Perimenopause and Leaky Gut: The Missing Estrogen Connection
If you’ve been trying to heal your gut with all the usual suspects—glutamine, probiotics, maybe even bone broth—but aren’t seeing lasting results, there’s a critical factor you might be overlooking: your estrogen levels. Specifically, the protective role of estriol and ER-beta receptors in maintaining your gut integrity.
It turns out, estrogen does more than regulate your cycle or fuel hot flashes during menopause. Estrogen, especially estriol (the form most prevalent during pregnancy), plays a significant role in gut health, tight junction integrity, and even protection against inflammatory bowel diseases like colitis. And if your estrogen levels are low—whether from perimenopause, menopause, or even due to birth control pills—you might find it almost impossible to heal your gut completely. Let’s dig into why.
The Gut is One Cell Thick—Yes, You Read That Right
Your gut lining is only one cell layer thick, made up of delicate columnar enterocytes. These cells form a tight barrier between your intestinal contents and your bloodstream—a fortress against pathogens, toxins, and undigested food particles that could otherwise trigger systemic inflammation. When working optimally, your gut cells should open and close on demand, like well-oiled gates that let in nutrients and keep out harmful invaders.
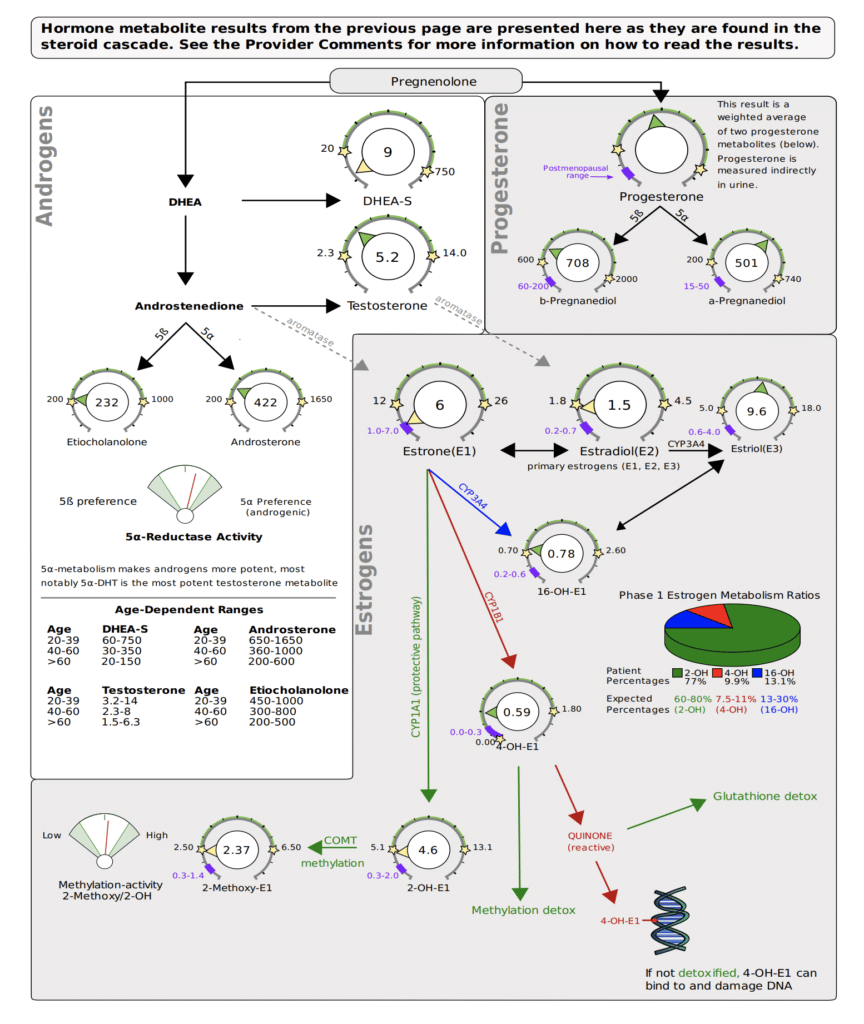
But without adequate estriol and ER-beta receptor activation, these gates can malfunction. This is where the importance of estrogen, particularly estriol, comes in. When estrogen levels drop, especially during menopause or as a result of birth control pills (which block ER-beta), the proteins that help keep those tight junctions closed—proteins like occludins and junctional adhesion molecule-A (JAM-A)—stop functioning properly. Without these proteins, your gut lining becomes porous, a condition commonly known as leaky gut.
Estrogen, ER-Beta, and Gut Health: The Missing Link
Estrogen receptors, particularly ER-beta, are heavily expressed in your intestinal epithelial cells. ER-beta and estriol oversee the proper function of the gut’s tight junctions. According to a study published in Microbiome (2022), estradiol modulates paracellular permeability and tight junction function, reinforcing the intestinal epithelial barrier. These effects are particularly significant for estriol, which acts as a major gut protector by upregulating proteins like occludins that control the space between your gut cells.
As you age, declining estrogen levels reduce this protective mechanism, making you more prone to conditions like microscopic colitis, which is more common in postmenopausal women. Why? Because when your gut opens up, it can’t re-close without enough estrogen to signal the production of these critical proteins. The result is a gut that’s constantly inflamed, permeable, and susceptible to irritation and inflammation.
Colitis and Low Estrogen: Another Layer of Protection Lost
It’s not just leaky gut that’s exacerbated by low estrogen. Colitis, an inflammatory condition of the colon, is also influenced by estrogen levels. A study published in Toxicology and Applied Pharmacology (2020) highlights the protective effect of estradiol against colitis, demonstrating that estrogen plays a crucial role in regulating inflammation in the gut. Without sufficient estrogen, the gut becomes more vulnerable to chronic inflammation, increasing the likelihood of developing colitis and other gut-related disorders.
Birth Control Pills Block ER-Beta—and Worsen Gut Health
Now, what about birth control pills? These are often prescribed to women for hormone regulation but could be working against you if you’re struggling with gut issues. Birth control pills block ER-beta, meaning they halt one of your body’s primary protective mechanisms for the gut lining. Studies in animal models have shown that oral contraceptives worsen gut permeability and even liver injury by promoting an increase in endotoxin release from the gut into circulation.
In simple terms: birth control pills could be contributing to your leaky gut by disabling the very receptors that estrogen needs to heal it. This creates a vicious cycle—without adequate estrogen (especially estriol), your gut lining remains vulnerable, allowing toxins to enter the bloodstream, worsening inflammation, and potentially leading to more severe conditions like colitis.
Why You Can’t Heal Leaky Gut with Low Estrogen
If you’re perimenopausal, menopausal, or using birth control pills, you’re at an even higher risk for developing or maintaining a leaky gut. You can take all the gut-healing supplements in the world, but without addressing your hormone levels, particularly estriol, you might be missing the foundational key to recovery.
This is why women in their 40s and 50s are more prone to gut issues like colitis, bloating, and food intolerances. As estrogen levels drop, your gut lining becomes less resilient, leaving you more susceptible to chronic conditions that seem to come out of nowhere.
Conclusion: Healing Requires More Than Supplements
The key takeaway? Without proper estrogen support—especially estriol and the activation of ER-beta—your gut won’t have the tools it needs to rebuild tight junctions, regulate inflammation, or stay resilient against toxins. Whether you’re dealing with leaky gut, colitis, or other inflammatory gut issues, addressing your hormonal health is not just important—it’s essential.
You can take all the gut supplements and probiotics on the market, but if your estrogen is low, your gut will keep struggling. The power to heal might lie in balancing your hormones first.
Citations:
- Luong T et al. (2022). Estrogen and Gut Health. Microbiome. https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-022-01356-2
- Estradiol Protects Against Colitis. (2020). Toxicology and Applied Pharmacology. https://www.sciencedirect.com/science/article/pii/S0304383520303517
Hormone Therapy, Anti-Aging, and Health Inequity: Why Balanced Hormones Are the Key to Longevity—And Why Every Woman Deserves Access
Hormone therapy (HT) is often discussed as a solution for managing the symptoms of menopause—hot flashes, night sweats, mood swings—but it’s so much more than that. Emerging research shows that HT is also a powerful tool for anti-aging and long-term health, particularly in slowing down biological aging and reducing the risk of chronic diseases like cardiovascular disease (CVD) and cancer.
However, as we look closer at the data, it becomes clear that this conversation isn’t just about hormones. It’s also about access to care, medical racism, and the inequities in our healthcare system that leave certain women behind. Let’s break down the science of HT, what the latest research reveals, and why the way we think about hormone therapy, especially for marginalized women, needs to change.
The JAMA Study: What You Need to Know
In 2024, a major study published in JAMA analyzed data from 117,763 postmenopausal women to understand how HT impacts biological aging. The study used phenotypic age, a calculation based on a range of biomarkers (like inflammation and immune function), to compare a woman’s biological age with her actual chronological age. The results were clear: women using HT had younger biological ages than those who didn’t.
Here are the key takeaways:
- HT users showed an average of 0.17 fewer years of biological aging compared to non-users.
- Women who started HT at age 55 or older had an even greater benefit, showing 0.32 fewer years of biological aging than their actual age.
- HT use was linked to a 12.7% lower risk of all-cause mortality, particularly from cardiovascular disease.
- HT users also saw about a 5% reduction in major cancers, with better cancer survival rates and lower chances of recurrence for those who returned to HT after treatment.
Clearly, HT isn’t just about symptom management. It’s about longevity and anti-aging.
Timing and Duration: Is There Really a Limit?
One of the more surprising conclusions from the study was that using HT for more than 7.4 years might be associated with increased biological aging. But when we take a step back and look at the bigger picture of hormone health, this conclusion seems flawed. Here’s why:
- Self-Reported Data Issues: The study relied on participants’ self-reported data regarding when they started and stopped HT. This opens the door to inaccuracies, as people often misremember dates or durations, which could skew the study’s findings.
- Lack of Clarity on HT Types and Routes: The study didn’t clarify which types of hormones were used (e.g., estrogen alone or estrogen-progesterone) or how they were administered (e.g., orally, transdermally). This is critical because different forms of HT can have very different effects on health outcomes, and without this clarity, it’s hard to draw firm conclusions.
- Contradictory Evidence on Long-Term Use: Other studies, such as the Million Women Study and extensive research on breast cancer, show that long-term HT use is linked to lower cancer rates, better survival rates, and even reduced recurrence of cancer. These studies clearly support the idea that staying on HT longer could offer more protection against aging-related diseases.
- Hormone Deficiency and Aging: When we’re in our 20s and 30s, our hormones are at their peak, and we see lower rates of chronic diseases like cardiovascular issues and cancer. Our tissues are younger, heal faster, and regenerate better. As hormones decline with age, diseases become more common, and tissues age and lose the ability to regenerate effectively. Given this, it doesn’t make sense that longer HT use—which helps maintain hormone balance—would lead to negative outcomes. In fact, keeping hormones balanced longer should logically help tissues stay healthier and younger for longer.
So, while the JAMA study suggested a limit of 7.4 years, the broader body of research indicates that long-term HT use can actually provide significant health benefits. This is why it’s important to interpret the study’s findings with caution.
Medical Racism and Social Justice: Who Gets Left Behind?
Beyond the data, this study brings to light a much deeper issue: the role of medical racism and social injustice in healthcare access. The study showed that women from lower socioeconomic backgrounds (SES)—who often come from marginalized racial and ethnic communities—benefited the most from HT. These women had more pronounced reductions in biological aging when they used HT compared to women from higher SES backgrounds.
However, these same women are the least likely to have access to HT. Here’s why this matters:
Systemic Barriers to Care
Women from lower-income backgrounds and marginalized communities face multiple barriers to healthcare:
- Implicit bias from healthcare providers often leads to women of color being dismissed or not offered treatments like HT, even when they report severe menopausal symptoms.
- Financial barriers mean that many low-income women can’t afford HT or don’t have access to healthcare providers who offer it.
- Geographic and systemic inequalities in healthcare access further marginalize these women, keeping them from receiving treatments that could significantly improve their health and longevity.
This isn’t just a healthcare issue—it’s a social justice issue. The women who stand to benefit the most from HT are the ones being denied access because of structural inequalities embedded in the medical system.
