All About Food Sensitivities - New Cutting Edge Test Available! (KMBO FIT Test)
One of the primary tenants of Functional Medicine is to identify triggers for inflammation and reduce exposure. Sometimes, this looks like parasites or yeast overgrowth, sometimes it looks like an imbalance in amounts of Omega 6 to Omega 3 in the diet. And other times, this has to do with otherwise healthy, everyday foods that we eat, that simply aren’t a good fit for us at the time.
In theory, this should be simple. But historically, identifying food sensitivities accurately has been a challenge. Hundreds of tests exist for evaluating your immune systems reactions to food. But it has been shown time and time again that many of these tests are inaccurate, either under diagnosing, or over-reporting sensitive foods.
This makes it really difficult to know what to eat and what to leave behind. When a client’s test comes back with 30 reactive foods, it just leads to overwhelm for both the patient and the practitioner.
If your immune system is our planet, then your gut is like the water. Everything that you feed or put into the water is going to circulate, universally, affecting everything else on that planet. The air, the soil, the vitality of anything that grows. Knowing the foods that trigger decay and disease on your planet is essential to the overall health and vibrancy of your body.
You have far greater quantities of gut immune molecules, than you do in the entire rest of your body. Your gut immunity “scans” more in one day than is scanned by the systemic immune system in a lifetime!! Gut issues are so important to overall health, for this reason.
The truth is that food sensitivities are an underlying problem for every condition that I see.
And I mean everything:
- Arthritis
- Weight Gain
- Insulin Resistance
- Eczema, acne, and other skin conditions
- Fatigue
- Reproductive Hormone imbalance (PMS, PCOS, Menopausal symptoms)
- Infertility or recurrent miscarriage
- Autoimmunity of any kind
- Thyroid imbalances
- Adrenal issues
- Migraines
- Digestive issues ranging from IBS to Chrons or Ulcerative Colitis
- Depression, anxiety, insomnia, and brain fog
- and even addiction
Basically, any health concern where having increased inflammation would worsen symptoms or the disease process, can be worsened by exposure to foods that trigger your immune system. And inflammation is the bottom line in the vast majority of illness!
Even without illness or symptoms, anyone looking to live a long healthy life should run this panel, to prevent the development health issues later! I’m so excited to announce that it’s never been an easier or more reliable process to learn which foods are triggers for YOU! The FIT (Food Inflammation Test) by KMBO Diagnostics is cutting-edge lab testing that provides anyone who wants to rid their body of inflammation the information they need to avoid the foods that cause it! (***cut here for email, “read more”)
So, if it’s not an “allergy” what exactly is Food Intolerance or Sensitivity?
Hold up—let’s break this down a bit.
A whopping 85-90{0ace9f30246476cbe34912402cc70dd667071e9efa13e47cc458477e17894418} of our total immunity resides in the gut. There are several potential ways that you can have an immune reaction to a food. When we talk about Food “Allergy” and Food “Intolerances” or “Sensitivities”, these are very different things.
Our immune system is our bodyguard, working to protect us from “invaders” (like viruses and bacteria) that can cause us harm, 24/7. It works by tagging identifying proteins on the surface of the “invader” to mark it as a “bad guy” that should be attacked and eliminated.
Most of the time, this helps us. However, our immune system can also tag pollens, mold, toxins or chemicals, and other things we are exposed to. In the case of food allergies and sensitivities, a specific type of immune compound overreacts to the presence of a protein marker on the surface of a food molecule. The type of reaction is determined ultimately by type of immune compound that is doing the attacking in each reaction.
In a true food allergy, an immune compound called Immunoglobulin E (IgE) over-reacts to a certain food and causes a reaction within minutes or seconds. You can think of immunoglobulins like soldiers enlisted in our own personal immune army. Substances like egg, corn, or apples are normally harmless or healthy, but if you have an allergy, your body sees the food as a threatening invader!
