Understanding the Link Between Stress and Perimenopause
Stress - we’re all living with it.
And you don’t need me to tell you stress isn’t great for your health…
But for women in or near perimenopause, stress deserves special mention. Research has shown chronic stress actually worsens the hormonal symptoms of perimenopause, like hot flashes and PMS - as well as weight gain, decreased sex drive, and overall feelings of wellbeing.
But as we all know, “getting rid of” stress really isn’t an option. As a long-time health practitioner, my goal isn’t to help my clients eliminate stress, but rather teach them strategies to better manage stress.
This is especially important during the perimenopause transition, when we are already in a hormonal shift and have less “wiggle room” to manage things like stress, blood sugar imbalances, and inflammation from hidden infections.
But I’m not just talking about starting a meditation practice or saying no to that extra project at work. Targeted use of the right bioidentical hormones, herbs, and adrenal support supplements can help your body handle stress better, and help you transition through menopause seamlessly.
Today, let’s explore what stress and menopause do to the body on a hormonal level - and what we can do to better support the body for more energy, less hormonal symptoms, and a better life.
How Stress Impacts Your Hormones
When I say “hormones” I don’t just mean your sex hormones like testosterone, estrogen, and progesterone. I’m also talking about adrenal hormones like cortisol and DHEA, which play a role in controlling your sex hormones as well.
During perimenopause, hormone levels fluctuate, and it's fluctuating hormones that can cause symptoms like hot flashes, mood swings, and weight gain. Research shows that stress only intensifies this.
Stress triggers the release of cortisol. This is good, as cortisol is the “fight or flight” hormone that helps us respond to danger. But when stress is on-going, it can lead to an on-going state of elevated cortisol. Elevated cortisol in turn depletes the hormone DHEA, which is already in a natural state of decline as we age.
Low DHEA is a problem for anyone, but especially for perimenopausal women because DHEA is a precursor to both testosterone and estrogen. Low levels of DHEA can therefore cause low levels of both testosterone and estrogen, intensifying the already changing hormone levels during this time.
Low DHEA & The Pregnenolone Steal
So far, we’ve covered how stress can lead to elevated cortisol, which causes lower levels of DHEA. Because DHEA is a precursor for testosterone and estrogen, it can impact sex hormones.
But why does elevated cortisol deplete DHEA? That’s thanks to a process commonly called the “Pregnenolone Steal.”
The basic premise of the pregnenolone steal is that pregnenolone - a hormone produced by the adrenal gland - is a precursor for both cortisol and DHEA. When stress is high, the body reacts by producing more and more cortisol, “stealing” all the pregnenolone and leaving none for DHEA production.
That’s a bit of an oversimplification, though. There’s not just one pool of pregnenolone that gets depleted. In reality, pregnenolone is in the mitochondria of each of the cells. Rather than thinking about pregnenolone being stolen, it's more that the body prioritizes some pathways of hormone production that are about survival (cortisol), over reproductive hormones.
That being said, no matter “how” it happens, the decrease in sex hormone production this causes is particularly inopportune during the perimenopause years, when we are already hormonally in shift. It can make it seem like we are more sensitive to stress, or that it takes less stress to cause a noticeable change in how we look and feel. Coexisting issues like blood sugar imbalance or hidden infections - which are other common triggers for cortisol release - might suddenly become a bigger problem, too.
Perimenopause and Low DHEA Symptoms
If you’re dealing with stress related hormone dysfunction on top of perimenopause symptoms, you might feel like you’ve got the worst perimenopause of anyone you know. It can cause an intensification of already-known symptoms like:
- Hot flashes
- Night sweats
- Decreased sex drive (low libido)
- Decreased sexual pleasure
- Weight gain/ weight loss resistance
- Poor sleep
- Increased cravings
- Mood disturbances (depression, anxiety, etc.)
- Low energy
- Overall lack of wellbeing
So that’s the “bad news.” Now let’s talk about the good news - all the things you can do to help rebalance hormones, support your body’s stress response, and get back to feeling like yourself.
In fact, after 1-2 months on a customized plan based on your hormone test results, most of my clients see a 75% or more reduction in symptoms.
Can Hormone Therapy Help Low DHEA and Perimenopause?
For a deep dive into using bioidentical hormones safely during perimenopause, see my blog here.
But in addition to sex hormone replacement therapy, supplementing with hormones like DHEA can be an option too.
When used appropriately - and well monitored - DHEA is a safe way to help increase low testosterone in peri-and menopausal women. (It’s especially great for women with some types of hair loss, too!)
But, DHEA needs to be used carefully. Androgen dominance (too much testosterone) can be a main driver for the development or worsening of insulin resistance in perimenopause.
