Mood swings, hot flashes, nigh sweats, weight gain, loss of libido: these are just some of the most common “symptoms” of menopause.
Is it any wonder most women dread this transition?
But what if there was a way to skirt menopauses negative side effects completely, and sail through this major change without sweating, screaming, or stress? According to some, the secret to making it through menopause is hormone replacement therapy (HRT).
But is hormone replacement therapy right for you? Today, let’s talk what happens in the body on the hormonal and chemical level during perimenopuase and menopause, how hormone replacement can and can’t help, and options you have to support this transition even if you’re not interested in HRT.
Menopause vs. Perimenopause: What’s The Difference?
Menopause is defined as going 12 or more months without a menstrual cycle. Perimenopause is the time period – usually several years – leading up to menopause. It’s a transition period sometimes thought of as “puberty in reverse.”
The average age of menopause in the Untied States is 51, and perimenopause usually stars 4-10 years before that. For some women, perimenopause symptoms begin as early as age 35. And if you need another reason to quit, research has shown smokers reach menopause at a younger age than non-smokers.
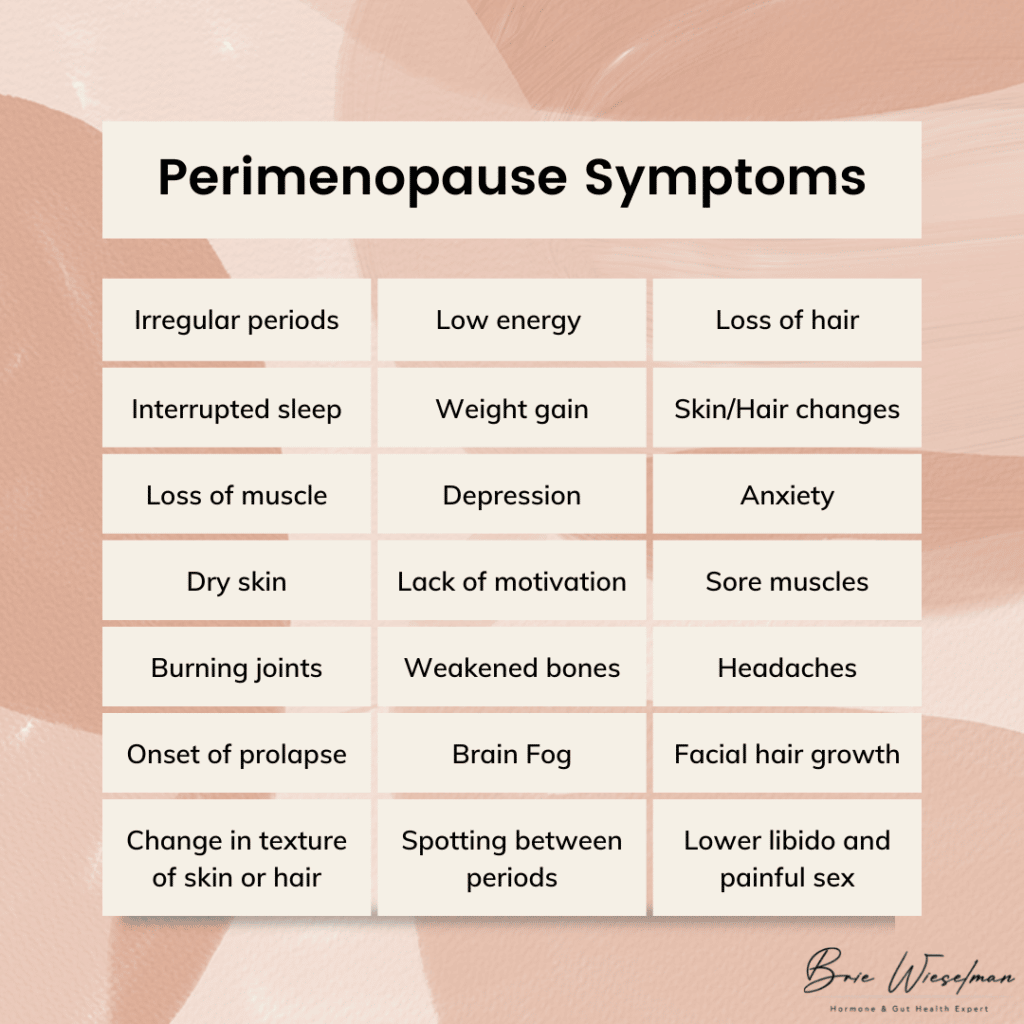 Perimenopause symptoms include:
Perimenopause symptoms include:
- More frequent or heavier periods or missing or less frequent periods
- Interrupted sleep
- Low energy
- Night sweats/hot flashes
- Weight gain
- Change in texture of skin or hair
- Loss of muscle
- Irritability and depression
- Anxiety
- Lack of motivation
- Dry skin
- Sore muscles
- Burning joints
- Weakened bones
- Lower libido and painful sex
- Headaches
- Onset or worsening of prolapse
- Spotting between periods
- Facial hair growth (especially on the chin)
- Loss of hair (on the head)
- Brain fog
Of course, not every woman has every symptom, and it’s not an overnight onslaught. Usually, the first signs of perimenopause are a slightly shortened cycle (think 21-24 days instead of 28) and an increase in PMS symptoms and irritability.
