Did you just reread that title 3 times? Then read on, this one’s for you! 😜
Introduction: Angela’s Journey
Meet Angela, a 45-year-old marketing director renowned for her sharp focus and meticulous work ethic, who recently began noticing unsettling changes in her cognitive functions.
“Let me tell you, it’s been quite the shift,” she tells me. “I used to have my mornings down to a science, but now, it’s like I’m always scrambling for my keys, which I’ve misplaced yet again. And it’s not just annoying—it really throws off my whole schedule since I end up running late.”
“And meetings? I used to be the one leading the charge, but lately, I stumble over my words, my thoughts scattering like marbles. It’s these little things… they’re adding up, you know?” she pauses, collecting my thoughts. “I’ve been dealing with ADHD for years, but this feels different. My friend was talking about an article she’d read about perimenopause, and it got me starting to think there might be a connection between the hormonal changes and my ADHD symptoms intensifying. It’s a lot to wrap my head around”.
Angela’s days are peppered with these small but significant disruptions: memory lapses, a sense of disorganization, and a once-unshakable concentration that now seems just out of reach.
This revelation sparked a quest for a more integrated treatment approach, one that would harmonize her hormonal health and neurological needs. Now, as Angela navigates her daily responsibilities against the backdrop of these challenges, she is more determined than ever to find balance and clarity amidst the chaos.
Understanding Neurodiversity: A Broader Perspective
The concept of neurodiversity acknowledges the rich variety of human brains and minds, seeing neurological differences such as ADHD, autism, and dyslexia not as deficits, but as natural variations in the human condition, with inherent challenges as well as distinct strengths. Neurodiversity can include both developmental and acquired changes in brain function due to injury or illness, along with transient neurodiverse states that affect how our brains work, like those brought on by hormonal shifts or stress. (**Note, if you don’t have an ADHD diagnosis formally, but are curious, this is my favorite self-assessment quiz. It highlights both strengths and challenges that are characteristic of the ADHD brain).
Is Perimenopause a type of transient neurodiversity?
Did you know that menopause can really shake things up for your brain? That’s right—perimenopause is actually a time of acquired neurodiversity, where the natural shifts in your body can significantly affect how your brain works. Common issues like forgetting where you put your keys, having trouble staying focused, or feeling moodier than usual are all part of this transition. These challenges are often made worse by other symptoms of perimenopause, such as sleep problems and emotional ups and downs.
Women with known ADHD entering perimenopause often find that the strategies they previously used to manage their symptoms are less effective. The additional cognitive load imposed by hormonal fluctuations can exacerbate previously compensated ADHD symptoms, making them more severe and harder to manage.
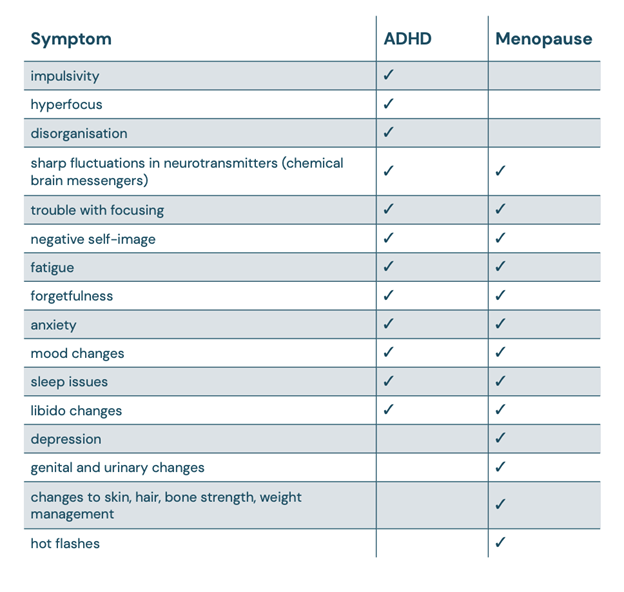
There’s a pretty noticeable overlap between perimenopause/menopause symptoms and ADHD. Once you stack up the list of what’s common to both, it’s clear to see why things might feel a bit more overwhelming when you hit perimenopause and menopause. Those ADHD symptoms you’ve been managing? They could get trickier to handle during these changes. So, if you’re feeling a bit off during this time, there’s a good biological reason for it.