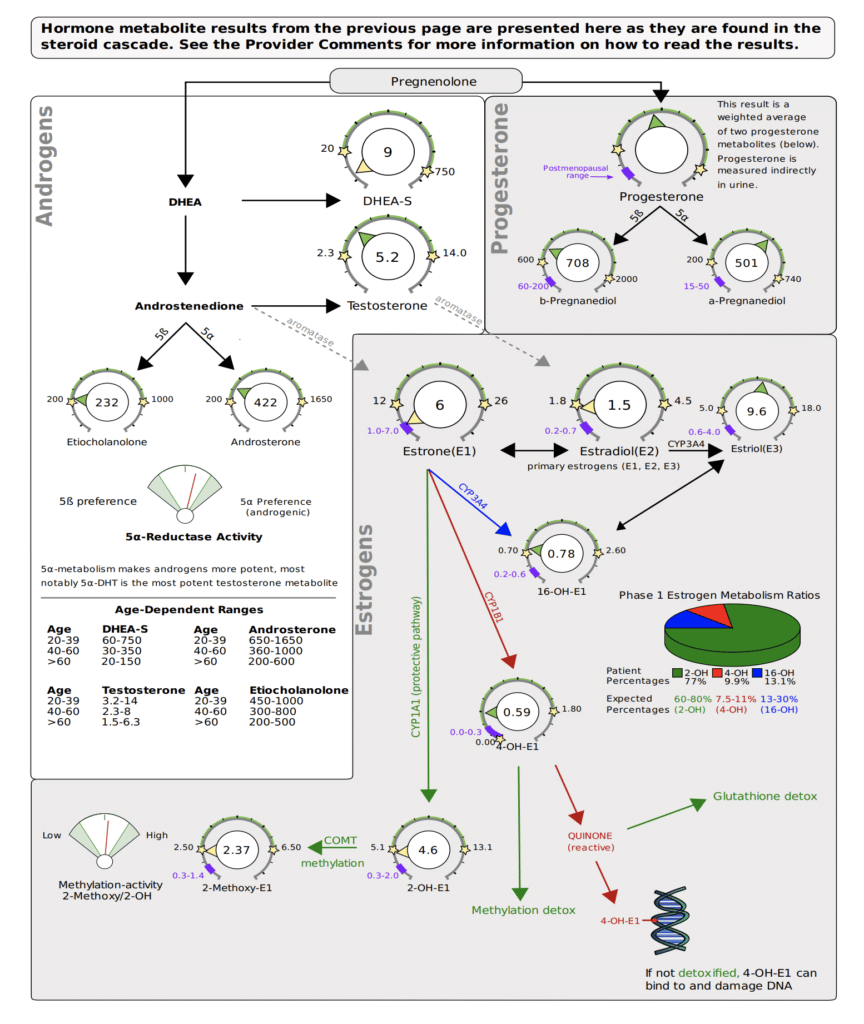
That’s why I always recommend testing before starting DHEA (even if it is available over the counter where you live) and on-going monitoring. I recommend a comprehensive hormone panel like the DUTCH test.
In the clinic, we also use pregnenolone supplementation when using DHEA. This helps with two main problems with DHEA supplementation. First, it can help offset the tendency of DHEA to lower cortisol levels, which can be a problem if someone is already dealing with low HPA output.
Secondly, DHEA has a tendency to put weight on some people, or cause water retention. Adding pregnenolone can prevent this tendency.
Active Stress Management and Supplements
Supplementing with hormones is just one part of the puzzle - just as, if not more, important are complementary lifestyle practices that help manage stress.
I make a custom plan for each of my clients, but some of the techniques we use include:
- Optimizing sleep hygiene (no blue light before bed, etc.)
- Introducing movement (finding an exercise you actually enjoy– and prioritizing muscle building over cardio)
- Circadian alignment (going to bed and rising with the sunset/sunrise)
- Balancing blood sugar and increasing protein intake
- Eliminating/reducing alcohol and processed sugar
Active stress management - like qi gong, walks in nature, meditation in any form, making time for art, getting involved in your community, and spending time with friends and loved ones - are also key.
And then of course there are the issues that you can control - like your relationships, overall task burden, time management, ability to delegate and ask for support, and cutting out toxic people or activities.
These steps can help you eliminate what stress you can and better tolerate the stress you have to live with.
A final piece of the puzzle are adaptogenic herbs and herbs for supplement symptoms. As a long-time Traditional Chinese Medicine practitioner, I’ve seen the incredible power of herbs for transforming health. But, as with all powerful tools, they should only be used after adequate testing or practitioner diagnosis has identified the imbalances that exist.
Look and Feel Your Best in Perimenopause
Perimenopause has a reputation as the worst time in a woman's life… but it doesn’t have to be that way!
With the right support, you can not just survive perimenopause - but actually enjoy the transition and step confidently into a new chapter in your life.
You don’t have to accept weight gain, low sex drive and lack of pleasure, hot flashes, mood swings, cravings, irritability, and all the other common symptoms of perimenopause.
My passion is guiding women through this change, helping to support their body’s unique needs, and watching them thrive in this phase of life!
If you’re interested in learning more, schedule a free 15 minute call by clicking here. We offer different programs for every need and budget, and would love to help you find the support that’s a perfect fit for you.
