Adrenal Fatigue Part 1: Stress and Your Symptoms--What Exactly IS Adrenal Fatigue?
This is Part 1 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it!
Last Sunday evening, I drove across town to meet up with a girlfriend. My husband Jacob and I had driven up the coast from our house in Santa Cruz, on highway 1, to go for a hike that morning. I had just gotten on the road to my friend’s house when I noticed my gas light was on. I drive a Honda Fit, and they never run out of gas. They get incredible mileage, so even when they are “out of gas”, you still have at least 20 miles.
On my way home, I was planning to stop to fill the tank, but decided I’d go first thing in the morning, and headed home instead. Big mistake.
The gas station is less than a mile from my house, but when I went the next morning, I was 100 yards away from it when my car….Slowly….Trudged…To..A. stop.
I was stuck in the middle lane during morning rush hour, people honking at me and yelling out their windows, with my hazard lights flashing, as I tried to push my car to the side of the road. How embarrassing! I haven’t done something like this since I was probably 16 years old!
It was another hour before I’d gotten my tank filled again and was on with my day, running late for my first appointment….sigh…
Not exactly how I wanted to spend my morning. As I rushed non-stop into my full schedule, I noticed that for the rest of the day I felt frazzled. Any capacity deal with an unexpected change of plans, or handle any conversation that required effort or patience went out the window. I wished that I’d had 10-minutes to meditate and re-center myself
When Jacob got home at the end of the day, he took one look at me and just laughed!
"Rough day, Babe?"
Luckily, after a warm bath, some gentle yoga, and a good night’s sleep, I woke up feeling refreshed and ready to charge Tuesday! But several years ago, when my adrenal hormones were on the fritz, a hectic day like Monday would have left me sleepless, exhausted, and stressed out for several days or more…..
It’s well established that all modern diseases and their symptoms are negatively impacted by chronic stress.
From PMS, to susceptibility to the common cold, to an increased tendency to develop chronic diseases like cancer and diabetes, stress clearly promotes the development and prevents healing of a multitude of health concerns.
If we feel stressed out all the time, the impact it has on our physiology can override the benefits that healthy nutrition and exercise provide to your body.
But what exactly is happening in your body when this occurs?
What Is Adrenal Fatigue?
There is a ton of misinformation about Adrenal Fatigue out there in Google-landia. Adrenal Fatigue is not a disease. It’s a syndrome that occurs as a consequence of chronic stress without relief, and is characterized by predictable symptoms like fatigue, poor mood swings, insulin resistance or low blood sugar swings, decreased sex drive, insomnia, increased susceptibility to colds and flus, and worsening PMS or menopausal symptoms. These are just a few of the signs that you might have imbalanced stress hormone levels.
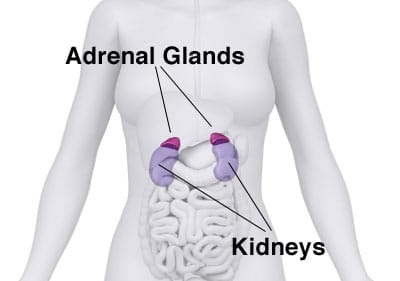
Your adrenals are two small pyramid-shaped glands that sit on top of each of your kidneys. The adrenals are responsible for the production of several types of hormones—glucocorticoids, mineralocorticoids, and androgens. Cortisol, our main adrenal hormone, is made mostly in the adrenal cortex (some is also produced in the mitochondria of cells around the body). Cortisol is often referred to as our “stress hormone”—and it can get a bad rap. More aptly it could be called our “stress response” hormone—and, while we don’t want it to be super elevated for prolonged periods of time, it’s also not great for it to get overtly low.
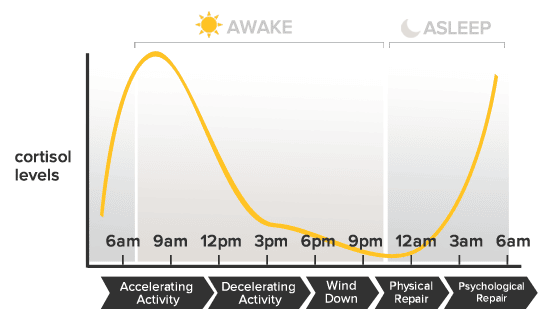
In truth, cortisol (along with meltonin) is one of the primary hormones that establishes our circadian rhythm, or sleep and wake cycle, in response to cycles of light and darkness. We want cortisol to spike highest within the first 30 minutes of opening our eyes in the morning, and then to gradually taper off over the course of the day, hitting its lowest point in the evening when we naturally fall asleep.
We need a moderate amount of cortisol to circulate daily to maintain body tissues, provide energy, put out inflammation, and to serve other vital metabolic functions. When we get in to trouble is when we keep giving our body the message to pump out high levels all the time.
Chronically high cortisol leads to:
-Imbalanced female hormones
-Increased rates of depresssion
-Increased fat storage, especially spare tire, which is good if you are in a famine, in order to survive, but not good if you are trying to look good in that cute new bikini.
-Lower thyroid hormone function and production
-Overall tissue breakdown and poor repair of injuries
-Increased risk of heart attack and stroke
-Increased risk of cancer
-And those are just to name a few...
On labs, Adrenal Fatigue is characterized when the current level of hormones produced by your adrenal glands (like cortisol) are consistently above or below the optimal ranges, or, when the daily circadian rhythm is doing something other than it should be (like being high at night and low in the morning!).
But don’t be fooled. Just because it’s not a diagnosable “disease” doesn’t mean that it can’t have a profound effect on your wellbeing! In fact, Adrenal Fatigue is often an early-warning sign of increased vulnerability to a variety of diseases and conditions such as diabetes, depression, autoimmune disease, thyroid disorders, and more.
The good news is that Adrenal Fatigue is measurable and fixable!
A trained professional can guide you through diet and lifestyle improvements, along with the strategic use of supplement and herbal protocols, to help get you back on the path to wellness.
If you think you might have Adrenal fatigue, (also called "HPA-Axis Dysregulation"--but more about in the upcoming posts) let’s get on the phone and talk about it, so that I can support you!
Click Here for the next section in this series where we’ll talk about what it feels like to have imbalanced adrenal hormones.
Adrenal Fatigue/HPA-D Part 2: How Adrenal Fatigue Feels
This is Part 2 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! To read more about the basics of Adrenal Fatigue, go to part 1, here.
The first time I ran adrenal testing on myself, I was completing my 4th year of Chinese Medicine School. After seeking help from all the best practitioners I knew (Acupuncturists, Herbalists, Ayurvedic practitioners, Nutritionists, and my gynecologist), I was desperately looking for answers to my intractable insomnia. A regular night looked like me getting in bed around 10:30 PM, and then laying awake, frustrated, anxious, and worried, until around 3 AM or later. Beside my bed was an arsenalt of herbs and supplements that at best, helped me fall asleep an hour or two earlier, some of the time.
I still had to be to clinic or class by 8 am most mornings, and prided myself on giving my all to my patients and my studies, and maintaining a workout schedule, even on 3-5 hours of sleep. After 3 years of this, I began to wonder if I was ever going to get a normal, full night of sleep again! It was my own personal kind of hell, and it had gone on waaaaay to long.
