What Causes Restless Leg Syndrome? Natural Remedies for RLS
You’ve just fallen asleep when it hits. That uncontrollable urge to move your legs.
Your legs also ache and throb.
It’s known as restless leg syndrome (RLS), and it makes you feel like you need to put a leash on your legs to keep them from trying to run away. Down boys! Down!
Restless leg syndrome is a condition where your legs are fidgety and uncomfortable, usually at night during sleep. But sometimes it can happen during the day when lying down or sitting for a long time, like when you’re in the car or at the movies.
Symptoms of Restless Leg Syndrome
The main symptom is the urge to move the legs. However, people with restless legs describe other symptoms such as:
- Aching
- An “electric” feeling
- Crawling
- Creeping
- Itching
- Pulling
- Throbbing
The condition is known for:
- Happening when lying or sitting for a long time.
- Relief with movement. The urge usually goes away when walking or stretching.
- Occurring mostly at night.
In some people, the disorder happens together with twitching or kicking of the legs while they’re sleeping. This condition is known as periodic limb movement of sleep.
Causes of Restless Legs Syndrome
There are a lot of reasons why you have restless legs. Since I specialize in treating women with gastrointestinal disorders I’m really familiar with one of the most common causes of RLS—small intestinal bacterial overgrowth, or SIBO for short. An imbalance in the gut microbiome—what scientists call dysbiosis—is also often to blame.
But there are other factors that can cause restless legs. In fact, there might be more than one culprit involved. Let’s dive into all those factors in this blog post and I’ll tell you the natural remedies for restless legs syndrome that have worked for my patients.
SIBO and Restless Legs
In my clinical practice, I see a lot of patients with SIBO who also have restless legs. Studies in medical journals confirm the link between SIBO and restless legs.
If you want to know more about what is SIBO, I recommend you read this blog post I wrote. Meanwhile, in a nutshell, SIBO is an imbalance in the microbes that live in the small intestine.
This can mean that there are too many bacteria or the wrong kind of bacteria that don’t belong in the small intestine.
So what does SIBO have to do with restless legs? A lot.
SIBO causes inflammation in the gut, which leads to the release of hepcidin, a hormone critical in delivering iron to the body and the brain.
Iron is necessary for growth and development as well as supplying the body with oxygen through the blood. But more important for our topic here, iron is a cofactor in the production of dopamine, a brain chemical (neurotransmitter) that tells leg muscles to relax at night. Without enough dopamine, muscles can remain hyperactive. The result? Restless legs syndrome.
When the body releases too much hepcidin, you might not even realize there’s a problem with iron. When you get tested for iron levels or for ferritin, the tests come back normal. And yet your body isn’t able to use the iron that’s available.
Eating enough protein is also critical for making dopamine. The body needs the amino acids tyrosine and phenylalanine from protein as well as iron to make dopamine.
I’m not the only one who connected the dots between SIBO and restless legs. In a small study published in the online version of the journal Sleep, SIBO was found in all seven participants with RLS. Compare this to the general population without restless legs; SIBO occurs in less than 15% of people.
Restless Legs Treatment #1: Work with a functional medicine provider to test for and treat SIBO. Dietary changes, probiotics, fiber, digestive support, and antimicrobials are often used to turn around SIBO. Eat 1-1.2 grams of protein per kilogram of body weight, taken daily in divided doses.
Gut Microbes Gone Bad
Sometimes, treating SIBO isn’t enough and the restless legs continue. There could be many reasons for that, but one of them could involve gut dysbiosis beyond just SIBO. Gut dysbiosis causes inflammation in the gut and the body. In my practice, I don’t just test for SIBO. I use stool testing to look for bacterial overgrowth, fungus, and parasites.
Imbalanced gut bacteria lead to many of the same problems that occur with SIBO, such as the release of hepcidin and the inability of the brain to use iron.
Restless Legs Treatment #2: Balance the gut microbiota through the use of a good probiotic and avoid factors that lead to an imbalance such as eating too much sugar and processed foods and stress. Your functional medicine provider may use antimicrobials, antiparasitics, and/or digestive support to optimize your gut microbiome. Eat 1-1.2 grams of protein per kilogram of body weight, taken daily in divided doses.
High Histamine
Another reason why SIBO or dysbiosis causes restless leg syndrome is because they can lead to histamine excess.
Histamine is a chemical found in many cells of the body. It causes allergy symptoms like itchy, red eyes, runny nose, and sneezing. When the body makes too much of it, it changes how the nervous system functions. This can be a problem for people with restless legs.
People who make too much histamine or who have histamine intolerance often have problems sleeping, since histamine is a brain stimulant.
The catch? Because histamine revs up the brain, people with restless legs who also are making too much histamine can get by on little sleep. They’re not sleepy in the daytime and can function even though they’re exhausted.
Scientists are now beginning to believe that targeting histamine receptors may reduce restless leg syndrome. Histamine receptors are proteins found on the surface of some cells. These proteins are triggered by histamine. Think of receptors like locks on a door and histamine as the key that fits into the lock and gets it to open.
Mast cells are immune cells found in the blood that release histamine as part of an allergic reaction. Now researchers are finding that when mast cells are activated, it may cause restless legs. People who have a condition known as mast cell activation syndrome are more likely to have restless legs compared to healthy controls.
Restless Legs Treatment #3: You can start by supplementing with DAO, an enzyme that breaks down histamine. Two other ways to support histamine levels are Natural D-Hist from Orthomolecular Medicine and quercetin. A low-histamine diet may also help.
But keep in mind that histamine excess is complicated. There are different pathways through which people have problems. It’s best to work with a functional medicine provider to find out if histamine excess is part of your problem and if so, why you’re making too much histamine.
B Vitamins for Restless Legs Syndrome
Vitamins B12 and vitamin B1 (thiamine or benfotiamine) can both fend off restless legs. For example, in patients with inflammatory bowel disease, vitamin B12 deficiency is linked to an increased risk of restless legs syndrome.
Vitamin B1 helps the body make a chemical called acetylcholine, which is involved in motor control. In other words, B1 supports the health of the nerves that control the muscles. So it makes sense that if you’re low in vitamin B1, your legs and body will fidget.
The body also needs vitamin B1 to make dopamine. As I mentioned earlier, dopamine is a brain chemical that says to the leg muscles: “Relax! Relax!”
I’ve had patients tell me that even when other restless legs treatments didn’t help, vitamin B1 worked miracles.
Restless Legs Treatment #4: Start by taking a B complex vitamin or vitamin B1 (up to 100 mg). You may need to go up to 300 mg, which you should only do under the supervision of a functional medicine provider.
Food Sensitivities
Food sensitivities may be to blame for restless legs in some people. A case study of three patients found that food sensitivities caused movement disorders including repeated shrugging of the shoulders. In these patients, milk, coffee, eggs, aspartame (Nutrasweet), tea, chocolate, citrus, raspberries, strawberries, potatoes, beef, and pork caused the most problems. This matches my experience in clinical practice.
Restless Legs Treatment #5: Work with a functional medicine provider, who can order food sensitivity tests to find out which foods don’t agree with you. They may also suggest an elimination diet or just removing the foods that bother you from your tests. After a trial period without the foods, your practitioner will instruct you to introduce one at a time while watching for symptoms. That way you can see which food is causing your restless legs.
Other Causes of Restless Legs
Here are other common reasons why my patients develop restless legs:
- Alcohol, caffeine, nicotine
- Certain medications
- Low vitamin D
- Pregnancy
- Stress/anxiety
- Vigorous exercise
Drugs That Cause Restless Legs Syndrome
Sometimes, the cause of restless legs is a certain prescription medication. Here are some of the most common drugs that cause restless legs.:
- Allergy meds
- Diphenhydramine
- Neuroleptics
- Selective serotonin reuptake inhibitors (SSRIs)
- Tricyclic antidepressants
Getting Rid of Restless Legs
I specialize in treating GI disorders and women’s health. So if you have digestive symptoms and restless legs, I know how to get at the root cause of why your legs are so fidgety.
The first step? Book a free 15-minute troubleshooting call with me to find out the best course of action.
If after the call you come on board as a patient, I’ll order certain tests to show whether your restless legs are caused by nutrient deficiencies, gut dysbiosis, or histamine excess. Whatever the cause, I’ll be on it until I find out what’s wrong. Book a call today so you’ll sleep more deeply tomorrow.
