDG to promote progesterone production. I use Calcium d-Glutarate to help prevent estrogen metabolites from recirculating back into the bloodstream from the gut and to help eliminate excessive estrogen. And there are many classical Chinese herbal formulas specific to women’s health and hormones that I will often incorporate based on your constitution and symptom presentation.
Liver Detox
If the liver has to work hard to filter out harmful toxins from the body, its capacity to cleanse the blood from estrogen can be compromised. In addition to decreasing your overall toxic load, eliminating alcohol can help improve your liver’s ability to detox excess estrogen. Alcohol increases allopregnanolone (a neurosteroid made from progesterone) which can reduce the effectiveness of GABA. Ultimately increasing symptoms of PMS and PMDD.
Say Goodbye to PMS and PMDD Naturally
The bottom line is…if your PMS symptoms occur month after month and affect your quality of life, it’s time to get some help! You don’t need to live with physical discomfort, mood swings, anxiety, or depression.
Based on your symptoms and lab results, we will develop a personalized treatment plan to help you say goodbye to PMS and PMDD!
Are you ready to say goodbye to PMS? Begin by scheduling a free 15-minute troubleshooting call.
Anxiety Disorder Symptoms, Hormonal Imbalance, and Histamine Intolerance: The Surprising Connection
Your brain is foggy. Making even small decisions feels overwhelming.
You’re worried about everything and it’s hard to sleep at night.
The fatigue that nearly overpowers you makes you want to go back to bed and pull the covers over your head and hide from everyone and everything.
You’re cranky, restless, and on edge. Panic attacks cause your heart to race and your palms to get sweaty.
Even if you only have only a couple of these problems, you may have generalized anxiety disorder. That’s the bad news.
The good news? You can feel at peace, happy, and calm again. The answer lies in balancing your hormones. But that’s not all. You’ll also need to get rid of problems like blood sugar imbalance that cause your hormones to get out of whack. Then there’s histamine intolerance, which is strongly linked to hormonal imbalances and anxiety.
Hormone Imbalance: The Victim Not the Villain
Imbalanced hormones are not the villains responsible for your anxiety disorder. They’re more like the victims of other problems happening in your body. That’s why as a functional medicine provider specializing in irritable bowel syndrome, inflammatory bowel disease, and women’s fertility issues I see a lot of patients who also suffer from anxiety and panic attacks.
In fact, 75% of my patients present to my clinic with anxiety along with other issues like acid reflux, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), digestive issues, endometriosis and many more.
Hormones are actually responders, the language the body uses to talk to itself. Hormones express what they’re seeing in the different tissues around your body and tell your body how best to respond.
In other words, when hormones break, it’s not typically the root cause of your problems. Rather, the hormones shift in response to the root cause or causes of your health problems.
That said, working to adjust and balance hormones can help you feel better. When your hormones are balanced, you will have more energy and bandwidth to work on the real root cause underlying your health problems.
In this article, I’m going to dive into one common factor that breaks hormonal balance. Then I’ll hone in on one of the most important hormones for people suffering from anxiety disorder and its link to histamine intolerance.
I’ll also shed light on some of the other reasons for anxiety and panic attacks and let you know what you can do to feel less anxious and more at peace.
First, though, let’s talk about what generalized anxiety disorder actually is and its symptoms.
What Is Generalized Anxiety Disorder?
Everyone gets anxious from time to time. Work deadlines, tests at school, dealing with relationship problems or other stressors can all lead to occasional anxiety.
People with generalized anxiety disorder, on the other hand, experience ongoing worry or fear much of the time.
Often, people with anxiety disorder feel anxious or get panic attacks even while trying to make simple decisions. Generalized anxiety disorder can cause problems at work, in school, and in your relationships.
Symptoms of generalized anxiety disorder include :
- Difficulty concentrating or brain fog
- Fatigue
- Insomnia (difficulty falling or staying asleep)
- Irritability
- Restlessness
- Worry
Generalized anxiety disorder and panic disorder are some of the most common mental disorders in the United States. These are different types of anxiety disorders. Technically, conventional medicine considers panic attacks to be a separate disorder. However, in my experience as a functional medicine provider, most people aren’t going to have panic attacks without already having generalized anxiety disorder.
Symptoms of panic attacks include:
- Feeling out of control
- Feelings of impending doom
- Pounding heartbeat or rapid heart rate
- Shortness of breath, smothering, or choking
- Sweating
- Trembling
Past trauma can trigger panic attacks. But they can also happen in people who have never experienced any trauma.
Blood Sugar Imbalances Wreak Havoc on Hormones
One of the most common reasons why hormones break is because your blood sugar isn’t balanced. I have seen many patients get 90% better just by balancing their blood sugar.
Low blood sugar mimics anxiety. When your blood sugar crashes, the body attempts to push up blood glucose levels. It does this by making epinephrine, otherwise known as adrenaline, which triggers glucose production in the liver.
Increased adrenaline leads to a “fight-or-flight” stress response in the body. This same biochemical process is also linked to anxiety.
If you tumble into a chronic, on-going low blood sugar state, your body may boost its production of the stress hormone cortisol. This helps tissues in the body be less reactive to insulin, which boosts glucose circulation in the bloodstream. But high levels of cortisol can cause problems, too.
Guess what higher cortisol levels are also linked to? Anxiety.
What’s more, in my work with thousands of patients, blood sugar swings have been the biggest driver of fatigue, anxiety, and mood swings!
A functional medicine provider can order the right tests for blood glucose and insulin sensitivity. These include LDH (lactate dehydrogenase), HbA1c (hemoglobin A1c), SHBG (sex hormone binding globulin), fasting glucose, fasting insulin, and sometimes glucose response testing.
To resolve low blood sugar problems that show up on the tests, eat more healthy fats, which are easier to assimilate and digest.
High quality protein is also important. Back before I knew I had polycystic ovary syndrome – a condition linked to insulin resistance – I was eating vegan and vegetarian and chowing down on carbs. This was the wrong approach because anytime you have a problem with blood sugar or insulin, carbs are the bad guys.
The Soothing Effects of Progesterone
Your brain has receptors for sex hormones like progesterone. So it’s not surprising that progesterone can influence brain function and mood.
If you have anxiety, progesterone is one of your best friends.
Women with low progesterone levels are prone to anxiety. That’s why in conditions of low progesterone such as during PMS, post-childbirth, perimenopause, and menopause there’s an increase in anxiety and frequency of panic attacks.
Progesterone and its metabolite allopregnanolone act as a natural antidepressant, enhance mood, and relieve anxiety. Progesterone has a calming effect on the brain. It increases the actions of a feel-good, calming neurotransmitter known as GABA (gamma-aminobutyric acid).
By giving GABA a helping hand, progesterone acts like a hormonal lullaby, helping you fall asleep easier and stay asleep longer.
What’s Histamine Intolerance Got to Do With It?
Histamine is a chemical released by some cells of the body. If you’ve ever had an allergic reaction or seasonal allergies, you’re likely familiar with its effects such as runny rose, sneezing, or hives.
Histamine isn’t always the bad guy. We need some histamine to release stomach acid and to help move food through the gut. The important thing is for histamine to complete its life cycle by being broken down and cleared from the body.
When that doesn’t happen histamine intolerance occurs. This is when the body makes too much histamine and too little of the diamine oxidase (DAO) enzyme needed to break it down.
Anxiety is a symptom of histamine intolerance. Other symptoms include headaches, fatigue, nausea, irregular menstrual cycles, sinus issues, digestive problems, tissue swelling, and dizziness.
In my experience, people most likely to suffer from histamine intolerance are people who are perfectionists. These are often the same people who suffer from anxiety and panic attacks. They want things to be a certain way and hold high expectations.
Characteristics of people most likely to develop histamine intolerance include:
- Academic overachievers
- Highly motivated
- Inner anxiety with a calm exterior
- Being competitive – with themselves and/or others
- Having obsessive/compulsive or ritualistic behaviors, or a need for structure and strong routine, feeling of order and control over things.
The above characteristics can actually be positive and work in your favor. If you have those characteristics you’re highly intelligent, super productive, and probably are successful in work and life. When your hormones are in balance these traits can work for you.
However, if your histamine is too high and your hormones are out of balance then you might develop poor stress tolerance, feelings of anxiety, and insomnia.
Progesterone Guards Against Histamine Intolerance
Progesterone enhances DAO, the enzyme that breaks down histamine. So progesterone helps histamine meet its maker and clear it from the body.