The Hormonal Changes That Cause Menopause
So what is actually happening in the body to cause everything from weight gain to hair loss?
To start, let’s talk about the normal hormone cycle that occurs each month. It all starts in the brain when the hypothalamus signals the pituitary gland via gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In turn, LH and FSH tell the ovaries it’s time to ovulate and release an egg from the follicle. Ovulation triggers the release of estrogen and progesterone. The release of estrogen and progesterone communicate back to the brain that the system has worked, creating a feedback loop.
During the reproductive years, GnRH is produced in a rhythmic cycle, leading to regular cycles. But as we age and enter perimenopause, the release of GnRH becomes more unpredictable. In addition, as we age the ovaries stop responding to LH, leading to erratic ovulation. Because ovulation is what triggers estrogen and progesterone, when ovulation becomes erratic, levels of these hormones drop.
This doesn’t happen all at once, though: the changes are often up and down. At first, estrogen levels may shoot up high, then drop back down. Progesterone is only made via ovulation, so it may be irregular in the early stages of perimenopause before beginning a gradual decline. The decline of progesterone often occurs faster than estrogen, leading to temporary estrogen dominance in perimenopause, as well.
The loss of progesterone affects the brain, GABA system, and HPA axis. Allopregnanolone, one type of progesterone, has a calming effect on the brain. Without adequate levels of it, sleep disturbances and reduced ability to cope with stress can occur. The loss of progesterone can also contribute to autoimmunity, especially Hashimoto’s thyroiditis. And without the anti-androgenic effect of progesterone, excess androgens can stimulate insulin, contributing to insulin resistance.
In addition to these changes, testosterone, which is produced in the ovaries and adrenal gland, continues to be produced after menopause (though it peaks in the 20s). It is common to go through a phase in perimenopause where testosterone is high relative to estrogen and progesterone, causing symptoms like hair loss, central abdominal weight gain/body shape change, and the onset or worsening of insulin resistance.
Some types of estrogen are produced outside the ovaries. Half of the body’s estrone (one type of estrogen) is made in the fat tissue and adrenal glands, and estrone becomes the predominant estrogen after menopause. This is good for bone density, brain tissue maintenance, and cardiovascular health – we need that estrone! This is why supporting adrenal health is so important for making it through menopause with optimal hormone levels (more on that to come).
The 4 Stages of Perimenopause
From a hormonal standpoint, I like to break perimenopause into 4 stages.
Stage 1: In this stage, estrogen is high, but progesterone levels have started to drop due to an increase in anovulatory cycles (when bleeding occurs and you have a “period” but your body doesn’t ovulate). The luteal phase is often shorter here, but periods might stay regular.
Stage 2: In this phase, estrogen levels are still high but start to fluctuate, causing symptoms associated with estrogen withdrawal, such as hot flashes, migraines, and night sweats. Cycle lengths may vary by as much as 7 days.
Stage 3: Stage 3 is marked by a significant increase in cycle length, going two or more months between cycles. The hormonal changes of Stage 2 remain and/or intensify, and estrogen remains high or rises and drops.
Stage 4: This final stage is often a waiting game: will you get your period again, or are you officially in menopause for good? Estrogen levels are low, unless you get a surprise period, which can raise levels back up temporarily.
Does Menopause Have to Be Miserable?
I could shout it from the rooftops: menopause is not a bad thing, and it doesn’t have to make you feel bad! If there is a menopause problem it’s simply that menopause and modern life are an evolutionary mismatch.