If you are living with “Adrenal Fatigue” (also called HPA-Axis dysregulation), you probably live what appears to be a normal life from the outside.
Most people can do the things they have always done and may not have any obvious signs of severe physical illness.
However, you’ll typically have a general overall feeling of burn-out, general fatigue, or a kind of flat tone to their previously vibrant lives. Or, you might not feel fatigued; instead you might feel constantly wired, or even have a hard time winding down at the end of the day.
These people often use mild stimulants like coffee to get themselves going in the morning, and keep themselves going throughout the day. In the more progressed cases, people can be so exhausted that it’s hard to get out of bed for more than a few hours per day.
Some Signs of Adrenal Fatigue Include:
- An overreaction to perceived stressors—like the pressure of writing a school paper.
- An increased susceptibility to colds, flus, and infections
- An inability to regulate blood sugar –getting shakey or spacey between meals.
- An extra 5 pounds of fat that you just can’t lose around your stomach, or 10+ that showed up out of no where and won’t budge no matter what you do!
- Feeling frazzled to the point of road rage, getting easily frustrated or overwhelmed, snapping at your partner or kids, or crying for no particular reason
- Feeling fatigued, especially if you wake up wanting to go back to bed
- Wanting to nap or snack between 3-5 pm—especially if you feel more alert and alive after 6 pm than you do all day
- Difficulty falling asleep or staying asleep
- Worsening PMS, or menopausal symptoms like hot flashes and night sweats
- Nonexistent or decreased sex drive
- Easy bruising, more easily injured, or prolonged healing time
- Lacking the same zest and drive for the things in life that used to drive you
- You want to exercise, but just can’t push it as hard, or, you feel achy or fatigued later.
- Low or high blood pressure
- Difficulty bouncing back from stress or illness
While none of the above symptoms are life-threatening in the immediate, left untreated, imbalanced cortisol levels can lead to chronic disease states down the road.
Some of the risks of untreated HPA-Axis Dysregulation/ Adrenal Fatigue are:
- Greater risk of diabetes
- Increased rates of autoimmune disease
- Increased risk of cancer
- Osteopenia or Osteoporosis
- Increased risk of Alzheimer’s
- Loss of muscle mass
- Increased rates of heart disease
- Greater chance of depression
- Higher overall inflammation.
HPA-Axis Dysregulation/ Adrenal fatigue is defined by abnormal levels or rhythms of cortisol, the main hormone produced by the adrenal glands in response to signaling from your brain. We’ll go into more depth about how this occurs, in my next post. Essentially, testing and treating adrenal hormone imbalances is not just important for feeling better now, it’s also critical for maintain long term health and well-being.
To read more about what happens in your body when stress activates your adrenal glands, click here to read Part 3.
Adrenal Fatigue Part 3: Adrenal Fatigue is actually a BRAIN problem!
This is Part 3 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read Part 1 and Part 2.
In the Parts 1 and 2, we talked about how adrenal fatigue (HPA-D) feels, and associated symptoms and disease states. But what is actually going on in our body when we experience stress, that leads to these changes and symptoms?
(warning: this post gets a bit more technical, so read on if you’re curious…or skip it and click here to get support)
How Your Adrenals and HPA-axis Work:
You are planting a garden outside of your hut, when a hungry bear and her 3 cubs stroll out of the forest. You know a hungry momma bear is not to be messed with.Your brain goes into“high alert” and, in a split second, you decide to run.
The shift into Fight-or-flight mode occurs because your brain perceives some type of danger or stressor.
This decision took you less than 2 seconds, but in that time, a complex chain of events occurred before you were able to get into Go-mode:
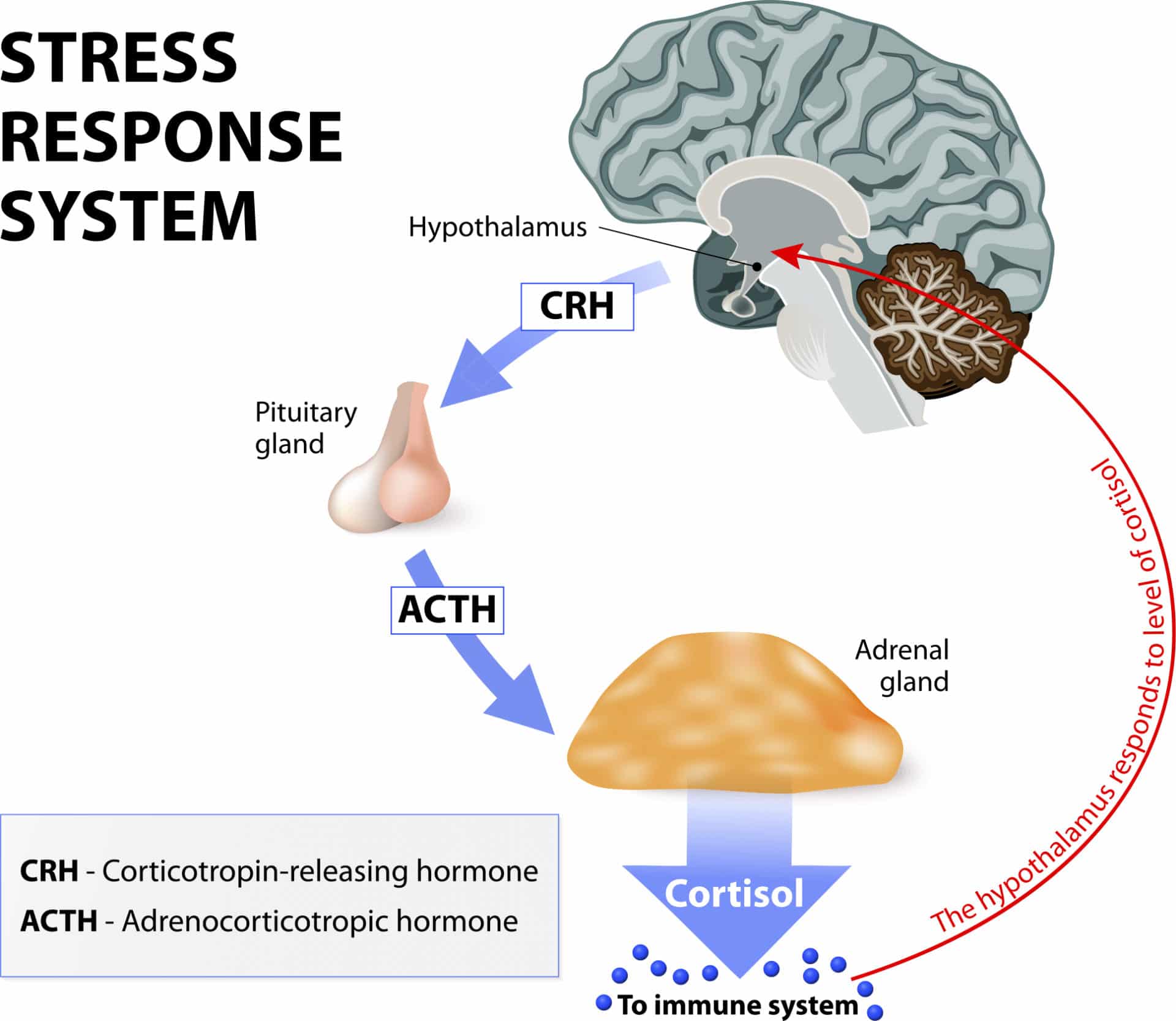
In a big game of physiological telephone, stress registers in the brain, where your hypothalamus signals the pituitary, which then signals the adrenals.