Pros and Cons of Hormone Replacement Therapy
Mood swings, hot flashes, nigh sweats, weight gain, loss of libido: these are just some of the most common “symptoms” of menopause.
Is it any wonder most women dread this transition?
But what if there was a way to skirt menopauses negative side effects completely, and sail through this major change without sweating, screaming, or stress? According to some, the secret to making it through menopause is hormone replacement therapy (HRT).
But is hormone replacement therapy right for you? Today, let’s talk what happens in the body on the hormonal and chemical level during perimenopuase and menopause, how hormone replacement can and can’t help, and options you have to support this transition even if you’re not interested in HRT.
Menopause vs. Perimenopause: What’s The Difference?
Menopause is defined as going 12 or more months without a menstrual cycle. Perimenopause is the time period - usually several years - leading up to menopause. It’s a transition period sometimes thought of as “puberty in reverse.”
The average age of menopause in the Untied States is 51, and perimenopause usually stars 4-10 years before that. For some women, perimenopause symptoms begin as early as age 35. And if you need another reason to quit, research has shown smokers reach menopause at a younger age than non-smokers.
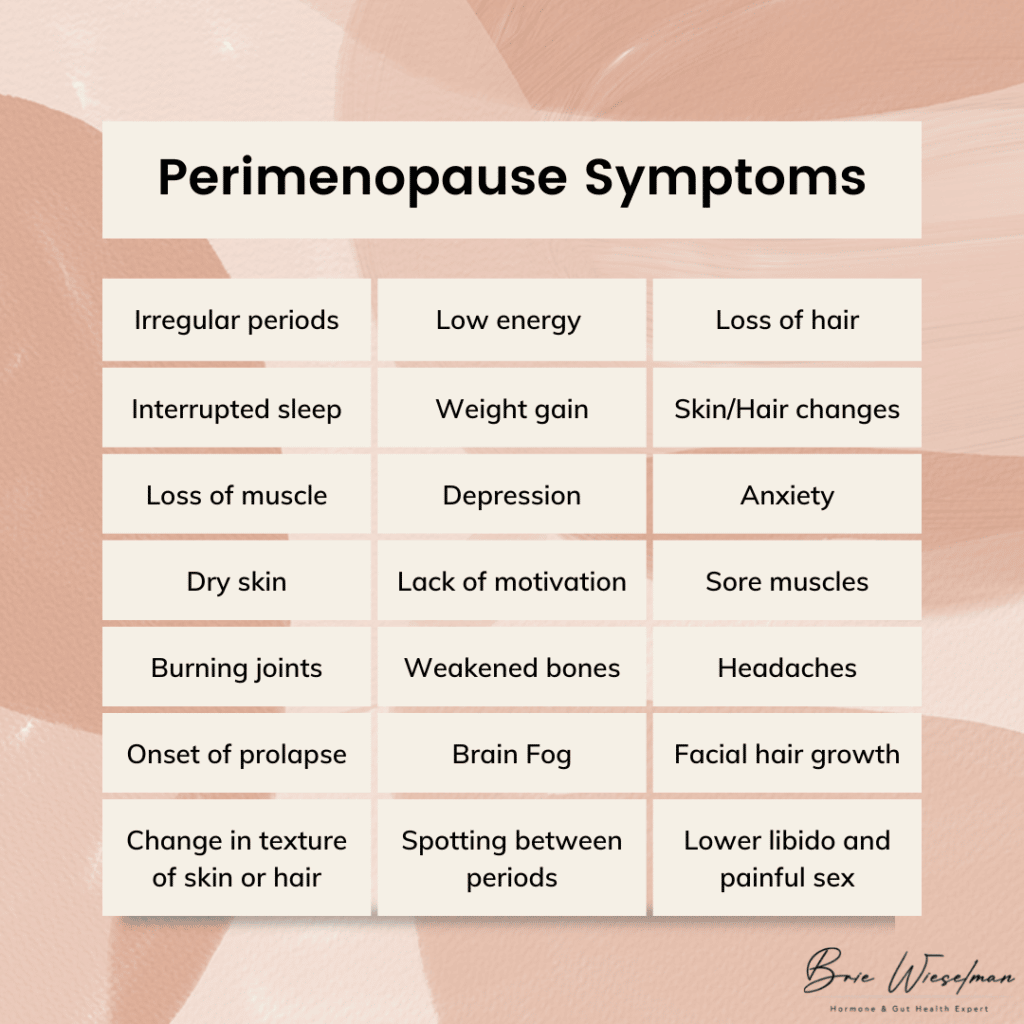 Perimenopause symptoms include:
Perimenopause symptoms include:
- More frequent or heavier periods or missing or less frequent periods
- Interrupted sleep
- Low energy
- Night sweats/hot flashes
- Weight gain
- Change in texture of skin or hair
- Loss of muscle
- Irritability and depression
- Anxiety
- Lack of motivation
- Dry skin
- Sore muscles
- Burning joints
- Weakened bones
- Lower libido and painful sex
- Headaches
- Onset or worsening of prolapse
- Spotting between periods
- Facial hair growth (especially on the chin)
- Loss of hair (on the head)
- Brain fog
Of course, not every woman has every symptom, and it’s not an overnight onslaught. Usually, the first signs of perimenopause are a slightly shortened cycle (think 21-24 days instead of 28) and an increase in PMS symptoms and irritability.