How to Prevent SIBO (Small Intestinal Bacterial Overgrowth) Relapse
You have SIBO (Small Intestinal Bacterial Overgrowth) and you completed all the necessary steps in the “kill phase” of treatment. You run a follow-up breath test and your gas levels have normalized! Or, you didn’t retest, but your symptoms are 90% better! This is great progress and it feels like you are finally moving forward!
But, if you’re just killing the bacteria – you’re only halfway there!!
Many SIBO patients get their initial SIBO treatments and feel good for a while. But then, all the bloating, gas, cramping, constipation, or diarrhea begin to make a very unwelcome comeback. For various reasons, too much bacteria will once again start colonizing the wrong part of the GI tract leading to SIBO relapse.
Unfortunately, it’s common to have SIBO relapse. But, don’t get discouraged. You’re not wading through the murky waters of SIBO treatment alone.
Let’s break down if your symptoms are IBS or SIBO, why SIBO relapse might happen, what you can do, and how to help prevent a relapse in the first place.
Are my symptoms IBS or SIBO?
When it comes to gut issues, it can be difficult to identify and understand your symptoms. In general, there are two common conditions of the intestines that can present very similarly: Irritable Bowel Syndrome (IBS) and SIBO.
IBS is a functional gastrointestinal disorder. It affects the two-way communication between your digestive system and your brain. When this communication system malfunctions it can throw off your entire digestive tract. Leading to symptoms like abdominal pain, bloating, and altered bowel habits such as constipation or diarrhea. Sounds a lot like SIBO, doesn’t it?
A single underlying cause of IBS has not been identified. But honestly, there are many factors that could lead to IBS including food sensitivities, severe infections, stress, or intestinal muscle issues. What’s interesting is that up to 78% of patients diagnosed with IBS have SIBO.
IBS and SIBO are complex conditions. But, since these conditions can present so similarly it’s important to rule out SIBO with a breath test so that we can customize your treatment plan.
What causes SIBO relapse?
I know what you’re asking…if I’ve done the work to identify the cause of SIBO and the SIBO treatment…why on earth is my SIBO coming back?!
Unfortunately, approximately 45 percent of all SIBO patients will experience a SIBO relapse. There are three primary reasons that my patients experience SIBO relapse: diet, underlying gut conditions, and medications.
Diet
Let’s call it like it is, diet changes are never a quick fix, they are a lifestyle change. A diet that is high in sugar, refined carbohydrates, FODMAP vegetables, or alcohol can make SIBO symptoms like gas, bloating, constipation or diarrhea worsen or relapse. It’s important to introduce foods like starchy veggies in the long run because it feeds the good gut flora. But introducing too much too soon is when you run into issues.
Underlying Gut Conditions
A physical obstruction in the gut can be both a cause of SIBO and subsequently the cause of SIBO relapse. Crohn’s disease, celiac, diabetes, and leaky gut are the four most common gut conditions that can cause SIBO.
Medications
Some medications may help with certain issues while wreaking havoc on others. Medications like antibiotics, antihistamines, NSAIDs, acid-blocking drugs (PPIs), and steroids all disrupt your normal gut flora. Some kill healthy bacteria and others increase the permeability of your gut. But, they all increase your chance of SIBO relapse.
How To Prevent SIBO Relapse
Preventing SIBO relapse starts during the “kill” phase of your SIBO treatment. There’s a lot you can be doing during and after SIBO treatment to prevent SIBO relapse. Here are a few things I like to include in SIBO treatment plans:
- Address Low Stomach Acid and Pancreatic Digestive Enzymes – These antimicrobial enzymes help enhance nutrient absorption and assimilation.
- Support your Oral Microbiome – 94 percent of Americans have some levels of gingivitis or bacteria in their oral cavities that can impact gut health. I recommend Blocidin toothpaste and dental rinse. Plus, don’t forget about flossing. Sorry, no water picks.
- Liver Support – The toxins from SIBO have inundated your liver. The endotoxins (the toxic substances bound to bacterial cell walls) from having SIBO saturate the bile and add to your total liver toxic burden. These systems need their own love to get back up to speed. Resolving the excess gram-negative bacteria is the first step. My favorite for bile support is MegaGuard by Microbiome Labs. Learn more about bile support and gut health.
- Repair Leaky Gut/Mucosal Inflammation and Damage – SIBO has likely led to an inflamed gut and has damaged the cellular walls and lining. Not only do you need to kill off harmful bacteria and rebuild healthy gut flora, but you also need to repair any structural damage. I recommend Super Curcumin by Apex, with either MegaMucosa by Microbiome Labs, or GI Balance by Xymogen.
What To Do After You’ve Cleared the Bacteria Causing SIBO
The first phase of SIBO treatment is tough and you’ve survived it. Congratulations! But now what?
Great question! There is a lot you can do after SIBO treatment to prevent relapse and stay healthy.
- Stay on a modified low FODMAP or SIBO Biphasic. To allow your microbiome to heal, I recommend following one of these diets for two to three months, followed by gradual reintroduction of foods that you have omitted.
- Add a Prokinetic to address gastroparesis and support the Migrating Motor Complex (MMC). Gastroparesis slows your stomach’s motility preventing it from emptying properly. MMC sweeps residual bacteria and leftover carbohydrates and protein particles out of the small intestine. Waiting 4 hours between meals allows MMC to work because it is only triggered during a fasted state. So, if we snack all the time or chug large amounts of liquid, we’re inhibiting the MMC housekeeping wave. Limit snacks and sip, don’t chug, your fluids. So remember, eat, stop, eat.
- Restore your vagal tone and your MMC by retraining your nervous system signaling. All of the approaches to restoring vagal tone for improved digestion focus on promoting your parasympathetic nervous system activity, over your sympathetic activity. The parasympathetic nervous system helps restore the body to a calm and composed state and prevents it from overworking. Sympathetic activity, on the other hand, prepares the body for a stress-related activity. Depending on what may be causing your sympathetic activity several techniques can be personalized based on your symptoms. This includes vagal nerve stimulation, gut-focused hypnotherapy, Frequency Specific Microcurrent, acupuncture, or the Gupta Program. And, if there has been a big stress or trauma other treatments like EMDR can be considered. Check out inaura.com to identify additional personalized therapy options.
- Add single-strain probiotics and prebiotics to your daily routine. Probiotics and prebiotics, added slowly to your diet, can help to rebuild and maintain your healthy gut flora. Because multi-strain probiotic blends are not generally tolerated by SIBO patients I recommend several single strain options based upon your specific symptoms and tendencies (i.e. bloating, constipation, diarrhea, histamine intolerance, etc.). I personalize your routine with some of my favorites including HU 58 (Microbiome Labs), BioGaia Protectis, probiomax by Xymogen, and Ideal Bowel Support (L Planetarium 299V). I start all my patients on a partial dose and work up to help bulk the stool without triggering SIBO. Once you are tolerating partial doses, we can reintroduce most FODMAP foods along with other strains of probiotics for continued gut repair. The key is going slow and steady. Adding any probiotics too soon or too quickly can flare SIBO.
To get you started, let’s focus on diet, probiotics, and prebiotics.
SIBO Treatment: Low FODMAP Diet and SIBO Biphasic Diet
Many of my SIBO patients hit the internet and find a lot of information on the “SIBO diet”. The SIBO diet is also known as a low FODMAP diet.
I recommend following a low FODMAP diet during SIBO treatment and for a short time after. But, in the long haul, a low FODMAP diet can be too restrictive. It does not offer you the necessary food diversity required for a robust and diverse microbiome. But, after the initial treatment, you can slowly reintroduce foods that will support your gut health and regularity.
Some patients also have a lot of success with a SIBO biphasic diet. This diet plan is as restrictive as the low FODMAP diet to start. But, it slowly reintroduces the most tolerated and least fermentable foods back in overtime. The foods eliminated don't change on the biphasic diet. Instead, it provides more guidance on what foods to reintroduce and when.
In reality, diet does not cause SIBO. Period. Diet can cause many other things like candida and poor microbiome health, but SIBO isn’t caused by diet. Instead, a highly-processed, low-quality diet tends to lead to increased symptoms and SIBO relapse. Diet is simply a way to manage your SIBO symptoms during the kill phase and long-term. And, it’s unique to each patient. Whether you follow a low FODMAP or biphasic diet, your SIBO treatment should include a full evaluation of your diet to help manage and control your symptoms.
Benefits of Probiotics and Prebiotics
I know it sounds strange, but utilizing probiotic and prebiotic supplements in the treatment of SIBO can be beneficial. It seems counter-intuitive. If excess bacteria in the small intestine cause SIBO, why would you want to add more?