Estrogen dominance, on the other hand, boosts the body’s production of histamine. Women whose histamine production is estrogen driven will see flares of their problems either right before ovulation or more likely right before their period, because that’s when they’re naturally estrogen dominant.
Does anything else cause histamine intolerance besides estrogen dominance? You bet. Genetics can play a role. My own histamine intolerance was partly caused by genetics. But the gut plays a huge role, too. For me, my high histamine and hormonal imbalance came down to the “bad” organisms in my digestive tract (Helicobacter pylori, Giardia, and Candida albicans)
Leaky gut leads to lower levels of DAO and in turn high histamine. This is because the place where your body makes DAO is mostly mucosal barriers like the intestines.
If your liver isn’t working its best, that will cause problems, too. The liver detoxifies histamine. If its detox abilities are weakened, histamine will build up in the body. It’s just one more thing to fill your bucket up to the point of overflowing.
Other Hormones to Watch in Anxiety and Panic
In my patients with anxiety, I always keep an eye on other hormones besides progesterone. These include:
- Thyroid – If thyroid hormone levels are up and down like in Hashimoto’s it can mimic bipolar disorder. Low thyroid hormones are also linked to low progesterone.
- DHEA (Dehydroepiandrosterone) – DHEA is the most abundant circulating hormone. Balancing levels of DHEA can lead to better mood and less anxiety.
- Serotonin/Estrogen – Serotonin makes you feel content, happy, calm, and ready for sleep. It reduces anxiety and the tendency to think about sad or dark thoughts over and over (cyclical thinking or ruminating). You need estrogen to convert amino acids into serotonin.
- Cortisol – Cortisol is primarily produced by the adrenal glands. Adrenal fatigue can make you less likely to cope with stress. If you have a poor stress response, cortisol can be too high or too low. If cortisol goes up due to stress, your progesterone levels can take a tumble.
Strategies to Reduce Anxiety and Panic Attacks
Here are some simple changes you can make to feel calmer and less anxious:
- Reset your inner clock. First thing in the morning, immerse yourself in bright outdoor sunlight without wearing sunglasses. After sundown, expose yourself to dim light. If you’re not doing these things, neither dietary supplements nor hormone replacement therapy will work.
- Let go of toxic people, habits, and behaviors
- Seek professional therapy
- Practice stress management techniques like transcendental meditation, hypnotherapy, somatic therapy, nature immersion, the Gupta Program, and psychedelic journeying.
Natural Hormone Replacement and Dietary Supplements for Stress
Natural Progesterone - Please email office to discuss
A functional medicine provider can prescribe personalized, low-dose bioidentical progesterone. This can relieve symptoms of histamine intolerance and estrogen dominance.
Vitamin B6 supplements can help with histamine balance including PMS related to histamine. Vitamin B6 can:
- Help produce progesterone.
- Promote GABA synthesis.
- Convert L-tyrosine and 5-hydroxytryptophan (5-HTP) to dopamine and serotonin, respectively.
- Enhance DAO production and lower histamine.
Start with 50 mg of vitamin B6 in the form of P5P. You can take more under the guidance of a functional medicine provider.
Magnesium is a natural stress reliever. I prefer the chelated form of glycinate and the product Neuro-Mag.
L-theanine, a substance found naturally in green tea, produces calming brain waves. Passionflower (Passiflora incarnata) also has soothing effects.
Taurine is an amino acid that promotes formation and release of GABA, which quiets down excitatory signals in the brain. A typical dose is 250 mg – 1,000 mg/day.
Best for acute panic attacks rather than chronic anxiety, glycine is an amino acid that interferes with the release of the neurotransmitter norepinephrine. At the first sign of a panic attack, place two grams of glycine powder under the tongue and let it slowly dissolve. This process can be repeated every few minutes if necessary and, in most cases, the problem will resolve within 10 to 15 minutes.
Cannabidiol (CBD)
This phytocannabinoid has calming, soothing effects. In human studies, CBD reduced anxiety caused by a public speaking test in subjects with social anxiety disorder.
This lavender-derived substance (also known as Silexan™) promotes relaxation and calms nervousness.
I Can Help Balance Hormones and Relieve Anxiety
To find out whether the root cause of your anxiety disorder and panic attacks is blood sugar issues, low progesterone, or problems with other hormones, you’re going to need an experienced functional medicine practitioner. The first step is to book a free 15-minute troubleshooting call with me.
If after the call you come on board as a patient, I’ll order the best tests for you and develop a treatment plan based on your unique biochemistry. You will find out the steps you need to take to feel calmer and happier. I know anxiety isn’t easy but together we’ll find a solution to make your life easier.
What Is Estrogen Dominance and Why Should a Woman Care?
Is Your Birth Control Method Making You Estrogen Dominant?
Irritable? No Sex Drive? Sugar Cravings Driving You Crazy? Birth Control Side Effects May Be to Blame
You’re cranky and feel like snapping at everyone around you.
You’re bloated but can’t stop thinking about that slice of pie or cake you saw at the bakery. It’s screaming for your attention!
Every month, before your period your head feels like someone is pounding it with a hammer. When that time of the month rolls around, you’ve got menstrual cramps like you wouldn’t believe.
Your libido has ghosted you. Sleep sounds more enticing than sex.
These are just some of the symptoms of estrogen dominance. That’s when your estrogen levels are high in comparison to progesterone.
Getting rid of estrogen dominance can work wonders on your mental and physical health. Yet, treating estrogen dominance symptoms never works. You’ve got to dig down to the root cause. I’ve had a lot of success with this approach in many patients.
In a little while I’ll share with you the story of one patient I’ll call Jennifer. By getting at the root cause of estrogen dominance, Jennifer was able to kick estrogen dominance to the curb. The result? Jennifer’s symptoms disappeared. She was happier and more relaxed, lost weight, and her libido was back in action.
I’ll tell you Jennifer’s story in a little while. But first, let’s talk about what is estrogen dominance. That way you’ll know why Jennifer’s treatment worked so well. And why you might have the same stellar results.
Too Much of a Good Thing
Estrogen isn’t always the villain. In fact, women need estrogen for many different areas of health including happy moods, heart health, and fertility.
It’s only when estrogen levels become too high in relation to progesterone that hormonal balance gets thrown off. This is what’s known as estrogen dominance.
Estrogen dominance symptoms include:
- Acne
- Breast tenderness or lumps (aka fibrocystic breasts)
- Breast, ovarian, uterine, and cervical cancer
- Disrupted sleep
- Endometriosis
- Fatigue
- Fibroids
- Headaches or migraines
- Holding on to body fat, especially in hips, thighs, belly, and butt.
- Infertility or subfertility
- Intense sugar cravings
- Low libido
- Mood changes: intense irritability, anxiety, devastating depression
- Stress
- Water retention
- Weight gain
Estrogen dominance can be especially nasty if you’re in perimenopause, the time before entering full menopause. If you’re one of the unlucky ones to be going through both at the same time you might have bad mood swings, horrible PMS, weight gain, and depression. And your libido tanks. Not fun!
What Causes Estrogen To Get Out of Whack?
Remember, our number one goal is to reach a healthy balance of both estrogen and progesterone. In a healthy woman, estrogen and progesterone are balanced and work together in harmony. Progesterone is critical because it counteracts the bad effects of too much estrogen.
There are a number of reasons for too much estrogen or too little progesterone. But hormonal birth control is a very common culprit that most women have never heard about it. A woman might be taking the mini pill or have a hormonal IUD (aka Mirena) and she has no idea it could make her symptoms worse.
Don’t get me wrong. Hormonal birth control has its time and place, but if you’re going to use it you should know about the risks and limitations. You should especially know it won’t fix a hormone imbalance. The problem will still be there after you start taking the pill.
Ironically, birth control is often used to treat symptoms of estrogen dominance like heavy bleeding and painful periods. However, hormonal birth control only makes the estrogen dominance worse.
How does this happen? Hormonal IUDs block ovulation. Without ovulation, you don’t get a healthy rise in progesterone each month. That’s not good. But it gets worse. Just because ovulation stops, doesn’t mean estrogen production stops. You’re still making estrogens- and you’re getting less and less progesterone.
How does your hormonal IUD or mini-pill block ovulation, send progesterone into a nosedive, and allow estrogen to rage out of control? It’s all thanks to progestin, a synthetic form of progesterone.