The Hormonal Changes That Cause Menopause
So what is actually happening in the body to cause everything from weight gain to hair loss?
To start, let’s talk about the normal hormone cycle that occurs each month. It all starts in the brain when the hypothalamus signals the pituitary gland via gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In turn, LH and FSH tell the ovaries it’s time to ovulate and release an egg from the follicle. Ovulation triggers the release of estrogen and progesterone. The release of estrogen and progesterone communicate back to the brain that the system has worked, creating a feedback loop.
During the reproductive years, GnRH is produced in a rhythmic cycle, leading to regular cycles. But as we age and enter perimenopause, the release of GnRH becomes more unpredictable. In addition, as we age the ovaries stop responding to LH, leading to erratic ovulation. Because ovulation is what triggers estrogen and progesterone, when ovulation becomes erratic, levels of these hormones drop.
This doesn't happen all at once, though: the changes are often up and down. At first, estrogen levels may shoot up high, then drop back down. Progesterone is only made via ovulation, so it may be irregular in the early stages of perimenopause before beginning a gradual decline. The decline of progesterone often occurs faster than estrogen, leading to temporary estrogen dominance in perimenopause, as well.
The loss of progesterone affects the brain, GABA system, and HPA axis. Allopregnanolone, one type of progesterone, has a calming effect on the brain. Without adequate levels of it, sleep disturbances and reduced ability to cope with stress can occur. The loss of progesterone can also contribute to autoimmunity, especially Hashimoto's thyroiditis. And without the anti-androgenic effect of progesterone, excess androgens can stimulate insulin, contributing to insulin resistance.
In addition to these changes, testosterone, which is produced in the ovaries and adrenal gland, continues to be produced after menopause (though it peaks in the 20s). It is common to go through a phase in perimenopause where testosterone is high relative to estrogen and progesterone, causing symptoms like hair loss, central abdominal weight gain/body shape change, and the onset or worsening of insulin resistance.
Some types of estrogen are produced outside the ovaries. Half of the body’s estrone (one type of estrogen) is made in the fat tissue and adrenal glands, and estrone becomes the predominant estrogen after menopause. This is good for bone density, brain tissue maintenance, and cardiovascular health - we need that estrone! This is why supporting adrenal health is so important for making it through menopause with optimal hormone levels (more on that to come).
The 4 Stages of Perimenopause
From a hormonal standpoint, I like to break perimenopause into 4 stages.
Stage 1: In this stage, estrogen is high, but progesterone levels have started to drop due to an increase in anovulatory cycles (when bleeding occurs and you have a “period” but your body doesn’t ovulate). The luteal phase is often shorter here, but periods might stay regular.
Stage 2: In this phase, estrogen levels are still high but start to fluctuate, causing symptoms associated with estrogen withdrawal, such as hot flashes, migraines, and night sweats. Cycle lengths may vary by as much as 7 days.
Stage 3: Stage 3 is marked by a significant increase in cycle length, going two or more months between cycles. The hormonal changes of Stage 2 remain and/or intensify, and estrogen remains high or rises and drops.
Stage 4: This final stage is often a waiting game: will you get your period again, or are you officially in menopause for good? Estrogen levels are low, unless you get a surprise period, which can raise levels back up temporarily.
Does Menopause Have to Be Miserable?
I could shout it from the rooftops: menopause is not a bad thing, and it doesn’t have to make you feel bad! If there is a menopause problem it’s simply that menopause and modern life are an evolutionary mismatch.
In comparison, the women of the remote Hadza tribe in Tanzania, who still practice hunting and gatherng as a subsistence pattern, don’t experience menopause the way American women do - in fact they report no symptoms associated with menopause, and don’t even have a name for this change.
How can that be? Some of the most important factors might be that Hadza women:
- Have robust gut microbiomes
- Have a strong sense of community and purpose
- Pre-menopausal women rest during their period
- Post-menopausal women eat less and walk more than pre-menopuasal women
- Spend more time pregnant and breastfeeding (and often transition directly from pregnancy/breastfeeding to perimenopause, softening the transition)
- Eat a foraged, high fiber diet without aunty farmed or processed foods
Fortunately, we don’t have to move off the grid to adapt some of these practices to our own lifestyles and reap the benefits. More on my suggestions for how to do this to come.
Understanding Hormone Replacement Therapy for Menopause and Perimenopause Symptoms
Hormone replacement therapy is the use of topical or oral estrogen, progesterone, and sometimes testosterone to temporarily increase hormone levels, treat the symptoms of perimenopause, and improve overall well-being.