Probiotics help to reduce bacterial overgrowth and hydrogen concentrations. And, probiotic supplements can help improve symptoms and restore a healthy gut microbiome. Which in turn increases your resilience against SIBO or general dysbiosis by promoting healthy expression of gut immunity and maintaining a strong and resilient mucosal membrane.
Prebiotic supplements, on the other hand, essentially provide the nutrients needed for healthy bacteria to flourish in your gut.
Ongoing research shows that probiotic and prebiotic supplements can be very effective in the treatment of SIBO. They can help improve symptoms, improve lab values, and support long-term gut restoration. Yet, not all probiotics and prebiotics are equal. It’s important to introduce the right supplements to focus on helping resolve your specific issues slowly and only as tolerated. Too much, or the wrong things can lead to SIBO relapse if the body isn’t ready. Generally, I start with PHGG (Partially Hydrolyzed Guar Gum) and Acacia.
Get Help With SIBO Relapse
SIBO is an incredibly complex condition that requires a great deal of time and energy to resolve.
Every case of SIBO requires personalized treatment. And as your health guide, we're here to put the pieces of your puzzle together and get you back on track. You deserve to live your life freely and feel well every day!
So, if you find yourself feeling defeated in your journey to better gut health, we are here to help!
Start by scheduling a no-cost, no-obligation 15-minute consultation call to regain control of your health.
References
"Probiotics for Preventing and Treating Small Intestinal Bacterial ...." https://pubmed.ncbi.nlm.nih.gov/28267052/. Accessed 10 Feb. 2022.
How To Know If You Have Hydrogen Sulfide SIBO - aka “Hidden SIBO”
Identifying and diagnosing SIBO (Small Intestine Bacterial Overgrowth) is tricky.
When it was first discovered, doctors thought SIBO was a rare disease…but now we know it’s actually incredibly common, with as much of 80% of people diagnosed with IBS (Irritable Bowel Syndrome) actually having SIBO.
But even with the knowledge that SIBO is actually super common, problems with reliable testing for SIBO mean it is STILL underdiagnosed.
But don’t worry - I’m not just here to complain. I have good news:
A new breath test for SIBO is now available that identifies all 3 main types of SIBO!
If you have “mystery” gut symptoms — and even if you’ve been tested for SIBO in the past and gotten a negative result — this information is very important for you!
The 3 Types of SIBO
SIBO is a condition where bacteria overgrow in the small intestine — as the name implies. The overgrown bacteria eat undigested food in the small intestine and produce gas as a by-product.
Different types of overgrown bacteria produce different types of gas: either methane, hydrogen, or hydrogen sulfide.
It’s the gas produced by the bacteria that causes SIBO’s hallmark symptoms: bloating and constipation or diarrhea.
Many practitioners classify SIBO into one of 3 types based on the type of gas:
Hydrogen SIBO - is associated with diarrhea
Methane SIBO - now also called “Intestinal Methanogen Overgrowth” or IMO, is associated methane SIBO symptoms of constipation
Hydrogen Sulfide SIBO - is the least well-understood and associated with diarrhea, but can also be present with constipation
Making it even more tricky, people can have more than one type of gas present, causing a mix of symptoms.
What Does Hydrogen Sulfide SIBO Feel Like?
People with Hydrogen Sulfide SIBO typically have some or all of the traditional SIBO symptoms:
- Bloating
- Gas
- Diarrhea
- Constipation
- Abdominal pain or discomfort
But I also look for these tell-tale signs of hydrogen sulfide:
- Bladder pain, frequency, or urgency
- Body or muscle pain
- Tingling or numbness in the hands and feed
- Sensitivity to noise and/or light
- Histamine sensitivity
- Sulfur-smelling gas (like rotten eggs)
- Whole body pain and overall feeling of unwellness
- Sulfur intolerance
Sulfur intolerance may be a condition you’re not familiar with. It’s symptoms are very similar to histamine intolerance: asthma, shortness of breath, hives/itchy skin, headaches, nausea, diarrhea, flushing, high or low blood pressure, brain fog, chronic stress (via elevation of cortisol and glutamate) and fatigue.
Sulfur is necessary to repair cells and carry out detox, but some people struggle with it for two reasons:
- Genetic mutations (like CBS or SOUX) that make it hard for them to process
- An abundance of sulfur-producing bacteria (like in hydrogen sulfide SIBO)
And some people have BOTH.
If you have a sulfur intolerance, you might find that high-sulfur foods — like kale, eggs, red meat, and garlic — make you feel worse, as do Epsom salt baths.
And if you’re a SIBO “tough case” or have chronic digestive issues, that’s another red flag for hydrogen sulfide SIBO.
Any of these signs are a great hint…but there’s only one way to know for sure. Let’s talk about that now.
How Do I Know Which Type of SIBO I Have?
The only way to know what type of SIBO you have is with a special test called a “breath test.”
To have a breath test, you’ll follow a special diet for 24 hours, then fast overnight. Then you’ll drink a sugar solution (made of either glucose or lactulose), and breath into a special collection device.
The idea is that the overgrown bacteria in your small intestine consume the sugar solution, ferment it, and produce gas. That gas can be measured in your breath sample. A practitioner trained in SIBO can interpret test results and prescribe treatment based on your gas type and level.
But the catch is that until now, only levels of hydrogen and methane could be detected in a breath sample.
That left many people who had the clinical symptoms of SIBO scratching their heads when their test results came back negative!
How could they have all the symptoms, but none of the methane or hydrogen gas? In many cases, the answer is hydrogen sulfide SIBO.
Hidden SIBO: Hydrogen Sulfide
Smart SIBO practitioners have found workarounds to help identify hydrogen sulfide SIBO even without a proper test - specifically looking for a test result pattern called a “flat line.”
But a flat line test result can only suggest hydrogen sulfide — not confirm it. Even more complicated, hydrogen sulfide may just be one of the gases present, and can explain why treatment for hydrogen or methane SIBO falls short of resolving all symptoms.
But all that is changing now!
New technology has created the first breath test for all three gases: hydrogen, methane, and hydrogen sulfide.
It’s called TrioSmart, and I’m really excited to have this as a tool in my kit for patients. While no test is 100% perfect, this can reveal some important information no other test can.
If you are tested and DO have SIBO of any type, we can use your gas levels and types to create a customized treatment plan.
Should I Get A SIBO Test?
Wondering if this new test might be for you?
Here are some of the indicators I look for:
- History of IBS or other “unexplained” digestive symptoms like bloating, constipation, or diarrhea
- History of restless leg syndrome or rosacea (both are commonly associated with SIBO)
- Past SIBO test was negative, but you still have symptoms
But you don’t need to figure this out…that’s MY job.
As your health guide, here’s what I do:
#1 Listen to you - your health history, your concerns, your questions.
#2 Create a customized plan - based on your health needs, your budget, and your schedule. Nothing one-size-fits-all.
#3 Support you along the way - answering questions, tweaking and updating your plan as needed, and anything else you need.
Sounds like what you need? It all starts with a no-cost, no-obligation 15 minute intro call with my team.
>>> Book a Free 15-Minute Consult
- Brie
PS - If you’ve been told you have IBS, and there is no solution, this test could change everything for you. I’d love to walk you through it, help you prep and order it, and most importantly: interpret the results and create a treatment plan! Step 1 is a free consult - book yours today.
The SIBO Testing Mistake I See All The Time (And How To Test For This Common Condition The Right Way)
Last week I had a consultation with a new patient who had the gut symptoms I see all the time: bloating, food intolerances, and bowel disturbances (yes, I’m talking constipation and diarrhea!).
After hearing her entire health history, I asked if she had ever been tested for SIBO (Small Intestine Bacterial Overgrowth).
“No, that’s not it” - she told me - “I had a stool test that was negative for SIBO.”
Major. Red. Flag.
This is a HUGE misconception - but stool tests cannot diagnose OR rule out SIBO.
I don’t blame this woman or her doctor for being confused. Even great practitioners are often unsure what tests can and can’t diagnose SIBO.
This is really important because with the right testing... SIBO can be treated and resolved, most of the time.
That means you can say goodbye to the bloating and gas (for good) and get back to enjoying life.
If you’ve got digestive complaints - even (and especially) if you’ve been told you don’t have SIBO before - this blog post is for you. Let’s clear up all the misconceptions about SIBO testing so you can get on the road to healing.
What Is SIBO?