The adrenals release hormones into the blood stream that make their way to the brain. This is the negative feedback loop that lets the hypothalamus and pituitary know the message has been received and the job performed.
Depending on whether the brain is perceiving the level to be high enough to meet the demands of the stress, it will keep signaling the adrenals to produce more cortisol, or stop sending the hormonal signal so that the gland will know it has put out enough.
The stress response happens in 2 phases: First, we release catecholamines (adrenaline and noradrenaline) that prime your body to act immediately. Secondarily, these chemicals trigger a series of neurochemical processes that tell the adrenals, “It’s go time!”, meaning, please make some cortisol--NOW!
Cortisol’s main role here is to increase your heart rate and therefore blood flow to your arms and legs, for running. It also mobilizes glucose to fuel the action.
The flood of cortisol helps to increase your breathing rate, initiate sweating, dilate pupils. It also shuts down movement in your digestive tract, to make sure our muscles have enough fuel to run from the bear, remain alert and keep our bodies cool, among other things. The overall effect is to prioritize energy to the Central Nervous System, Cardiovascular, and musculo-skeletal systems, which are critical to survival in a life threatening situation.
The rest of the body’s systems, such as digestion and reproduction, which are more essential for long-term survival are temporarily reduced in activity.
Priming your body to go into fight-or-flight when under duress is just one of the many hats that Cortisol wears. Cortisol receptors are found on almost every cell in the body—that’s how critical it is to almost every aspect of our metabolism.
Modern Stress
Our bodies were designed to survive and even thrive in situations that are stressful in the short term. For most of our lives as a species, this might have looked like the situation above. It might have been caused by something equally stressful, like falling into a river and having to swim to shore. In situations like these, increased levels of cortisol and adrenaline produce the perfect physiological response to help save your life.
But in our modern industrialized world, we are exposed to a constant barrage of ongoing, sub-acute stress throughout the day. Fighting traffic, meeting work deadlines, parenting issues, relationship glitches, the mortgage, the bills, taxes, and an endless influx of text messages, phone calls, emails, and social media alerts, each add to our stress.
Then there are the stresses that don’t always feel immediately stressful, but that add to our overall stress levels in more subtle ways. These include: sitting all day, lack of exercise, overtraining without enough recovery time, skipping breakfast in favor of coffee, eating processed foods, staying up late to watch one more TV episode, or exposure to lots of artificial light after sunset.
When the stress state is prolonged, cortisol is maintained at higher than normal levels for extended periods of time. Excessive exposure to cortisol actually causes a catabolic metabolic—this causes body tissue breakdown, as opposed to growth and repair. High cortisol levels in the brain permanently burn-out nerve cells in our hippocampus, our center of emotion and memory. So, when stress is too intense, or goes on for too long, our brain down-regulates the production of cortisol, in a disrupted feedback loop.
This is why "Adrenal Fatigue" is more accurately described by the term "HPA-Axis Dysregulation" (Hypothalmus-Pituitary-Adrenal Axis). As the HPA-Axis dysregulation progresses, cortisol production often drops lower and lower, as does the production of other adrenal steroid hormones like DHEA.
Adrenal fatigue is actually a brain problem
When we talk about “adrenal fatigue” and “adrenal repair”, it can give the impression that something is wrong or damaged in the adrenal glands themselves. But issues stemming directly from the adrenal glands are truly only at hand in specific medically diagnosed disease states like Cushings or Addisons diseases.
A more accurate description of what adrenal fatigue really is, is the term HPA-Axis Dysfunction (hypothalamic-pituitary-adrenal dysfunction….say that 3 times fast!). This term describes the breakdown of the communication systems that these three glands use to talk to each other and regulate hormone production and rhythm every day.
The HPA Axis is our central stress response system. When your brain perceives that there is either something stressful or threatening in your environment (or if emotions run high), or if your blood glucose levels get low, or if you have high levels of inflammation, the hypothalamus shouts at the pituitary to do something about it. The pituitary in turn, signals the adrenal glands (by releasing a hormone called ACTH) to crank up the production line on cortisol, to help deal with the situation.
Normally, when the “stressor” is gone, the signaling quiets down, and cortisol levels should return to normal. But if the stress/inflammation/glucose problem is ongoing or severe, sometimes, the levels either stay high, or, alternately, shut down.
When you experience symptoms like fatigue, anxiety, insomnia, or foggy-brain due to imbalanced cortisol levels, it’s because of a breakdown in the signaling from the brain to your adrenal glands. In other words, the problem is in the software or programming, not in the hardware!
When we test with cutting-edge labs, and create treatment protocols, our aim is to reset the rhythm of the output of adrenal hormones. This process is dependent on restoring the feedback loops between the control centers in the brain.
After long term stress or inflammation, we adopt a new normal. Treatment to restore balance is a bit like restarting the computer and rebooting the software.
To learn more about how stress and adrenal hormone dysregulation can throw a wrench in your sex hormone balance (like estrogen, progesterone, and testosterone), continue on to Part 4.
Adrenal Fatigue Part 4: The “Cortisol Steal”—or, How Increased Stress Creates Female Hormone Imbalance
This is Part 4 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read Part one, Part two, and Part three.
Two days ago, I was getting my haircut, and I saw a picture of my hairdresser’s two adorable kids at her station. She told me she’d raised them herself, thankfully with some support from her mother and brother, and that her young daughter was quite a handful these days!
Then she shared with me that she felt like now that she had turned 43, her hormones were “making her crazy” all of a sudden—the other day, she’d snapped at 7 year old daughter about something that would never have been a big deal in the past. This type of short fuse was always worse right before her period was due, but lately, it seemed like her mood, energy, patience, and brain function shifted almost 2 whole weeks before hand! As she remembered it, her mother had gone through a horrible menopausal phase. In fact, she’d had a really tough relationship with her mother during that time because of it, and she was terrified that her menopause was going to turn her into a crazy person too!
I don’t know first-hand, but the stress of being a single parent, even with some close family nearby, just seems like it requires super-powers to withstand. It was no surprise to me that after years of stress, her reproductive hormones were taking a hit.
So how does stress impact our female reproductive hormones?
Our bodies make most of our adrenal hormones and some of our “reproductive hormones” like estrogen, progesterone, and testosterone from the same precursor horomone - pregnenolone.
Ordinarily, pregnenolone is transformed into a multitude of various hormones, in optimal ratios, every minute of every day. But the minute our body perceives it is under stress, it prioritizes cortisol production, at the expense of the other hormones.
This prioritization is elegantly designed. Progesterone, estrogen and testosterone are all hormones designed for the long-term reproductive survival of the species. Cortisol is about rescuing You, Now.
If your body receives a hormonal message that the external environment is threatening, or you’re in a famine and therefore in a fasted, hypoglycemic state, it’s probably not the best environment to bring a new baby into, right?