Bioidentical hormone replacement therapy (B-HRT) is the use of replacement hormones that are identical to what the body produces. This is in contrast to the use of synthetic hormones, like those found in birth control pills.
As early as the 1930s, women were given placenta as a form of estrogen replacement therapy. In the 1940s, Premarin, a drug made from the urine of pregnant horses, was developed as a HRT. In the 1970s, studies linked estrogen therapy to endometrial cancer, revealing the importance of including progesterone to prevent estrogen-driven cancers.
From the 1960s to the 1990s, hormone replacement therapy grew in popularity. It was marketed as a way to stay youthful and feminine, and was widely used. But then, in the early 2000s, research showed HRT caused a slight increase in the risk of breast cancer, heart disease, stroke and blood clots.
Is Hormone Replacement Therapy Safe?
In 2002, a HRT trial was stopped early because of risks including a small increased risk of breast cancer, heart disease, stroke and blood clots, but fewer cases of hip fractures and colon cancer. This was followed by a 2003 report in the Lancet claiming the use of HRT increased the incidence of breast cancer, even though the data was not strong enough to document a clear harm.
This incomplete information created a change in public opinion that remains today: many women are hesitant to use HRT, even though we now know how to use it safely.
What we now know is that the most important factor for HRT safety is the age at which it is started. HRT is best started as young as possible, while in the perimenopausal window, and ideally continued for no more than 2 years beyond the last period. Starting HRT when older, or after the last period has occurred, increases the risk.
That’s why I’m glad you’re here reading this: if you want to start HRT, starting sooner is safer. But if you feel like you already missed your chance at HRT, and have now “aged out” - don’t give up hope. I have more suggestions for you at the end of this post.
In July 2017, the North American Menopause Society (NAMS) relased thier positon after reviewing the data amassed from millions of women usign HRT over several decades, and concluded the benefits of HRT outweigh the risk for healthy women, when HRT is started at the proper age. They found that being obese or having 4 or more alcohlic drinks per week actually increased the risk of breast cancer more than the proper use of HRT. Women using HRT had a 4 in 1000 chance of breast cancers vs a 3 in 1000 chance in women not using HRT.
In addition, they found there was no increased risk of heart attacks in women using HRT as long as they started taking HRT within 10 years of their last period or started between the age of 50 and 59.
In particular, bioidentical hormones are safer than synthetic hormones. Bioidentical progesterone likely decreases the risk of breast cancer, whereas synthetic progestins increase the risk. If started early in perimenopause, bioidentical hormones are actually heart protective as opposed to a risk factor for heart disease.
Pros and Cons of Hormone Replacement Therapy
When used correctly, the benefits of hormone replacement therapy include:
- Fewer hot flashes
- Improved insomnia & sleep disturbances
- Improved anxiety & depression
- Less brain fog
- Fewer menopausal symtoms in general
The primary cons are the potential slightly increased risk of breast cancer and heart disease.
When deciding to start hormone replacement therapy, there’s a lot to consider. Here’s some of what I go over with patients while developing a treatment plan:
- Age and proximity to menopause (starting earlier is generally better)
- History of breast cancer (self and family)
- Genetic predisposition to hormonal cancers
- Risk of cardiovascular disease (I screen for factor V and prothrombin in all patients before starting HRT)
The type of hormone therapy used matters, too. Options include pills, gels, creams, patches, troche, and liquids. While gels, creams, and patches are common , I actually prefer oral micronized progesterone, or, nanoliposomal topical serum. Most topical progesterones aren’t able to deliver a high enough dose to protect the uterine lining. In addition, there’s no “regular” rate of absorption for creams, gels, or patches. Each woman’s unique physiology determines how much and how fast she will absorb topical hormones. Topical progesterone can also be stored in the fat, then “dumped” by the body, leading to irregular levels in the blood, damaging the sensitive feedback loop in the brain. When used for longer periods of time, I’ve also seen fat-based topical progesterone build up to higher than physiologically normal levels, eventually causing progesterone receptor resistance, much like insulin resistance. When a woman has been using topical progesterone, has normal or even high levels when tested, but still has the symptoms of low progesterone, this is usually the reason.
Whatever form you choose, careful monitoring before, during and after use is an absolute must. After initial testing, hormones should be retested within 3 months of starting HRT to assess if levels need adjusting, as well as how estrogens are metabolized. Women often assume they need estrogen, but actually just need progesterone to start, as progesterone is often low relative to estrogen in early menopause. Progesterone can help with symptoms like night sweats and hot flashes just as much (if not more) than estrogen. When estrogen is needed, estradiol and estriol are both very safe when used in combination with progesterone.
I use the DUTCH Complete Estrogen metabolism test, and look to make 2-OH as high or higher than all types of estrogen and other metabolites, for optimal, safe metabolism.
I also want 4-OH to be moderate to lower, at least not higher than 2-OH.