Small Intestine Bacterial Overgrowth (SIBO) occurs when bacteria overgrow in the small intestine. Normally, there should be very few bacteria in the small intestine - instead, bacteria should live in the large intestine.
When bacteria overgrow in the small intestine, those bacteria can feast on undigested food as it leaves the stomach and enters the small intestine. As the bacteria eat, they produce gas (hydrogen, methane, and hydrogen sulfide) and that gas causes symptoms like diarrhea, constipation, and bloating.
So why do they overgrow? There are tons of reasons - but some of the most common reasons I see are:
- Endometriosis (which can cause sticky scars, called adhesions, inside that prevent the normal flow of bacteria)
- Certain medications that slow down the digestive system (opioids are a common culprit)
- Past food poisoning (which can trigger an autoimmune reaction that impacts motility)
If you’ve never heard of SIBO, you might think it sounds really rare or unusual… but it is very common. About one billion people worldwide have “Irritable Bowel Syndrome” - and of those, 60% are believed to actually have SIBO as a result of post-infectious IBS - which puts the estimate at about 600 Million people with SIBO!
Why Having SIBO Can Be Good News
The truth is I LOVE seeing a positive result on a SIBO breath test… not only does it explain why a patient has been dealing with symptoms (often for years)... but it is also a problem we can usually fix.
Depending on the type and severity of SIBO, it can be resolved in as little as one treatment cycle.
But successful treatment is wholly dependent on testing, since different types of SIBO require different treatments.
That’s why SIBO really requires not just an accurate test - but a practitioner who can interpret the results and create a customized treatment plan based on them.
Why Stool Tests Can’t Diagnose SIBO
To put it simply, stool tests are looking at the wrong part of the body. Stool tests tell us mostly what is happening in the large intestine - not the small!
So while it is possible that some of the organisms we see in stool testing are living in the small intestine, the results we get are more reflective of the large intestine.
Furthermore, while there can be some indicators that SIBO is likely from stool testing results, it's impossible to differentiate small vs. large intestine.
Stool tests can be really useful for diagnosing many other conditions - parasites, enzyme deficiency, and more - but they are not able to determine if bacteria is overgrown in the small intestine.
I love stool tests - and if you’re coming to me with gut issues, I almost always order a stool test - but it won’t tell you if you have SIBO!
Urine Organic Acids Tests Don’t Work Either
The urine organic acids test is another popular and really useful test - unless you want to diagnose SIBO.
The organic acids test can indicate if a bacterial overgrowth is present, but the problem is it can’t differentiate between the small and large intestine.
(Yes, Large Intestine Bacterial Overgrowth (LIBO) is a thing too!)