In mild reactions, we might get histamine-driven symptoms like sneezing, runny nose, or itching, like with seasonal allergies. In a more aggressive reaction, you can develop hives, swelling, and even go into anaphylactic shock, which can be life threatening.
IgG is another type of immunoglobulin. IgG is produced by cells in the gut, in response to protein markers on substances like foods and bacteria. While IgE causes reactions within minutes, IgG causes reactions in 2 hours to 4 days or more!
Unlike true food allergy (IgE), IgG reactions are responsible for most of the symptoms that we associate with being “intolerant” or “sensitive” to a food. While the symptoms from an IgG response typically won’t include risk of death, they can still be uncomfortable and dangerous. For this reason, food intolerances are often dismissed as less significant, but in truth they can have serious consequences, especially with regard to your long-term health!
Food Sensitivity, leaky gut, and symptoms outside of the gut:
Logically, food intolerances can cause digestive symptoms. But how do these reactions cause symptoms all over the body like headaches or acne? If you have some degree of Leaky Gut, your immune system can react to the given food protein, forming immune-antigen complexes. When food proteins get through the gut lining, (through structures known as “tight junctions” in the intestinal wall), the resulting inflammation and immune activation causes further break down of the gut barrier. This in turn causes more leaky gut, and allows more food proteins in, creating a vicious cycle or increasing gut permeability and worsening food intolerances.
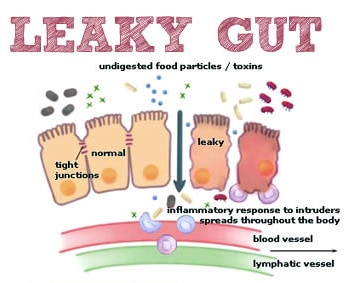
The over-activated immune system attacks local sites in the gut, but can also circulate in your bloodstream to tissues in distant locations around the body, such as joints, skin, your thyroid, or neurological tissue. Virtually any tissue in the body can be effected.
IgG-mediated symptoms can show up from 4 hours to 4 days after exposure to the reactive food. Clearly, this makes it difficult to identify what food caused what symptom!
Enter the FIT test!
The KBMO Fit Test is a revolution in food sensitivity testing. Like its ancestors, it still tests for IgG reactions to 132 different foods.

So, what’s so different and great about this test?
The main advantage that the FIT test offers, is that it screens for IgG types 1-4 (most IgG testing only looks at 1-2 types), and more importantly, screens for something called “complement”. When it comes to generating inflammation, complement is even more important than the level of IgG response to a food.
Let’s say that the initial IgG reaction is like the fire alarm going off at the fire station, and the first responders showing up at the scene. Compliment is like the rest of the squad showing up to help handle the situation…..they show up a bit later, but often create much larger hubbub at the scene of the accident or fire. The alarm (IgG) had to sound in the first place, to trigger the chain of events, but the responding teams (complement) were really what caused the biggest stir in the end. Foods that activate compliment can cause both local and systemic destruction of tissue by increasing inflammation.
In other words, you might have 10 or more foods with a significant IgG reaction, but the ones with complement are the ones that are significant in terms of boosting your inflammatory response. Knowing this information confirms which foods are most important to eliminate, instead of having a list of 40 foods to avoid! No other food sensitivity test currently available screens for IgG 1-4 and complement levels.
But there’s more…how the FIT Test can confirm if you have leaky gut
The FIT test is also a test for leaky gut, so you don’t need second test! If you show up as having a positive Candida antibody, it doesn’t mean that you have candida overgrowth. Candida is present in everyone’s gut, in low levels. A positive reaction to candida means that it is getting through the gut barrier, where it can present to your immune system. This confirms the presence of a leaky gut. The higher the reaction level, generally the worse the leaky gut. Having a high number of food reactions show positive (20 or more) also suggests leaky gut.