In comparison, the women of the remote Hadza tribe in Tanzania, who still practice hunting and gatherng as a subsistence pattern, don’t experience menopause the way American women do – in fact they report no symptoms associated with menopause, and don’t even have a name for this change.
How can that be? Some of the most important factors might be that Hadza women:
- Have robust gut microbiomes
- Have a strong sense of community and purpose
- Pre-menopausal women rest during their period
- Post-menopausal women eat less and walk more than pre-menopuasal women
- Spend more time pregnant and breastfeeding (and often transition directly from pregnancy/breastfeeding to perimenopause, softening the transition)
- Eat a foraged, high fiber diet without aunty farmed or processed foods
Fortunately, we don’t have to move off the grid to adapt some of these practices to our own lifestyles and reap the benefits. More on my suggestions for how to do this to come.
Understanding Hormone Replacement Therapy for Menopause and Perimenopause Symptoms
Hormone replacement therapy is the use of topical or oral estrogen, progesterone, and sometimes testosterone to temporarily increase hormone levels, treat the symptoms of perimenopause, and improve overall well-being.
Bioidentical hormone replacement therapy (B-HRT) is the use of replacement hormones that are identical to what the body produces. This is in contrast to the use of synthetic hormones, like those found in birth control pills.
As early as the 1930s, women were given placenta as a form of estrogen replacement therapy. In the 1940s, Premarin, a drug made from the urine of pregnant horses, was developed as a HRT. In the 1970s, studies linked estrogen therapy to endometrial cancer, revealing the importance of including progesterone to prevent estrogen-driven cancers.
From the 1960s to the 1990s, hormone replacement therapy grew in popularity. It was marketed as a way to stay youthful and feminine, and was widely used. But then, in the early 2000s, research showed HRT caused a slight increase in the risk of breast cancer, heart disease, stroke and blood clots.
Is Hormone Replacement Therapy Safe?
In 2002, a HRT trial was stopped early because of risks including a small increased risk of breast cancer, heart disease, stroke and blood clots, but fewer cases of hip fractures and colon cancer. This was followed by a 2003 report in the Lancet claiming the use of HRT increased the incidence of breast cancer, even though the data was not strong enough to document a clear harm.
This incomplete information created a change in public opinion that remains today: many women are hesitant to use HRT, even though we now know how to use it safely.
What we now know is that the most important factor for HRT safety is the age at which it is started. HRT is best started as young as possible, while in the perimenopausal window, and ideally continued for no more than 2 years beyond the last period. Starting HRT when older, or after the last period has occurred, increases the risk.
That’s why I’m glad you’re here reading this: if you want to start HRT, starting sooner is safer. But if you feel like you already missed your chance at HRT, and have now “aged out” – don’t give up hope. I have more suggestions for you at the end of this post.
In July 2017, the North American Menopause Society (NAMS) relased thier positon after reviewing the data amassed from millions of women usign HRT over several decades, and concluded the benefits of HRT outweigh the risk for healthy women, when HRT is started at the proper age. They found that being obese or having 4 or more alcohlic drinks per week actually increased the risk of breast cancer more than the proper use of HRT. Women using HRT had a 4 in 1000 chance of breast cancers vs a 3 in 1000 chance in women not using HRT.
In addition, they found there was no increased risk of heart attacks in women using HRT as long as they started taking HRT within 10 years of their last period or started between the age of 50 and 59.
In particular, bioidentical hormones are safer than synthetic hormones. Bioidentical progesterone likely decreases the risk of breast cancer, whereas synthetic progestins increase the risk. If started early in perimenopause, bioidentical hormones are actually heart protective as opposed to a risk factor for heart disease.
Pros and Cons of Hormone Replacement Therapy
When used correctly, the benefits of hormone replacement therapy include:
- Fewer hot flashes
- Improved insomnia & sleep disturbances
- Improved anxiety & depression
- Less brain fog
- Fewer menopausal symtoms in general
The primary cons are the potential slightly increased risk of breast cancer and heart disease.