If you don’t know where the overgrowth is, you don’t know which treatment to use.
Again, this is a really useful test (and one I often use for other conditions) but it can’t diagnose SIBO.
The Right Way To Test For SIBO
There are 2 ways to test for SIBO properly:
- Endoscopy with culture (not commonly used anymore)
- Breath test (the gold standard and what I use)
(There is also a blood test for post-infectious IBS (which is a form of autoimmune IBS caused by food poisoning) that can be used, since most people with post-infectious IBS have SIBO. I use this if a breath test was inconclusive.)
The breath test is far and away the most simple, accurate, and useful of these tests, and it’s what I alway use with my clients.
That being said... Even though the breath test is the best, it doesn’t mean it’s perfect.
The breath test works by measuring hydrogen and methane gas in your breath after a special 24-hour prep diet and consuming a sugar solution (aka the test substrate). There are two options: glucose or lactulose.
The glucose test is only able to diagnose SIBO in the beginning of the small intestine (the small intestine can be over 20 feet long!). Because glucose is rapidly absorbed in the intestine, it isn’t good for finding SIBO that is farther down the small intestine.
The lactulose breath test can diagnose SIBO in any part of the small intestine, but it does have a higher rate of false positives.
Glucose is more likely to miss some cases of SIBO, but the ones it does identify are more likely to be true positive diagnoses.
Therefore, I sometimes run glucose and lactulose tests side by side to get a more complete picture.
Why The Right Test Matters So Much
I’ve said it before, but it’s so important that I will repeat it now: in SIBO, testing guides the treatment.
Depending on which gases are detected in your breath, and at what levels, treatment will differ.
That’s why it’s also really key to have help interpreting a test from a skilled practitioner. SIBO breath test results aren’t a simple “positive” or “negative” - you’ll get a graph that shows different gas levels at different points in the test.
If you’ve never seen them before, these graphs are confusing and overwhelming. But to someone who knows what they’re looking at, your breath tests results are like a map to healing your SIBO and resolving your symptoms.
Bottom line: if you suspect SIBO, get a breath test!
Get Help With SIBO
SIBO is a really complex condition (let’s not sugar coat it!). But it’s not incurable… and if you DO have it, resolving SIBO might be the answer to years of uncomfortable gut symptoms.
Every case of SIBO requires personalized treatment, but that’s part of why I love my job - helping you put the pieces of your health puzzle together and achieve your goals is my purpose in life!
I’ve helped hundreds of people diagnose and resolve SIBO… and I’d love to help you, too! There’s no need to make a commitment right now - book a free 15-minute consultation with my team to learn about how we could help you and what options you have here ---> Book a Free 15-Minute Consult