So, your body focuses its energy and resources on saving you, and diverts its “attention” away from making hormones that are specific to reproduction and other “non-essential” activities. This allows for the production of a huge amount of cortisol, but inhibits the production of virtually every other hormone. When the stress resolves, our brain stops sending the signal to increase cortisol production, and hormone levels return to normal…in theory.
Pregnenolone can convert down either of two main pathways:
- Conversion into progesterone, as a first step on the path to being converted into cortisol, and/or cortisone, our main anti-inflammatory hormone.
- It can be made into DHEA, which is the precursor to all of our sex-hormones.
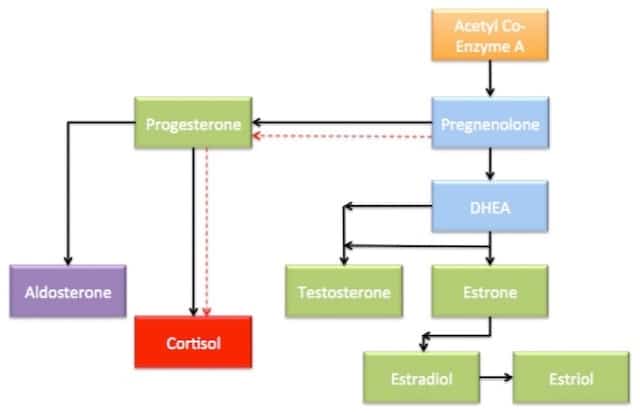
When under stress, the body will decrease DHEA production and prioritize the cortisol production. While the majority of our reproductive hormones are produced in the ovaries and testes, roughly 30-40{0ace9f30246476cbe34912402cc70dd667071e9efa13e47cc458477e17894418} is produced in the adrenals. This amount significantly impacts the maintenance of the overall stable hormone levels in circulation.
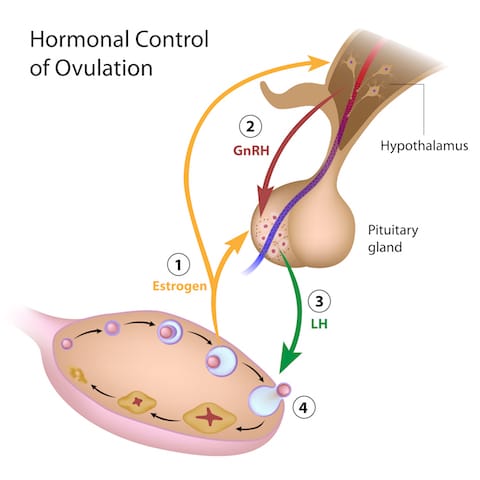
But there are other ways that stress impacts our monthly hormone cycles as well! The HPA axis is closely related to the HPO (Hypothalamic-Pituitary-Ovarian) axis. Just like these glands in the brain have feedback loops and signaling systems that tell the adrenals what to do when, we also have telephone lines between the hypothalamus, pituitary, and ovaries.
High cortisol levels block the HPA axis at each step in the chain. High cortisol stops the secretion of the hormone that our Hypothalamus send to the pituitary (GnRH) that tells it to make LH and FSH. LH and FSH are the hormones that the pituitary makes in order to signal the ovaries to make estrogen and progesterone. When these are suppressed, the ovaries don’t get the message. And, to make matters worse, elevated cortisol levels also interfere directly with ovarian hormone production, which is the bottom line.
This system is meant to protect you, and ultimately, to help your body know when the situation is safe for reproduction. But this brilliant system isn’t built to cope with today’s messy, stress filled world. We used to live in villages where everyone shared the responsibilities of life, food, shelter, and survival. For most of the humans on the planet, most of the time, everyday life was pretty ho-hum, and big stresses only occurred from time to time. Now we’ve each become our own village, wearing all of the hats every day, in industrialized countries. Our lifestyle of convenience and high-speed access to everything may not be so convenient after all.
Worsening PMS, stronger menstrual cramps, increasing hot flashes and night sweats, or periods that go AWOL are some of the red flags that Adrenal Fatigue and stress may be causing female hormonal imbalances!
Read on in Part Five, about the types of Stress (it's not just emotional stress!) that can disrupt adrenal hormones!
Adrenal Fatigue Part 5: When the Bear Isn't Really a Bear—What Causes Adrenal Function to Become Compromised?
This is Part 5 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read part one, part two, part three, and part four.
"Girl, I've had the craziest week!" How many phone calls with my best girlfriends start off something like that?
A lot.
Life happens; kids, husbands/wives, job related stuff, disagreements with other friends, and the stuff that pops up out of left field, like the water heater breaking down. These are the things we call "stressful" in conversation--but there are several other types of stress that our body will respond to in the same way hormonally, even though we don't feel stressed out at the time.
When The Bear Isn’t Really A Bear:
Cortisol increases neurological excitability and heightens sensory perception. This is great for a survival situation, but the same mechanism can cause anxiety, panic –and stress. Good if running from a hungry bear, not so much if you are sitting in a job interview.
Types Of Stress:
Stress is classified in three broad categories:
Emotional or Circumstantial – a few common examples are:
- Grief
- stressful relationships
- a rocky divorce or breakup
- caring for ailing family members
- toxic work environments
- Starting a new job or moving to a new place
- post-college graduations expectations
- starting a new business, while buying a house and having a kid, all in the span of a few years
- lack of regular movement, or excessive exercise & overtraining, (especially too much endurance cardio)
- Inadequate sleep depth or not enough hours
- overwork
- keeping late hours
- having a constant feeling of having too much on the "To Do" list and never quite keeping up
Obviously not all of these “stressors” are unpleasant or traumatic. Just being in “Go-mode” all the time is enough to dysregulate stress hormones!
Dietary:
- Skipping meals
- overeating sugar and processed carbs
- too much carb intake for your body in one sitting
- alcoholism/drug abuse
- restricting calories
- eating poor quality food with lack of nutrient density (like snack food, fast food, or frozen dinners)
Eating pastries at the coffee shop, or even bowl of oatmeal with raisins elevates your blood sugar. As a result, insulin rises to help the glucose get into cells to be used for fuel. But the residual insulin from the surge can easily drop your blood sugar levels too low, so you crash a few hours later.
Your adrenals then pump out cortisol to try to level out the glucose levels.
Going excessively long without eating also causes the body to secrete cortisol, due to stress, just as if the bear jumped out of the forest. Except we don’t register starvation as “stressful” mentally because the stress takes a different form. High sugar, high carb, and high grain diets, especially those low in fats and protein, act on our bodies in the same manner. Ever found yourself in an argument (about nothing important) with your spouse or friend, and had it occur to you that you were "hangry"? Blame it on cortisol!
Chronic Pain & Inflammation
Pain is obvious: migraine headaches, knee problems, bad backs, old unresolved injuries from sports or accidents, severe menstrual cramps every month are just a few common examples.
But people are rarely aware that they are inflamed.
Inflammation is anything that ends in “it is” - arthritis, colitis, gingivitis, etc.