The best part is that this test is a blood spot panel. This means that we can mail it to you to do in the comfort of your own home– no blood draw needed! Based on your results, we design a 6-12 week elimination of your trigger foods, and then a systematic reintroduction to check for reactions. In most cases, antibody production in response to a given food will decrease or be eliminated within that time. When that happens, you may be able to reintroduce the food again without symptoms.
8 Reasons Your SIBO Isn't Clearing
If you’re like most people, you probably felt a mixed sense of frustration and relief when you found out that you have Small Intestinal Bacterial Overgrowth (SIBO). Relief, because all of your symptoms finally made sense. Frustration, because you’d heard how difficult treating SIBO could be; diet changes, herbs, antibiotics, pro-kinetics. It’s a lot to learn about, let alone put into action!
You ran a breath test. You changed to a low FODMAP diet. You found a practitioner and took a protocol of herbs or supplements. All of this felt empowering, and, at first, your symptoms started to get noticeably better. In fact they may have even resolved for the first time in years! But, then things changed and those old familiar symptoms started to return….
When things don’t go as planned…
What is even more frustrating than finding out that you have SIBO, is when you complete the protocol…..and the bloating, discomfort, diarrhea, or constipation, come right back, despite your best efforts. It’s just not fair, right?
What is even more frustrating than finding out that you have SIBO, is when you complete the protocol…..and the bloating, discomfort, diarrhea, or constipation, come right back, despite your best efforts. It’s just not fair, right?
I’m doing everything right….so why won’t my SIBO go away?
There are a few main reasons why people repeatedly fail to resolve their SIBO, despite using appropriate treatment strategies:
-
Using the wrong cocktail of herbs and supplements
A quick Google search will produce dozens of herbs that have been used to treat SIBO. But knowing which herbs or supplements to use for which type of SIBO (methane or hydrogen dominant, or mixed), or what dosage is necessary, is not always obvious.
-
Not treating for long enough
Duration of treatment should be based on several factors. Most important is what levels of hydrogen and methane gasses were found on your lactulose breath test, prior to the 120-minute mark. Many practitioners will recommend a standard treatment length of 2-4 weeks. While this is adequate for some cases, more progressed cases may require 8-12 weeks of continuous treatment with antimicrobials.
-
Not including probiotics during treatment
Many people hesitate to include probiotics during treatment, thinking that they might make SIBO worse. This is especially understandable if you took a certain probiotic formula and immediately felt symptomatic. Yes, some strains (especially d-lactate forming ones like acidophilus), can aggravate pre-existing SIBO. But some strains of antibiotics are shown to be more effective at treating SIBO than prescription antibiotics! Stick to soil based organisms, spore based probiotics, or Bifidus strains to be safe.
-
Not considering prescription antibiotics
I get it. I’m a trained herbalist first, always. And that means that I am just as reluctant for you to use prescription drugs as you are. However, we learn in pharmacology training in medical school that everything is a toxin, taken in the right dose. That’s right; even water can be toxic if you drink too much of it. Every medical practitioner eventually thinks about something called the cost to benefit ratio– “does the benefit given by this treatment, in this situation, outweigh the risk of using (or not using) it?”. In the case of antibiotics used for SIBO–specifically Rifaxamin– the benefit almost always outweighs the cost.
Rifaxamin is an antibiotic with several unique properties. It is not absorbed into systemic circulation– meaning that it stays in the gut. You can’t, for example, use Rifaxamin, to treat an ear infection, because it would never get to the inner ear. Rifaxamin is largely inactive by the time it makes it through the small intestine and into the colon. This means that it doesn’t upset the beneficial flora in the large intestine, leaving our good bacteria intact.
In other words, Rifaxamin isn’t associated with many of the negative actions that are associated with antibiotics in general. It is only used for one thing, and it does that thing very well. Dr Mark Pimentel, associate professor of medicine at Cedars-Sinai Medical Center, and a leading researcher in the area of IBS and SIBO diagnosis and treatment, says that he sees Rifaxamin be effective in at least 70% of patients SIBO.
While it’s certainly not a magic bullet, it’s worth a second look, if you’ve written it off as a potential treatment option!