What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
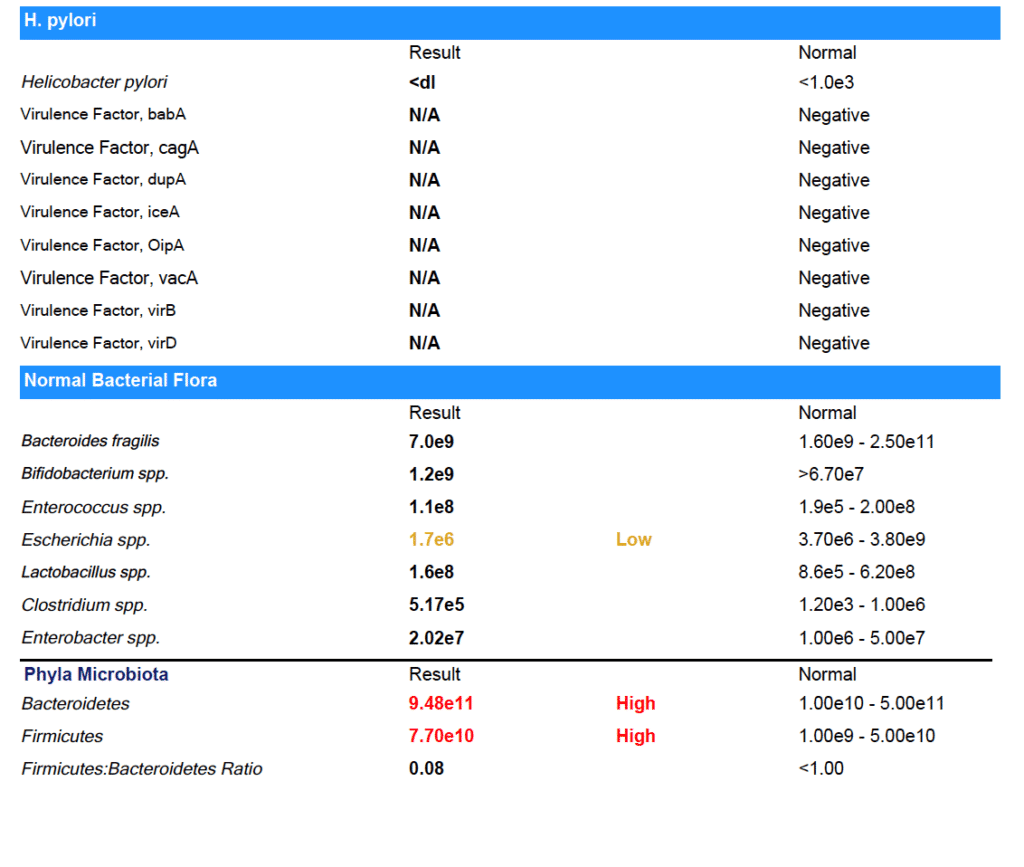
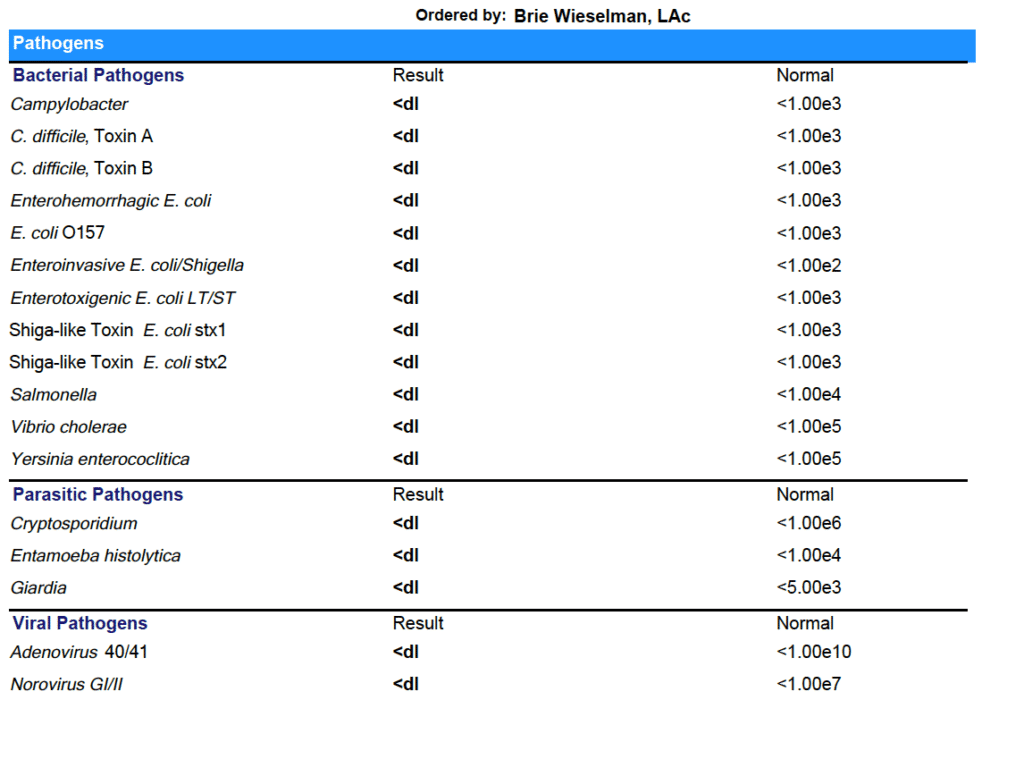
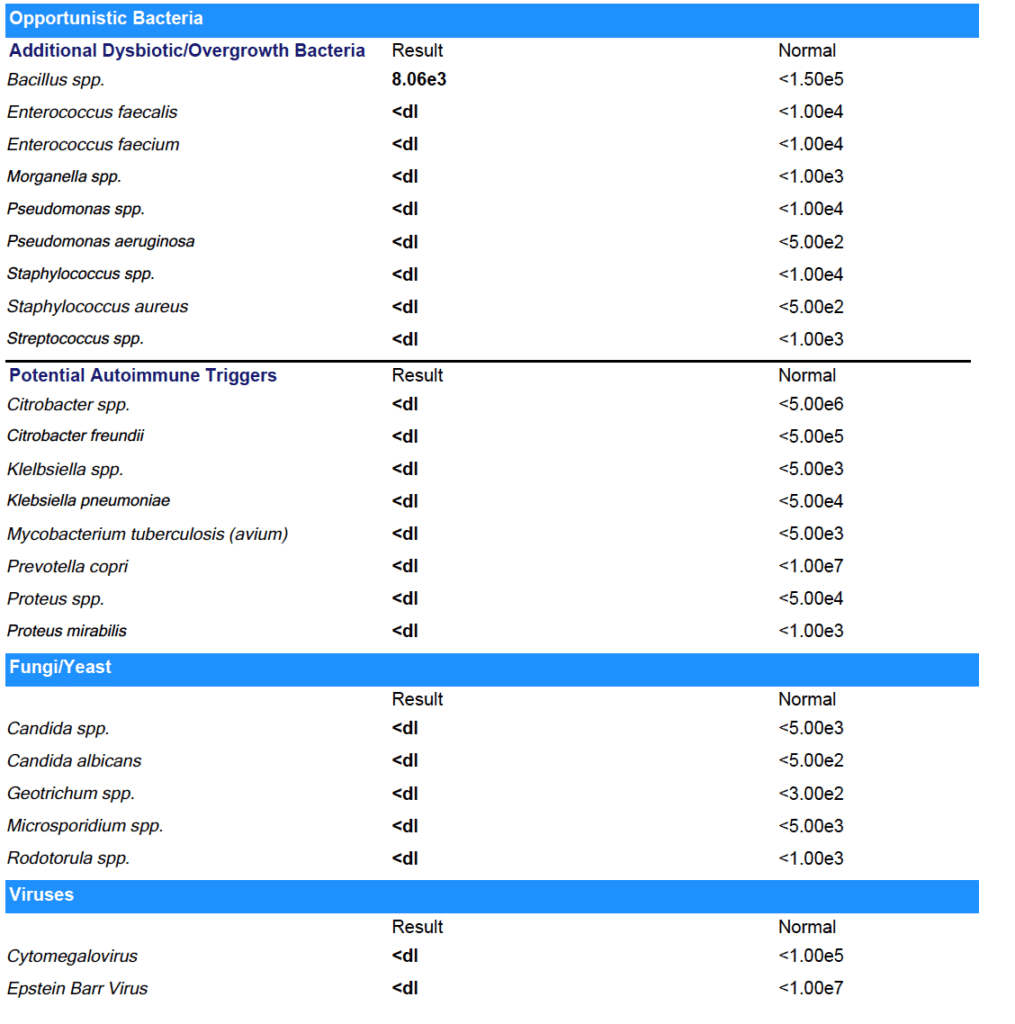
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
Marina agreed to the test, and a few weeks later, results were in:
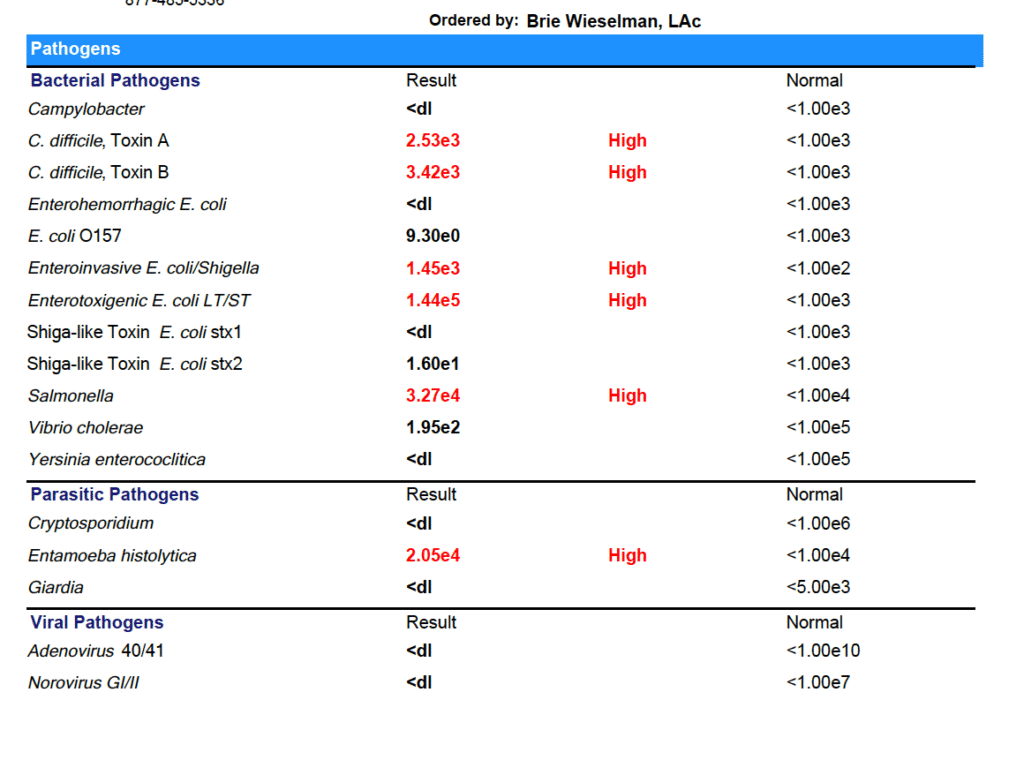
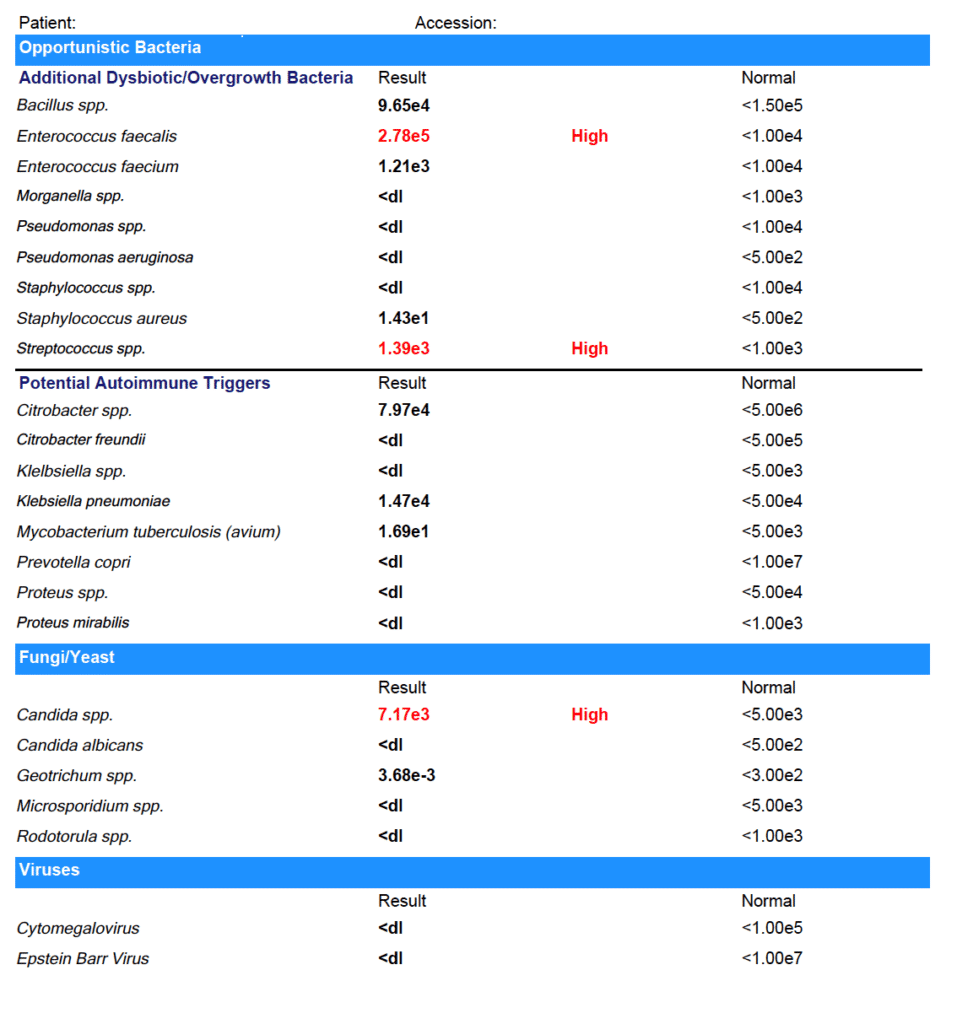
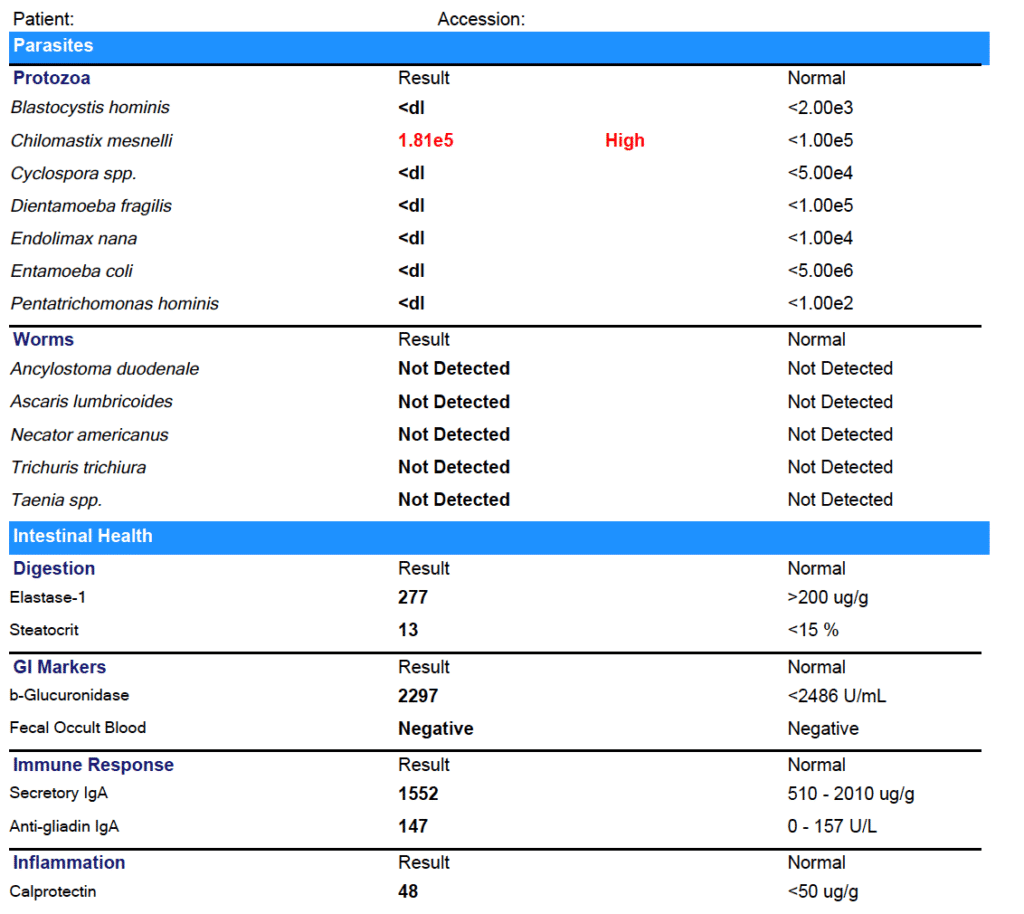
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
Step 3: The Second Test Results:
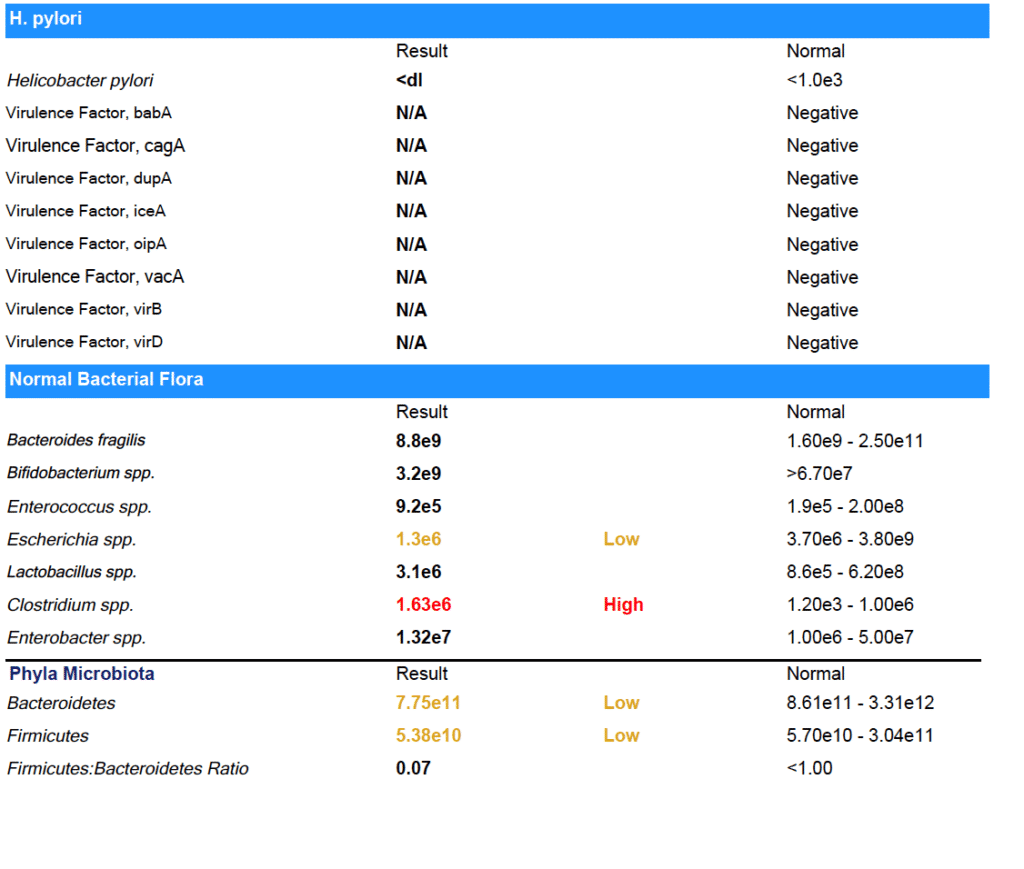
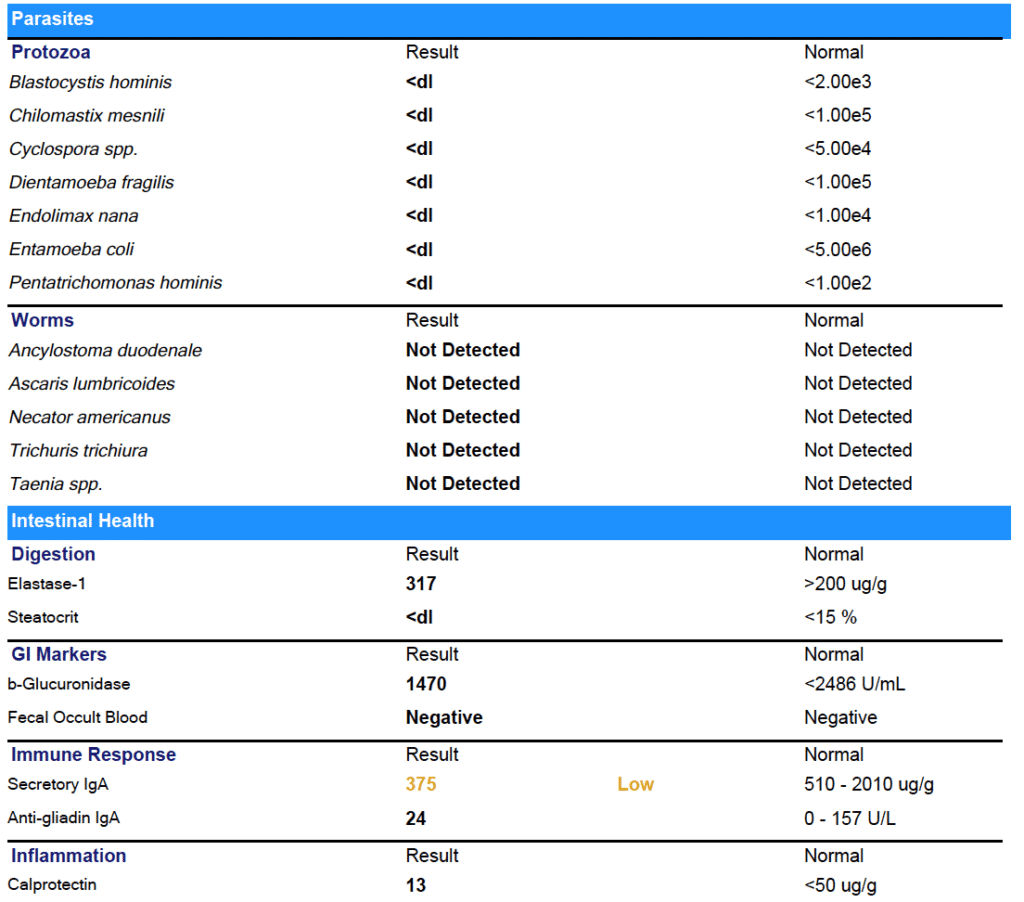
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
My Top Travel Tips for A Healthy Gut
Traveling is one of my biggest passions. When I got married, we chose to do a destination ceremony and reception with all of our friends and family in Sayulita, Mexico, instead of a traditional wedding (no regrets there!).
Traveling hasn’t always been fun for me, though. When I was younger, I felt like EVERY time I traveled, I got sick. And I’m not talking about a cold, folks - I’m talking about the nemesis of every globetrotter: traveler’s diarrhea.
Traveler’s diarrhea, Montezuma’s revenge, Delhi/Bali belly - it’s all caused by food poisoning. And while it will definitely ruin your trip, it also has a more sinister side - food poisoning can cause lasting damage to your digestive system leading to a lifetime of #gutproblems.
Want to know how food poisoning can cause long-term digestive issues - and what I do to avoid traveler’s diarrhea (even in the most exotic locales!)? Keep reading!
(Not interested in the science? Skip here for my travel tips).
How Food Poisoning Can Wreck Your Gut Long Term
I can’t tell you how many patient in my clinic can trace their digestive symptoms back to a case of food poisoning. And the science backs them up! Food poisoning is a known cause of irritable Bowel Syndrome (IBS). IBS after food poisoning is called “post-infectious IBS.”
But this gets a little complex, so bear with me here...
IBS isn’t a disease - it’s a syndrome. That means it’s just a name for a group of symptoms (fun stuff like gas, bloating, diarrhea, constipation, and food intolerances). IBS is a diagnosis of exclusion, meaning your doctor will call your symptoms IBS when they can’t find any other cause for them.
For many people - perhaps as much as 60% - the actual cause of IBS symptoms is something called Small Intestine Bacterial Overgrowth (SIBO). SIBO occurs when bacteria that should be confined to the large intestine migrates up and into the small intestine. A healthy small intestine should have very little bacteria in it!
So how does bacteria get from the large intestine to the small to cause SIBO?
It’s usually do to a problem with the Migrating Motor Complex (MMC). The MMC is what creates movement in your intestines - called peristalsis - and moves food from your stomach down through your intestines and eventually out of your body.
So what can harm your MMC? The most common causes are chronic viruses like Lyme disease, structural abnormalities, high stress levels, and… food poisoning!