Alternatives & Complements to Hormone Replacement Therapy
Ready to start hormone replacement therapy? You’ll get the best results when also addressing your glucose, gut, and adrenal health in check, while paying attention to your diet, exercise, social life, and life purpose.
But even if you decide against HRT, addressing these other aspects of your health can have a radical impact on how you feel during perimenopause and menopause.
Eat For Balanced Blood Sugar
Research has linked hot flashes to insulin resistance, finding that glucose levels and the degree of insulin resistance rose as the frequency of hot flashes rose. Glucose levels were 33% higher in women who reported hot flashes 1 to 5 days per week than in those who reported no hot flashes. In another study of 6,000 menopausal women, diets high in fat and sugar led to a 20-percent increase in hot flashes and night sweats. After working with hundreds of women in my clinic, I’ve found that the more stable we keep their glucose levels, the fewer menopause symptoms they have.
Ditch Caffeine
There may be a link between caffeine use and certain menopause symptoms — namely, hot flashes and other symptoms related to the body's regulation of the diameter of blood vessels (vasomotor symptoms).
Avoid Spicy Foods
Like alcoholic beverages, spicy food causes vasodilation of the blood vessels, triggering hot flashes.
Eliminate or Reduce Alcohol
Cut back on drinks to 2 or less per week. When you do drink, expect to see menopause symptms return that night. (And surprisingly, wine is usually worse than clear spirits in this case - so maybe go with the vodka soda!) Cutting alcohol and sugar completely eliminates or minimizes night sweats and hot flashes in most women I see.
Exercise Regularly
Movement is always great, but it's most effective if you’ve been moving regularly in the time leading up to perimenopause, and then keep moving. Too much exercise or high intensity can actually trigger hot flashes because of the influence on blood flow to brain and skin and how the brain regulates body temperature.
Do Active Stress Management Daily
This can look like meditation, relaxation tracks, or hypnosis. CBT has also been shown to be very effective, especially in women who can’t use HRT due to breast cancer.
Support Gut Health
The gut plays a major role in the production and clearance of hormones. I always recommend a comprehensive gut health test and gut health practices like using a probiotic.
Try Phytoestrogen Foods
In some cases, phytoestrogen-rich foods like soy and legumes can be helpful.
Rehab Your Adrenals
Your adrenals are responsible for synthesizing appropriate levels of testosterone, progesterone, and estrogen in the perimenopause transition and beyond. Test your hormones with a DUTCH Complete panel and work with a practitioner who can create a customized protocol to rehab your adrenal hormone function.
Get Personalized Help with Hormone Replacement Therapy & Menopause
If you’re entering perimenopause (or already in the thick of it), hormone replacement therapy can help ease the transition. But even if you’re not ready (or not interested in) HRT, using diet, lifestyle, and herbs can help significantly. Either way, you don’t have to just accept the night sweats, hot flashes, weight gain, and mood swings - we can help!
If you’re looking for support in menopause, perimenopause, HRT, or natural alternatives to HRT, click here to book a free consult with our team.
We’ve helped hundreds of women in this life transition, and we’d be honored to help you, too.
Dude, Where’s My Period?
Where's my period? To some women, it sounds like a dream…
And when it happens to you, at first you might think… “Hey, that's really not so bad.”
But as a functional medicine practitioner, I can assure you:
Your period going missing IS a problem.
(Or rather, it indicates a problem!)
Today, let’s dig into why your period is so important, and why it might have gone missing (AKA amenorrhea). Plus, how worried should you really be?
Why Your Period Is Really, Really Important
For women of reproductive age, there’s really no other health marker as important as your menstrual cycle.
A normal menstrual cycle is anywhere from 24-35 days long and includes 4 parts:
- Menstrual Phase - this is what we think of as your period, the part of your cycle when you bleed. Hormones are lower at this point.
- The Follicular Phase - this occurs after your period, and is really the start of a new cycle, when the body prepares for potential pregnancy. Hormone levels rise during this part of the cycle as the body prepares an egg to be released during ovulation.
- Ovulation - this is the day somewhere in the middle of your cycle when your body releases an egg in response to peaking LH (luteinizing hormone) levels. Ovulation causes progesterone levels to rise.
- The Luteal Phase - this is the phase after ovulation, when you either get pregnant (which must happen within a few days of ovulation), or don’t. If you don’t get pregnant, you move back to phase 1 and have your period again.
And while talk of the menstrual cycle is very procreation-focused, your menstrual cycle actually isn’t just about getting pregnant or not.
The hormones that are driven to rise and fall by your menstrual cycle play other important roles in your health - most importantly, progesterone, which keeps bones strong and healthy and lowers the risk of certain cancers.
Not only that, but your hormones are meant to exist in balance: each hormone is counterbalanced by another, and if you’re not moving through each phase of the cycle, you can become dominant in one hormone - most commonly estrogen, which should be balanced by adequate progesterone. Estrogen dominance can lead to symptoms like weight gain, mood swings, tender/swollen breasts, and loss of libido.