-
Underlying structural abnormalities
While this isn’t the most common reason, it does exist, and won’t show up on breath testing. Changes in the intestine (like strictures, a blind-loop resulting from a GI tract surgery, problems with the ileocecal valve, or other structural issues) provide an ideal environment for bacterial colonization and overgrowth. These cannot be detected by physical examination or on a breath test, and can only be seen on imaging studies like x-rays and MRIs.
-
Co-infections
“Hey, who invited that guy to the party?” Some people with SIBO either haven’t had their stool tested for parasites, or, have used panels that weren’t good enough to catch them. If you have one or more parasites living in your gut, you will generally not get a full response to your SIBO treatments until you have properly diagnosed and treated the parasitic infections.
Another common scenario is having a mixed pattern of candida or other fungal overgrowth alongside of SIBO. Some SIBO may in fact really be “SIFO”– small intestine fungal overgrowth. Although there is some overlap, fungal/yeast overgrowth tends to respond to different herbs and supplements than are used to treat bacterial overgrowth. Sometimes, people need to adjust the treatment approach to target both bacteria and yeast, in order to get full results.
-
The wrong diet at the wrong time
Eating low FODMAP can be a helpful way to manage symptoms. But eating low FODMAP, or too low-carb whiletreating with anti-microbial agents can actually be counter-productive!
Studies show that using Rifaxamin plus Partially Hydrolyzed Guar Gum (PHGG) is more effective at clearing SIBO than Rifaxamin used alone. PHGG is a pre-biotic, which means that it feeds bacteria. So you would think that it would worsen SIBO by feeding the bacteria in the small intestine. In fact, it does exactly this, except that feeding the bacteria while using an agent that targets them while they are reproducing, yields exactly the opposite effect– it kills them off in higher numbers.
In this way, prebiotics make the treatment work better. Feeding the bacteria (either with a prebiotic like PHGG, or with FODMAP foods, as tolerated) is generally a good idea while taking herbs or prescriptions to treat SIBO.
Cops & Robbers: Clearing SIBO isn’t all about “killing the bad guys”
Reason number 8 is its whole own section, because it is probably the most significant driving cause in your stubborn or recurrent SIBO. Many people, in fact many practitioners, are treating SIBO as if it’s a parasite. If your SIBO treatment only consists of using things to “kill the bad guys”, you’re missing the boat.
To see why this is true, we have to recognize that SIBO isn’t an infection that we “pick up” from somewhere out in the world, but rather a situation that arises because the terrain of the gut has changed so that it is now hospitable to bacteria. While we are supposed to house trillions of bacteria in the large intestine, the small intestine is supposed to be relatively sterile. There are several aspects of the “terrain” that need to be considered.
-
Digestive secretions
Pancreatic enzyme insufficiency, or inadequate stomach acid or bile production all set the stage for less-digested proteins, carbohydrates, and fats. This means less nutrition for you, but also means more fermentable matter for the bacteria causing the problem!
-
Motility and the MMC
People with SIBO have altered digestive motility. This can be either a cause or an effect of SIBO, depending on the individual case. Although most people with SIBO will have symptoms of diarrhea or constipation, the kind of motility that is most important when it comes to getting rid of SIBO, and keeping it gone, is the Migrating Motor Complex. The migrating motor complex is responsible for cleaning the small intestine, specifically between meals. It functions like house keeping, in order to sweep bacteria, and undigested carbohydrates and fibers that might feed bacteria, out of the small intestine and into the colon.
Re-establishing proper motility and MMC activity is critical to your recovery from SIBO, as well as for future prevention. There are many ways to encourage proper patterning of gut motility. Using prokinetic herbs or drugs is standard, but many therapies (like abdominal massage, acupuncture, and neurological chiropractic) can enhance the benefits.