Medical Racism in Menopause Care
Women of color, particularly Black and Hispanic women, are more likely to experience worse menopause symptoms but are less likely to be offered or informed about HT. This neglect is part of a broader pattern of medical racism that impacts everything from maternal care to chronic disease management.
The JAMA study indirectly highlighted this inequality by showing that women from lower SES backgrounds saw the greatest benefits from HT in terms of reduced biological aging and mortality. But without addressing the systemic barriers preventing these women from accessing care, this research simply becomes another statistic in a long line of health disparities.
The Call to Action: Healthcare for All Women
This study underscores the urgent need to fight for health equity. We can’t talk about hormone therapy and anti-aging without addressing the fact that many women, particularly women of color and those from low-income communities, are being left behind.
What can we do?
- Push for policies that make hormone therapy accessible and affordable for all women, regardless of their socioeconomic background.
- Address implicit bias in healthcare by ensuring that women of color receive the same level of care and treatment options as their white counterparts.
- Raise awareness about the benefits of HT, especially for women who may not even know that these options exist due to systemic barriers in healthcare access.
Hormone therapy is a powerful tool for promoting healthy aging, reducing mortality, and improving quality of life for postmenopausal women. But for it to be truly effective, everyone must have access to it.
The Bottom Line: Hormone Therapy for Longevity
Hormone therapy isn’t just about relieving menopause symptoms. It’s about slowing biological aging, reducing chronic disease risk, and enhancing longevity. For women in marginalized communities, HT could be a key part of closing the gap in health disparities. But without equitable access to care, those who need it most will continue to miss out on its life-changing benefits.
As we move forward, we need to rethink how we offer and provide HT, ensuring that it’s not just available to the privileged few, but to every woman who can benefit from it. After all, aging well is something that should be within reach for everyone.
Will Using Hormone Replacement Therapy Help Me Lose Weight?
Hormone Replacement Therapy (HRT) is often the first line of defense women consider when they experience the upheaval of perimenopause and menopause. Hot flashes, night sweats, mood swings, and sleep disturbances are some of the well-known symptoms. But what about weight gain? Can HRT help you lose those stubborn pounds that seem to pile on during this transitional phase?
In this in-depth blog, we’ll explore the multifaceted relationship between HRT and weight loss. We’ll dive into the hormonal changes during perimenopause, the role of diet and protein intake, the significance of mitochondrial function, gut health, and the impact of muscle mass on metabolism.
Understanding Hormones and Weight Gain
During perimenopause, levels of estrogen and progesterone fluctuate and eventually decline. Estrogen, in particular, has a significant impact on body weight and fat distribution. As estrogen levels drop, many women notice an increase in abdominal fat – often referred to as “menopause belly.”
Estrogen and Fat Distribution
Estrogen helps regulate body weight by influencing insulin sensitivity and glucose metabolism. Lower estrogen levels can lead to increased fat storage, particularly around the abdomen. This shift in fat distribution is not just a cosmetic concern; it’s also linked to an increased risk of metabolic disorders like type 2 diabetes and cardiovascular disease.
Progesterone and Fluid Retention
Progesterone has a diuretic effect, meaning it helps your body eliminate water. As progesterone levels decline, women may experience bloating and water retention, which can contribute to a feeling of weight gain.
The Role of HRT
Hormone Replacement Therapy can help mitigate some of these changes by supplementing the body’s estrogen and progesterone levels. While HRT can alleviate many symptoms of perimenopause, its effectiveness in promoting weight loss is more complex.
Insulin Resistance: A Key Factor in Weight Gain
Insulin resistance is a condition where the body’s cells become less responsive to insulin, a hormone that regulates blood sugar levels. This leads to higher levels of insulin in the blood, which can cause weight gain, particularly around the abdomen. During and after perimenopause, women are more vulnerable to developing insulin resistance due to hormonal changes.
Hormones and Insulin Sensitivity
Estrogen plays a crucial role in maintaining insulin sensitivity. As estrogen levels decline during perimenopause, the risk of insulin resistance increases. Lower estrogen levels can disrupt the normal function of insulin, making it harder for your body to use glucose for energy. This can lead to higher blood sugar levels and increased fat storage.
The Muscle-Fat Dynamic
Our bodies are always in a state of flux, either building muscle and losing fat or losing muscle and gaining fat. This dynamic becomes more pronounced after age 40, when muscle mass naturally declines. Maintaining or increasing muscle mass is essential for counteracting this trend.
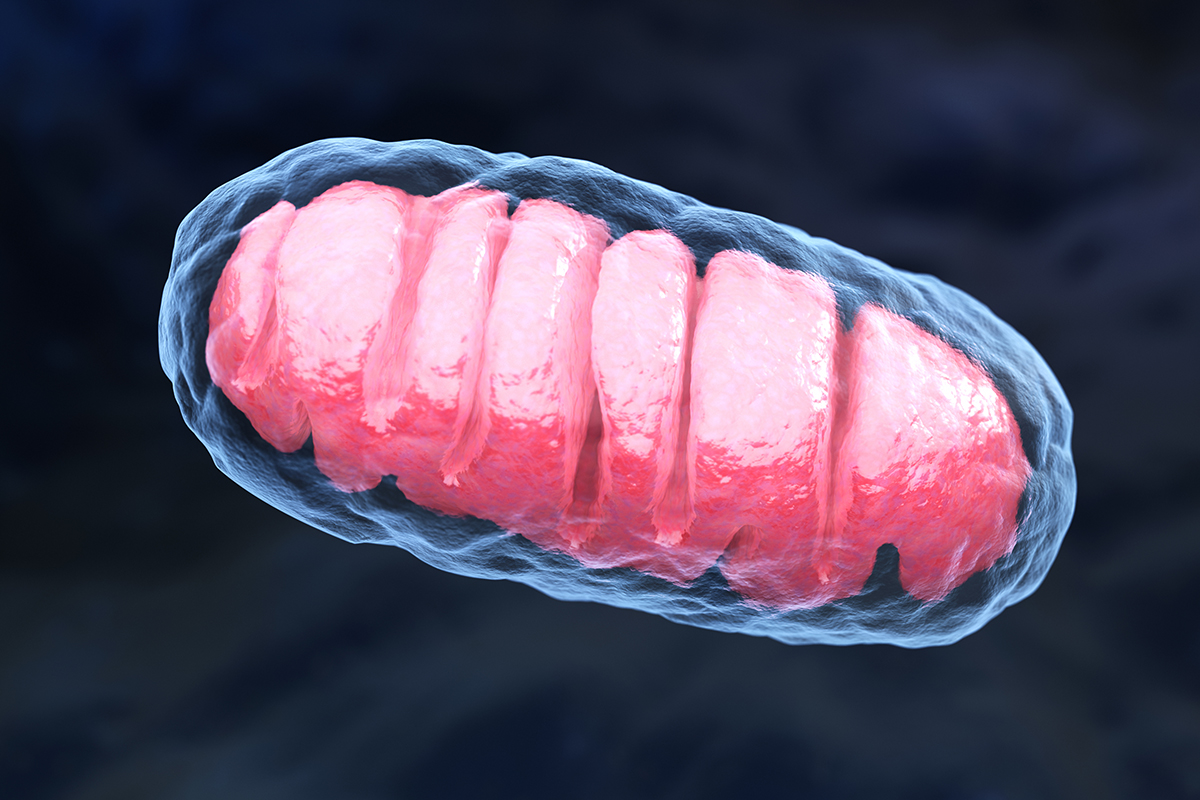
Muscle Mass and Metabolism
Muscle tissue has more mitochondria – the powerhouses of our cells – than fat tissue. More mitochondria mean higher metabolic activity, which is crucial for burning calories and maintaining a healthy weight. However, for mitochondria to function well, they need proper nutrient co-factor and antioxidant levels and a healthy lifestyle.
Muscle and Insulin Receptors
Muscle cells have more insulin receptor sites than fat cells because they require more glucose to fuel skeletal activity. More muscle mass increases insulin sensitivity, allowing your body to utilize glucose more efficiently rather than storing it as fat. This is why building and maintaining muscle is so important, especially as we age.
Protein: The Building Block of Muscle
Protein is essential for preserving muscle mass, which is crucial for maintaining a healthy metabolism. As estrogen levels drop, the body tends to lose muscle mass more quickly. Ensuring adequate protein intake can help counteract this loss. Aim for 1 gram of protein per pound of body weight (or target body weight if more than 20 pounds over your ideal weight). This amount supports muscle maintenance and growth, crucial for boosting metabolism and improving insulin sensitivity.
How to Distribute Protein Intake
To maximize muscle protein synthesis, it’s best to distribute your protein intake evenly throughout the day. Aim for 4-5 meals, each containing roughly 20-30 grams of protein. Here’s an example of how you can split this up:
- Breakfast: Greek yogurt with berries and nuts (20-25 grams)
- Mid-Morning Snack: Protein shake or a handful of almonds (20 grams)
- Lunch: Grilled chicken salad with mixed greens and quinoa (25-30 grams)
- Afternoon Snack: Cottage cheese with sliced cucumber (20 grams)
- Dinner: Baked salmon with roasted vegetables and sweet potato (30 grams)
Carbohydrate Intake: Quality and Quantity
As we age, our bodies often become less efficient at utilizing carbohydrates due to a decline in insulin sensitivity and mitochondrial function. This means we may need to adjust our carbohydrate intake to avoid storing excess glucose as fat. However, this doesn’t mean eliminating carbs entirely. Instead, focus on the quality and quantity of carbs you consume, eating them with fiber, and with protein.
Adjusting Carbs for Your Needs
Everyone’s body is different, and genetic factors play a role in how we metabolize carbohydrates. While some may tolerate higher carb intake, others may need to reduce their intake to maintain a healthy weight. Here are some tips to help you adjust your carb intake:
- Choose Complex Carbs: Opt for whole grains, legumes, fruits, and vegetables over refined sugars and processed foods.
- Monitor Portions: Pay attention to portion sizes to avoid overeating carbs.
- Balance with Protein and Fats: Pair carbohydrates with protein and healthy fats to slow digestion and promote stable blood sugar levels.
- Increase Activity: Regular exercise and building muscle mass can help improve insulin sensitivity and allow you to utilize carbohydrates more efficiently. In particular, eating carbohydrates just before or just after exercise, helps your body utilize them instead of storing them as fat.
Time for a Transformation
Understanding these concepts is powerful, but real transformation happens when you put this knowledge into action. This is where the Reverse-Age Method shines. With a proven track record of 20 years in hormone management and creating actionable, step-by-step plans, we ensure you’re not just learning but living these principles. Testing can show us exactly what support you need for gut health, liver detoxification, nutrient replacement, and mitochondrial optimization. Let us guide you through a customized approach designed for your success. Join our free Reverse-Age Method Masterclass to start your journey towards lasting change.
Mitochondria: The Powerhouses of Your Cells
Mitochondria are the energy factories of your cells, converting nutrients into energy. During perimenopause, mitochondrial function can decline, contributing to fatigue and weight gain. Optimizing mitochondrial function is crucial for maintaining a healthy metabolism.
Nutrients for Mitochondrial Health
Certain nutrients are essential for mitochondrial function, including:
- Coenzyme Q10 (CoQ10): This antioxidant helps produce energy in the mitochondria.
- Magnesium: Vital for over 300 biochemical reactions in the body, including energy production.
- B-Vitamins: Essential for energy metabolism and red blood cell formation.
- Alpha-Lipoic Acid: An antioxidant that helps turn glucose into energy.
Lifestyle Factors
In addition to diet, several lifestyle factors can support mitochondrial health:
- Regular Exercise: Physical activity enhances mitochondrial function and promotes the formation of new mitochondria.
- Adequate Sleep: Quality sleep is essential for mitochondrial repair and energy production.
- Stress Management: Chronic stress can impair mitochondrial function. Practices like meditation, yoga, and deep breathing can help mitigate stress.
Gut Health: The Foundation of Wellness
The gut microbiome plays a crucial role in overall health, including weight management. An imbalance in gut bacteria can lead to inflammation, insulin resistance, and weight gain.