That’s why moving through each phase of your menstrual cycle is so important, even if you’re not looking to have a baby now (or ever).
If Your Period Is MIA, You Probably Aren’t Ovulating
When you ovulate, an egg is released from the follicle. That follicle becomes the corpus luteum. The corpus luteum produces progesterone, which tells the body to build up a thick lining in the uterus.
If you don’t become pregnant, the corpus luteum withers, and the uterine lining is shed as your period.
What this means is that having a period - where you shed blood - is entirely dependent on ovulating. If you don’t ovulate, there won’t be a follicle to turn into the corpus luteum, so your body won’t be told to build up the uterine lining, and there won’t be anything to shed.
What I’m getting at is that a missing period tells us you’re not ovulating. And that’s what really matters, because it is ovulation that produces estrogen-balancing, bone-protecting, cancer-risk-reducing progesterone.
Now there are a couple exceptions: some women who ovulate irregularly may have bleeding, even without ovulation. It is more likely that you won’t - but it can happen.
Secondly, women who are on hormonal contraceptives (the birth control pill), may bleed every month, but are not ovulating (because hormonal contraceptives suppress ovulation). The “period” that you have on a hormonal contraceptive shouldn’t be thought of as a true period. Instead, it is actually a “withdrawal bleed” because the bleeding is triggered by the withdrawal from the artificial hormones during the placebo week of your birth control pill.
Is Your Period Up and Gone, Or Just Flaky?
When I’m working with a patient who has missing periods, here are some of the questions I ask to help point me in the right direction toward the cause, and ultimately, the solution.
Did you ever have normal cycles?
If you used to have normal, predictable cycles - and then suddenly they stopped or became unpredictable, that suggests to me something has disrupted your otherwise healthy hormones. If you’ve never had a normal cycle, all’s not lost- it just points me in a different direction.
Has your period been gone for months (or years) straight, or is it just unpredictable?
A period that comes and goes can suggest oligoovulation - which means ovulation is unpredictable. Anovulation is the complete absence of ovulation. Again, neither one means all hope is lost: this can just help suggest what might be going on.
Did you have any major life changes around the time your period disappeared?
This is another important detective question. The menstrual cycle is delicate - and is designed to prevent pregnancy during times of extreme stress or upheaval (since having a baby in a famine or war wasn’t really ideal for our ancestors!). It’s a good idea to try and create a timeline of when your period went missing and what was going on in your life at that time.
Reasons Your Period Could Be Missing
Now that you know why it matters that your period is missing, let’s get into the good stuff: figuring out why your period is gone!
Here is a list of the most common causes of a missing period I see with my patients:
Pregnancy
Ok, this one is pretty obvious: if you’re pregnant, you won't have your period. Luckily, it’s also really easy to rule out: if there’s any chance you could be pregnant, take a pregnancy test and know for sure.
Perimenopause
On the opposite end of the spectrum from pregnancy is the possibility of perimenopause. Perimenopause is the years-long period before the onset of menopause, when your hormone levels start fluctuating and your periods can become suddenly abnormal. In perimenopause, you might have longer cycles (34+days), skip a few cycles, or have lighter or heavier periods. Other perimenopause symptoms include mood changes, hot flashes, and night sweats. Perimenopause begins for most women sometime in their 40s - if you think you’re experiencing perimenopause early, that is something we can address. Even if you’re the “right age” for perimenopause to have begun, it is a myth that perimenopause has to be a horrible time. There is so much we can to help stabilize hormones and provide symptom relief as your body goes through this big (normal) change.
Polycystic Ovarian Syndrome (PCOS)
PCOS is a hormonal disorder that affects millions of women (myself included). It is distinguished by elevated levels of androgens (male hormones) and the absence of regular ovulation. (Remember, no ovulation = no period.) PCOS is complex to both diagnose and treat - but it can be done. Click here to read my ultra in-depth blog post on all aspects of PCOS and learn more about treatments.
It should be noted that PCOS can occur alongside another cause of a missing period, commonly hypothalamic amenorrhea (HA).
Hypothalamic Amenorrhea (HA)
Hypothalamic amenorrhea (amenorrhea is the technical term for a MIA period) is a hormone imbalance that prevents ovulation caused by 1) over-exercise, 2) stress, 3) undereating, or 4) some combination of all 3. If you used to have normal cycles, and suddenly lost them, HA is one to consider. Your physiology is designed to prevent ovulation (and therefore, reproduction) when stress is high or nutrition levels are low, and HA is a result of this. Some women experience HA even when at a normal weight, or doing an amount of exercise that is deemed normal by society. Developing HA is all about crossing your body’s threshold, and that level is different for all women.
There is no definitive test for HA, and it is usually diagnosed by eliminating other causes of a missing period first. If you have HA, learning to manage stress, eating more, and exercising less can all lead to the restoration of normal cycles, though the process can take time.
HA can occur alongside PCOS, but doesn’t always.