Stay with me here - food poisoning can cause your Migrating Motor Complex to malfunction. When the MMC malfunctions, bacteria can move from the large to small intestine and overgrow, causing SIBO - and SIBO is the cause for as much as 60% of IBS!
As you can see, it’s a complex chain of events - and that’s why for years doctors have missed the connection between IBS, SIBO, and food poisoning. Luckily they are catching up now.
Toxins & Autoimmune Responses
So how exactly does the food poisoning cause damage to the Migrating Motor Complex?
Common food poisoning bacterias like E. coli, salmonella, Campylobacter jejuni, and Shigella all produce a toxin called cytolethal distending toxin B. It sounds bad, doesn’t it?
Your body will start producing antibodies against the cytolethal distending toxin B. For some people, they’re able to fight it off over in a few days and move on without long-term problems, but for about 10% of us (raising my hand!) we can’t fight it off as quickly - and therefore we keep producing more and more antibodies.
These antibodies don’t just fight the cytolethal distending toxin B - they also reduce a kind of protein in our intestine called vinculin.
Vinculin is very important in the health of Migrating Motor Complex - vinculin is crucial for proper function of nerve cells in the gut that cause peristalsis. When the MMC isn’t functioning and movement of food through the gut is slowed down, bacteria can overgrow and cause SIBO - plus other symptoms like bloating and gas.
The good news is that your gut can recover vinculin over time. First, you need to heal the SIBO. But it’s also critically important that you don’t get food poisoning again. So if you already have some gut issues, don’t stop reading now!
Here’s What I Do To Avoid Traveler’s Diarrhea
The key to avoiding traveler’s diarrhea is being proactive - think about where you’re going, research, and prepare! There are supplements I take to prevent illness, supplements I bring with me for defense in case I start feeling sick, and hygiene practices I follow, too.
Supplements I Use When Traveling To Keep My Gut Happy
When I’m travelling, I always take a probiotic. My favorites are Floramyces (which contains the yeast Saccharomyces boulardii) or UltraFlora Acute Care (this one blends S. boulardii with Bifidobacterium and Lactobacillus). I take 1 capsule of either, 1-2 times daily.
I also take Biocidin Advanced Formula Liquid to help boost my immunity. I start with 3 drops per day and work up to 5-10 drops twice daily.
Finally, I always take an Adaptogen blend. Adaptogens are herbs that help mitigate the stress of traveling. Yes, traveling is fun - but it is also hard on our bodies! Moving through time zones, awkward sleep schedules, and even just enjoying all the “newness” are all registered as stress to our bodies. I like blends that contain herbs like rhodiola for emotional and mental stress and eleuthero for physical stamina. NanoMojo Liquid and HPA Axis Homeostasis are my two go-tos.
Don’t Eat That!
Hygiene practices are so important for avoiding traveler’s diarrhea.