Probiotics and Prebiotics
- Probiotics: These beneficial bacteria can improve gut health and aid in weight management. Foods rich in probiotics include yogurt, kefir, sauerkraut, kimchi, and other fermented foods.
- Prebiotics: These are non-digestible fibers that feed the beneficial bacteria in your gut. Sources include garlic, onions, leeks, artichokes, asparagus, and bananas.
Gut-Brain Axis
The gut-brain axis is the communication network between your gut and brain. Imbalances in gut bacteria can affect this connection, influencing mood, appetite, and overall well-being.
Muscle Mass: The Metabolism Booster
Muscle mass is directly linked to metabolic rate – the more muscle you have, the more calories you burn at rest. As women age, muscle mass naturally declines, which can slow metabolism and contribute to weight gain.
Strength Training
Incorporating strength training into your exercise routine is essential for preserving and building muscle mass. Aim for at least two to three sessions per week, focusing on all major muscle groups.
Protein and Muscle Synthesis
As mentioned earlier, adequate protein intake is crucial for muscle maintenance and growth. Consuming protein-rich foods within 30 minutes of a workout can enhance muscle protein synthesis.
Integrating It All: A Holistic Approach
HRT can alleviate many symptoms of perimenopause and menopause, increase longevity by up to 21%, and is the platform for getting the change in body composition that you want….but it is not a magic bullet for weight loss. A holistic approach that includes a menopause-specific diet plan, the right kind of exercise, stress management, and proper sleep is essential for optimal health and weight management.
Personalized Nutrition and Lifestyle
Every woman’s body is different, and a personalized approach is key to achieving and maintaining a healthy weight. Functional medicine testing can help identify imbalances and tailor a nutrition and lifestyle plan to your specific needs.
Detoxification and Antioxidants
Supporting the body’s natural detoxification processes and ensuring adequate antioxidant intake can help reduce oxidative stress and support weight management. Foods rich in antioxidants include berries, leafy greens, nuts, and seeds.
Hydration
Staying hydrated is essential for overall health and can aid in weight management by promoting a feeling of fullness and supporting metabolic processes. Aim for at least eight glasses of water per day, more if you’re physically active.
Ready to Put This Into Action?
Knowing what to do is one thing, but putting it into action and following through is where the magic happens. That’s where the Reverse-Age Method comes in. With over 20 years of experience in managing hormone therapy and crafting simple, actionable step-by-step plans, we sequence everything for your success. Functional testing can pinpoint the exact areas where you need support, whether it’s gut health, liver detoxification, nutrient replenishment, or mitochondrial optimization. This isn’t just about knowledge – it’s about transformation. Watch my Reverse-Age Method Masterclass to learn how we can help you turn these insights into real results.
The Ultimate Guide to Intermittent Fasting for Women: Balancing Hormones and Boosting Health at Every Age
Intermittent fasting (IF) is all the rage these days, but let’s be real: what works for men doesn’t always cut it for us women. Whether you’re cycling, navigating perimenopause, or enjoying your post-menopausal years, the impact of IF on your body can vary. Let’s dive into the research and see how IF can fit into our lives at different stages, without messing up our hormonal harmony.
Intermittent Fasting and Pre-Menopausal Women
When you’re pre-menopausal and still cycling, intermittent fasting can offer some great benefits. It can help with weight management, improve insulin sensitivity, and boost cardiovascular health. Think of it as a way to reset your metabolism and give your body a break. Improved insulin sensitivity means better blood sugar control, reducing the risk of type 2 diabetes, which is always a win. Plus, say hello to improved lipid profiles and reduced inflammation – your heart will thank you.
But here’s the catch: our hormonal balance is delicate, and IF might mess with your menstrual cycle, decrease fertility, and cause other hormonal issues. Our bodies are complex, and sometimes they don't appreciate the extra stress. Timing is everything. During the follicular phase (the first half of your cycle), fasting might feel manageable. But in the luteal phase (the second half), it can spike stress hormones and make PMS worse.
And if you’re trying to conceive? It’s best to steer clear of fasting altogether. Your body needs all the support it can get during this time, and fasting can be an unnecessary stressor. We also have higher nutrient needs, especially when we're cycling, so fasting can lead to deficiencies if we’re not careful.
Intermittent Fasting and Perimenopausal Women
Perimenopause is already a rollercoaster, and adding fasting into the mix can sometimes feel like throwing fuel on the fire. While hormonal changes during perimenopause often bring weight gain, IF can help manage this and keep your metabolism humming. Improved insulin sensitivity and reduced inflammation can ease the transition through this phase.
However, fasting can also ramp up stress hormones like cortisol, making symptoms like hot flashes and mood swings worse. This period of our lives is one of relative hormone fragility, and fasting beyond 12-13 hours can be a stressor that provokes cortisol spikes. These spikes can further aggravate pre-existing hormone imbalances, like low progesterone, leading to worse symptoms.
Responses to fasting vary widely among perimenopausal women. For some, fasting exacerbates symptoms, while others might find relief. It’s all about tuning in to your body and adjusting accordingly. If you decide to try IF, start slowly and pay close attention to how you feel.
Intermittent Fasting and Post-Menopausal Women
Post-menopausal women often face weight gain, and intermittent fasting can be a game-changer here. Once menopause is behind you, your body may handle fasting better, and it can be a powerful tool for maintaining health. Improved insulin sensitivity, reduced inflammation, and better lipid profiles help lower the risk of diabetes, heart disease, and certain cancers.
But we can’t forget about bone health. Post-menopausal women are at higher risk for osteoporosis, so it’s crucial to ensure you're getting enough calcium, vitamin D, and other nutrients. Maintaining muscle mass is also vital for metabolic health and functional strength, so make sure you're consuming enough protein during your eating windows. A good rule of thumb is to aim for 1 gram of protein per pound of your target body weight each day.
Most post-menopausal women can benefit from a minimum of 13 hours of fasting daily, but you can personalize the duration to suit your goals and how you feel. Whether it’s 13 hours or a bit longer, the key is consistency and ensuring you’re hitting your nutrient goals during your eating windows.
Acknowledging the Research Gap
It’s important to note that most studies on intermittent fasting have been conducted on men. Many of these studies intentionally excluded women, especially those of reproductive age, due to the confounding results researchers anticipated. This means that the unique physiological responses of women to fasting are often underrepresented in the literature.
To Fast or Not To Fast?
Intermittent fasting can offer numerous health benefits, but it's essential to tailor your approach based on your reproductive stage and individual needs. Pre-menopausal women should be mindful of their cycles and nutrient requirements, and avoid fasting if trying to conceive. Perimenopausal women need to be cautious of the stress fasting can place on their already fragile hormonal balance. For post-menopausal women, IF can be a fantastic tool for maintaining health, as long as you ensure you're meeting your nutrient needs, particularly protein.
Start with shorter fasting periods and adjust based on your body's feedback. Always consult with a healthcare provider before making significant changes to your diet or fasting routine. Remember, your body knows best – listen to it, nourish it, and take steps that make you feel strong and vibrant.
Supporting Studies
- **Melby, A. D., et al.** "Intermittent Fasting in Women: Current Research and Application." *Journal of Women’s Health*, 2020.
- **Varady, K. A., et al.** "Impact of Intermittent Fasting on Reproductive Hormones and Ovulatory Function in Healthy Women." *American Journal of Clinical Nutrition*, 2017.
- **Atkinson, F. S., et al.** "Effects of Intermittent Fasting on Health Markers in Perimenopausal Women." *Menopause*, 2019.
- **Riedlinger, J. A., et al.** "Intermittent Fasting and Bone Health in Post-Menopausal Women." *Osteoporosis International*, 2018.
- **Racette, S. B., et al.** "Comparative Study of Intermittent Fasting and Continuous Caloric Restriction in Women." *Obesity*, 2016.
- **Weaver, S. J., et al.** "Intermittent Fasting and Its Effects on Hormonal Balance in Women." *Endocrinology*, 2021.
Should I Follow a Plant-Based Diet During Perimenopause and Menopause?
As a health professional working with women in perimenopause and menopause, I’ve seen firsthand how diets that once seemed ideal—like veganism and vegetarianism—start to present new challenges. Many women who previously thrived on these diets begin to struggle with body composition, weight gain, mood, sleep, brain function, and even the severity of hot flashes and night sweats.
The Perimenopause Challenge: Carbohydrate Tolerance and Protein Sources
One of the primary issues is carbohydrate tolerance. During perimenopause and menopause, hormonal shifts—especially the decline in estrogen and progesterone—make 100% of us less sensitive to insulin, rendering us less capable of utilizing the same amount of daily carbohydrate. This makes it harder to manage blood sugar levels. Vegan and vegetarian diets, rich in plant-based proteins, come with a high carbohydrate load. While lentils, beans, and grains provide necessary protein, they also contribute significant carbohydrates, which can exacerbate blood sugar swings and insulin resistance.
The Science Behind It
Studies have shown that women in perimenopause and menopause experience a natural decline in insulin sensitivity due to hormonal changes. Estrogen plays a crucial role in maintaining insulin sensitivity, and its decline can lead to increased blood sugar levels and fat storage, particularly around the abdomen. This makes it essential to adjust carbohydrate intake and focus on balanced macronutrients.
*Fact**: Research has found that high carbohydrate intake can worsen hot flashes and night sweats due to its impact on blood sugar regulation and insulin levels.
Protein Recommendations and Carbohydrate Balance
To support optimal health and body composition during perimenopause and menopause, it’s recommended that women consume 1 gram of protein per pound of target body weight. This high protein intake is crucial for maintaining muscle mass, supporting metabolic health, and preventing weight gain. However, achieving this protein goal with plant-based sources can be challenging without significantly overshooting carbohydrate intake.
**Example**: To meet a target of 140 grams of protein per day, a woman might need to consume large amounts of lentils, beans, and grains, which would also add a considerable amount of carbohydrates, potentially leading to fat storage and metabolic issues.
The Omega Dilemma: Inflammation and Fatty Acid Balance
Another critical aspect is the balance of omega fatty acids. Plant-based diets often rely on nuts and seeds for protein, which are high in omega-6 fatty acids. While these are necessary for health, an imbalance with omega-3 fatty acids can promote inflammation. This is particularly problematic during perimenopause and menopause, as these stages are already associated with increased inflammatory responses due to hormonal shifts.
Estrogen Decline and Inflammation
Estrogen helps regulate inflammation by modulating cytokine production. As estrogen levels drop, there is an upregulation of pro-inflammatory cytokines, leading to increased inflammation. This can manifest in various ways, from chronic disease risk to visible signs of aging, joint pain, and slower connective tissue repair. Consequently, women in this stage of life are more prone to injuries and aches in the knees, back, shoulders, and other joints.
**Fact**: Lower estrogen levels are linked to higher levels of inflammatory markers like CRP and IL-6, which contribute to chronic inflammation and related health issues.
Practical Solutions and Adjustments
1. Reducing Carbohydrate Intake
Women in perimenopause and menopause should consider reducing their overall carbohydrate intake compared to their younger years. This helps manage weight and prevent insulin resistance. Focus on low glycemic index (GI) foods, which release glucose slowly and help maintain stable blood sugar levels.
2. Diversifying Protein Sources
Incorporate a variety of vegan protein sources, such as pea, hemp, and rice protein powders, to avoid excessive carbohydrate intake. These sources provide concentrated protein without the high carb load.
3. Balancing Omega Fatty Acids
To maintain a healthy omega-3:6 ratio, consider incorporating omega-3 supplements, such as algal oil. This helps counteract the inflammatory effects of omega-6 fatty acids prevalent in nuts and seeds.
4. Prioritizing Anti-Inflammatory Foods
Focus on anti-inflammatory foods like leafy greens, berries, and flaxseeds. These foods can help mitigate the increased inflammatory response during perimenopause and menopause.
Conclusion: Meeting You Where You Are
As a practitioner, my goal is to meet you where you are and provide the most effective strategies for your unique needs. While veganism and vegetarianism can be more challenging during perimenopause and menopause, with thoughtful adjustments and a focus on balanced nutrition, you can continue to thrive. Understanding and managing these dietary challenges can lead to improved body composition, better mood, enhanced brain function, and a reduction in hot flashes and night sweats.
By addressing these issues head-on, we can navigate this transformative stage with grace and vitality.