Doesn’t synthetic progestin work just like natural progesterone? Not at all. In a nutshell, progestin is kind of like progesterone’s evil twin. Progestin doesn’t act like progesterone in the body - it acts more like testosterone, and with none of the benefits of natural progesterone! That’s why it doesn’t improve your PMS, mood, or sleep symptoms.
Progestin-based birth control spells trouble for your body’s hormonal balance. And it throws your progesterone and estrogen levels out of whack.
In fact, the whole reason you might have had heavy periods in the first place is because you suffer from progesterone deficiency!
A Double Whammy
What’s worse, perimenopausal women are often using hormonal IUDs. That’s because several birth control pills’ side effects including risk of stroke, heart attacks, and blood clots, go up after you turn 35. At that time, your doctor may recommend a hormonal IUD. And many women keep using this form of birth control right through the perimenopause period.
Not only are you in perimenopause, which already makes estrogen dominance worse—but you’re also using a birth control device that can cause progesterone levels to plummet. This causes you to go deeper into estrogen dominance. And your symptoms continue to get worse. How crazy is that?
Other Causes of Too Much Estrogen
It’s bad enough that hormonal birth control like IUDs cause estrogen dominance. But if you’ve got one or more other problems going on, everything just gets worse. It’s like a snowball rolling downhill getting bigger and bigger.
Things that worsen estrogen dominance include:
- An overgrowth of bad bacteria in the gut (aka dysbiosis). Bad gut bacteria put estrogen back into circulation where it doesn’t belong.
- Constipation.
- Sluggish liver detoxification, which slows the clearance of hormones from your body.
- Stress, which hampers your ability to make healthy progesterone levels.
- Too much body fat.
- Xenoestrogens accumulate in our bodies and act like estrogens. These chemicals come from plastics, fragrances, pesticides, and processed soy products, to name a few.
Many doctors go after the symptoms of estrogen dominance rather than tackle the root cause. But symptom relief isn’t the same as hormone balance. In fact, trying to relieve symptoms by inserting a hormonal IUD only leads to more hormonal imbalance.
Instead, I go after the underlying hormonal imbalance issues such as healing the gut, balancing hormones, relieving stress, detoxification, and nutrient deficiencies. If these aren’t addressed, your whole health will suffer.
You remember I mentioned my patient Jennifer? Now we’ll get down to the nitty gritty on how I helped her get rid of the root cause of her estrogen dominance. At the same time we switched her over to one of the safest and best birth control methods.
Jennifer’s Path to Hormone Balance and Better Health
Jennifer was a 34-year-old patient of mine frustrated she couldn’t lose weight. She also had digestive problems. She was constipated and only had a bowel movement every third day. She felt bloated, although this symptom improved after she stopped eating gluten, grains, and dairy. Eating too much fat at one time caused her GI symptoms to act up.
To make matters worse, Jennifer struggled with severe anxiety, carb cravings, and low libido.
Sound familiar?
A few years ago, her doctor installed a hormonal IUD. Her periods became light and only lasted three days. This is a common side effect of these devices. In fact, it’s the main reason doctors recommend an IUD, to lighten heavy periods. This is because the progestin in the IUD reduces the thickness of the uterine lining, which in turn leads to lighter bleeding or makes periods go away completely.
Testing revealed Jennifer was estrogen dominant. No surprise there! Her estrogen levels were actually ideal but her progesterone levels had nearly hit rock bottom.
She also had low bile flow. Bile is needed to lose weight and detoxify the body. Bile deficiency happens a lot in women with estrogen dominance.
In addition, lab results showed she had a parasite and the harmful bacteria in her gut were growing out of control.
I felt bad this lovely woman was suffering. I knew we could turn things around for her.
Address Estrogen Dominance and Gut Health to Feel Happier, Sexier, and Lose Extra Pounds
We started working on the root causes of Jennifer’s problems. First, upon my recommendation, she had the hormonal IUD removed and replaced it with a copper IUD. These aren’t as hard on hormonal health. However, the copper IUD can promote heavier periods and increased cramping, especially in the first several months for certain women. In women like Jennifer, I address heavy menstrual bleeding by using Slow Flow and Chinese herbal formulas for one to three months. I supported Jennifer’s natural ability to make progesterone using vitamin C and Vitex.
To her surprise, she lost eight pounds! And she did it without doing anything other than just getting the hormonal IUD removed and taking those few supplements.
At that point I started working on her imbalanced gut bacteria and her sluggish liver, the cause of her low bile flow. The low bile was also the culprit behind her inability to digest fat, which in turn led to bloating and gas, sluggish bowel movements, and low levels of essential fat soluble nutrients such as vitamins A, D, and K.
We addressed the gut dysbiosis and the sluggish liver and—Viola!—her constipation and GI symptoms went away.
Throughout the course of treatment, she also said sayonara to her anxiety, carb cravings, and low libido.
Find Serenity, Boost Your Libido, Cure Carb Cravings, and More
I know how frustrating estrogen dominance symptoms can be. My heart goes out to all women suffering from this condition. I can work with you to pinpoint what’s holding you back from optimum health and turn it around, just like I did with Jennifer.
Your path to peace, sanity, and your best life ever begins with a free 15-minute troubleshooting call. During this chat, I’ll get to know more about what troubles you. If after the call you come on board as a patient, I’ll work with you on estrogen dominance treatments and run the right tests that can put you on the path to vibrant good health. Book your call today and you can feel younger, happier, and more energetic tomorrow.
PCOS 101: Everything You Need to Know About Polycystic Ovarian Syndrome
I’ve been where you are right now… Maybe your doctor just told you, “You have PCOS.” Maybe you’re questioning it yourself… Googling for answers.
Or maybe - and this might be the most frustrating situation of all - you’ve been told for YEARS you had PCOS, only to be told now, you somehow, suddenly don’t.
The fear, overwhelm, frustration, uncertainty - I get it! (I have PCOS, myself.)
Nothing about PCOS is straightforward. (Even the name doesn’t make sense!)
So let me hold your hand for a minute - today I want to explain everything you need to know about PCOS, start to finish.
What Is PCOS?
PCOS stands for Polycystic Ovarian Syndrome - and it’s an endocrine (AKA hormonal) disorder that affects women of reproductive age.
PCOS is the most common hormone dysfunction among women and affects 10-20% of all women of reproductive age.
(That means if you get a group of 10 of your friends together, it’s likely 1-2 of you will have PCOS!)
And despite the name, PCOS really has nothing to do with cysts on your ovaries. Instead, PCOS is a condition marked by elevated levels of androgens (commonly called male hormones.) This is often testosterone, but can include other androgens.
People with PCOS often also have elevated luteinizing hormone (LH), and prolactin and lower follicle stimulating hormone (FSH).
And while your doctor might not make a big deal out of it, the truth is that PCOS is a lifelong disease with big medical and emotional impacts, and potentially the additional burden of obesity.
What Are The Symptoms of PCOS?
Symptoms of PCOS include:
- Hirsutism
- Male pattern hair loss or thinning
- Acne
- Oligo or amenorrhea (chronic anovulation)
- Obesity
- Sub/ Infertility
- Low libido and sexual problems
- Skin tags or darkened skin in the folds (acanthosis nigricans)
- GI problems (IBS, leaky gut)
- Arthritis and tendonitis
- Depression, anxiety, stress, eating disorders, and body dysmorphia
- Increased vaginal infections
- Sleep dysfunction
- Increase in certain cancers (uterine and breast)
- Increased rates of other gyn conditions, like fibroids, endometriosis
PCOS can also lead to:
- Pregnancy complications
- High blood pressure
- Diabetes
- Dyslipidemia
- Fatty liver
- Higher risk of cardiovascular disease
PCOS can present very differently in different women, and there are at least 4 different types (more on that to come).
One big misconception? That all people with PCOS are overweight. Although overweight/obesity is common in PCOS, it is not a symptom for all people with the condition.
Another misconception is that PCOS causes painful periods or pain. That’s not true either. If you have pain or painful periods, it is likely caused by something else (though it’s possible you have PCOS, too - it just isn’t the cause of the pain!)
How Do I Know If I Have PCOS?
How PCOS is diagnosed has changed over the years, which is part of why there is so much confusion around who does and doesn’t have PCOS. If you’ve been told you did have PCOS, but don’t now - the changes in diagnostic criteria explain why.