Inflammation can also come on after an acute infection that is severe, such as influenza or pneumonia, appendicitis, etc. But the majority of inflammation is caused by one of 4 things:
- Chronic low grade Infections (such as parasites, yeast overgrowth, SIBO, mold/biotoxin illness, or chronic viral infections)
- Exposure to foods or chemicals that we are “sensitive” or “intolerant” to.
- The toxicity of heavy metals trapped in the body’s tissues after exposure
- Too much sugar or too much Omega 6 (from industrial oils) in the diet.
Emotional stress, dietary stress, pain/inflammatory stress. Think about this for a minute: We’ve all gotten in a fight, or had some really bad news, or lost a pet or someone we love, and felt the immediate impact of the stress and high emotions.
But our body responds in the same way to chronic pain (like migraines and unresolved injuries), or chronic low-grade inflammation from undiagnosed gut infections, food reactions, or chronic viral infections. We have the same hormonal/chemical response. We don’t feel it on a conscious emotional level, yet it impacts our body just as profoundly.
Read part Six to find out if cortisol imbalance is to blame for your blood sugar issues or weight gain.
Adrenal Fatigue Part 6: Is Cortisol to Blame For Your Blood Sugar Balance or Weight-Loss Resistance?
This is Part 6 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it!. Click here to read parts one, two, three, four, and five.
When Mary came to see me, she was extremely frustrated because, despite cooking most meals at home, and exercising most days of the week, she just couldn't’ seem to get rid of the 10 extra pounds that she was carrying, mostly around her hips and stomach.
“I get it,” I told her. Hey, I’m a woman too, and while my priority is to be healthy and to feel good, I’m not gonna lie, I want to stay fitting into my date-night jeans too!
In post number 3 in the series, I mentioned how one of cortisol’s main roles in Fight-or-flight is to keep higher levels of circulating glucose in the blood for fuel. It does this by inducing a process known as gluconeogenesis, where fatty acids and amino acids are converted into useable blood glucose in the liver.
Generally, when our blood glucose levels rise, our pancreas secretes insulin to move the glucose into cells for storage, so that it can be used later during periods of activity. Having elevated cortisol long term leads to consistently higher glucose levels, which leads to consistently elevated insulin levels, as the body attempts to get glucose out of the blood and into storage. The purpose of the stored carbs is to generate a source of rapid fuel for the body. This is required if you, say, need to run from a bear.
But what if the bear isn’t a bear, but is rush hour traffic that‘s making you late for an important presentation. Rather than running down the highway to burn off some of your excess adrenaline, you’re forced to sit there and feel anxious as the minutes tick by. Now you’re just sitting still, with high blood sugar levels circulating, and no good use for them.
After a while, your body recognizes that you’re not using the liberated glucose. Your body then pumps out higher levels of insulin, to transport the glucose into fat cells to be stored. When you have high insulin and high cortisol levels your body typically stores this energy in fat cells located around the midsection or belly. Overall weight gain, or weight loss resistance are also common. To add insult to injury, adipose tissue can actually generate it's own cortisol, jump-starting a vicious circle of chronically elevated cortisol that makes fat just impossible to budge.
Chronically high levels of insulin can also lead to a pre-diabetic condition called metabolic syndrome (or insulin resistance) and type 2 diabetes, which also leads to increased weight gain. Because of the relationship to blood sugar regulation, anyone with diabetes, pre-diabetes, whether overweight or thin, should have their adrenals tested and seek treatment if necessary.
Chronic stress also impacts appetite-regulating hormones like ghrelin and leptin, affecting our levels of hunger and satiation, as well as food preference.
If you’re struggling to lose weight, despite your best efforts, testing your cortisol levels may provide you with valuable insights into what’s getting in the way of your weight loss, and how to fix it!
Stay tuned for the final posts in the series, where I'll discuss different types of testing, and some simple-but-powerful steps you can take to start to heal adrenal fatigue on your own.
Recipe: The Best Waffles in the World! (Cassava Flour Waffles)
A large percentage of my patients have SIBO and are on Low Fodmap diets, are on a version of AIP (Autoimmune Paleo), or a paleo diet. So I’m always looking for safe starches to include to ensure proper carbohydrate intake and to act as food for their good gut bugs. Squashes, sweet potatoes, and root veggies make up a good amount of the carb sources in my diet as well as many of my clients.
But once in a while, I want something with that perfect amount of CRUNCH.
Something that you can slather with grass-fed butter when you need some comfort food from childhood....
Growing up, my house was a waffle house, at least on some weekends. Now, since we have (mostly) eliminated grains in our house, bread-like things happen less frequently, and waffles were unheard of.
But then I fell in love with Cassava.
Many of you know next to practicing Functional Medicine, my biggest passion is dancing, specifically dances of the African and afro-brazilian diaspora. On my last trip to Brazil, I realized how many things are made with cassava/tapioca, and also how absolutely delicious it is! Besides frying the chunked root, it is made into cakes, mashed, and (my personal favorite) miniature cheese-bread rolls called “pao de quiejo” (cheese bread).
Cassava (also known as yuca) is a starchy tuber, and is a staple for millions of people in South America, Asia, and parts of Africa. This plant can be processed into both tapioca starch as well as cassava flour (which maintains the fiber content), each of which have slightly different properties when it comes to using them in cooking and baking.
And, it can be used to make, hands down, the best waffles in the world.
I made these at a birthday breakfast for my extended family recently, and no one could believe they were grain-free. Even the pickiest eaters downed at least 2
Cassava is naturally gluten, grain, and nut-free, and is also low FODMAP. But somehow, it’s a pretty close replacement for wheat flour in terms of texture, and can be used as a replacement in most recipes 1:1.
One thing to note before going on a cassava binge: it is very high in carbohydrate per gram, compared to other roots like sweet potatoes or beets. This can lead to glucose/insulin spikes in those who are sensitive, or if you eat too much. If you’re on a low carb diet, or have diabetes or other blood-sugar issues, avoid cassava, or save it for the occasional treat.

The only brand I use is Ottos Naturals, as I’ve heard of other people having less-than-stellar results with other brands. There are tons of great recipes out there for tortillas, breads, naan and other treats out there in the inter-webs if you do a quick google search. But this waffle recipe takes the cake, IMHO! (Credit to Laura Franklin of Fresh & Frank)
Crispy Cassava Blender Waffles
Makes about 10 standard square waffles
Ingredients
1 cup Otto’s Cassava Flour
1/2 tsp Himalayan salt
2 tsp baking powder
1/2 tsp cinnamon
1 ripe banana
2 organic eggs
1-2 tsp real vanilla extract
2 Tbsp organic virgin unrefined coconut oil
1.5 cups coconut or almond milk
Directions
1. Preheat waffle iron.
2. Throw all ingreidnets into blender.
3. Blend all for about 30 seconds to 1 minute.
4. Check batter; if it seems too thick still, add a splash more almond/coconut milk or water. You want it thick but still able to pour.
5. Pour onto waffle iron. Depending on the integrity of your waffle iron, you may need to cook these twice to make sure the inside cooks through.
6. Remove when crispy and golden brown on the outside. (I know it’s hard to wait, but don’t remove too early!) Top with desired ingredients.
Waffles freeze well and can be thrown directly in the toaster to crisp up!