Sources
Carbohydrate Intake and Vasomotor Symptoms: Thurston, R. C., Sowers, M. R., Sutton-Tyrrell, K., Everson-Rose, S. A., Lewis, T. T., & Edmundowicz, D. (2011). Abdominal adiposity and hot flashes among midlife women. Menopause, 18(6), 726-733. doi:10.1097/gme.0b013e318204a94b
Estrogen and Insulin Sensitivity: Carr, M. C. (2003). The emergence of the metabolic syndrome with menopause. The Journal of Clinical Endocrinology & Metabolism, 88(6), 2404-2411. doi:10.1210/jc.2003-030242
Omega-3 and Omega-6 Fatty Acid Balance: Simopoulos, A. P. (2002). The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & Pharmacotherapy, 56(8), 365-379. doi:10.1016/S0753-3322(02)
Groundbreaking Study Shatters Myths About Hormone Replacement Therapy for Women Over 65
Menopause symptoms don’t magically disappear as we age. In fact, many women continue to struggle with them well into their 60s, 70s, and beyond. Yet, family practice physicians, OB/GYNs, and primary care doctors often hesitate to prescribe hormone replacement therapy (HRT) to women over 65. Age is frequently seen as a barrier to HRT use, but emerging studies prove this thinking is outdated. Let’s dive into the latest research and discuss why HRT is not just safe, but essential for older women who want to safeguard their health and longevity.
The Persistent Impact of Menopause Symptoms
As women, we spend up to ½ our lives in a menopausal state. Arriving at menopause doesn't always end the discomfort of hot flashes, night sweats, and insomnia. In many cases, they remain as intense or even worsen. This ongoing discomfort can affect mental health, physical health, and overall well-being. Symptoms like vaginal dryness, sexual discomfort, and urinary issues often escalate over time. These symptoms can persist for decades, significantly impacting quality of life.
A client of mine named Carol, age 59, had struggled with osteoporosis and other menopausal symptoms for three years while trying to find a provider willing to prescribe HRT, when we first met. Misconceptions about the risks and benefits of HRT for older women create unnecessary hurdles for Carol and countless others.
Breaking Down the Latest Research
In April of 2024, a groundbreaking study involving over 10 million US women aged 65 and older, recently published in the journal Menopause, provided new insights into the effects of HRT on older women. This was the largest study ever run on women taking hormone replacement therapy, and it is significant that it was conducted by the NIH and the National Library of Health. Contradictory to popular belief, this research highlights significant benefits and minimal risks associated with continued HRT use.
Estrogen Therapy: A Game-Changer in Cancer Prevention
Key Findings from the Study:
- Longevity: Women taking estradiol alone experienced a 21% decrease in all-cause mortality compared to those not on HRT. That’s a 21% lower death rate from any cause!
- Cancer Protection: Estrogen therapy statistically reduced the risk of five cancers—breast, ovarian, uterine, lung, and colorectal.
- Heart and Cognitive Health: Estrogen therapies reduced the risk of severe heart issues (like congestive heart failure, venous thromboembolism, atrial fibrillation, and acute myocardial infarction) and cognitive issues, including dementia.
Estrogen use statistically reduced the risk of all cancers studied, including breast cancer. Every form of estrogen therapy was protective against breast cancer.
Delivery Methods Matter
Older women did best with topical and vaginal deliveries of estrogen, with vaginal delivery being the ultimate best. Both methods effectively protected against breast cancer and supported brain health without the increased stroke risk seen with oral estrogen. Oral estrogen had a slight increased risk of ischemic stroke but offered the best breast protection.
Addressing Breast Cancer Concerns
The study showed that all forms of estrogen therapy were protective against breast cancer. However, combining estrogen with synthetic progestins increased the risk of breast cancer by 19%, while combining it with natural progesterone (oral) only increased the risk by 10%. Notably, lower dosages and vaginal delivery of estrogen did not show any increased risk of breast cancer in any study. Topical bioidentical progesterone showed no increase in risk of cancer alone or with estrogens.
Additional Findings
- Progesterone Use: Bioidentical Progesterone, when used alone, was associated with a 10% reduction in breast cancer risk, but progestin (synthetic) increased the risk by 21%.
- Lung Cancer: Progesterone was associated with a 19% reduced lung cancer risk, while progestin was associated with a 14% increased risk.
- Multiple Benefits: The study highlighted reduced risks of three cancers (breast, lung, and colorectal), four cardiovascular conditions (congestive heart failure, venous thromboembolism, atrial fibrillation, and acute myocardial infarction), and dementia with estrogen replacement or combined estrogen and progesterone replacement. .
Estrogen Therapy Beyond 65
Perhaps the most profound finding was that the use of estrogen therapy beyond age 65 was associated with a significant 19% reduction in mortality from any cause.
Older women on estrogen therapies lived statistically longer and healthier lives.
The Women's Health Initiative: Correcting the Record
The Women’s Health Initiative (WHI) was the original study that created widespread, undeserved alarm by falsely correlating estrogen use to breast cancer due to misinterpreted data and flawed study design. The study was not designed to look at cancer risk– it was originally designed to look at the impact of hormone replacement on cardiovascular risk, and examined only synthetic hormones. The study didn’t control for factors like smoking, past hormone use, and other risk factors compared to the test group, and also didn’t distinguish prior use of synthetic hormones like progestins–now known to be a risk factor for cancer. Subsequent reanalysis and the WHI post-intervention study reported a significant 21% decreased risk of breast cancer with conjugated equine estrogen alone and a 28% increase with conjugated equine estrogen plus medroxyprogesterone (synthetic progestins), giving credence to our current understanding.
Author's Conclusions: Groundbreaking Findings
Here’s what the authors of the 10 million women study concluded: "Our study suggests the possibility of important health benefits with use of menopausal HT beyond age 65 years."
"The use of Estrogen therapy can protect against risks of all-cause mortality, developing cancers (breast, lung, and colorectal), congestive heart failure, venous thromboembolism, atrial fibrilation, acute myocardial infarction (heart attack), and dementia."
The study also noted that the use of combined estrogen and progestin therapy does not increase risks for almost all conditions but does increase the risk of breast cancer. However, low doses of transdermal and vaginal estrogen/progesterone combination therapy (especially E+ bioidentical progesterone) can mitigate this risk. In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (bioidentical estradiol) rather than Conjugated Equine Estrogren (synthetic) as emphasized by others.
Conclusion
Women over 65 are still experiencing hot flashes and other menopause symptoms. Turning 65 doesn’t mean these symptoms magically disappear or that women no longer need hormone optimization. Going without hormones from the onset of menopause for 10-15 years or longer may allow serious health risks to increase, especially for cardiovascular disease and osteoporosis. Seeking trained, experienced hormone optimization specialists is essential in order to get help from practitioners who understand the nuances of hormones and health risks and how to navigate them effectively. The latest findings offer a hopeful and potentially life-changing perspective. Working with an informed practitioner who understands the science and delivery methods can help you navigate the best options for your health and longevity.
FAQs
What is hormone optimization?
Hormone optimization is the process of ensuring that hormone levels aren’t too high or too low but are “just right.” Just-right hormone levels reduce or eliminate menopause symptoms (some of which can persist for decades) and reduce long-term health risks (like heart disease and osteoporosis).
Is it safe to start HRT after 65?
Absolutely. A study involving 10 million women on HRT showed that HRT past 65 is not only safe but essential for a longer, healthier life.
When should women start HRT?
While the recent study focused on women aged 65 and older to highlight the benefits of HRT later in life, other research indicates that starting HRT earlier can offer additional advantages, particularly for brain health. Studies show that beginning HRT during the perimenopausal transition, specifically five or more years before actual menopause, can significantly reduce the risk of Alzheimer's disease by 50%. This brain-protecting effect diminishes once a woman reaches menopause, emphasizing the importance of timely intervention. The earlier you start, the greater the benefits, and longer use helps mitigate progressive issues like changes in brain volume, heart risk, and bone loss. Additionally, starting HRT early can help prevent the weight gain often associated with perimenopause when combined with appropriate nutrition and exercise. By initiating HRT before menopause, women can not only alleviate menopausal symptoms but also safeguard their cognitive health and overall well-being for the future.
References
- Menopause. "Use of menopausal hormone therapy beyond age 65 years and its effects on women's health outcomes by types, routes, and doses." PubMed
- Brinton, R. D. "Association of Hormone Therapy With Risk of Alzheimer Disease in Women." JAMA Neurology
- Jensen, L. B., Vestergaard, P., Hermann, A. P., Gram, J., Eiken, P., Abrahamsen, B., Brot, C., Kolthoff, N., Sørensen, O. H., Beck-Nielsen, H. "Hormone Replacement Therapy Dissociates Fat Mass and Bone Mass, and Tends to Reduce Weight Gain in Early Postmenopausal Women: A Randomized Controlled 5-Year Clinical Trial of the Danish Osteoporosis Prevention Study."
- Yüksel, H., Odabaşi, A. R., Demircan, S., Karul, A., Kozaci, L. D., Köseoğlu, K. "Effects of oral continuous 17β-estradiol plus norethisterone acetate replacement therapy on abdominal subcutaneous fat, serum leptin levels and body composition." Pages 381-387 | Received 12 Dec 2005, Accepted 05 Jun 2006, Published online: 07 Jul 2009.
- Gambacciani, M., Ciaponi, M., Cappagli, B., Piaggesi, L., De Simone, L., Orlandi, R., Genazzani, A. R. "Body Weight, Body Fat Distribution, and Hormonal Replacement Therapy in Early Postmenopausal Women." The Journal of Clinical Endocrinology & Metabolism, Volume 82, Issue 2, 1 February 1997.
- Espeland, M. A., Stefanick, M. L., Kritz-Silverstein, D., Fineberg, S. E., Waclawiw, M. A., James, M. K., Greendale, G. A. "Effect of Postmenopausal Hormone Therapy on Body Weight and Waist and Hip Girths." The Journal of Clinical Endocrinology & Metabolism, Volume 82, Issue 5, 1 May 1997.
Solutions for a Thriving Sex Life: Vaginal Dryness and Low Libido During Perimenopause🔥💜
Perimenopause, the years leading up to menopause, can sneak up on you and throw your sex life for a loop. You might start noticing some changes down there, like dryness, irritation, or discomfort during sex. And let's be real, it's not exactly a topic that comes up often in casual conversation, leaving many of us feeling alone and unsure of what to do.
I can't tell you how many women have confided in me about their concerns over their dwindling sex drive and how it's impacting their relationships. They love their partners to pieces and are happy in their marriages, but that urge to rip each other's clothes off just isn't there like it used to be. When things do get steamy, it can be harder to get turned on, and even when you do, orgasms might feel like a pale imitation of their former glory. If you're nodding along right now, trust me, you're not the only one, and there are plenty of solutions to help you get your groove back.
First things first, let's get one thing straight: your pleasure and comfort should never take a backseat. You deserve to feel sexy, satisfied, and fulfilled, no matter where you are in life. And the good news is, there are tons of tools and techniques out there to help you do just that. When you make your sexual well-being a priority and embrace pleasure, it can have an amazing ripple effect on every part of your life – your relationships, family, career, and how you feel about yourself.
So, where do you even begin? Allow me to introduce you to some game-changers that are backed by science.

If you're looking to give your vaginal health a boost, Joylux is definitely worth checking out. This innovative device uses LED light therapy, sonic vibration, and therapeutic warmth to rejuvenate vaginal tissue, increase natural lubrication, enhance sexual pleasure, and give your confidence a major boost. Plus, a study in the Journal of Cosmetic and Laser Therapy found that low-level light therapy significantly improved vaginal health in postmenopausal women by increasing collagen production and promoting tissue regeneration. Pretty cool, right?
So how does shining light where the sun doesn't shine, work, exactly? By encouraging the growth of new capillaries, Joylux boosts blood flow, sending a surge of nourishing nutrients to tissues that need it most. The soothing warmth of the device relaxes you while stimulating circulation, reaching a comfy 42°C (108°F) during the 12-minute session. Joylux also kickstarts collagen production, helping to restore elasticity and natural lubrication to your vaginal walls.