In the past, PCOS was diagnosed primarily based on missing or irregular periods and the presence of multiple cysts on the ovaries, as seen via ultrasound.
But now we know that there are many reasons cysts can appear on the ovaries - and sometimes, those cysts are entirely normal and not indicative of any disease state.
That’s why, today, PCOS is diagnosed based on updated guidelines from 2018 for missing or irregular periods AND androgen excess, which is determined as:
1) high androgens (male hormones) measurable on a blood test,
and/or 2) significant facial hair or jawline acne.
PLUS other reasons for androgen excess have been ruled out.
Ultrasound is no longer required to diagnose PCOS, though many practitioners still do perform one.
Even if you are missing periods, or have them irregularly, or if you had an ultrasound that featured cysts on your ovaries, if you do not have androgen excess as defined by labs or symptoms mentioned above, then it’s not considered PCOS. (Missing your period, but no androgen excess? There are lots of other reasons for missing periods. Read more here.)
Other signs of PCOS include the following, but these all are not always present, even with PCOS:
- Bilateral polycystic ovaries
- Elevated LH and LH to FSH ratio
- Oligoovulation (irregular or infrequent ovulation)
- Elevated free testosterone and DHEAS
- Glucose intolerance and elevated insulin
When Hormone Levels Are “Normal” But You Still Have PCOS Symptoms
If you have key symptoms of androgen excess - such as severe jawline acne and facial hair growth - but your lab tests are normal, don’t rule PCOS out.
Some women are extremely sensitive to even “normal” amounts of androgens. This means that even with normal levels, they may have key symptoms like jawline acne and facial hair growth. That’s why the guidelines state that PCOS diagnosis can be based on either elevated androgen levels on a blood test or symptoms of high androgens.
But, there are also other conditions aside from PCOS that can cause the symptoms of androgen excess, including:
- Congenital adrenal hyperplasia (an inherited condition that impacts the adrenal glands and sex hormones)
- High prolactin secretion
- History of using an oral contraceptive pills that contain progestins, which behave more like testosterone than progesterone in the body
Is It PCOS… Or Something Else?
Other conditions can sometimes be mistaken for the more-common PCOS. These include:
#1 Non-Classic Adrenal Hyperplasia (NCAH)
This condition is similar to congenital adrenal hyperplasia, but comes on later in life (usually around the time of puberty) and is not as severe. For women, symptoms include delayed first period (menarche), male-pattern hair growth and loss, and infertility. It is hard to tell the difference between PCOS and NCAH, but if a person presents with PCOS symptoms and is not insulin resistant, it could be NCAH - though some people with NCAH do have insulin resistance. NCAH is more rare than PCOS. The only way to distinguish PCOS from NCAH with certainty is by measuring 17-hydroxyprogesterone levels.
#2 Functional Hypothalamic Amenorrhea
This is the loss of normal menstrual cycles due to overexercise/undereating, and it often occurs in both normal and underweight women. It can be really difficult to distinguish a woman with FHA from a woman with PCOS who is lean. Tell-tale signs that it is FHA include low to normal basal FSH and LH levels and low estrogen (vs. elevated serum LH levels and low to normal FSH levels in women with PCOS). Women with FHA don’t usually have the severe jawline acne or male-pattern hair growth seen in PCOS. On an ultrasound, both women with PCOS and FHA may have cysts, but the ovaries and uterus of a woman with FHA are small or normal, whereas a woman with PCOS typically has increased ovary size. To make it a little more complicated… it is possible to have both PCOS and FHA simultaneously.
What Causes PCOS?
The exact cause of PCOS is not known, but it is likely a combination of genetic predisposition and environmental effects. Some known risk factors are:
- Mother had gestational diabetes (it’s thought that the exposure to higher levels of insulin levels in utero could lead to PCOS in adulthood).
- Exposure to endocrine disrupting chemicals in utero or in life. So far the focus has been of BPA.
- Diabetes or metabolic syndrome in first degree relatives
- Gut inflammation, such as IBS, SIBO, or leaky gut (because they cause chronic inflammation)
- Higher levels of oxidative stress, beginning in utero and continuing through life
- Vegetarian diet, which may contribute to low levels of zinc and
- Autoimmunity
- Hypothyroidism
It’s also suspected that a genetic mutation of the CYP17 enzyme, which is responsible for forming androgens from DHEA-S, could play a role.
Beyond these risk factors, it isn’t known exactly why some women develop PCOS and others don’t.
While what starts the initial process of PCOS remains mostly unknown, we do know what happens in the body that leads to PCOS. It’s a hormonal cascade that starts with hypothalamic gonadotropin-releasing hormone (GnRH).
First up, in a woman without PCOS, here’s what happens: hypothalamic gonadotropin-releasing hormone (GnRH), stimulates the release of LH - luteinizing hormone. The LH tells special cells in the ovaries called theca cells to convert cholesterol (a type of fatty acid in the body) into two androgens: testosterone and androstenedione. The androgens then move into the granulosa cells, where the hormone FSH (follicle stimulating hormone) converts them into estrogen via a process called aromatization.
But in a woman with PCOS, the process gets stalled out before the androgens can be converted into estrogen. Here’s what happens...
Women with PCOS have increased pulsatile GnRH release, which results in higher levels of LH and lower levels of FSH in most individuals. These higher LH levels cause increased androgen production by follicular theca cells. That means a woman with PCOS has more androgens to convert to estrogen to start - plus a lower FSH level, which is the hormone needed to convert the androgens to estrogen.
All those extra androgens in the ovaries stop the normal growth and maturation of follicles, and prevent ovulation. As a result, the ovaries wind up with lots of small, antral follicles that become cysts on the ovaries. This enlarges the ovaries and can also create an elevated serum estrogen level.
But that’s not all! In addition, the cells of people with PCOS respond to normal levels of the “blood sugar hormone” insulin by making increased amounts of testosterone. In a woman without PCOS, these levels of insulin would not result in excess testosterone.
This is intensified by the fact that women with PCOS also are far more likely than people without PCOS to have insulin resistance and elevated insulin levels.
PCOS and Insulin Resistance
PCOS and insulin resistance have a complex relationship: insulin resistance is both a symptom and a potential cause of PCOS.
But before we dig any further, let’s do a quick refresher on what insulin and insulin resistance are.
Insulin is a hormone secreted by the pancreas in response to blood sugar. When you eat food, it is broken down and absorbed into the bloodstream in the small intestine. This causes a rise in blood sugar. In response to this rise in blood sugar, the body pumps out insulin from the pancreas. The insulin helps shuttle the sugar out of the bloodstream and into the cells, where it can be used as energy.
Insulin resistance is one way this system can break down. Essentially, the pancreas continues making insulin, but the body stops listening. That can lead to both high levels of insulin (because the pancreas keeps making more) AND high blood sugar levels, since the insulin isn’t doing its job of moving the sugar out of the bloodstream and into the cells.
Insulin resistance is often the first step on the road to developing Type 2 diabetes and gaining weight, which is harder to lose.
Insulin resistance is very common in PCOS: even in non-obese women with PCOS are far more likely than other women of the same weight without PCOS to wind up with insulin resistance.
And while we don’t know for sure if the PCOS causes the insulin resistance… or the insulin resistance causes the PCOS… what we do know is that high levels of insulin stimulate the ovaries to make more testosterone. At the same time, high testosterone levels in women lead to insulin resistance and weight gain.
Being overweight with PCOS only intensifies the metabolic problems. Excess fat cells lead to fatty acids spilling into the bloodstream. Combined with the low antioxidant and high oxidative stress seen in PCOS, this leads to increased oxidation of the fats, which damages tissues. This creates yet another cycle where oxidative stress increases testosterone production, which only increases insulin resistance. Once this cycle is set in motion, it’s really difficult to stop.
PCOS is also inflammatory, and this inflammation further increases insulin resistance and abdominal visceral fat. The inflammation also promotes abnormal adipose function with inappropriate adipokine release. Adipokines include the “hunger and fullness” hormones leptin and ghrelin.
PCOS and The Microbiome
PCOS doesn’t just affect your hormones, however. It can also have major, negative consequences for the microbiome.
The microbiome is the collective name for all the bacteria that live in your gut and perform vital roles in digestion, metabolism, hormone production, and communication between body systems.
Stool testing showed the microbiome of people with PCOS was less diverse and had an altered composition compared to healthy controls.