I always carry hand sanitizer with me - but not the conventional kind! Commercial hand sanitizers are full of BPA and other chemicals. Instead I make my own from aloe vera gel with lavender and tea tree essential oils, plus some Silvercillin. If you don’t want to make your own, this is good alternative. And of course - wash your hands with hot soap and water whenever you can.
Only drink bottled water - and never get ice! (Yes, even on the plane and in fancy restaurants!)
Avoid salad and uncooked veggies - especially lettuce. Cooked veggies (and cooked, hot food in general) are better when traveling. Worried about missing your greens? I bring a greens powder with me and mix it with bottled water. This one is my favorite.
Make sure you wash any produce you buy. As tempting as it is, don’t eat fruit straight from the farmer’s market cart. Wash it with a non-toxic fruit and veggie disinfectant first!
When eating out, look for food carts and restaurants with long line and plenty of locals.
Do This If You Feel Something Coming On
The minute I start to feel “off” - fatigued, grumbling stomach, or even a headache - I switch from my prevention to my treatment protocol.
I up the Biocidin Liquid to 10 drops, 3x per day.
I double up the probiotic.
I add in Oregano Oil Gelcaps for several days - 2 caps 3x daily.
And if diarrhea strikes? I go to a classic Chinese remedy called Huang Lian Su. It’s a blend of berberine-containing herbs that always works for me. I use 4-5 tablets, 3-4 times daily.
Happy Trails To You!
I hope these suggestions helps ease your fears about traveler’s diarrhea - and allow you to travel the world without getting sick!
And if you think food poisoning is at the root of your SIBO or gut problems, I hope you’ll consider working one-on-one with me to get it resolved. There is hope for overcoming gut problems - even one you’ve had for years! You can book a free consult with my team anytime. We’d love to help you!
Acid Reflux and Chronic Urinary Tract Infection; Totally 'Unrelated' Symptoms With the Same Root Cause?
One of the principles of Functional Medicine is finding and treating the “root cause.”
But sometimes, it isn’t as simple as finding one root cause and getting rid of it. Most of my clients have multiple health concerns - and multiple causes behind them. Helping them is about peeling back the layers and addressing each one as we go.
For my client Jane, peeling back the layers was exactly what we needed to do! She came in because she was experiencing tightness in her chest caused by acid reflux - and we wound up working through multiple gut infections, addressing vaginal dryness, and putting interstitial cystitis (a condition that causes chronic bladder pain like a urinary tract infection) into remission.
Every time we treated another “layer” Jane felt better than before.
Today, Jane wants to share her story in her own words. If you’re considering pursuing help with a Functional Medicine Practitioner like me, I hope this story helps you better understand the process of working with a practitioner.
Jane’s Story
About three years ago, I started dealing with some bloating. Then, I’d occasionally have constipation - not all the time, but enough that I noticed it. I had a colonoscopy and the results came back normal. I started taking a probiotic. The bloating and constipation just became kind of a general annoyance I was living with.
But then I started feeling tightness and pain in my chest. That was really scary. I went to the doctor right away, but the tightness and pain weren’t heart-related. That’s when I realized they were actually a digestive issue. I decided to go see a physician at my regular clinic, and they told me it was acid reflux, prescribed Prilosec, and referred me to a GI doctor.
Luckily I had read enough about Prilosec to know I didn’t want to take a proton-pump inhibitor. Instead, I decided to get a second opinion from a Functional Medicine Practitioner - that was Brie.
Working With Brie
From the start, Brie was very thorough. She took a really detailed history that helped me connect some dots about what had started all my digestive symptoms in the first place. The past summer, I’d had a urinary tract infection and taken a course of antibiotics. Then in the fall, I went traveled out of the country and had to take a course of the antibiotic Cipro for traveler’s diarrhea. That's when the bloating and constipation became worse and the other acid reflux symptoms started.
But she wasn’t just interested in the acid reflux - Brie asked questions about my overall health. When I told her I was experiencing vaginal dryness, urinary pain, and low libidio, she took me seriously. My doctor had diagnosed my with interstitial cystitis - basically pain in my reproductive organs for no reason.
Brie explained to me how the antibiotics had killed the good bacteria in my gut as well as the bad. She recommended stool testing and a breath test for Small Intestine Bacterial Overgrowth (SIBO), as well as hormone testing. She also recommended I cut out dairy and gluten temporarily to give my system a break, since those foods are common gut irritants. She also recommended some supplement that would soothe my gut and help with symptoms until we got the test results back. All this happened at our very first meeting!
The Test Results Came In
The test results came back a few weeks later - they showed low cortisol, low estrogen, H. pylori, low beneficial flora, and a few overgrown bacteria (citrobacter, pseudomonas). Plus, I had both methane and hydrogen type SIBO and was under-producing pancreatic enzymes.
It was a lot to take in and I was so glad I had Brie to help me understand what the results meant. She saw how everything was connected.
Brie explained that the H. pylori infection was likely causing the acid reflux, and that the SIBO was probably the cause of the constipation and the uti bloating. My hormone problems were tied in to all of it and causing the vaginal dryness, urinary pain, and low sex drive.
It was a relief to know there was a reason I was feeling the way I was feeling - especially because my symptoms had gone into a flare as we waited for the test results. I remember going to visit a friend for a few days and having to come home early because I was just so uncomfortable.
Brie started my on a supplement protocol for 6-8 weeks for both the H. pylori and the SIBO. I kept avoiding gluten & dairy, too.
After I finished the first supplement protocol, we re-tested. The H. pylori was gone! The SIBO levels had come down, but it wasn’t completely gone. On the second stool test, I also had positive results for some other common gut infections and parasites, including candida overgrowth. Brie explained that all of this was normal - the first protocol of supplements had helped destroy the “biofilm” - the protective cover the bad bacteria use to protect themselves and hide. With the biofilm gone now, we could see other parasites and better treat the SIBO, too.
By, then my acid reflux was totally gone and I was feeling pretty good gut-wise. But I was still struggling with the vaginal dryness and hormone symptoms. And, what I initially thought was a bladder infection turned out to be Interstitial Cystitis. The “UTI” pain didn’t respond to normal treatments, and the pain turned chronic. Can a UTI cause bloating and constipation?
Putting Interstitial Cystitis Into Remission
My hormone symptoms were slowly improving as my gut healed - but Brie also suggested using a plant-based bioidentical estrogen replacement. She also had me use vaginal DHEA, a vaginal probiotic, and some herbs. Those helped me feel better right away.
Brie also explained that two of the bad bacteria that the tests had shown were overgrown in my gut - proteus and citrobacter - were related to the Interstitial Cystitis, too. As we treated those, my symptoms disappeared completely.
Brie suggested I work with a pelvic floor therapist, too. That helped me relax some overly tight muscles that were contributing to the pain.
Changing My Diet
Brie suggested I follow a gluten and dairy-free, low-FODMAP diet. It helped me a lot in the beginning, but I was anxious to reintroduce more foods as soon as I could.
After a few months, I was able to reintroduce beans and some other legumes, which I hadn’t been able to tolerate for years, and I really missed. I am now back to eating all fruits and veggies, and I can even add in a little gluten here and there. That makes me feel good!
Where I Am Now
After working with Brie, I feel great for the first time in years.
I came to see her because of the acid reflux - but she opened my eyes to a lot of problems I had been writing off as “normal” or just “part of getting older.”
Gut-wise, I am feeling so much better now! After having given up gluten and dairy for years, I’m finally able to experiment with adding them back into my diet again now.
The interstitial cystitis pain is gone now, too. I didn’t realize how much the pain held me back from enjoying life - I even cancelled an overseas trip because of it!
I’m so happy to be where I am now with my health. I’m following a maintenance protocol now and continuing to meet with Brie occasionally to make sure I’m doing the right things moving forward.
Working with Brie has made a huge difference for me, and I wish more people could have access to it! I hope my story helps to spread the word.
Do You Need Help, Too?
Jane had amazing success - she cleared multiple gut parasites, fixed her digestion, reversed interstitial cystitis, and was even able to reintroduce foods she hadn’t eaten in years.
Why was she so successful? Because she dedicated herself to working through the process of Functional Medicine. She didn’t give up even when it got complicated - and neither did I!
I hope reading Jane’s story has helped you understand better understand the process of working with a Functional Medicine Practitioner like me.
If you’re inspired and ready to start your own journey, you can book a free, no-obligation Prospective Patient Interview with my team. During this 20-minute appointment, we’ll learn about you and discover if you’re a good fit for working with us.