Most women start noticing changes within just 3 weeks of consistent use, with the full "wow" effect hitting around the 6-8 week mark. To keep those good vibes going, maintenance sessions 1-2 times a week are all you need.
Now, let's talk options. Joylux comes in two flavors: the standard Vfit Gold and the souped-up Joylux Plus. The Plus model takes things to the next level with: A full 12-minute session 32% more power for faster results A variety of vibration patterns to customize your comfort While both models deliver the goods, the Plus is like the first-class ticket to vaginal rejuvenation. Best part? When you buy through a medical professional or use our special affiliate code, you'll get the Joylux Plus with the programming upgrade included – a $99 value, on the house! Just get in touch with us for the code and the scoop on the free perks. 💡So, are you ready to shine a light on your intimate health? With Joylux, you can rediscover the joy of comfort, confidence, and satisfaction in the bedroom and beyond. Your vagina deserves this – trust us. 💎 Order Joylux devices here.

For those of you who want to tone up your pelvic floor (and trust me, you do), Perifit is a smart little device that connects to an app, turning pelvic floor exercises into a game.
It syncs up with an app on your phone, transforming those sometimes tedious kegels into interactive challenges that'll have you eager to crush your high score. But Perifit isn't just about fun and games – it's a serious tool for boosting your pelvic health. A strong, toned pelvic floor is like a secret superpower for your lady bits.
It can:
👍Improve bladder control (helpful when jumping on trampolines with your kids!)
👍Reduce the risk of pelvic organ prolapse
👍Rev up your sexual function by increasing blood flow and sensitivity in all the right places
And the best part? You'll actually look forward to your pelvic floor sessions–and do them. No more setting reminders or forcing yourself to do those exercises – with Perifit, you'll be jumping at the chance to level up your strength and have a blast doing it. It's time to say goodbye to the days of lackluster kegels and hello to a revolutionary approach to pelvic health. Perifit isn't just a device – it's a game-changer. It's your personal trainer, your cheerleader, and your secret weapon all rolled into one adorably addictive little package.The more you play, the stronger your pelvic floor gets, which can lead to better bladder control, increased sexual sensations, and improved intimate wellness overall. And if you need more convincing, a 2018 study in the Journal of Sexual Medicine found that pelvic floor muscle training significantly improved sexual function in women with pelvic floor disorders.

When it comes to toys, not all are created equal. These little bundles of joy can take our solo or partnered play to a whole new level, but did you know that not all toys are created equal? A 2006 study by the Danish Environmental Protection Agency found that many sex toys contained harmful chemicals like phthalates, which can mess with your hormones and cause irritation. No, thank you. Many conventional sex toys contain sneaky chemicals like BPA, phthalates, TPE, fake silicone, and other toxins that can leach into our delicate vaginal tissue. And trust me, that's not the kind of "tingling sensation" we're looking for!
These chemicals can mimic estrogen in our bodies, throwing our endocrine system out of whack and potentially leading to some seriously uncool reproductive health issues.
But don't worry, you don't have to kiss your beloved buzzing besties goodbye! There are plenty of body-safe options out there that prioritize your pleasure AND your health. Brands like Lelo, Fun Factory, and Dame offer a tantalizing array of toys made from medical-grade silicone, ensuring safety and sustainability without sacrificing any of the toe-curling goodness.
So, how can you tell if a toy is safe? Look for materials like:
👉Medical-grade silicone
👉Borosilicate Glass
👉Stainless steel
These non-porous materials are easy to clean and won't hang onto any icky bacteria or toxins that could crash your pleasure party. Order here.

If you're looking for a luxurious way to pamper your lady bits, Julva, a vulvar cream containing DHEA, could be your new best friend. We'll spend hundreds of dollars on creams and serums for our face and body, but when it comes to our most intimate area, we tend to neglect it. That's where Julva comes in – it's like a daily dose of nourishment for your delicate vulvar skin and vaginal canal. This luxurious cream is packed with DHEA, a hormone precursor that our bodies naturally convert into estrogen and testosterone right where we need it most.
Julva helps by:
👉Boosting moisture levels
👉Improving skin resilience
👉Enhancing sensitivity
👉Less dryness and irritation
👉More comfort during sex and daily life
👉Increased sensation and orgasmic potential
Julva is all-natural, hormone-free, and backed by scientific research. It's like giving your vulva a superfood smoothie, but without the kale-in-your-teeth part (joking). It can help restore moisture, improve skin texture, enhance sensation, and increase intimate comfort. A 2018 pilot study in the Journal of Drugs in Dermatology found that daily application of a DHEA-containing cream significantly improved vaginal dryness, irritation, and discomfort in postmenopausal women. Order Julva here

And if you really want to bring out the big guns, AnteAGE VRS, a cutting-edge serum containing growth factors derived from stem cells, can help revitalize aging vaginal tissue at the cellular level. This powerhouse product can rejuvenate vaginal tissue, increase lubrication, enhance sexual sensation, and improve overall vaginal health. A 2019 study in the Journal of Clinical Medicine found that stem cell-derived growth factors significantly improved vaginal health in postmenopausal women, including increased epithelial thickness, reduced pH, and enhanced lubrication. Please contact [email protected] to order AnteAGE VRS.
If dryness, low sensation, and discomfort are putting a damper on your sex life, allow me to introduce: low-dose vaginal estrogen. 🙌 This little miracle worker comes in the form of a transdermal gel, creams, or suppositories , and it's like a targeted moisture bomb for your V. By delivering a dose of estriol and estradiol right where you need it most, vaginal estrogen can:
💃Restore thickness and elasticity to vaginal walls
💃Boost natural lubrication (goodbye, sandpaper sensation!)
💃Reduce irritation and discomfort
💃Make sex feel amazing again (hallelujah!)
And the best part? If you look back at my reel from last week, you’ll see that the most current data clearly demonstrates that estrogen replacement reduces your risk of 5 types of cancers, including breast cancer, and also increases longevity in women.
Now, I know what you're thinking – "But isn't estrogen therapy risky?" Well, when it comes to vaginal estrogen, the doses are really low. And when managed by a trained practitioner who knows how to optimize your hormone receptors and make sure you’re metabolizing hormones correctly, estrogen can help keep your brain, your bones, your cardiovascular system, and your metabolism on lock– for life. So, if you're battling with menopausal symptoms don't suffer in silence. Let’s talk about if vaginal estrogen is right for you. Your vagina (and your sex life) will thank you. These topical hormones work by restoring vaginal tissue thickness and elasticity, and a 2019 meta-analysis in JAMA Internal Medicine concluded that vaginal estrogen therapy effectively treated vaginal symptoms in postmenopausal women, with minimal systemic absorption.
This is just one aspect of the work I do with women in perimenopause. In my Reverse-Age Method 6-month group program, I utilize a proprietary science-backed 3-step system that I call Balance (hormones), Clear (gut health and cellular detoxification), and Empower (mitochondrial optimization and muscle as medicine). This lab-based program includes personalized nutrition and personal training programs, as well as bespoke custom protocols for each of the three systems, tailored to the specific needs of each woman. In addition to addressing weight gain, skin aging, energy/mood/brain issues, and hormone symptoms like flashes, sweats, and crazy periods, libido and sexual wellness are never put on the back burner in this program!
If you're interested in learning more about the Reverse-Age Method or my Hormone Balance Quick Start program (a 3-month, lower-investment option), I encourage you to book a discovery call with me. Together, we can explore how these programs can help you reclaim your vitality, confidence, and passion for life.
At the end of the day, this journey is all about reconnecting with your body, your pleasure, and your inherent sexual power. It's about having open, honest conversations about vaginal well-being and refusing to settle for anything less than the mind-blowing intimacy you deserve.
So go ahead and explore these transformative tools, knowing that they're grounded in scientific research and designed with your unique needs in mind. Play around and discover what works best for your body and desires. And remember, you're not alone in this. By prioritizing your pleasure and intimate well-being, you can tap into a whole new level of confidence, energy, and fulfillment in every aspect of your life.
Is Perimenopause Impacting Your ADHD? Unraveling the Cognitive Connection
Did you just reread that title 3 times? Then read on, this one’s for you! 😜
Introduction: Angela's Journey
Meet Angela, a 45-year-old marketing director renowned for her sharp focus and meticulous work ethic, who recently began noticing unsettling changes in her cognitive functions.
"Let me tell you, it's been quite the shift," she tells me. "I used to have my mornings down to a science, but now, it's like I'm always scrambling for my keys, which I've misplaced yet again. And it's not just annoying—it really throws off my whole schedule since I end up running late."
"And meetings? I used to be the one leading the charge, but lately, I stumble over my words, my thoughts scattering like marbles. It's these little things... they're adding up, you know?" she pauses, collecting my thoughts. "I've been dealing with ADHD for years, but this feels different. My friend was talking about an article she’d read about perimenopause, and it got me starting to think there might be a connection between the hormonal changes and my ADHD symptoms intensifying. It's a lot to wrap my head around”.
Angela's days are peppered with these small but significant disruptions: memory lapses, a sense of disorganization, and a once-unshakable concentration that now seems just out of reach.
This revelation sparked a quest for a more integrated treatment approach, one that would harmonize her hormonal health and neurological needs. Now, as Angela navigates her daily responsibilities against the backdrop of these challenges, she is more determined than ever to find balance and clarity amidst the chaos.
Understanding Neurodiversity: A Broader Perspective
The concept of neurodiversity acknowledges the rich variety of human brains and minds, seeing neurological differences such as ADHD, autism, and dyslexia not as deficits, but as natural variations in the human condition, with inherent challenges as well as distinct strengths. Neurodiversity can include both developmental and acquired changes in brain function due to injury or illness, along with transient neurodiverse states that affect how our brains work, like those brought on by hormonal shifts or stress. (**Note, if you don’t have an ADHD diagnosis formally, but are curious, this is my favorite self-assessment quiz. It highlights both strengths and challenges that are characteristic of the ADHD brain).
Is Perimenopause a type of transient neurodiversity?
Did you know that menopause can really shake things up for your brain? That’s right—perimenopause is actually a time of acquired neurodiversity, where the natural shifts in your body can significantly affect how your brain works. Common issues like forgetting where you put your keys, having trouble staying focused, or feeling moodier than usual are all part of this transition. These challenges are often made worse by other symptoms of perimenopause, such as sleep problems and emotional ups and downs.
Women with known ADHD entering perimenopause often find that the strategies they previously used to manage their symptoms are less effective. The additional cognitive load imposed by hormonal fluctuations can exacerbate previously compensated ADHD symptoms, making them more severe and harder to manage.
There’s a pretty noticeable overlap between perimenopause/menopause symptoms and ADHD. Once you stack up the list of what’s common to both, it’s clear to see why things might feel a bit more overwhelming when you hit perimenopause and menopause. Those ADHD symptoms you've been managing? They could get trickier to handle during these changes. So, if you’re feeling a bit off during this time, there’s a good biological reason for it.
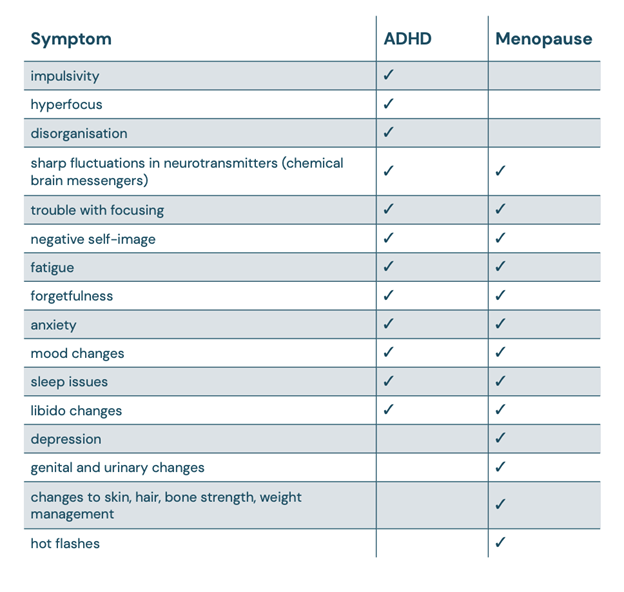
What’s happening behind the scenes? Well, it’s all about hormones. The ebb and flow of estrogen and progesterone during perimenopause don’t just affect your body; they also mess with your brain’s chemical messaging system and even the flow of blood in your brain.