The dysbiosis in the microbiome that PCOS can cause promotes even more inflammation, as well as allergies and autoimmunity. Research has shown that women with PCOS (both those who were lean and those who were overweight) had significantly higher LPS levels, a marker of inflammation and leaky gut, compared to healthy controls.
And, in another example of the way PCOS symptoms can be self-perpetuating, a dysbiotic microbiome as a result of PCOS could contribute to further weight gain and insulin resistance, further fueling excess androgens. Studies have shown that changes in gut microbiome trigger mechanisms that promote obesity, Type 2 diabetes, and metabolic syndrome. And, it’s known that people with Type 2 diabetes also have an altered microbiome.
Both obesity and dysbiosis, two common results of PCOS, directly increase gut permeability (leaky gut), which promotes insulin resistance, which drives further testosterone production in the ovaries, creating PCOS, which impairs ovulation and promotes further androgen dominance.
Bottom line: if you’re struggling with weight loss and obesity, and have PCOS, a dysbiotic microbiome could be a reason why.
What Happens If PCOS Is Ignored
For most people with PCOS, symptoms like unwanted facial hair and jawline acne are enough to make them want to seek treatment. PCOS can really impact quality of life.
But even if PCOS symptoms aren’t bothersome, leaving this condition untreated long-term has serious consequences.
Of course, PCOS affects fertility: it is more difficult or impossible for those with PCOS to become pregnant due to their irregular/absent ovulation.
However, even if you never want to become pregnant, PCOS does far more than affect fertility.
The high androgens produced in the ovaries lead to insulin resistance and inhibited ovulation. The insulin resistance puts you at risk for Type 2 diabetes and weight gain. In addition, even if insulin resistance isn’t a feature of your PCOS, the high testosterone levels seen in PCOS also increase the risk of Type 2 diabetes.
The inhibited ovulation leads to low levels of progesterone (because progesterone rises when ovulation occurs). Progesterone should balance estrogen, but when progesterone is low estrogen can become chronically high, and over a lifetime this increases the risk of estrogen-driven cancers like ovarian and breast cancer. Both low progesterone and absence of ovulation have been linked with significantly higher risk of breast cancer.
And, because another role of progesterone is to block androgens, the absence of progesterone only adds fuel to the fire. In this way, PCOS becomes a self-perpetuating cycle. This means it’s very unlikely to just “go away” on its own.
Is There Hope for Healing PCOS?
I know that this blog post has been really heavy so far.
Lots of scary symptoms and confusing hormones… that might leave you feeling like “Is there any hope for healing PCOS??”
So let me reassure you right now: there IS hope for healing PCOS!
I speak from personal experience - I was diagnosed with PCOS in my twenties. In fact, it was this diagnosis that really lit a fire in my soul for natural healing.
Today, my PCOS is well managed. My weight is stable, I have hair on my head, not my face. I was able to get pregnant and give birth to a beautiful daughter. To be totally transparent, we did use IVF - but I had PCOS, was almost 40, and have only one ovary! With those factors in mind, it went as smoothly and easily as it possibly could have - due in large part to the work I had done to optimize my health and hormones.
Life is good… and I want these kinds of results for you, too!
The rest of this article will be dedicated to healing PCOS.
Step 1 to actually treating PCOS is determining what type of PCOS you have.
The 4 Types of PCOS
While PCOS is the umbrella term, clinically, I see people with PCOS fall into one of four categories based on their symptoms and presentation.
Knowing what type of PCOS you have is critical because it guides what treatment plan will be most effective for you.
Read through all four types and see which one you identify most with.
Type #1: Insulin Resistance PCOS
Insulin Resistance PCOS is the most common type, and accounts for about 70-75% of all PCOS cases. The defining criteria? If a patient has insulin resistance of any degree and PCOS, they have Insulin Resistance PCOS. In addition, if you have pre-diabetes, you likely also are in the Insulin Resistance PCOS category.
High insulin levels promote high androgens, creating PCOS.
What years of working with PCOS patients has taught me is that, usually, there is some level of insulin resistance present in people with PCOS, even if it’s subtle. One tell-tale sign I look for are changes in energy levels after eating. In a healthy person, eating should only make you feel less hungry. If eating makes you feel tired and sluggish, or conversely, clears your head and gives you a major boost of energy, that’s a red flag.
To know if you have insulin resistance, your blood can be tested for high insulin levels using a fasting insulin test. Fasting glucose and hemoglobin A1c blood tests can also help provide a snapshot of your body’s response to insulin. However, sometimes a person has a normal fasting insulin, but still has a poor glycemic response to carbs. This means their blood sugar spikes above 140 or that their insulin resistance is more exaggerated than it should be. To assess this, an oral glucose tolerance test is used. Glucose tolerance tests are preferred because they can catch insulin resistance at lower levels and in earlier stages.
Another option is at-home glucose monitoring with a glucometer or continuous glucose monitor. I love this option because no doctor’s orders are needed (you can get a glucometer and test strips over the counter) and it can provide a bigger picture of what’s happening to your body when you eat real food over a longer period of time. If you want an exact, step-by-step guide to tracking your glucose measurements over the course of 3 days, click here to download my free At Home Blood Sugar Testing Guide.
Type #2: Inflammatory PCOS
All types of PCOS feature some inflammation, but in Inflammatory PCOS, inflammation is the hallmark symptom, and insulin resistance isn’t present.
People with Inflammatory PCOS often have known causes of chronic inflammation or other inflammatory symptoms and conditions, like:
- Autoimmune disease
- IBS or SIBO
- Joint pain or body aches
- Chronic headaches
- Chronic fatigue
- Depression
- Skin issues like eczema or psoriasis
Sometimes, Inflammatory PCOS is best diagnosed by ruling out the 3 other types. If you’re feeling uncertain if this type describes you, keep reading about the other types.
Type #3: Post-Pill PCOS
For some people, stopping hormonal birth control pills can lead to the development of PCOS. Stopping the artificial progesterone in the pill (called progestins) can cause a temporary surge in androgens that creates PCOS. This is most common with Yasmin, Yaz, and the Mirena IUD, although it can happen with other pills
People with this type of PCOS usually report that their periods were normal before starting the pill, and symptoms only began once they stopped. The good news is that, if treated, this type of PCOS is usually more temporary. Detox support and herbs that lower androgens can often reverse this type. (More on treatments to come.)
Type #4: Adrenal PCOS
Adrenal PCOS is largely genetic, but can also be triggered by extreme stress, weight loss diets, overexercise, and lack of sleep, all of which further tax the adrenal system.
Adrenal PCOS often looks a lot like congenital adrenal hyperplasia (CAH), which was discussed above. However, unlike with CAH, with Adrenal PCOS, 17-OH progesterone won’t be elevated. In addition, women with adrenal PCOS often only have elevated DHEAS, not testosterone or androstenedione.
For this type of PCOS, the best approach is supporting adrenal hormone function and managing stress, alone with nutrients and botanicals that help normalize androgens.
My Treatment Goals for PCOS
When you have any goal - but especially a big health goal like treating PCOS, it’s important to break it down into smaller, trackable, manageable goalposts.
PCOS treatment isn’t a one-pill-and-you’re-done kind of thing… it can take months of consistent work to see changes. Having clear-cut goals in mind helps power you through the process.
(And we also have health coaches on staff who are specially trained in helping you break down goals and achieve them step-by-step!)
My PCOS treatment goals include:
- Regulating hormone levels (increasing progesterone secretion, LH:FSH, decreasing prolactin)
- Improving the stress response and HPA (hypothalamus-pituitary-adrenal) function
- Optimizing the microbiome
- Optimizing detox pathways and function
What About Standard Treatments?
Two of the most common standard treatments for PCOS are hormonal contraceptives and the drug metformin.
Metformin is an insulin sensitizing drug that can help with insulin resistance. However, it doesn’t enhance ovulation for many patients. As far as drugs go, I don’t think metformin is a bad one, and it may have some benefit for you. Talk to your doctor about it. But, because metformin tends to displace vitamin B12, be sure to supplement or monitor your levels while using it.
Hormonal contraceptives (aka the birth control pill) are one of the most common “treatments” for PCOS, but aren't one I recommend. That’s because all the pill cna do is further suppress ovulation and hormone production - it does nothing to address the root cause of the imbalance. When you inevitably stop the pill (and all women have to stop the pill at some point, even if only because increased age has made the risk of blood clots too high), PCOS symptoms come roaring back.