The vagus nerve is the main player here, and we know that vagal tone can be disrupted by trauma and ongoing stress. While physiologic approaches (like probiotics, prokinetics, abdominal massage, acupuncture, gargling, or chanting) are helpful, sometimes it is more important to find ways to gently face into the underlying mind-body issue. Therapy, hypnosis, and MBSR can prove to be indispensable in these situations. Often times the experience of having SIBO can facilitate an opportunity for deeper exploration of what is living in our hearts, minds, and spirit that is unresolved.
-
Dysregulated cortisol levels and the Immune system
One of the main reasons SIBO can arise is if your digestive immunity is compromised. Around 86% of your total body immunity is located in the GI tract.
Anything that suppresses or alters this immune activity can leave you more vulnerable to fostering bacterial growth where it shouldn’t be–in your small intestine!
Adrenal fatigue (HPA-axis dysregulation) leads to imbalanced stress-hormone levels (cortisol). And having cortisol levels that are chronically either too high or too low can lead to reduced levels of immune secretions in the gut. They can also slow down repair of the tissues that make up our stomach and intestinal lining, leading to leaky gut.
You need to test, to know.
-
Sympathetic Dominance
If you are constantly in “fight-or-flight” (also known as sympathetic dominance), your gut is at a disadvantage. Chronic stress overstimulates the sympathetic branch of our nervous system (like the gas pedal), and suppresses the parasympathetic branch (like the breaks). We need both, in balance.
Sympathetic dominance is known to slow motility; digesting the nutrients you’ll need tomorrow simply isn’t a priority if you’re running to save your butt, NOW!, if you’re running from a wild boar. It also shuts down digestive secretions, and suppresses immune activity, while up-regulating inflammatory compounds. Not a good look.
Digestive-focused hypnosis, Heart-rate Variability training, and meditation techniques such as Mindfullness Based Stress Reduction are a great way to give input to the nervous system and retrain it to kick off it’s shoes and relax a little.
The factors leading to your SIBO were really the perfect storm. Addressing these issues can make or break the success of your treatment. To learn more about how to get rid of SIBO, please schedule an appointment, or, contact my office to set up a FREE 15-minute consultation.
I Had To Take Antibiotics...How Can I Protect My Gut?
Many of my patients are surprised to hear that I, too, grew up with the ubiquitous bottle of pink bubblegum flavored prescription syrup in the fridge each winter. Amoxicillin—it’s the go-to antibiotic of choice for everything from ear infections to strep throat or pneumonia in children everywhere. Trust me; I had my fair share! Back when I was growing up, we just didn’t understand the ramifications of repeat antibiotic use, so it seemed that one could rarely leave the pediatrician’s office without a prescription for one.
Antibiotics are only effective for bacterial infections, and won’t have any impact on viral infections such as the common cold. With the rise of antibiotic resistant infections, or so called “superbugs”, even the doctors prescribing these drugs have taken a muchmore judicious approach to using them. We now know that the risks of repeat antibiotic use during childhood are long-lasting and have been linked to increased risk of allergies, autoimmune diseases, diabetes, obesity and even ADHD later in life.
There are many situations where antibiotic use can be avoided. For instance, most urinary tract infections, ear infections, sore throats, and the weepiest of oozing red eyes can be treated safely and effectively by aggressively using the right herbs or natural treatments. —In fact, I’ve treated hundreds of these types of ailments in my own clinic with only natural medicines and have seen great success. . Even the dreaded diagnosis of “strep throat” can be treated with appropriate herbs by a trained professional. The overwhelming benefit of using a natural approach to these ailments is that the “good” bacteria in your gut stays protected. Additionally, you avoid the side effects that often come with antibiotic use, like bloating, diarrhea, constipation, fatigue, and loss of appetite.
Certainly, there are situations where antibiotics can be lifesaving–I personally owe my life to IV antibiotics used for a bad case of sepsis I experienced several years ago. And while ear infections and urinary tract infections almost never need to be treated with antibiotics, if you’re in pain, or have been up every night for a week with a sick, crying kid, and are at your wit’s end, you may wind up gladly accepting that prescription.