What’s happening behind the scenes? Well, it’s all about hormones. The ebb and flow of estrogen and progesterone during perimenopause don’t just affect your body; they also mess with your brain’s chemical messaging system and even the flow of blood in your brain.
The Estrogen-ADHD Connection: Exploring Estrogen’s Impact on Neurotransmission
Estrogen plays a crucial role in the brain, especially in how it relates to ADHD. This hormone helps regulate neurotransmitters like dopamine and serotonin, which are key players in managing our mood, focus, and overall executive functions. When women go through significant hormonal changes, like during perimenopause, the rollercoaster of estrogen levels can lead to a spike in ADHD symptoms. This is often due to what’s known as estrogen withdrawal, where the sudden drop in estrogen levels disrupts the normal balance of neurotransmitters, making symptoms more noticeable.
Estrogen and Serotonin
Estrogen isn’t just about mood swings—it’s a big player in how your brain handles serotonin, which you totally need for nailing those executive functions and keeping your emotions on an even keel. Here’s a kicker: when your estradiol levels dip, studies have shown that the hippocampus (yep, that’s the part of your brain where long-term memories chill) can shrink by up to 40%. Don’t panic, though—this doesn’t mean your memories are wiped; it’s more like the pathways to access them aren’t as wide open as before. The hippocampus is like the central hub for your personality, storing all those experiences and interactions that make you, well, you. So, maintaining healthy estrogen levels is pretty essential not just for remembering where you left your keys, but for keeping ‘you’ feeling like ‘you.’
Estrogen’s Influence on Dopamine
Estrogen plays a pivotal role in regulating dopamine, a neurotransmitter that’s essential for our reward system and focus mechanisms. Low dopamine can feel like a persistent fog of fatigue, lack of motivation, and difficulty finding joy or satisfaction in activities that normally feel rewarding. Research has shown that estrogen helps manage how dopamine transporters and receptors function in the brain. As women enter perimenopause and their estrogen levels start to wane, so does the regulation of dopamine, which can intensify ADHD symptoms.
The Relationship Between Estrogen and Acetylcholine
Years of research have highlighted the critical role of the central nervous system’s cholinergic systems in our ability to learn, remember, and pay attention. Estrogen also significantly influences acetylcholine, another key neurotransmitter that’s crucial for learning and memory. Studies have repeatedly shown that estradiol bolsters various cognitive processes, enhancing attention and boosting both verbal and visual memory. However, during perimenopause, as estrogen levels decline, the production of acetylcholine also tends to decrease.
While Ritalin and similar stimulants are commonly used to manage ADHD, they primarily target dopamine pathways and are generally more effective in treating severe inattention rather than milder forms. These medications can improve tasks involving visual memory but often fall short in enhancing focus amid distractions or in complex task planning– because they fail to directly support acetylcholine function. Additionally, they come with a host of potential side effects, ranging from mild (sleep disturbance, anxiety, reduced appetite, or headaches) to more serious risks (increased blood pressure and risk of stroke and heart attack, development of or worsening of manic symptoms or other psychiatric conditions, decreased bone density with higher risk for early onset osteoporosis and higher fracture risk).
Unlike these stimulants, strategies that support acetylcholine can offer broader cognitive benefits. Both personally and clinically, I have found the supplement Optimal Focus by Seeking Health, to be incredibly valuable as a component of a well-rounded ADHD support program. It includes ingredients like Ginkgo Biloba and Huperzine A. These components are intended to enhance cognitive functions such as memory and attention, providing a more comprehensive approach to managing ADHD symptoms, particularly in women experiencing perimenopause. This combined support for both dopamine and acetylcholine pathways could be key in developing more effective ADHD treatments.