Birth control pills also contain artificial progestins, which actually behave more like testosterone in the body than they do real progesterone. For women with PCOS, this can exacerbate symptoms.
Furthermore, one of the biggest issues with PCOS is that it suppresses ovulation, and ovulation is necessary for healthy hormone balance, preventing cancer, and maintaining bone integrity. The birth control pill also suppresses ovulation… which means it does nothing to fix the problem.
Step #1: Testing
Testing is an essential step for my work as a practitioner. But I’m not just talking about the run-of-the-mill tests you’ve likely had before… I use advanced, in-depth testing to get a deep look at what is happening throughout your body.
Here’s some of the tests I commonly use with PCOS patients:
- Testosterone
- SHBG
- DHEA
- Epi-Testosterone
- 5a-Androstanediol
- 5b-Androstanediol
- DHT
- Androsterone
- Etiocholanolone
- Estradiol
- Prolactin
- AMH
- LH
- FSH
- C-RP
I prefer to use the DUTCH Complete test for most of these hormones and metabolites, but they can also be tested via blood serum, as well. Some are only available via serum testing.
In addition to these, I also run some tests to rule out other conditions and assess overall health:
- 17-OH progesterone, to rule out CAH
- Thyroid panel, to rule out amenorrhea due to thyroid issues, and because thyroid issues often co-occur with PCOS
- Lipid panel, to assess metabolic syndrome and cardiovascular risk
I also sometimes use a month-long cycling panel to assess ovulation, and to look at overall progesterone levels/exposure over the month/cycle, because you can’t assess this with a one day snapshot. To do this, I use the Menstrual Cycle Mapping test from ZRT Labs or the Oova. Oova catches LH surges and can confirm ovulation, even in women with PCOS. This is HUGE because standard ovulation tests can’t detect the LH surge, since LH is already high in women with PCOS. For more on the Oova, read this. The Menstrual Cycle Mapping measures progesterone, LH, and estradiol, which can be really useful in some cases.
Step #2: Add Lifestyle Changes
The lifestyle changes I have patients implement vary based on their unique case, but there are some general principles that help most people with PCOS.
First, and maybe most importantly: prioritize sleeping 8 hours per night.
And while I know everyone says this… you also have to find a way to manage stress that works for you. Research has shown people with PCOS actually have a greater stress response than women without PCOS, even when the stressor is the same. It makes women with PCOS more inflamed, and more likely to experience anxiety and depression, too.
Some of my favorite tools for managing stress:
- EMDR therapy (with a trained practitioner)
- The ApolloNeuro wearable - this uses specialized touch therapy against your skin to promote feeling of calm and well-being. There is nothing else like it available!
- Inaura.com - a new platform that provides a wide array of therapies to help deal with stress and trauma
In addition, improving diet can help, too. I recommend eating 2-3 meals per day of an organic, plant-heavy diet avoiding gluten, most dairy, artificial sweeteners, trans fat, and alcohol. Eat plenty of healthy fats - like olive, coconut, and avocado oils, plus high quality animal fats, but avoid trans-fats. And if your diet is lower in carbs, be sure you’re including lots of variety of veggies to get the plant fibers your gut microbiome needs to thrive. And, if you’re not overly sensitive to caffeine, add 2-3 cups of green tea daily.
Step #3: Supplement Smart
Most people want to start with supplements, but it’s really the third step, after testing and diet and lifestyle changes. Remember that supplement regimens need to be customized to your needs - so while the ideas here are a great place to start, they can’t replace working one-on-one with a trained practitioner.
With my own patients, I use the results of their lab testing and the lifestyle changes to create custom, one-of-a-kind supplement protocols, with their specific type of PCOS and symptoms in mind.
One last thing, more isn’t always better. While all of these supplements have benefits, I usually use no more than 3-5 at any given time.
Here are some of my go-to supplements:
Magnesium
Magnesium is an essential cofactor for thousands of processes in the body and is especially key for insulin sensitivity. Research has shown people with Type 2 diabetes (which is common with PCOS) may excrete higher-than-normal amounts of magnesium in their urine, and that magnesium deficiency may be associated with the development of insulin resistance - which is another key component of PCOS.
In addition, magnesium absorption is interfered with by birth control pills, which many women with PCOS have taken or are taking for long periods of time. A good place to start is with this magnesium, 300 mg, twice daily.
Pre and Probiotics
Pre and probiotics promote “good” flora in the gut - prebiotics by acting as food for the gut bacteria, and probiotics by introducing new, beneficial strains. This leads to a greater production of anti-inflammatory Short Chain Fatty Acids (SFCAs), which are a byproduct of bacterial fermentation. SFCAs help improve tight junction function, reducing LPS passing into the bloodstream, which can overstimulate the immune system.
In an animal study, those with PCOS even showed reversal of PCOS with a microbiome transplant and lactobacillus (a type of beneficial bacteria). In another study, supplementing with probiotics and the mineral selenium reduced excess androgen levels and improved hirsutism.
My recommended probiotic is MegaSporeBiotic. Be sure to eat plenty of fruits and veggies for pre-biotic plant fibers, or add a prebiotic supplement like MegaPreBiotic.
Zinc
The mineral zinc has been shown to improve ovarian function, lower androgens, raise progesterone, and promote ovulation. My recommended brand is Designs for Health and the recommended dose is 30 mg daily.
Vitex
Vitex is an indirectly progesteronic herb that has been found in some research to benefit PCOS. Vitex can decrease prolactin by stimulating dopamine. Prolactin is often elevated in women with PCOS, and elevated prolactin promotes higher androgen levels.
While clinically, vitex seems to help many women with PCOS (including me), in theory, it could make PCOS worse. This is because vitex may stimulate LH, and in women with PCOS, LH levels are already too high. However, it is a game-changer for many women with PCOS. If you decide to try it, keep a close eye on your symptoms for signs of improvement or backslide. Especially consider it if you’ve been diagnosed with elevated levels of prolactin.
This product is my favorite blend with clinically meaningful levels of Vitex.
Inositol
Inositol is a plant compound (often thought of as one of the B-vitamins, but technically a sugar) that has been proven beneficial in those with PCOS. One potential mechanism could be that inositol contains the phosphoglycan that helps mediate insulin, and this phosphoglycan is often deficient in people with PCOS.
Research has shown inositol:
- Improves insulin sensitivity
- Improves ovulatory function
- Decreases serum androgens
- Decreases elevated blood pressure
- Decreases elevated plasma triglycerides
- Improves oocyte quality in women with PCOS
There are several forms of inositol: most commonly myo-inositol and d-chiro inositol. Both forms were shown effective in improving ovarian function and metabolism in patients with PCOS, although myo-inositol showed the most marked effect on the metabolic profile (i.e. insulin resistance), whereas d-chiro-inositol was better able to reduce hyperandrogenism. Myo-inositol may also protect against gestational diabetes in women with PCOS.
Most commonly, myo-inositol and d-chiro inositol are used in combination, as there is evidence they balance each other and provide the most benefits together. A standard dose is 4 grams daily. This is my recommended brand.
Licorice & Peony
Licorice and peony are often used together in traditional chinese medicine formulas, such as Shao Yao Gan Cao Tang. Research has shown they block the production of testosterone and promote aromatization, which converts testosterone to estrogen. Licorice in particular can help lower testosterone and block androgen receptors. They may also improve low progesterone, and modulate estrogen and prolactin.
N-Acetyl-Cysteine
N-Acetyl Cysteine (NAC) is a powerful antioxidant that works to reduce inflammation and oxidative stress in the body, both of which may be higher in women with PCOS. NAC promotes antioxidant activity by increasing the production of glutathione, which studies have shown women with PCOS have 50% less of than normal.
NAC can help lower testosterone and improve insulin resistance. One study even showed NAC was more effective at reducing insulin than the drug Metformin (more on this to come).
For women with PCOS looking to become pregnant, NAC may be especially important. Women with PCOS who took NAC were 3.5 times more likely to become pregnant, had a greater likelihood of a live birth, and reduced risk of preterm delivery.
In women using the drug Clomid to promote fertility, adding NAC improved ovulation rate, cervical mucus, mature follicles, endometrial thickness, follicular E2 levels, and luteal progesterone levels.
My recommended brand is Designs for Health, 900 mg, 3 times daily.