When deciding to start hormone replacement therapy, there’s a lot to consider. Here’s some of what I go over with patients while developing a treatment plan:
- Age and proximity to menopause (starting earlier is generally better)
- History of breast cancer (self and family)
- Genetic predisposition to hormonal cancers
- Risk of cardiovascular disease (I screen for factor V and prothrombin in all patients before starting HRT)
The type of hormone therapy used matters, too. Options include pills, gels, creams, patches, troche, and liquids. While gels, creams, and patches are common , I actually prefer oral micronized progesterone, or, nanoliposomal topical serum. Most topical progesterones aren’t able to deliver a high enough dose to protect the uterine lining. In addition, there’s no “regular” rate of absorption for creams, gels, or patches. Each woman’s unique physiology determines how much and how fast she will absorb topical hormones. Topical progesterone can also be stored in the fat, then “dumped” by the body, leading to irregular levels in the blood, damaging the sensitive feedback loop in the brain. When used for longer periods of time, I’ve also seen fat-based topical progesterone build up to higher than physiologically normal levels, eventually causing progesterone receptor resistance, much like insulin resistance. When a woman has been using topical progesterone, has normal or even high levels when tested, but still has the symptoms of low progesterone, this is usually the reason.
Whatever form you choose, careful monitoring before, during and after use is an absolute must. After initial testing, hormones should be retested within 3 months of starting HRT to assess if levels need adjusting, as well as how estrogens are metabolized. Women often assume they need estrogen, but actually just need progesterone to start, as progesterone is often low relative to estrogen in early menopause. Progesterone can help with symptoms like night sweats and hot flashes just as much (if not more) than estrogen. When estrogen is needed, estradiol and estriol are both very safe when used in combination with progesterone.
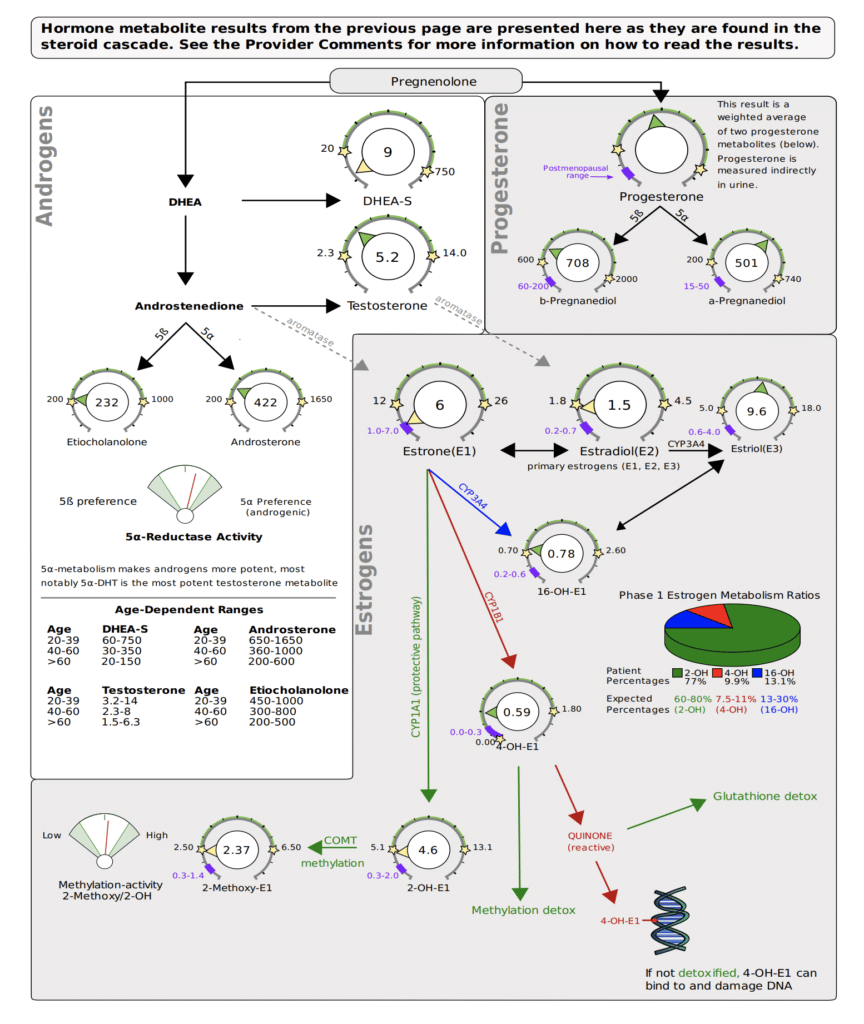
I use the DUTCH Complete Estrogen metabolism test, and look to make 2-OH as high or higher than all types of estrogen and other metabolites, for optimal, safe metabolism.