10 Common Signs & Symptoms of Polycystic Ovarian Syndrome
If you've ever struggled with infertility, irregular menstrual cycles, or other reproductive problems, please know that you're not alone. Thousands of women out there are striving for help and healing in the face of such frustrating health issues.
One relatively unknown yet common cause of reproductive health problems is a condition known as Polycystic OvarianSyndrome, or PCOS for short. PCOS is so common that it affects as many as 1 in 10 women of child-bearing age, although even girls as young as 11 can be affected. Considered a hormonal and metabolic imbalance, PCOS is the leading cause of infertility worldwide.
10 Top Signs & Symptoms of PCOS
By definition, PCOS is a syndrome, not a specific disease. This means there is no one test or procedure that can confirm a diagnosis. Instead, clinicians must rely on a thorough evaluation of each individual woman's signs, symptoms, lab markers, and patient history in order to determine if PCOS is the cause of her symptoms.
Effectively, PCOS is a diagnosis of exclusion. That is, a woman may receive a diagnosis only if and when other diseases that could explain her symptoms have been ruled out. As the most common hormonal disorder in women of reproductive age, PCOS impacts over 100 million women around the world, and has impacts on health that extend beyond the reproductive system to cardiovascular health, metabolic and immune health.
So, what are the indicators of this syndrome? Could you or someone you know be affected? Take a look at the following 10 signs and symptoms. They could suggest the presence of PCOS:
1. Irregular ovulation and/or menstrual cycles.
Women with PCOS may experience long or irregularly timed menstrual cycles, sporadic or missing ovulation (oligo-ovulation or anovulation, respectively) amenorrhea (absence of a period), or dysfunctional uterine bleeding (spotting). Additionally, a pelvic ultrasound may show increased thickening of the endometrial lining of the uterus. Ultrasound imaging can also show enlarged ovaries covered with a series of cyst-like formations which often resemble a "string of pearls."
2. Infertility.
This may be one of the most stressful and troubling symptoms for many women with PCOS who are otherwise trying or would like to become pregnant.
3. Hirsutism. (Excess hair growth)
This is a medical term that refers to male-patterned hair growth in women, including excessive hair on the upper lip, chin, chest, abdomen, and/or back—exactly where most women don’t want it.
4. Hair loss.
A bit of a double-edged sword, isn't it? In addition to excessive hair growth in unwanted places, PCOS can also cause thinning of hair on the scalp and in some cases male-pattern baldness. It’s just not fair.
5. Acne.
Breakouts can be moderate to severe, or newly developing in adulthood, when everyone else’s teenage-acne is ancient history.
6. Obesity and overweight.
Weight gain is common, as is the increased likelihood of related metabolic disturbances including pre-diabetes and diabetes. Interestingly, not every woman with PCOS will be overweight—in fact up to 50% of women affected by this syndrome may be normal weight or even underweight.
7. Darkening of skin.
This hyperpigmentation, called acanthosis nigricans, is usually the most obvious around the groin, underneath the breasts, and in the creases of the neck.
8. Skin tags.
These small flaps of excess skin typically grow around the axilla (armpits) and/or neck area.
9. Depression.
The distress caused by other symptoms can lead many women with PCOS to feel depressed, although depression or anxiety can be symptoms in and of themselves. Additionally, women with PCOS often experience a low or absent sex drive, and a lower stress tolerance.
10. Abnormal lab tests.
Blood work and other tests may indicate elevated levels of male hormones such as Testosterone (also known as androgens), and a ratio greater than 2:1 between two hormones known as the lutenizing hormone, or LH, and follicle stimulating hormone, FSH (a normal ratio is around 1:1). There are other lab markers that can further characterize PCOS, and I will discuss these in the next article in this series.
Recognize any of these symptoms in yourself or another woman in your life?
If so, be sure to consider requesting screening with labs and ultrasound. If you're looking for a holistic, effective, and individually-tailored approach, I invite you to consult with myself (PCOS whisperer) and the rest of my integrative team. We're here to help you heal, and it's my honor to join you on your journey toward better reproductive health.
To learn more about the role of Functional Medicine in the treatment and management of PCOS, schedule your initial consultation or a FREE 15-minute Consultation today.
Recipe: Grandma Fleischer’s Chopped Liver
Liver.
You either love it or you hate it. Or you're too scared to find out.
If you ask someone who grew up in a family where you regularly ate liver, or other organ meats, they'll inevitably grin with deliciousness. But for those of us who didn't dish up liver and onions regularly, the idea can be a bit foreign.
Given the opportunity, most little kids that get introduced at an early age actually LOVE liver.
Personally, I grew up on the east coast, near lots of kosher delis, and ate my fair share of chopped liver. I remember being held in my grandfather's arms, at the fridge, eating it on a spoon out of a deli container and begging for more. Somewhere in my later childhood years, it stopped being something we had around, and by the time I was 23, (after a 15 year stint as a vegetarian), you couldn't pay me to touch the stuff.
A few years ago, with the bone-broth-slurping, organ-meat-eating trends that came with the advent of the Paleo movement, I started really looking at nutritional content of organ meats. Bite for bite, liver holds it's own against virtually anything you can call food, when it comes to nutrient content. Liver is particularly high in Vitamins A, C, Biotin, Folate, and B12, as compared to other foods that are considered to be good sources of these nutrients. In Chinese medical nutrition, liver has been touted for centuries as the best "blood builder" and fertility food-- and indeed, with high levels of iron, folate and b12, it's a sure fire way to help alleviate anemia.
Armed with this knowledge, I was determined to re-learn to eat liver.
If my 3-year-old self could do it, so could my 38-year old self!
Now I learn a lot from my patients. And on my mission to love liver, it was one of my long time patients, Adam, who came to my rescue. After a discussion about this in my office, about once a month or so, Adam brings me a little glass jar with his grandma's chopped liver, and some celery sticks or Mary's Crackers.
And as I sit and munch, it's like I'm 4 all over again....