Berberine
Berberine is an herb that can benefit women with PCOS in many ways. First, berberine can improve insulin resistance in theca cells. It has been shown to be particularly effective against obesity and visceral adipose tissues (hormonally active fat). It also improved ovulation and increased fertility. Berberine was shown to reduce testosterone and improve LH:FSH rations compared to placebo.
Berberine may also benefit the gut microbiome of women with PCOS by increasing production of Short Chain Fatty Acids (SFCAS - for more on this, see Pre and Probiotics, above).
I like this brand of berberine.
Reishi
The mushroom reishi blocks 5-alpha reductase, which is the enzyme that converts testosterone into its stronger metabolite, DHT. This can help reduce overall androgen excess in women with PCOS. Reishi is also beneficial for the hypothalamic-pituitary-adrenal axis, as well.
My favorite reishi supplement is Mushroom Science Reishi, dose is 2 capsules, twice daily.
Gymnema
Gymnema is an herb that has insulin-modulating activity in those with PCOS, and can reduce elevated triglycerides, which are often also associated with PCOS.
**Important-- Gymnema is not for use during pregnancy or lactation.
Chromium
Chromium picolinate is an essential trace element that is particularly beneficial for insulin-resistant types of PCOS. Research has shown chromium had effects comparable with the drug metformin on ovulation and pregnancy rates, and was better tolerated.
I recommend Thorne Chromium Picolinate, 1000 mcg a day.
Saw Palmetto
Saw palmetto is an herb that can block prolactin receptors on ovarian cells, helping to reduce excess androgens.
Designs for Health Prostate Supreme 2 capsules twice daily.
Bioidentical Progesterone
Using bioidentical progesterone can lower androgens and LH, leading to less ovarian testosterone production. It also blocks 5-alpha reductase, the metabolite that converts testosterone into the more potent DHT, which is often elevated in PCOS. Bioidentical progesterone also slows the and GnRH pulses that are too rapid in people with PCOS, helping to treat the actual root of PCOS.
This is one of my top choices for every woman with PCOS - but be sure to work with a practitioner on this one, as bioidentical progesterone requires specific dosing to be effective and safe.
One thing to note is that adding bioidentical progesterone is not the same as starting a hormonal contraceptive (birth control pills). Birth control pills do not contain bioidentical progesterone - instead they contain artificial progestins, which actually behave more like testosterone in the body.
PCOS Is Complicated, But There Is Hope!
As you can tell by the length of this article, PCOS is incredibly complex. (And I could have written so much more!)
But if you take away only one thing, I hope it’s this: there is hope for effectively treating PCOS.
You don’t just have to suffer through and try to cover up the symptoms. With the right care, you can find and address the root cause.
If you’re ready to start treating your PCOS from the root cause on up, I’d be honored to help guide you there. Having struggled with PCOS myself, helping other women with the condition isn't just my job. It is my passion!
Just click here to book a FREE, no-obligation 15-minute consultation with my team. We use these short calls to get to know you, your health concerns, and see if working together would be a good fit. Think of it like a first date.
Brie
PS - Overwhelmed with all the info on PCOS? I know how that feels, and I’d love to help you find a customized plan (diet, lifestyle, supplements) to help manage PCOS and achieve your health goals. Book a free consultation here so we can chat about a plan for you. (No obligation!)
The Truth About Hormones & Your Sex Drive
Which of these best describes your sex drive?
“Want it, need it, gotta have it!”
“Could take it or leave it...” or
“Don’t even think about it!”
Whatever you answer, there’s no shame.
Women are pretty reluctant to say our libido (or lack thereof) is one of our top health concerns. But when I dig deep with the women I work one-on-one with in my clinic, I find that almost all of them are struggling with their sex drive.
And personally, when I was struggling with hormone imbalance, my sex drive was non-existent. I thought it was just “normal.” After all, as women we are conditioned to believe we should want sex less than men.
Truth: healthy women have robust sex drives!
Our libido isn’t just dictated by whether our partner brings home flowers or we’ve shaved our legs - it is controlled by a complex group of hormones and neurotransmitters. Too much or too little of one or another can cause our sex drive to dwindle away or get out of hand.
That means that if your libido is lacking, you don’t just need to try lighting candles or new lingerie (although if your sex drive is healthy, that would sound fun instead of like a chore!). Balancing your hormones can restore a healthy libido.
Today, I want to explain how your hormones impact your sex drive. I hope this information empowers you - and if you have more questions or need more support, please reach out to me!
What This Article Can’t Do
Before I dig in to all the juicy hormone info, there are a couple other things I want to get out in the open.
First, most of the research on hormones has been done based on cisgender, heterosexual people and in heterosexual relationships. More research on hormones in other populations is long overdue. If you’re outside this group, some of this information will apply to you and some of it won’t - but I’d love to support you in overcoming hormone issues one-on-one until more inclusive research is available.
Secondly - as you're reading this I know symptoms of too much or too little of various hormones are going to jump out at you. But know this: the only way to diagnose hormone imbalances is with proper testing! That means blood, saliva, and/or urine testing.
Treatment for hormone imbalance is highly individualized, and I always recommend anyone who suspects hormone imbalance work one-on-one with a trained practitioner like myself for accurate testing and treatment! At the end of the article, I’ll share about my favorite hormone tests.
OK - disclaimers done - let’s get to the good stuff!
Estrogen - “The Feminine Hormone”
Estrogen is the hormone we associate with women. It makes women softer - both emotionally and physically. Estrogen is responsible for women’s curves: breasts, hips, and more fat on the butt! In studies of heterosexual men, women with higher estrogen levels were rated as more attractive.
It also increases a woman’s receptive sex drive—the part that makes her interested and open to penetration. Estrogen says “Take me now!” Women with higher estrogen levels may have more of a seductive sex drive - they are more likely to be receptive to sex, more likely to flirt and give “I’m available” signals, than they are likely to initiate it.
Testosterone - “The Masculine Hormone”
What hormone causes horniness? Testosterone is the hormone associated with men - but healthy women have testosterone, too. It helps us build muscle and causes us to feel more competitive and aggressive. In the bedroom, testosterone makes us want to initiate sex and governs the drive for genital sex and orgasms. Women with higher testosterone levels tend to have more of an aggressive sex drive and are more likely to initiate sex than wait for a partner to start things up. Interestingly, some post menopausal women have relatively higher testosterone levels (as compared to other hormones like estrogen) and may notice more of an interest in initiating at this phase in their lives.
Testosterone makes us less interested in relationships and commitment and more likely to want time alone (that’s what the Man Cave is for!). Women with higher testosterone levels tend to masturbate more, too. Too much testosterone can make us feel irritable - but too little can make us feel depressed.
Dopamine - “The Pleasure Chemical”
Dopamine isn’t exactly a hormone - it’s actually a neurotransmitter. Dopamine helps us anticipate pleasure - therefore having the drive and motivation to take action. It’s dopamine that makes us anticipate that sex = pleasure.
People who are low in dopamine tend to seem “flat” - they lack interest, enthusiasm, and get-up-and-go.
Testosterone increases the activity of dopamine in our brains, so supplementing with testosterone is often prescribed for women with low libido. But in my experience, this rarely works - or at least not without other support - probably because the issue isn’t just low testosterone, but also low dopamine. (Just another reason why you have to test!)
DHEA - “The Master Hormone”
DHEA is our most abundant circulating hormone. It’s produced both in the Adrenal glands and in the brain, and most of our other hormones are derived from it. DHEA levels peak in our 20s and start to decline from there - faster for some than others based on factors like your genetics and stress. Oral contraceptives are also know to lower DHEA levels.
Ideally, I like to see DHEA levels on the higher end of the normal range because DHEA can:
- Lower risk of depression
- Provide better function in old age
- Protect against immune suppression when cortisol levels are high (from stress)
- Prevent osteoporosis
- Maintain muscle mass
And of course, DHEA plays a major role in sex drive, orgasms, and sex appeal. Higher levels of DHEA in women correlated with higher rates of sexual desirability in studies. Most of our pheromones are derived from DHEA - scents that in the animal world dictate attraction and mating. Pheromones are often what make us feel an “instant connection” or drawn to someone. When a woman complains of low libido, I always test her DHEA levels first!
In times of stress, DHEA levels decrease significantly -and this can cause a cascade of low hormones throughout your body, since most other hormones are derived from DHEA.