The Estrogen-ADHD Connection: Exploring Estrogen's Impact on Neurotransmission
Estrogen plays a crucial role in the brain, especially in how it relates to ADHD. This hormone helps regulate neurotransmitters like dopamine and serotonin, which are key players in managing our mood, focus, and overall executive functions. When women go through significant hormonal changes, like during perimenopause, the rollercoaster of estrogen levels can lead to a spike in ADHD symptoms. This is often due to what’s known as estrogen withdrawal, where the sudden drop in estrogen levels disrupts the normal balance of neurotransmitters, making symptoms more noticeable.
Estrogen and Serotonin
Estrogen isn’t just about mood swings—it’s a big player in how your brain handles serotonin, which you totally need for nailing those executive functions and keeping your emotions on an even keel. Here’s a kicker: when your estradiol levels dip, studies have shown that the hippocampus (yep, that’s the part of your brain where long-term memories chill) can shrink by up to 40%. Don’t panic, though—this doesn’t mean your memories are wiped; it's more like the pathways to access them aren’t as wide open as before. The hippocampus is like the central hub for your personality, storing all those experiences and interactions that make you, well, you. So, maintaining healthy estrogen levels is pretty essential not just for remembering where you left your keys, but for keeping 'you' feeling like 'you.'
Estrogen's Influence on Dopamine
Estrogen plays a pivotal role in regulating dopamine, a neurotransmitter that's essential for our reward system and focus mechanisms. Low dopamine can feel like a persistent fog of fatigue, lack of motivation, and difficulty finding joy or satisfaction in activities that normally feel rewarding. Research has shown that estrogen helps manage how dopamine transporters and receptors function in the brain. As women enter perimenopause and their estrogen levels start to wane, so does the regulation of dopamine, which can intensify ADHD symptoms.
The Relationship Between Estrogen and Acetylcholine
Years of research have highlighted the critical role of the central nervous system's cholinergic systems in our ability to learn, remember, and pay attention. Estrogen also significantly influences acetylcholine, another key neurotransmitter that's crucial for learning and memory. Studies have repeatedly shown that estradiol bolsters various cognitive processes, enhancing attention and boosting both verbal and visual memory. However, during perimenopause, as estrogen levels decline, the production of acetylcholine also tends to decrease.
While Ritalin and similar stimulants are commonly used to manage ADHD, they primarily target dopamine pathways and are generally more effective in treating severe inattention rather than milder forms. These medications can improve tasks involving visual memory but often fall short in enhancing focus amid distractions or in complex task planning– because they fail to directly support acetylcholine function. Additionally, they come with a host of potential side effects, ranging from mild (sleep disturbance, anxiety, reduced appetite, or headaches) to more serious risks (increased blood pressure and risk of stroke and heart attack, development of or worsening of manic symptoms or other psychiatric conditions, decreased bone density with higher risk for early onset osteoporosis and higher fracture risk).
Unlike these stimulants, strategies that support acetylcholine can offer broader cognitive benefits. Both personally and clinically, I have found the supplement Optimal Focus by Seeking Health, to be incredibly valuable as a component of a well-rounded ADHD support program. It includes ingredients like Ginkgo Biloba and Huperzine A. These components are intended to enhance cognitive functions such as memory and attention, providing a more comprehensive approach to managing ADHD symptoms, particularly in women experiencing perimenopause. This combined support for both dopamine and acetylcholine pathways could be key in developing more effective ADHD treatments.
Histamine: Beyond Allergies, A Neurotransmitter with Wide-Ranging Effects
Histamine is well-known for its role in allergic reactions—think sneezing, itching, and red eyes. But histamine's job description goes way beyond making us miserable during allergy season. It's also a key neurotransmitter, playing roles in our digestion, sleep-wake cycles, mood and brain function. This makes it a substance of interest not just for allergists but for anyone interested in maintaining optimal health.
When Histamine Highs Lead to Health Lows
Histamine's influence extends into what's known as Speer Allergic Tension-Fatigue Syndrome (SATFS), a condition marked by fatigue, irritability, depression, and cognitive fog–often alongside typical allergic symptoms like asthma and eczema. This overlap hints that when dealing with persistent allergies and cognitive or mood disruptions, histamine could be a common denominator.
DAO: The Histamine Handler
Central to managing histamine levels in the body is the enzyme diamine oxidase (DAO). DAO is primarily responsible for breaking down histamine that our bodies produce, preventing its accumulation. In the context of Attention Deficit Hyperactivity Disorder (ADHD), DAO's role becomes particularly significant. Research suggests that reduced DAO activity could lead to heightened histamine levels, potentially exacerbating or contributing to ADHD symptoms.
How Perimenopause Amplifies Histamine
Estrogen dominance is characterized by either high levels of estrogen or insufficient progesterone to counterbalance estrogen's effects. This hormonal imbalance can lead to an increase in histamine levels because estrogen can stimulate the release of histamine from immune cells known as mast cells. When estrogen levels are high, more histamine is released, which can exacerbate symptoms like allergies, hives, mood swings and anxiety– and ADHD symptoms.
On the other hand, progesterone naturally helps to regulate and stabilize mast cell membranes, preventing them from releasing histamine unnecessarily. Low levels of progesterone, therefore, can lead to increased histamine release because there's less hormonal regulation keeping mast cell activity in check. Progesterone also upregulates the production of DAO, the enzyme that helps break down histamine.
For women in various stages of perimenopause, these mechanisms are particularly relevant. During perimenopause, hormone levels fluctuate significantly, and periods of estrogen dominance accompanied by low progesterone are common. These hormonal shifts can result in increased histamine-related symptoms, which may manifest as worsening allergies, sleep disturbances, or changes in mood, brain function, focus, and emotional well-being.
Keeping Histamine in Check
Several factors can cause histamine levels to get out of hand:
- Genetic Factors: Variations in genes like HNMT or DAO can slow down histamine breakdown, leading to higher levels.
- Nutrient Deficiencies and Liver Detoxification Pathways: Certain nutrients are crucial for breaking down histamine. Without them, our bodies struggle to keep histamine levels balanced.
- Gut Health: A healthy gut is critical for producing DAO. If the gut is compromised, so is DAO production, which can lead to increased histamine. Additionally, the presence of specific types of gut pathogens (certain bacteria, parasites, or candida overgrowth) can stimulate the production of higher levels of histamine.
- Diet and Lifestyle: Certain foods and lifestyle factors can trigger histamine release or inhibit DAO, exacerbating symptoms.
For those wrestling with ADHD understanding and managing histamine levels can be transformative. This is just one reason why an integrative approach that considers hormone balance, gut health, detox support, and potentially using supplements to support DAO production can be very effective for some women. By addressing histamine management from multiple angles, it's possible to achieve a better balance and improve overall mood and cognitive function.
Bringing It All Together: ADHD, Perimenopause, and Whole-Body Health
When it comes to managing ADHD symptoms during perimenopause, hormone replacement therapy (HRT) really should be on your radar. HRT can help stabilize those roller-coaster hormone levels, easing some of the intensified ADHD symptoms that come with this life stage. This approach is a breath of fresh air compared to just ramping up doses of stimulant medications, which often miss the mark on addressing the deeper hormonal imbalances and can leave you dealing with some pretty annoying side effects.
But there’s more to the story than just hormones. Keeping your blood sugar stable throughout the day with a well-rounded diet can make a huge difference in how you feel—think fewer energy crashes and mood swings that can kick your ADHD into overdrive. Also, giving a boost to your brain’s neurotransmitters with the right supplements or botanicals can really sharpen your mental clarity and help your brain stay on point.
Don’t overlook the importance of checking for food sensitivities either. Figuring out if certain foods are causing you trouble and cutting them out can seriously help calm ADHD symptoms and boost your overall well-being. And let’s not forget about gut health—it’s a game changer. A happy gut means better detox, better nutrient absorption, and better overall hormone and neurotransmitter balance, which all adds up to you feeling better.
Tackling ADHD during perimenopause with these strategies offers a well-rounded approach that looks at your health from multiple angles.
Give yourself some grace during this transition! Embracing tools like notepads, organization apps (Sunsama, Inflow, Focus@Will) and reminders to help bridge memory gaps is a smart strategy, not a setback. It’s also perfectly okay to take a bit more time with tasks or to ask for help. Remember, you're navigating a significant shift—this isn't about failure, it's about adapting and finding strength in vulnerability. Treat yourself with kindness and compassion as you adjust.
References
- Eng, A. G., Nirjar, U., Elkins, A. R., Sizemore, Y. J., Monticello, K. N., Petersen, M. K., Miller, S. A., Barone, J., Eisenlohr-Moul, T. A., Martel, M. M. (2023). Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. University of Kentucky, Department of Psychology. Link to article
- Roberts, B., Eisenlohr-Moul, T., Martel, M. M. (2018). Reproductive Steroids and ADHD Symptoms Across the Menstrual Cycle. Psychoneuroendocrinology, 88, 105–114. PMC5803442
- Jongkees, B. J., Hommel, B., Colzato, L. S. (2014). People are different: tyrosine's modulating effect on cognitive control in healthy humans may depend on individual differences related to dopamine function. PMC4186281
- Perimenopause, Menopause and ADHD. (2023). Cambridge University Press. Journal of the International Neuropsychological Society
- Roberts, B. A. (2016). Ovarian Hormones, ADHD, Risk-Taking, & Impulsivity. University of Kentucky. Link to thesis
- ADHD Symptoms in Females of Childhood, Adolescent, Reproductive and Menopause Period. (2021). Mater Sociomed, 33(2), 114–118. PMC8385721
- Cumulative exposure to ADHD medication is inversely related to hippocampus subregional volume in children. (2021). Neuroimage Clin., 31, 102695. PMC8141923
- Estrogen-Cholinergic Interactions: Implications for Cognitive Aging. (2015). Horm Behav., 74, 173–185. PMC4573353
- Johansson, J., Landgren, M., Fernell, E., et al. (2013). Decreased binding capacity (B max) of muscarinic acetylcholine receptors in fibroblasts from boys with attention-deficit/hyperactivity disorder (ADHD). ADHD Atten Def Hyp Disord, 5, 267–271. Link to article
- The diamine oxidase (DAO) enzyme, which metabolizes histamine extracellularly, could contribute to ADHD symptoms. PMC10455974
Dude, Where’s My Orgasm?!: Unpacking Sexual Wellness In Perimenopause
Today I’m unpacking a topic that doesn’t get the attention it deserves: sexual wellness during perimenopause. While this is a powerful time in our lives, it can come with a lot of changes that make us feel like those orgasms we once had are now a thing of the past.
What’s worse than searching for our former sensuality is we’re often told by doctors, “That’s common at your age,” and sent on our way without a solution, wishing we hadn’t taken our turn-on for granted.
But here’s the thing: sexual wellness is not a luxury reserved for our younger selves. It’s an essential part of our health and wellbeing in all stages of womanhood: even perimenopause, menopause, and beyond. Pleasure is our birthright, ladies, and together we’re going to reclaim it!
Understanding the Link Between Hormones and Sexual Pleasure
Perimenopause brings a lot of hormonal fluctuations as our bodies prepare for menopause. But there’s more to it than hot flashes and mood swings: hormones like estrogen, progesterone, and testosterone can have a significant impact on our sexual health and intimacy leaving us with reduced sensation, discomfort, or no desire to “do it” in the first place.
If you're facing any of these challenges, you’re not alone–over 40% of perimenopausal women report sexual dysfunction. And sexual dysfunction isn’t just lacking the drive to get down–it can mean having trouble at any of the four stages of sexual response:
- Desire: Lasting anywhere from minutes to hours, desire is when the body begins to prepare for sexual activity in response to thoughts or sensations by increasing blood flow to the vaginal area.
- Arousal: The Lubrication of the vagina and swelling of the clitoris that began in the Desire stage intensified in the Arousal stage.
- Orgasm: During orgasm, or climax, pelvic muscles contract and tension is released.
- Resolution: This is when muscles begin to relax, heart rate slows, and the body returns to its unaroused state.