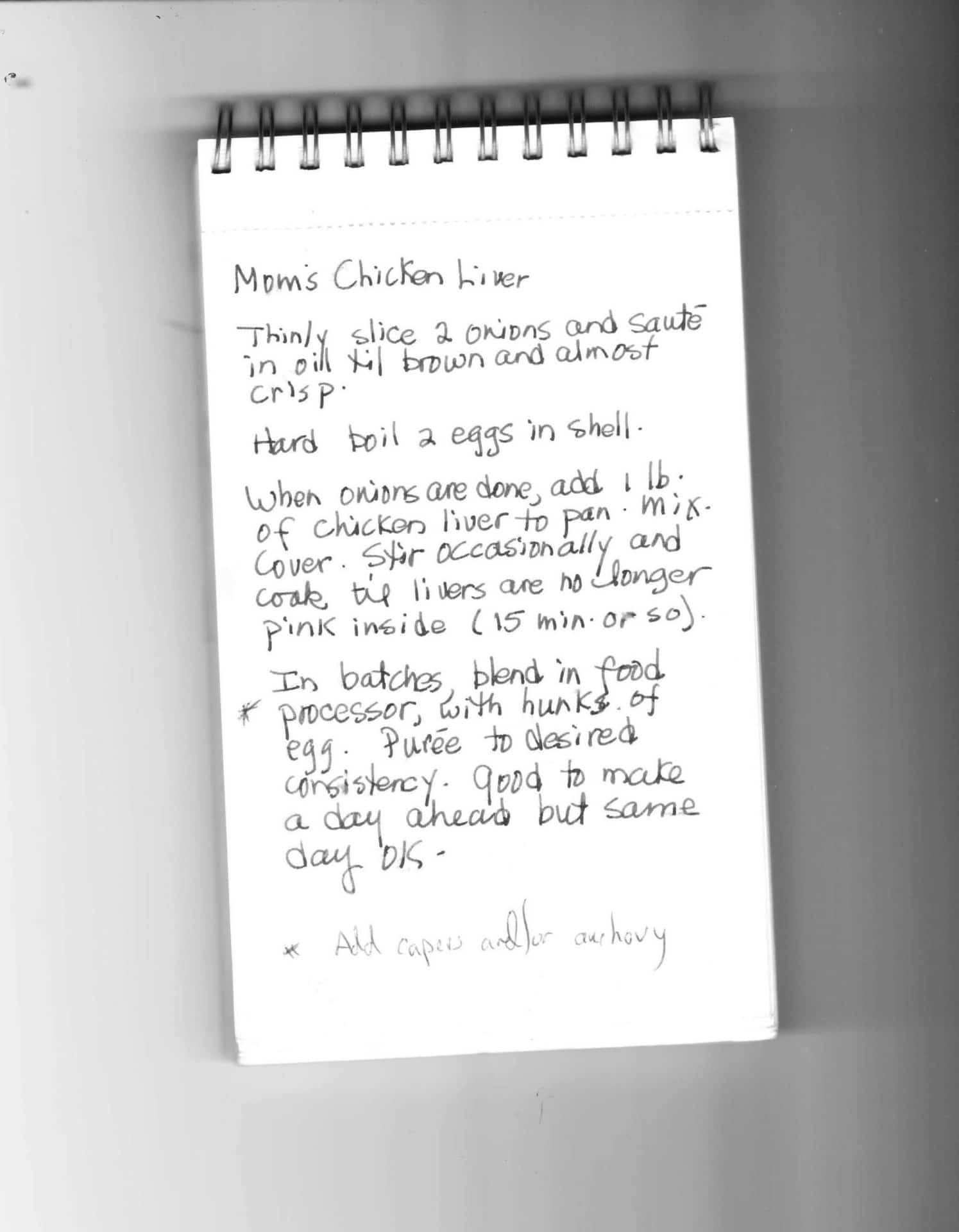
Grandma Fleischer’s Chopped Liver
(With huge gratitude to Adam F)
Ingredients
1 Lb Pasture Raised/Organic Chicken Livers
2 Yellow Onions
2 Eggs, hard boiled
Salt
Pepper
Optional: 2-4 slices of Bacon, Anchovies and/or Capers
- Thinly slice 2 onions and sautée in oil until caramelized brown and almost crisp. Be sure to salt and pepper liberally as you sautée. You can use avocado oil or grass-fed butter for sautéeing, or you can start with 2-4 chopped up pieces of bacon in the pan, and then use that fat to sautée the onions. Cooking time for the onions is 10-20-mins.
- When the onions are done, add 1 LB of chicken livers to the pan, salt and pepper again. Cook 8-12 minutes, on medium (not high) heat, turning or stirring every few minutes (but not too much stirring).
- Very important! DO NOT OVERCOOK THE LIVER--The livers should still have a little pink in the centers when done.
- In batches, remove livers and onions from the pan and transfer to a food processor with chunks of the hard boiled egg. Puree until it reaches the desired consistency. For an added kick, toss in a handful or two of capers and/or some small anchovy fillets. It just takes a few pulses in the food processor, don’t overdo it.
Serve with celery sticks, crackers, or other veggies and enjoy. This is best prepared a day in advance and then served the next day, but is still delicious when made the day of!
Top 3 Uses for This Amazing Probiotic Yeast
In the world of natural health, yeasts get a bad rap. But one of my favorite probiotics, Saccharomyces boulardii, is actually a beneficial medicinal yeast!
Commonly referred to as S. Boulardii, it was originally found on lychee fruit in the 1920s. When taken as an oral supplement, it colonizes the gut within three days. But the colonization is temporary—S. Boulardii disappears from stool within five days of discontinuing supplementation. Interestingly, the health benefits that it provides last beyond the time of oral consumption—which means that, like most other probiotic supplements—the benefits are not due to the probiotic strains taking root and colonizing.
Used for prevention and treatment of diarrhea
Many types of diarrhea are caused by dysbiosis (bad organisms living in the gut). When this occurs, the healthy microbial population takes a significant nose dive--especially important species like Bacteriodies, Ruminococus and Prevotella.
At the same time, the gap formed by the notable decrease in these beneficial bacteria, creates a void-like vulnerability that allows for increases in opportunistic bacteria like Enterobacter and less desirable Clostridia strains—these are aptly referred to as “pioneer bacteria” because they migrate to an area when there is an opportunity!
In this situation, Saccharomyces Boulardii has been shown to help in several ways:
- S Boulardii actually helps to bind pathogenic bacteria and carry them out of the digestive tract, especially Staphylococcus aureus, Klebsiella, Candida, and Salmonella
- Several human studies have demonstrated that S boulardii supplementation leads to faster re-establishment of a healthy microbiome, when recovering from infectious diarrhea.
- It increases the population of specific types of bacteria that are known to produce short chain fatty acids (SCFAs) by fermenting dietary fibers (prebiotics) and resistant starch. SCFAs are the energy substrate of cells in the gut lining that allow it to constantly heal and regenerate, preventing Leaky Gut. They also directly support some of the commensal (or good) bacteria as well.
S Boulardii is most notably useful in infectious Clostridium difficile infection. Clostridium Difficile (also called “C Diff”) is the primary cause of acute diarrhea after antibiotics, and it not an infection to take lightly. In extreme cases, it can even be life threatening. When 124 patients on high dose vancomycin (an antibiotic) for C. difficile related colitis were given S. boulardii, rates of recurrence plummeted from 50% to 16.7%.
But bacteria are not the only micro-organisms that can cause diarrhea. Overgrowth of yeasts like Candida Albicans can also induce diarrhea by causing inflammation of the gut lining. S boulardii has been shown to decrease tissue inflammation in the gut caused by colitis from Candida overgrowth, alleviating diarrhea from this cause.
Disrupts candida colonization in vaginal and other tissues
Candida albicans is the most common opportunistic fungal pathogen found in the human body. It has many tools at its disposal that allow it to thrive and take root; the ability to adhere to tissues and even penetrate them, biofilm formation and the ability to transformation into different forms at various stages of its life cycle.
In order to get an overgrowth in the first place, adherence is the first necessary step. Candida albicans is capable of adhering to the inside of cheeks, labia, vaginal and intestinal epithelial cells, as well as catheters, dental implants or artificial joints.
Not only has it been shown to interrupt Candida’s adherence, but S. boulardii is uniquely able to stimulate Secretory IgA (SIgA), our first line of defense against invading microbes. SIgA is essential to maintaining intestinal mucosal integrity, preventing leaky gut, and ensuring a stable, diverse microbiome—which is key to bulletproofing your gut. This is the main immune agent found in mucous membranes, saliva, tears and vaginal secretions, as its main function is to help protect you against pathogens.