In cases of bacterial infection, antibiotics will do the job, but not without massive casualties among the beneficial flora in the gut that form our defense system.
Our digestive tract houses around 500 species and up to five pounds of bacteria that help preserve our health every day. We have trillions of bacteria populating our large intestines—in fact, their cells out-number our human cells; one could say that we are “more bacterial” than human. These tiny organisms are so critical to our survival, it’s like having another essential organ that you couldn’t live without! Beneficial (or probiotic) bacteria in our guts play a host of vital roles for our health:
Nutrition:
Intestinal bacteria actually synthesize essential nutrients like B12 and K2, or convert them from the food we eat into active forms. In fact, while we get some of our vitamin K2 from eating dark leafy veggies, up to 75% of it is made in the gut.
Studies have recently shown that some gut bacteria are able to produce the active methylated form of Folate (5-MTHF), a key component in things like brain function and mental health, cell division and DNA replication, and normal fetal development during pregnancy. Having adequate amounts of the right type of good bacteria can be a game changer for individuals with MTHFR mutations, who are notoriously at a disadvantage in producing adequate quantities of this essential nutrient.
Hormone Balance:
A healthy microbiome is an indispensable part of the process by which we maintain hormone balance. Specific bacteria produce enzymes that help us break down and metabolize our estrogen. Essentially, these bacteria work to flush hormones that have been used, and are ready for elimination, out of the body, making way for fresh new hormones to take their place.
If you have the wrong types of bacteria in your gut, then estrogens get reabsorbed and recirculated, setting the stage for estrogen dominance and associated symptoms such as infertility, PMS, low libido, cramps, heavy menstrual bleeding , and PCOS. This also makes us more susceptible to estrogen related cancers like breast and uterine cancer.
Without enough of the good guys, we are setting ourselves up for a toxic build-up of hormones that can lead to PMS, menopausal symptoms, or worse.
What is living in our gut strongly influences almost every conceivable aspect of our health. In fact, most people don’t know that symptoms like allergies, acne, depression, fatigue and autoimmune diseases often have digestive problems at their root.
Immunity and Respiratory Illness:
Our microbiome also supports our overall immunity. Approximately 70% of your immune system is located in your gut and the good bacteria are informing this at all times. Studies show that gut microbiota influences our immune system, both in the intestines, but also systemically.
The use of broad spectrum antibiotics, (and other factors like chemical exposure, diet, and environmental exposure) alter the makeup of our microbiome. Multiple studies report that this alteration can negatively influence the immune response in your airways leading to greater susceptibility to many allergic airway diseases, including seasonal rhinitis and asthma, as well as viral infections of the respiratory tract.
Acute respiratory tract infections are the leading cause of death in infants and young children worldwide, and while these can be bacterial in origin, the majority of them are caused by viral infections. Researchers believe that that the composition of the microbiome may affect the severity of viral infection in children.
Digestive Disorders:
Locally, in the gut, disruption of the balance in the microbiota (dysbiosis) has been associated with inflammation-linked disorders, like inflammatory bowel disease.
Metabolic Syndrome and Weight Gain:
A Danish study with 169 obese and 123 non-obese participants confirmed that people with lower amounts of good bacteria had higher body fat percentage, increased insulin resistance, higher markers of inflammation, and poor cholesterol balance. They also gained more weight over time.
Several days to a week of antibiotics will wipe out majority of the bacteria, both good and bad–decreased diversity and altered composition can be seen within 3-4 days. Even a single dose of Clindamycin (commonly prescribed for things like bacterial vaginosis or sinus infections) causes an enduring loss of 90% of normal microbial diversity.
Our intestines are somewhat like an apartment building—there is only space for so many tenants. You want to have primarily good tenants, who pay the rent on time, take care of the place, and like to keep tidy. But wiping out the majority of the tenants, both good and bad, leaves it as a toss-up in terms of who will take residency after you stop taking the antibiotic.