I also want 4-OH to be moderate to lower, at least not higher than 2-OH.
Alternatives & Complements to Hormone Replacement Therapy
Ready to start hormone replacement therapy? You’ll get the best results when also addressing your glucose, gut, and adrenal health in check, while paying attention to your diet, exercise, social life, and life purpose.
But even if you decide against HRT, addressing these other aspects of your health can have a radical impact on how you feel during perimenopause and menopause.
Eat For Balanced Blood Sugar
Research has linked hot flashes to insulin resistance, finding that glucose levels and the degree of insulin resistance rose as the frequency of hot flashes rose. Glucose levels were 33% higher in women who reported hot flashes 1 to 5 days per week than in those who reported no hot flashes. In another study of 6,000 menopausal women, diets high in fat and sugar led to a 20-percent increase in hot flashes and night sweats. After working with hundreds of women in my clinic, I’ve found that the more stable we keep their glucose levels, the fewer menopause symptoms they have.
Ditch Caffeine
There may be a link between caffeine use and certain menopause symptoms — namely, hot flashes and other symptoms related to the body’s regulation of the diameter of blood vessels (vasomotor symptoms).
Avoid Spicy Foods
Like alcoholic beverages, spicy food causes vasodilation of the blood vessels, triggering hot flashes.
Eliminate or Reduce Alcohol
Cut back on drinks to 2 or less per week. When you do drink, expect to see menopause symptms return that night. (And surprisingly, wine is usually worse than clear spirits in this case – so maybe go with the vodka soda!) Cutting alcohol and sugar completely eliminates or minimizes night sweats and hot flashes in most women I see.
Exercise Regularly
Movement is always great, but it’s most effective if you’ve been moving regularly in the time leading up to perimenopause, and then keep moving. Too much exercise or high intensity can actually trigger hot flashes because of the influence on blood flow to brain and skin and how the brain regulates body temperature.
Do Active Stress Management Daily
This can look like meditation, relaxation tracks, or hypnosis. CBT has also been shown to be very effective, especially in women who can’t use HRT due to breast cancer.
Support Gut Health
The gut plays a major role in the production and clearance of hormones. I always recommend a comprehensive gut health test and gut health practices like using a probiotic.
Try Phytoestrogen Foods
In some cases, phytoestrogen-rich foods like soy and legumes can be helpful.
Rehab Your Adrenals
Your adrenals are responsible for synthesizing appropriate levels of testosterone, progesterone, and estrogen in the perimenopause transition and beyond. Test your hormones with a DUTCH Complete panel and work with a practitioner who can create a customized protocol to rehab your adrenal hormone function.
Get Personalized Help with Hormone Replacement Therapy & Menopause
If you’re entering perimenopause (or already in the thick of it), hormone replacement therapy can help ease the transition. But even if you’re not ready (or not interested in) HRT, using diet, lifestyle, and herbs can help significantly. Either way, you don’t have to just accept the night sweats, hot flashes, weight gain, and mood swings – we can help!
If you’re looking for support in menopause, perimenopause, HRT, or natural alternatives to HRT, click here to book a free consult with our team.
We’ve helped hundreds of women in this life transition, and we’d be honored to help you, too.
At the Reverse-Age Method, we believe in a holistic approach to perimenopause and beyond, that addresses the root causes of your symptoms (like insomnia, hot flashes, night sweats, erratic periods, fatigue, skin aging, weight gain, and brain fog)– to also slow the pace that your cells are aging. Whether it’s improving gut health, optimizing detox function, enhancing mitochondrial function, or building muscle mass, our comprehensive program has got you covered.
If you’re new here, be sure to check out our Blog Page for more insights and tips on how to thrive during perimenopause. Our blog is packed with practical advice, success stories, and the latest research to help you on your journey.
For more updates and community support, follow us on social media:
You May Also Like...
A Functional Medicine Practitioner’s Approach To Treating IBD
When a patient visits me for the first time with inflammatory bowel disease (IBD)—ulcerative colitis or Crohn’s—they’re…
How To Treat Depression & Anxiety Holistically – Part Two
In Part One of this series, I delved into the fact that depression and anxiety are not problems of JUST the brain or…
Whether you’re looking for help with your gut, your hormones, or both, our team of practitioners work together to treat the WHOLE you – guiding you to a healthier mind, body, and spirit day by day.