Oxytocin - “The Love Molecule”
Oxytocin is a molecule that is triggered by physical touch. Oxytocin levels increase if you hug, hold hands, have sex, hold a baby - and even if you look at a dog! Levels of oxytocin also spike when you’re aroused and when you orgasm - it’s also what causes the uterus to contract during orgasm. If you’re in love, just thinking about the person can make your oxytocin levels go up.
Oxytocin helps you bond and feel love. It’s especially important for maternal bonding, and oxytocin levels rise during breastfeeding. Higher levels of oxytocin both reduce stress and rational thought - making it easier to “fall in love.”
Progesterone - “The Cock Blocker”
Does progesterone increase libido? In my practice I call progesterone the cock-blocking, (or clam-jamming) hormone. Basically, progesterone stops your sex drive. The effect of progesterone on your sex drive is so powerful, monks used to take the herb Vitex (aka Chaste Tree Berry!) to promote progesterone production and block their sex drive. Progesterone actually numbs the erogenous zones, meaning you’re likely to have dull orgasm with more stimulation - or no orgasm at all.
Many women have high levels of progesterone because they take hormonal contraceptives. The birth control pill contains a synthetic form of progesterone called progestin. Great birth control, right? Just kill your sex drive completely!
Progesterone isn’t all bad though - it promotes maternal behavior and has a mild sedative effect. It can make you feel calm, happy, and that everything is a-okay.
Does ovulation make you horny? In the second half of the menstrual cycle (after ovulation), progesterone is naturally higher. That makes sense biologically - once you’ve ovulated, your body won’t drive you to sex for reproductive reasons. When natural progesterone is balanced with estrogen, the dip in sex drive isn’t as strong and some women don’t notice it at all. Others might just be more interested in cuddling rather than going for an orgasm.
Prolactin - “The Nursing Hormone”
Prolactin is mostly associated with lactating women - it is the hormone that triggers your milk to let down after birth. Prolactin also tends to lower your sex drive - that’s why, in general, women have less sex when they are breastfeeding. Depending on your estrogen levels, you might retain some “receptive” sex drive even when prolactin is higher.
Promoting dopamine opposes prolactin. So if your prolactin levels are high and you’re NOT breastfeeding, using dopamine-promoting herbs can help lower prolactin and improve your sex drive. The only way to accurately gauge your prolactin levels is with testing!
Serotonin - “The Happy Chemical”
Serotonin is dopamine’s partner - together they are the two main neurotransmitters in the brain. Serotonin can impact your sex drive whether it’s too high or too low. Certain medications (like SSRIs) can cause high levels of serotonin. Dieting and chronically low calories can cause low serotonin, too.
Very high levels of serotonin dull your sex drive. That's why SSRI antidepressants have lowered sex drive and delayed/weaker orgasms as a side effect.
Conversely, low levels of serotonin can magnify your sex drive. In people with depression, low serotonin levels can even lead to sex addiction. In women with low serotonin, orgasms happen faster and easier. Men with low serotonin ejaculate right away.
Your Menstrual Cycle - “The Conductor”
Your menstrual cycle is like the conductor of all these hormones and chemicals. As the cycle progresses, hormone levels naturally rise and fall, leading to a shift in your sex drive.
At the beginning of your cycle, all hormone levels are low. Mid-cycle, estrogen and testosterone both spike - leading to an increase in sex drive (you’ll be both more aggressive and receptive to sex).
Many women also notice their libido peaks right before they start their period, as progesterone is naturally falling relative to testosterone. Your genitals will be more sensitive and it’s easier to orgasm during progesterone withdrawal.
During menses, some women have an increased sex drive - again because progesterone is lower relative to testosterone. But because serotonin levels can also drop during this time you might be grouchy too. Grumpy and horny!
The natural shift in hormones throughout the month can explain why sometimes you want sex more for the cuddling, emotional bonding, and skin-to-skin contact, - and why other times you just want an orgasm without all the bells and whistles.
Your Hormones & Your Libido
Our sex drive is completely dependent on our hormones. And as you’ve learned in this article, it’s not as simple as “more testosterone makes you horny!” Balanced hormones are the key to a healthy sex drive.
If your sex drive isn’t how you’d like it to be - either too much or too little - looking at your hormone balance is a great place to start. I know you’re sick of hearing me say this by now, but the ONLY way to accurately diagnose hormone imbalance is with advanced testing. You never want to “guess and check” by starting treatments or supplements for what you “think” is the problem. This can cause even greater imbalances that take more time and work to resolve.
Over the years I’ve used blood and saliva hormone tests - but now I almost exclusively use the DUTCH hormone test. This test is a kit your practitioner orders and you complete at home. It uses dried urine (that’s what the D and U stand for in DUTCH) to accurately test various hormone levels. It’s more accurate than saliva testing, and much simpler than blood testing. You just pee on a stick, let it dry, and mail it back to the lab.
Once I know a patient’s hormone levels, we can work together to come up with a plan to balance them. I never share exact protocols publicly because I’ve never had 2 patients who needed the exact same treatment! Hormones really are that unique.
If this article has resonated with you and you think hormone imbalances could be at the root of your sex drive struggles, I hope you’ll book a free 20-minute exploration call with my team. There’s zero obligation, but we’ll dive deep into your issues and then share what we can do to help.
Having come out the other side of hormone imbalance, I can tell you - having my sex drive back is great! (And my husband loves it too.) I want the health and radiance that comes from balanced hormones for all women. Book a 20-minute call for free here!
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
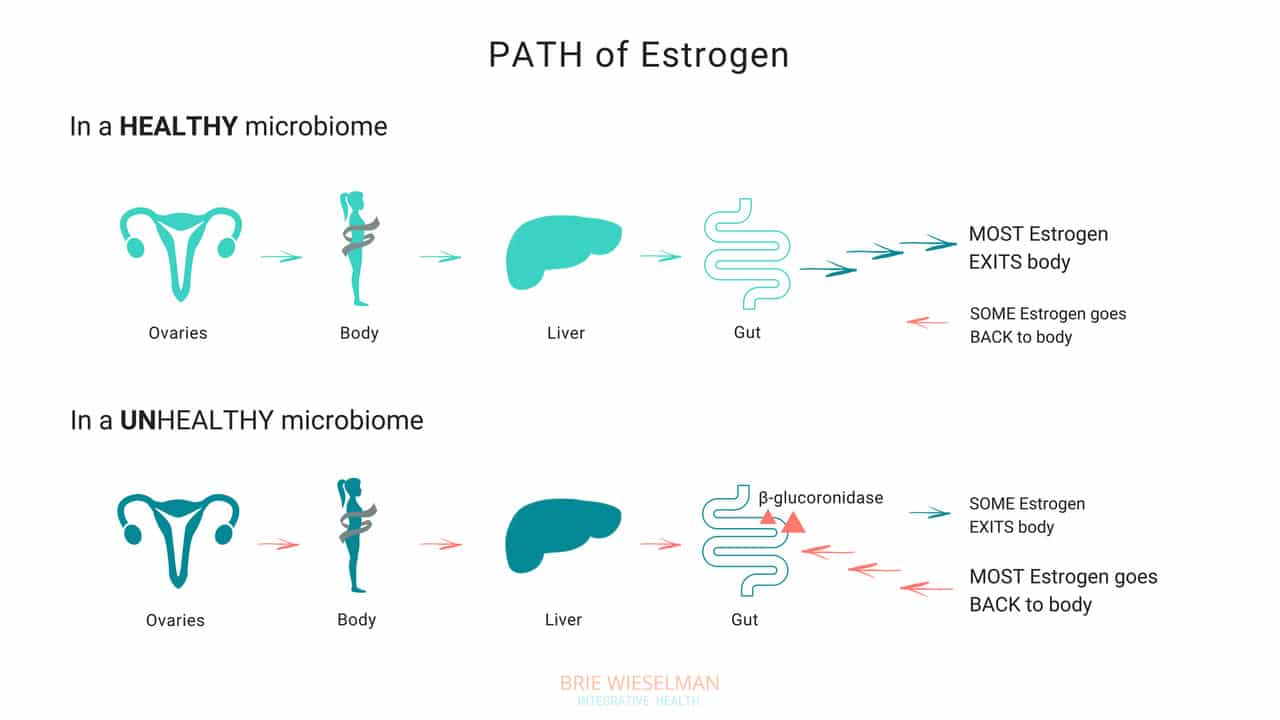
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.