So, while bacterial counts in the gut start to recover within a week, studies show that the composition of the microbiome is significantly altered from what was present prior to treatment. And because antibiotics only work against bacteria, this leaves room for pathogenic yeast or fungal strains to gain a running head-start while you are taking the prescription. While yeast like Candida are a normal part of our healthy microbiome, they should only comprise a small percentage of a diverse population. When they start to overgrow, and run the show, a myriad of problems and increased production of toxins can disrupt our digestive health and also impact other body systems outside of the gut.
The good news is that we have a lot of influence over who we promote when it comes to rebuilding the good guys! If you must take antibiotics, here are a few things you can do to help protect your gut and immunity while taking them:
Foods
Avoid sugar, alcohol, dairy (except fermented), and gluten: These foods either contain proteins that are harder to digest across the board, or tend to feed yeast.
Eat probiotic fermented foods: sauerkraut, kim chi, any other fermented veggies such as beets or carrots, coconut kefir, kombucha, yogurt (preferably homemade and 24-hour).
Drink bone broth: collagen heals the gut and is also prebiotic (feeds the beneficial flora).
Eat Prebiotic foods: Prebiotics are fibers found in specific foods that are food for the beneficial flora. Jerusalem artichokes (sunchokes), raw dandelion greens, garlic, leeks, onions, jicama, Chicory root (which you can find in Dandy Blend beverage), asparagus, green bananas and plantains, cacao, burdock root, or foods high in resistant starch (such as cooked and cooled rice, legumes, or potatoes) are all foods with high prebiotic content. You can also take a prebiotic supplement, like Mega PreBiotic—start slow! Interestingly, these types of starches onlyfeed the beneficial flora, and not the “bad guys”.
Supplements
Butyrate: Part of the reason why prebiotics are so helpful is that they provide raw material for the good bacteria to ferment, producing short chain fatty acids.
Butyrate, one of the SCFA’s produced in this process, is the energy source of choice for the cells lining the colon and helps regenerate colonic mucosal membrane. It has several different actions that are cancer-preventative. Butyrate also fights inflammation in the gut. In fact, not having enough Butyrate can trigger or worsen ulcerative colitis, chron’s Crohn’s disease or colon cancer.
While most of our butyrate is produced by our healthy flora, grass-fed butter is also a great source of dietary butyrate, and, it is also available in supplement form. Generally, I recommend taking it for 2-4 weeks following antibiotic use.
Probiotics: The most important probiotic you can take during and after a round of antibiotics is actually a strain of yeast. Saccharomyces boulardii is a beneficial, non-pathogenic yeast that was first identified on lychee and mangosteen fruits in the tropics. While it may sound strange to intentionally put yeast into your digestive tract, S. Boulardii is a completely different species from the pathogenic candida species that are associated with digestive and other health problems. Besides increasing short-chain fatty acids (remember those from above? We want those!) that soothe the mucosal cells in the gut, these yeast are also stellar at treating and preventing diarrhea, and also boost secretion of IgA (immune agents) in the gut. They are helpful for treating C. Difficile infection, reducing inflammation in IBD, and help to prevent the formation of food-allergies. I recommend Designs For Health Floramyces, or Saccromycin DF by Xymogen. The dosage that I recommend in this case is 5-10 billion CFUs 3-4 times daily. It is important to start taking Saccharomyces Boulardii as soon as possible, as it can (and should) be taken during course of antibiotics to help prevent yeast overgrowth and calm inflammation. Since they only work on bacteria, antibiotics won’t kill the yeast. Keep taking it for 2-3 weeks after completing the antibiotic.
Generally, after the antibiotic is completed, I recommend adding in an additional Acidphilus/Bifidus containing probiotic blend for several weeks, such as Klaire Labs Therbiotic Complete.
Have you taken antibiotics and noticed health changes after taking them? Or, have you taken preventative measures like the ones above that you felt safeguarded your health? If so, what differences did you notice?