Histamine: Beyond Allergies, A Neurotransmitter with Wide-Ranging Effects
Histamine is well-known for its role in allergic reactions—think sneezing, itching, and red eyes. But histamine’s job description goes way beyond making us miserable during allergy season. It’s also a key neurotransmitter, playing roles in our digestion, sleep-wake cycles, mood and brain function. This makes it a substance of interest not just for allergists but for anyone interested in maintaining optimal health.
When Histamine Highs Lead to Health Lows
Histamine’s influence extends into what’s known as Speer Allergic Tension-Fatigue Syndrome (SATFS), a condition marked by fatigue, irritability, depression, and cognitive fog–often alongside typical allergic symptoms like asthma and eczema. This overlap hints that when dealing with persistent allergies and cognitive or mood disruptions, histamine could be a common denominator.
DAO: The Histamine Handler
Central to managing histamine levels in the body is the enzyme diamine oxidase (DAO). DAO is primarily responsible for breaking down histamine that our bodies produce, preventing its accumulation. In the context of Attention Deficit Hyperactivity Disorder (ADHD), DAO’s role becomes particularly significant. Research suggests that reduced DAO activity could lead to heightened histamine levels, potentially exacerbating or contributing to ADHD symptoms.
How Perimenopause Amplifies Histamine
Estrogen dominance is characterized by either high levels of estrogen or insufficient progesterone to counterbalance estrogen’s effects. This hormonal imbalance can lead to an increase in histamine levels because estrogen can stimulate the release of histamine from immune cells known as mast cells. When estrogen levels are high, more histamine is released, which can exacerbate symptoms like allergies, hives, mood swings and anxiety– and ADHD symptoms.
On the other hand, progesterone naturally helps to regulate and stabilize mast cell membranes, preventing them from releasing histamine unnecessarily. Low levels of progesterone, therefore, can lead to increased histamine release because there’s less hormonal regulation keeping mast cell activity in check. Progesterone also upregulates the production of DAO, the enzyme that helps break down histamine.
For women in various stages of perimenopause, these mechanisms are particularly relevant. During perimenopause, hormone levels fluctuate significantly, and periods of estrogen dominance accompanied by low progesterone are common. These hormonal shifts can result in increased histamine-related symptoms, which may manifest as worsening allergies, sleep disturbances, or changes in mood, brain function, focus, and emotional well-being.
Keeping Histamine in Check
Several factors can cause histamine levels to get out of hand:
- Genetic Factors: Variations in genes like HNMT or DAO can slow down histamine breakdown, leading to higher levels.
- Nutrient Deficiencies and Liver Detoxification Pathways: Certain nutrients are crucial for breaking down histamine. Without them, our bodies struggle to keep histamine levels balanced.
- Gut Health: A healthy gut is critical for producing DAO. If the gut is compromised, so is DAO production, which can lead to increased histamine. Additionally, the presence of specific types of gut pathogens (certain bacteria, parasites, or candida overgrowth) can stimulate the production of higher levels of histamine.
- Diet and Lifestyle: Certain foods and lifestyle factors can trigger histamine release or inhibit DAO, exacerbating symptoms.
For those wrestling with ADHD understanding and managing histamine levels can be transformative. This is just one reason why an integrative approach that considers hormone balance, gut health, detox support, and potentially using supplements to support DAO production can be very effective for some women. By addressing histamine management from multiple angles, it’s possible to achieve a better balance and improve overall mood and cognitive function.
Bringing It All Together: ADHD, Perimenopause, and Whole-Body Health
When it comes to managing ADHD symptoms during perimenopause, hormone replacement therapy (HRT) really should be on your radar. HRT can help stabilize those roller-coaster hormone levels, easing some of the intensified ADHD symptoms that come with this life stage. This approach is a breath of fresh air compared to just ramping up doses of stimulant medications, which often miss the mark on addressing the deeper hormonal imbalances and can leave you dealing with some pretty annoying side effects.
But there’s more to the story than just hormones. Keeping your blood sugar stable throughout the day with a well-rounded diet can make a huge difference in how you feel—think fewer energy crashes and mood swings that can kick your ADHD into overdrive. Also, giving a boost to your brain’s neurotransmitters with the right supplements or botanicals can really sharpen your mental clarity and help your brain stay on point.