Premature Ovarian Failure
This condition occurs when the ovaries stop functioning normally at an early age. This can cause irregular, come-and-go periods, rather than a complete stop.The exact cause of premature ovarian failure is unknown, though its thought genetics and autoimmunity may play a role. Unfortunately, premature ovarian failure usually causes infertility, but treatment with bioidentical hormones can help manage other symptoms.
High Prolactin
Prolactin is the hormone that causes the breasts to produce milk, and it also suppresses ovulation. If you’re breastfeeding exclusively, high levels of prolactin can keep your period at bay. But if you’re not breastfeeding, high prolactin indicates a serious issue. It can be a result of a tumor on the pituitary gland or thyroid issues. Besides a missing period, tell-tale signs to look for are a milky discharge from the breasts, vaginal dryness, and acne.
Hormonal Contraceptives
Hormonal contraceptives (AKA the birth control pill, patch, ring or hormonal IUD) work by suppressing your body’s natural production of hormones and replacing them with artificial counterparts. Most hormonal contraceptives suppress ovulation, and the only “period” you get is a withdrawal bleed during the placebo week of the pill. Some pills allow you to skip the placebo week - sometimes called continuous pills - and skip the withdrawal bleed altogether. One exception is the hormonal IUD (Mirena), which doesn’t always stop ovulation, but often still causes lighter or absent periods.
So, does this mean hormonal contraceptives are bad? It’s a little more complicated than that. Hormonal contraceptives have a time and place. However, there are other non-hormonal birth control options I prefer - check those out here. And I don’t like seeing hormonal contraceptives used as a “treatment” for hormone issues like PCOS or heavy periods, because all they can do is cover up these issues, not fix the root cause.
Post-Pill Amenorrhea or Post-Pill PCOS
Recently stopped using hormonal contraceptives? That could be a cause of a missing period. Post-pill amenorrhea is a condition where periods remain absent after going off the pill. When you’re using hormonal contraceptives, your body’s normal hormone production is shut off. When you quit the pill, it can take time for hormone production to normalize, and a missing period can be the result. This should resolve in a couple months - if it takes longer, seek help. With my clients, focusing on diet, lifestyle, and key supplements can help speed up this process. Post-pill PCOS is similar - when hormones come back online after using the pill, androgens (male hormones) may surge, causing a temporary state of PCOS. Jumping in right away to help normalize hormone levels can help prevent this imbalance from becoming permanent. See this post for more on PCOS.
Stress, Illness, or Travel
One of the simple explanations of a missed cycle? Periods of intense stress - whether psychological or physical, which can result in missing or delayed periods. The “stress hormone” cortisol is to blame. When you experience stress, your body produces more cortisol to help you respond to the stress. However, cortisol also interferes with communication between your brain and ovaries, where hormones are produced, preventing ovulation and therefore, your period. One missed or late cycle after a period of stress is likely NBD - as long as things normalize again quickly. But if you are chronically stressed, there are steps we can take to support your body in managing cortisol to hopefully take the burden off your menstrual cycle.
Chronic Disease
This is one of the less common reasons I see for missing periods, but it does happen. Again, your body will shut down reproduction first thing if it senses you’re not well enough to successfully reproduce, as a protection mechanism. If you have a chronic disease that is constantly taxing your body, it makes sense that your cycle could be disrupted. Most commonly, I see this with women with undiagnosed or poorly managed Celiac disease, since Celiac prevents proper nutrient absorption and causes chronic inflammation. Treating the chronic condition (and getting it under control) can help restore normal cycles again.
Thyroid Issues
An overactive or underactive thyroid (Hypo or hyper hypothyroidism) can also be a cause of missing or skipped periods, among other symptoms like feeling hot/cold, weight gain or loss, and hair loss. If you’re missing your period, and don’t know why, a full thyroid panel is a great place to start to rule out the possibility of thyroid issues.
How Do I Know Why MY Period Is Missing?
Now that you know the most common reasons your period could be missing, the next step is to narrow it down to what the issue is for you.
Some of these potential issues are easy enough to rule out, but for the rest, testing is the next best step. With my own clients who are struggling with amenorrhea, I use a combination of blood, saliva, and urine tests to help narrow down the root cause. (And if you are working with me, I’ll help you figure out which tests you can ask your regular doc to order and bill through insurance, too!)
Once we know the root cause, we can create a customized treatment plan to help restore ovulation and normal, healthy cycles.
If you’re missing your period and need support finding the root cause and getting it back, book a free 15-minute consult to get started working with me. This no-obligation first call is like a coffee date where we can test the waters and see if working together might be a good fit.
>>> Book a no-obligation free consultation <<<
Whether you’re trying to get pregnant or just worried about what a missing period means for your ehealth, I’d be honored to help get your cycles back on schedule.
Brie
PS - If there's ONE thing you take from this article, let it be this: missing your period is NOT normal, and needs to be addressed! In fact, a missing period is a major red flag that something is not quite right with your health. Don’t ignore it!