The good news? These issues can often be addressed, bringing you back to a place of sexual satisfaction. Before we talk about how to address them, though, let’s take a look at what’s causing these unwanted changes.
Decreased Sensitivity and Sensation
Estrogen plays a vital role in maintaining vaginal lubrication and blood flow. As estrogen levels begin to drop during menopause, women may experience decreased sensitivity and sensation, particularly in the clitoris. This can lead to orgasms that are less intense, more difficult to achieve, or are even non-existent. So if you’re feeling like someone “turned down the volume” on your orgasms or they’re completely MIA, estrogen may be to blame.
Discomfort
Estrogen is also responsible for overall vaginal tissue health. Decreasing estrogen can lead to vaginal atrophy: thinning and inflammation of the vaginal walls, along with vaginal dryness. All of this can contribute to discomfort, irritation, and pain during sex.
Low Sex Drive
We can’t place all the blame on estrogen for trouble in the bedroom, though. Progesterone and testosterone can also start to decline during menopause, bringing your mood and–you guessed it–libido right down with them.
A Holistic Approach to Rediscovering Sexual Pleasure In Perimenopause
So, what can we do to relight the fire and restore intimacy? Here’s where to start:
- Address Hormone Imbalances: Just as I emphasized the significance of hormone balance for skin health, the same applies to your sexual health. Comprehensive hormone testing is key to addressing imbalances. The DUTCH panel can give invaluable insight into your hormone levels and guide a personalized protocol to restore balance.
- Nurture Your Gut: Surprisingly, gut health also impacts sexual health. A healthy gut supports nutrient absorption, including essential vitamins and minerals crucial for hormone production and overall well-being. Prioritize a diverse, nourishing diet and consider probiotics to support your gut microbiome.
- Manage Stress & Boost Adrenals: Chronic stress can negatively impact adrenal and sex hormone levels–and can make-or-break the feeling of being “in the mood”. The stress hormone cortisol can also reduce estrogen, leading to decreased sensitivity in the vagina and clitoris. To support adrenal health and balance cortisol levels, practice stress-reduction techniques like mindfulness, meditation, or gentle exercise. In addition, shoot for 8 hours of sleep each night. If you have ongoing signs of HPA Axis imbalance (constant fatigue, feeling “wired but tired”, trouble falling or staying asleep, or a poor stress response) talk with your Functional Medicine provider about running a DUTCH Adrenal panel to get a customized repair protocol.
- Embrace Self-Care and Connection: We talked about how self-care is essential for healthy skin, but it's equally vital for your sexual well-being. Prioritize time for relaxation, self-exploration, and connection with your partner to enhance intimacy. Share your experiences, concerns, and desires with your partner to build trust and understanding as you navigate perimenopause.
- Explore New Avenues: As our bodies evolve, so can our desires and interests. Embrace this opportunity to explore new ways of intimacy and sensuality, whether through mindfulness practices, tantra, or simply trying something new with your partner. Studies have shown that women in their 40s and 50s tend to become more independent, confident, and decisive, and less self-critical. They also generally feel better in their own skin and more comfortable with who they are, which can lead to new levels of sexual confidence and willingness to explore what they actually find pleasurable. Give it a try! Who knows, you might discover ways of connecting that bring you to new levels of intimacy and satisfaction.
- Address Trauma: If you’ve been affected by trauma, please know that you are not alone. Any experience with trauma–not just sexual trauma–can cause issues with sexual function. Addressing your trauma with a qualified professional is the first step to resolving any sexual challenges you may be facing.
Here are some other great treatment options to consider:
- Topical DHEA: Julva, a topical DHEA cream, can help rejuvenate vaginal tissue and support sexual health. It’s generally safe when used as directed, but always consult your healthcare provider–especially if you’ve had breast cancer. A recent study found that the use of vaginal DHEA in women after breast cancer treatment did result in increased hormone concentrations, though the levels were still within the lower postmenopausal hormone range.
- Topical Estriol or Estradiol: Topical estriol or estradiol can increase clitoral sensitivity, improve vaginal tissue health, and prevent or treat atrophy. Estriol is a safer alternative to estradiol, and is just as effective. One study found that hormone levels remained unchanged after a 12-week treatment with 0.005% estriol vaginal gel in postmenopausal women with early hormone receptor-positive breast cancer. These results support the safety of 0.005% estriol vaginal gel for the treatment of vulvovaginal atrophy symptoms in women who have had breast cancer. While low-dose, locally applied estrogen can be a safe option, hormone levels should be closely monitored by your healthcare provider while using topical creams through testing like the DUTCH Sex Hormone Panel.
- Pelvic Floor Physical Therapy : If you haven’t seen a pelvic floor physical therapist, now might be the time! Pelvic floor therapists are trained physical therapists who specialize in treating pelvic floor dysfunction. The pelvic floor refers to the muscles supporting the reproductive, urinary, and bowel organs. If you’ve ever given birth (vaginally or via cesarean), you should be assessed by a pelvic floor physical therapist. This type of therapy isn’t just for women who have given birth, though–it can be highly effective in treating pelvic pain, urinary and bowel problems, pelvic organ prolapse, sexual dysfunction, and more. In fact, research supports the use of pelvic floor physical therapy as a minimally invasive, first-line treatment for pelvic issues–including sexual dysfunction.
- Perifit: Ever think you’d get to play video games with your vagina? Perifit is a device similar to a sex toy that uses video game technology to help visualize, measure, and strengthen your pelvic floor muscles. It can help restore sexual function and pleasure and reduce incontinence. Not to mention, it’s fun and addictive!
- Joylux vFit - Red Light Therapy: Red light therapy isn’t just for anti-aging skin treatments–it can also work wonders for vaginal health! vFit by Joylux is a non-invasive red light therapy device designed to improve vaginal moisture, tissue resilience, sensitivity, sensation, and sexual satisfaction in just three 10-12 minute sessions a week. Painless and hormone-free, vFit is easy to use from the comfort of your home. Some women see results in as little as 3 weeks! For faster and more complete results, Joylux offers a $99 upgrade to the vFit Gold Device that includes a 32% increase in power and 2 additional minutes of treatment time. You can access this upgrade and accelerate your results for free by purchasing through our office! For more information, contact us today. Contact our office for more information if you’re interested in the vFit–we can get you free access to the upgrade!
- Bonafide Ristela: Ristela is a plant-based, hormone-free supplement formulated to improve orgasm and overall sexual satisfaction by increasing blood-flow to the vaginal area. After just two months of taking Ristela, 75% of women reported an increase in both physical arousal and sexual satisfaction, and 74% reported an increase in orgasm!
Other Factors Contributing to Sexual Dysfunction
It’s important to note a few other factors, not necessarily related to perimenopause, that can contribute to sexual dysfunction. Here are some common situations to consider, and how to address them.
- Clitoral Atrophy: Clitoral atrophy is when the clitoris shrinks in size and loses sensation due to impaired blood flow to the area, menopause, or having a hysterectomy. In the case of clitoral atrophy, the saying “use it or lose it” may actually come into play! Masturbation and exercises can help redirect blood flow to the clitoris, which can help in certain cases with clitoral atrophy. Don’t be afraid to ask your doctor about hormone therapy–estrogen may also be helpful.
- Pelvic Organ Prolapse: Pelvic organ prolapse is a condition where one of the pelvic organs (most commonly the uterus or bladder) drops down into the vagina. This is common and not life threatening, but can significantly impact quality of life, sometimes causing symptoms like painful intercourse and decreased vaginal sensation. Other symptoms may include a feeling of fullness in the vagina, urinary problems, and feeling or seeing a lump inside or coming out of the vagina. If you think you’re dealing with pelvic organ prolapse, get evaluated by your doctor. Surgery isn’t the only option–he or she may recommend pelvic floor physical therapy, hormone therapy, or a vaginal pessary (a flexible device inserted into the vagina designed to support the areas affected by the prolapse).
- Childbirth: Scarring and weakened pelvic muscles after childbirth can contribute to decreased sensation or discomfort during intercourse. This is extremely common, but can be addressed. Talk with your functional medicine provider, doctor, or pelvic floor physical therapist for recommendations.
Empower Your Perimenopausal Sexual Health
Perimenopause doesn't mean your nights between the sheets are over. Sexual wellness and satisfaction are an essential part of your health and happiness today and everyday!
OPTION 1 My goal is to support you on this journey, helping you rediscover your vitality and sexual pleasure along the way. If you’re ready to embrace this phase of life with confidence, schedule a 15 minute call to learn more about how I can help guide you.
OPTION 2 If you’re ready to embrace this phase of life without hormonal symptoms dragging you down, come learn more about our new program, The Reverse Age Method.
This group coaching program is compassionately designed for women in perimenopause who want to stop menopausal weight gain, supercharge their energy, boost brainpower, and support glowing, vibrant skin. Oh yeah…and have great sex! Join us today.
Harnessing the Power of Hormones: Menopause, Weight Management, and Beyond
As women navigate the winding path of perimenopause and enter the world of menopause, a whole gamut of changes start to occur within their bodies. These changes are mostly driven by shifts in hormone levels, most notably, the decline in estrogen. One area of our health that takes a significant hit during this time is weight management. It’s as if an internal switch has been flicked, and suddenly, maintaining a steady weight becomes a challenge. Who’s body is this? When did these jeans get too small?
But why does this happen? And is there anything we can do about it?
Estrogen, Appetite, and Weight
Estrogen, one of the primary female sex hormones, performs numerous functions beyond its role in reproductive health. It is intricately linked with our metabolic health, affecting how our cells convert glucose into energy.
During the perimenopausal transition, estrogen levels decline, leading to what we could call a "temporary energy crisis". Our cells find it harder to convert glucose into energy, which can trigger increased appetite, hot flashes, and night sweats. The latter can disrupt sleep, which can then further exacerbate these symptoms. This combination of physical discomfort and heightened appetite often leads to overeating or binge eating, contributing to weight gain.
The Glucose-Ketone Transition
As estrogen levels decrease, our bodies need to adapt to this new metabolic environment. The hormone estradiol, a form of estrogen, usually increases glucose sensitivity by enhancing the ability of mitochondria (the powerhouses of our cells) to turn glucose into energy.
With the decline in estrogen levels, our cells have to switch from burning glucose to burning ketones. This switch requires a certain degree of "metabolic flexibility". If the brain can adapt to a higher ketone state, the symptoms should be temporary. However, if the body cannot adapt due to whole-body insulin resistance, this can potentially lead to more serious conditions such as dementia.
What Are Ketones?
Ketones are produced in the liver from the breakdown of fats. This production occurs in the absence of glucose, which comes from sugars and carbohydrates. This process can occur overnight, during fasting, or when we eat meals that are primarily made up of proteins and fats, without adding more than 5 grams of carbohydrates.
Embracing Metabolic Flexibility for a Healthier Perimenopause
Metabolic flexibility is your body's ability to switch between using glucose or ketones as a fuel source. This flexibility is essential, especially during the perimenopause transition, as it allows your body to adapt to changing hormone levels and efficiently use available energy sources.
When your body can seamlessly shift from glucose to ketones, you can experience fewer menopausal symptoms, improved energy levels, and better weight management. Here are some strategies that can enhance your metabolic flexibility:
Dietary Approaches
The foods we consume play a crucial role in how our bodies metabolize energy. Specific types of diets can enhance metabolic flexibility by optimizing your body's ability to switch between glucose and ketones.
Low-Carbohydrate, High-Fat Diets (LCHF)
These diets, such as the ketogenic diet, are designed to shift your body's primary fuel source from glucose to ketones. By reducing carbohydrate intake and increasing healthy fats, you can stimulate your liver to produce ketones more efficiently, promoting metabolic flexibility.
Mediterranean Diet
This diet emphasizes fruits, vegetables, whole grains, legumes, and healthy fats, like olive oil and fatty fish. It's rich in nutrients that support metabolic health and can enhance insulin sensitivity, a crucial aspect of metabolic flexibility.
Fasting
Intermittent fasting, whether it's time-restricted eating or alternate-day fasting, gives your body a break from processing food. This pause allows your body to deplete its glucose stores and start producing and using ketones, increasing metabolic flexibility.