Prevention
Perhaps the best use of S Boulardii is prophylactically.
With Antibiotic use: Since it yeast are not killed by antibiotics (only bacteria are susceptible to antibiotic drugs) you can (and should) take S boulardii during antibiotic therapy to prevent Candida overgrowth and other diarrhea-inducing opportunistic pathogens. Several studies have demonstrated that in patients with known H. pylori infection, S Boulardii supplementation improved eradication rates and reduced treatment-related side effects.
You can also take it before, during, and after travelling—it helps prevent traveler’s diarrhea! Meta-analysis of probiotics used preventatively for travelers diarrhea all showed significant reduction in the risk of traveler’s diarrhea when probiotics are used—but two randomized control trials showed a significant reduction in traveler’s diarrhea in the S. boulardii group compared with other types of probiotics used as controls.
For this particular purpose, I suggest 1000 mg daily. Should you get sick while travelling, you can continue to take it during traveler’s diarrhea, or ongoing diarrhea, to shorten the duration and promote recovery.
A word of caution
S Boulardii has been shown in studies to be helpful helping improve symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome. For example, in a 6-month study of patients with Chrons Disease, the relapse rate was significantly lower in patients treated with mesalazine plus S. boulardii (6%) than in those treated with mesalazine alone (38%).
That said, in my clinical experience, people with Inflammatory bowel disease should proceed with caution, when initially introducing S boulardii. The reason for this Anti-Saccharomyces cerevisiae antibodies (ASCA) have been associated with Crohn's disease (CD). Saccharomyces Cervisiae (Brewer’s/Bakers yeast)—used in baking as well as in brewing beer and wine—is similar enough to Saccharomyces Boulardii that the immune systems of sensitive individuals can cross react, potentially triggering a symptom flare. If any flare in symptoms is noted with oral consumption, discontinue use. Like other probiotics, S boulardii is also not appropriate in severely immunocompromised individuals.
To buy Saccharomyces Boulardii, click here!
Have you ever used this probiotic yeast for your gut health? What was your experience?
11 Ways to Minimize Toxic Estrogen Exposure
It’s a fact of modern life that environmental estrogens are everywhere these days.
These estrogenic chemicals (estrogen mimickers) are endocrine disruptors (they disrupt hormone signaling) and can also mimic estrogen in their structure. Toxic estrogens can take the place of your healthy estrogens in your estrogen receptor sites, yielding an overall more powerful net estrogenic effect in your body. We love healthy estrogen levels, but more of a good thing isn’t always better!
This phenomenon is one of the biggest factors impacting our hormonal health, increasing rates of health concerns like infertility, breast cancer, and PCOS (Polycystic Ovarian Syndrome). Even without causing a namable syndrome or disease, xenoestrogen exposure can still promote estrogen dominance, a common condition where the levels of estrogen in the body outweighs the relative amount of progesterone available to balance it. Estrogen dominance commonly shows up in your body as things like PMS, breast swelling and tenderness, heavy menstrual bleeding, fibroids and cysts, or weight gain around the hips and thighs.
Xenoestrogens can be found in shampoo, conditioners, lotions, air fresheners, household and industrial cleaning agents, and even in your food!
Here is how to reduce estrogen exposure and estrogen mimickers:
1 Filter your drinking water
Trace amounts of estrogens from Oral Contraceptive Pills have been found in city water supplies, but over 90% of the estrogen found in drinking water actually comes from run off from animal manure. These make it to your tap, so unless you filter your water, you may be drinking a dose of estrogen daily. Bottled water isn’t any better, especially if it’s in BPA containing plastic. In other hormonal news, chemicals like Organochloride and Fungicide in water have also been shown to cause hypothyroidism.
2 Limit processed foods
As though we needed one more reason to ditch processed foods, estrogen-laden BPA is a common ingredient in found in the lining of packages which can soak into the foods stored inside of them. BPA is found in the linings of cans (including canned beverages), plastic windows on food boxes, hot beverage lids, and others types of food packaging.
3 Limit dairy and choose wisely
All dairy contains hormones, naturally—think about it, this is breast milk used to feed baby cows, so just like post-partum human breast milk, it is naturally chock full of hormones. If you tolerate dairy, choose organic since this ensures that no hormones or antibiotics were used to treat the cows. Choose grass-fed for an extra nutritional bonus.
4 Use glass, stainless steel, or silicone food storage containers and drinking vessels
Plastic food containers may contain bisphenol A. Never heat plastic containers or wraps in the microwave; heating plastic causes estrogens to leach into your food. But so does freezing food in plastic, so avoid that also.
5 Choose organic when possible
Fruits and veggies grown with pesticides are literally sprayed with estrogen. If you can’t buy all organic, prioritize organic for the foods found on the “Dirty Dozen” list.
6 Minimize soy products
A few of the proven health risks that soy-researcher Kaayla Daniel mentions in her extensive book on the subject, The Whole Soy Story are:
- Soy formula contains as much estrogen as 4 birth control pills, which can vastly alter hormone balance in babies and can predispose them to cancer later in life.
- Soy consumption has been linked to infertility, breast cancer, kidney stones, and immune system impairment.
- Soy isoflavones can lower thyroid function.
7 Eat brassicas and flax seed every day
Flax seeds contains powerful little plant chemicals called lignans that are actually phytoestrogens (plant-based estrogens). Phytoestrogens have a weaker overall effect than the estrogens that we produce in our body, so they can be used to help block excess estrogen from estrogen receptors in women with estrogen dominance. In women with low estrogen, flax can help boost levels. Flax also has anti-cancer properties and supports digestive and cardiovascular health. Broccoli, bok choy, Brussel sprouts, cabbage, cauliflower and collard greens are all Brassica family vegetables. Brassicas contain a natural compound called IC3 that is a potent antioxidant and helps clear excess estrogen from the body.
8 Avoid using chemical pesticides and fertilizers
In studies, Women who used pesticides experienced 60-99% increased odds of longer menstrual cycles, missed periods, and mid-cycle bleeding compared with women who never used pesticides. Using non-toxic products for household cleaning is similarly important.
9 Ditch your nonstick pans
The perfluorooctanoic acid (PFOA) used to make products grease- and waterproof is an environmental estrogen. When the cookware is heated, PFOA can seep into your food. Nonstick pans also release chemicals that block thyroid hormone receptors.
10 Avoid phthalates in your cosmetics and body-care products
Phthalates disrupt both estrogen and testosterone receptors. These are mainly used in fragrances, and the FDA doesn’t require them to be labelled on personal care products. Using fragrance-free and organic products helps to limit exposure. While these are still allowed to be sold in the US, the EU has banned their use proactively since 2004.
11 Avoid hand sanitizers and handling receipts.
Both contain BPA that can absorb through your skin. Hand sanitizer contains alcohol which helps the BPA to absorb in greater rates.
Are you concerned that you have symptoms of Estrogen Dominance and estrogen mimickers or looking for information on how to reduce estrogen? Let's talk about it!