Don’t overlook the importance of checking for food sensitivities either. Figuring out if certain foods are causing you trouble and cutting them out can seriously help calm ADHD symptoms and boost your overall well-being. And let’s not forget about gut health—it’s a game changer. A happy gut means better detox, better nutrient absorption, and better overall hormone and neurotransmitter balance, which all adds up to you feeling better.
Tackling ADHD during perimenopause with these strategies offers a well-rounded approach that looks at your health from multiple angles.
Give yourself some grace during this transition! Embracing tools like notepads, organization apps (Sunsama, Inflow, Focus@Will) and reminders to help bridge memory gaps is a smart strategy, not a setback. It’s also perfectly okay to take a bit more time with tasks or to ask for help. Remember, you’re navigating a significant shift—this isn’t about failure, it’s about adapting and finding strength in vulnerability. Treat yourself with kindness and compassion as you adjust.
References
- Eng, A. G., Nirjar, U., Elkins, A. R., Sizemore, Y. J., Monticello, K. N., Petersen, M. K., Miller, S. A., Barone, J., Eisenlohr-Moul, T. A., Martel, M. M. (2023). Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. University of Kentucky, Department of Psychology. Link to article
- Roberts, B., Eisenlohr-Moul, T., Martel, M. M. (2018). Reproductive Steroids and ADHD Symptoms Across the Menstrual Cycle. Psychoneuroendocrinology, 88, 105–114. PMC5803442
- Jongkees, B. J., Hommel, B., Colzato, L. S. (2014). People are different: tyrosine’s modulating effect on cognitive control in healthy humans may depend on individual differences related to dopamine function. PMC4186281
- Perimenopause, Menopause and ADHD. (2023). Cambridge University Press. Journal of the International Neuropsychological Society
- Roberts, B. A. (2016). Ovarian Hormones, ADHD, Risk-Taking, & Impulsivity. University of Kentucky. Link to thesis
- ADHD Symptoms in Females of Childhood, Adolescent, Reproductive and Menopause Period. (2021). Mater Sociomed, 33(2), 114–118. PMC8385721
- Cumulative exposure to ADHD medication is inversely related to hippocampus subregional volume in children. (2021). Neuroimage Clin., 31, 102695. PMC8141923
- Estrogen-Cholinergic Interactions: Implications for Cognitive Aging. (2015). Horm Behav., 74, 173–185. PMC4573353
- Johansson, J., Landgren, M., Fernell, E., et al. (2013). Decreased binding capacity (B max) of muscarinic acetylcholine receptors in fibroblasts from boys with attention-deficit/hyperactivity disorder (ADHD). ADHD Atten Def Hyp Disord, 5, 267–271. Link to article
- The diamine oxidase (DAO) enzyme, which metabolizes histamine extracellularly, could contribute to ADHD symptoms. PMC10455974
At the Reverse-Age Method, we believe in a holistic approach to perimenopause and beyond, that addresses the root causes of your symptoms (like insomnia, hot flashes, night sweats, erratic periods, fatigue, skin aging, weight gain, and brain fog)– to also slow the pace that your cells are aging. Whether it’s improving gut health, optimizing detox function, enhancing mitochondrial function, or building muscle mass, our comprehensive program has got you covered.
If you’re new here, be sure to check out our Blog Page for more insights and tips on how to thrive during perimenopause. Our blog is packed with practical advice, success stories, and the latest research to help you on your journey.
For more updates and community support, follow us on social media:
You May Also Like...
It Takes Two To Tango: Testing Your Household for Candida Overgrowth and Common Bugs
You’ve done a full lab work-up with a functional medicine provider and found out you’ve got an overgrowth of some bugs.…
PCOS 101: Everything You Need to Know About Polycystic Ovarian Syndrome
I’ve been where you are right now… Maybe your doctor just told you, “You have PCOS.” Maybe you’re questioning it…
Whether you’re looking for help with your gut, your hormones, or both, our team of practitioners work together to treat the WHOLE you – guiding you to a healthier mind, body, and spirit day by day.