Resistance Training
Physical activity, especially resistance or strength training, can boost your metabolic flexibility by enhancing insulin sensitivity and promoting muscle growth. Having more muscle mass means your body can store more glucose, thus reducing the likelihood of insulin resistance.
Lifestyle Steps
Implementing simple lifestyle changes can also greatly enhance your metabolic flexibility.
Adequate Sleep
Sleep deprivation can lead to insulin resistance, impairing your metabolic flexibility. Aim for 7-9 hours of quality sleep per night.
Stress Management
Chronic stress can negatively impact your metabolic health, including your body's ability to switch between fuel sources. Regular mindfulness practices, like yoga or meditation, can help manage stress levels.
Empower your journey through perimenopause by improving your metabolic flexibility. Our group program integrates these dietary, physical activity, and lifestyle approaches, providing a comprehensive plan to help you navigate this transition with grace and strength.
Why wait? Book a discovery call with us today. It’s time to take control of your health and embrace a brighter, leaner, and more energetic you during perimenopause and beyond.
Your Path to a Healthy Perimenopause
Understanding these complex processes is the first step towards taking control of your health during perimenopause and beyond. There are ways to navigate these changes and manage the symptoms effectively.
The transition into menopause should not equate to giving up on your health goals. This is a time for empowerment, for harnessing the change and using it to propel yourself into a phase of increased longevity, youthful skin, solid energy, a fiercely sharp brain, and a lean body.
Our group program is designed specifically for women in perimenopause who want to 'reverse-age'. Our scientifically-backed strategies will help you adapt to the hormonal changes, improve your metabolic flexibility, and help you avoid weight gain. Better yet, we understand that your body is not identical to the next woman’s body and metabolism, and we utilize state of the art lab testing to personalize your protocol for longevity optimization and reclaiming your body, energy, mind, and beautiful skin.
I encourage you to take this journey with us. Book a discovery call today, and let’s work together to not just weather the menopausal transition, but to thrive through it. Embrace this change as an opportunity to become the best version of yourself. Because you deserve nothing less.
Unlocking the Secrets of Hormonal Changes and Conquering Menopausal Weight Gain
Aisha, a client of mine, is an energetic and dynamic woman in the prime of her life. At 49 years young, she's a loving mother and a dedicated business owner, juggling life's demands with grace and determination. When I met with her last week, she expressed feeling increasingly frustrated as she’s noticing changes in her body that she never expected. Despite sticking to her tried-and-true diet and lifelong exercise routines that once worked like magic, she's now facing the reality of having to buy a size up in jeans because her old ones no longer fit. This unexpected shift has left her questioning what's happening and longing for answers. If you’re having a similar experience (or want to learn how to avoid it!) read on– I’ll share with you exactly how I broke it down for her so that you can have the knowledge of exactly what steps to take charge of your own body as you navigate these hormonal changes.
Hormonal Changes During Menopause
Menopause is a natural phase in a woman's life when her ovaries gradually produce fewer hormones, leading to the end of menstruation. Two key hormones involved in this process are estrogen and androgen (think “male” hormones like Testosterone and its precursor DHEA). During perimenopause, the 15 year lead up to menopause, a reduction in estrogen and a relative increase in circulating androgen occur. These hormonal shifts can influence body composition, muscle mass, and the distribution of fat within our bodies.
A 2021 journal publication titled "Changes in Energy Metabolism and Lipid Metabolic Abnormalities Underlying Weight Gain in Postmenopausal Women" breaks down this physiological cascade in detail. This study focused on understanding how our body's energy and fat processing change during menopause. During menopause, many women tend to gain weight, and to redistribute fat around the abdomen, and this research aimed to figure out why it happens. First let’s look at the roles these hormones play with fat storage:
- Estrogen: Estrogen is a critical hormone that plays many roles in our bodies. One of its essential functions is to regulate fat distribution. Before menopause, estrogen levels are higher, and this helps to keep fat stored in subcutaneous (under the skin) areas rather than visceral (around organs) regions.
- Androgen: Androgens are another group of hormones, often referred to as the "male hormone," though they are present in women too. (Androgens typically refer to testosterone, DHEA, and their metabolites). During menopause, as estrogen levels decrease, the relative balance of hormones shifts, leading to a relatively higher level of androgen in the body. This shift can contribute to changes in body composition, such as increased fat accumulation in the abdominal area.
The relative balance of estrogen and androgen is crucial in maintaining a healthy body composition and metabolism. When estrogen levels decline during menopause, it disrupts this balance. As a result visceral fat lipolysis increases and Beta oxidation decreases. Let’s break down what each of those are and what they mean for you:
Visceral Fat Lipolysis
To explain this, let's imagine fat in our body like tiny little storage units. Visceral fat is a specific type of fat that surrounds our internal organs, like the liver and intestines. When we talk about "lipolysis," it means the process of breaking down these fat storage units to release the stored fat as energy. During menopause, there's an increased breakdown of this visceral fat, which can lead to an excess of fatty acids floating around in our bodies. When Visceral Fat Lipolysis increases, due to falling estrogen levels, the body tends to break down more visceral fat through a process called "lipolysis." This means that the stored fat around our organs is released into the bloodstream as fatty acids. Studies show that having consistently elevated circulating levels of fatty acids in the bloodstream can lead to insulin resistance.
Beta Oxidation
Beta oxidation is like a special team within our body that helps convert these released fatty acids into energy for us to use.Normally, the body efficiently converts these released fatty acids into energy through "beta oxidation." But during menopause, the team's performance can be affected because of certain hormonal changes, like a decrease in estrogen. As a result, these released fatty acids may not get converted into energy efficiently, and they end up staying as fat in our bodies, especially in the belly area.
Insulin Resistance
Additionally, the hormonal changes can also contribute to insulin resistance. Insulin is a hormone that helps regulate blood sugar levels. Increased levels of circulating fatty acids can lead to insulin resistance, where our body's cells become less responsive to insulin's actions. This can hinder the body's ability to use glucose for energy, resulting in higher blood sugar levels.
Metabolic Rate
Furthermore, these hormonal shifts can impact the body's overall metabolic rate, which is the speed at which our body burns calories for energy. A decrease in estrogen can also lower the metabolic rate, by upregulating genes that promote fat storage, leading to potential weight gain.
In summary, hormonal changes during menopause, particularly the decrease in estrogen and relative increase in androgen, play a vital role in altering body composition and metabolism. These changes can lead to increased visceral fat lipolysis, impaired beta oxidation, insulin resistance, and a lower metabolic rate, all contributing to menopausal weight gain, especially around the belly area. Understanding these hormonal shifts is crucial for developing personalized approaches to support women's health and well-being during this natural phase of life. Seeking guidance from healthcare professionals can help navigate this journey with better insight and make informed decisions for a healthier future.
So, What Does it all Mean?
In simple terms, this study found that hormonal changes during menopause may lead to an increase in abdominal fat storage and increased tendency to develop insulin resistance, even without changes in diet and lifestyle. However, with informed steps, this challenge can be tackled effectively.
Clinically, I have found four main steps that are essential to preventing or reversing the weight creep up many women experience:
Step 1: Optimizing Nutrition
1. Low Carb Diet Variations:
Exploring lower carb diet variations can be a game-changer for women’s bodies. By focusing on nutrient-dense, low carb foods, we can stabilize blood sugar levels and support your body's metabolism. It's essential to find the right balance that suits your individual needs, ensuring she gets enough energy for your activity level while still managing carbohydrate intake.
2. Timing of Carbohydrates:
Timing plays a vital role in optimizing how your body processes carbohydrates. Consuming carbs closer to physical activity allows your body to use them more efficiently as fuel for her workouts. This helps prevent excessive storage of carbohydrates as fat and maximizes their energy benefits.
3. Intermittent Fasting: A Powerful Tool for Menopausal Women
Intermittent fasting involves cycling between periods of eating and fasting, allowing the body to tap into its natural rhythms and optimize various physiological processes, and can be a valuable tool when used in the right way, at the right time. The benefits of Intermittent Fasting for Menopausal Women include:
Hormonal Balance: Intermittent fasting has shown promise in helping to balance hormone levels in menopausal women. By allowing the body to experience periods of fasting, insulin sensitivity can improve, which in turn positively impacts the balance of sex hormones and adrenal hormones.
Insulin Regulation: As menopausal women often face an increased risk of insulin resistance, intermittent fasting can be a powerful strategy. It helps regulate blood sugar levels, reducing the likelihood of insulin resistance and supporting overall metabolic health.
Weight Management: Intermittent fasting can assist menopausal women in managing their weight. By promoting fat burning during fasting periods and limiting calorie intake, it can help shed excess weight and support a healthy body composition.
Cellular Repair and Longevity: Intermittent fasting triggers a process called autophagy, where cells remove damaged components and repair themselves. This process supports cellular health and has been linked to potential longevity benefits.
Enhanced Energy: By optimizing insulin sensitivity and cellular repair, intermittent fasting can lead to increased energy levels and improved overall well-being.
While intermittent fasting can offer numerous benefits for menopausal women, it's essential to approach this practice mindfully. As we navigate this new aspect of your journey, it's crucial to listen to your body and make adjustments as needed. Consulting with a trusted expert ensures that intermittent fasting becomes a positive and supportive addition to your health journey.
4. Resistance Training for Muscle Building:
Incorporating resistance training into your routine can do wonders for your body composition. Building lean muscle mass through strength training boosts metabolism and increases insulin sensitivity. As you put on muscle, your body becomes more effective at using insulin to control blood sugar levels.
The Role of Muscle and Insulin: Muscles are like little powerhouses in our bodies. When you engage in resistance training, your muscles become more responsive to insulin, allowing them to efficiently use glucose for energy. This reduces the risk of insulin resistance, a condition where cells don't respond well to insulin's signals, leading to elevated blood sugar levels.
Boosting Mitochondrial Function: Mitochondria are like tiny energy factories within our cells, and they play a crucial role in energy production. By engaging in resistance training and maintaining a balanced diet, you can enhance your mitochondrial function, leading to improved energy levels and overall metabolic health.
Action Steps: Working with a Trusted Expert
Functional Medicine testing to optimize hormones and cellular metabolism can take diet and lifestyle efforts to the next level in terms of getting results. By running hormone testing, you can gain valuable insights into hormone levels, including sex hormones, adrenal hormones, insulin, and other hormones related to metabolism. This personalized approach allows you to tailor interventions that optimize your hormonal balance.
Reprogramming optimal mitochondrial function. We use Organic Acid testing to assess your personal level of mitochondrial efficiency and levels of oxidative stress. We can also gain insights into precisely the nutrients or approaches your body can best use to rehab any shortcomings to optimize mitochondrial function and ultimately your longevity and wellspan/playspan! By addressing any imbalances and providing targeted interventions, you can unlock her body's potential for renewed energy and vitality.
Remember, this phase of your journey is an invitation to embrace the power within and discover the incredible potential of your body! Embracing this specialized approach to healthcare empowers us to restore hormonal balance and optimize overall well-being.
If you’re interested in learning more, schedule a free 15 minute call by clicking here. We offer different programs for every need and budget, and would love to help you find the support that’s a perfect fit for you.
Understanding the Link Between Stress and Perimenopause
Stress - we’re all living with it.
And you don’t need me to tell you stress isn’t great for your health…
But for women in or near perimenopause, stress deserves special mention. Research has shown chronic stress actually worsens the hormonal symptoms of perimenopause, like hot flashes and PMS - as well as weight gain, decreased sex drive, and overall feelings of wellbeing.
But as we all know, “getting rid of” stress really isn’t an option. As a long-time health practitioner, my goal isn’t to help my clients eliminate stress, but rather teach them strategies to better manage stress.
This is especially important during the perimenopause transition, when we are already in a hormonal shift and have less “wiggle room” to manage things like stress, blood sugar imbalances, and inflammation from hidden infections.
But I’m not just talking about starting a meditation practice or saying no to that extra project at work. Targeted use of the right bioidentical hormones, herbs, and adrenal support supplements can help your body handle stress better, and help you transition through menopause seamlessly.
Today, let’s explore what stress and menopause do to the body on a hormonal level - and what we can do to better support the body for more energy, less hormonal symptoms, and a better life.
How Stress Impacts Your Hormones
When I say “hormones” I don’t just mean your sex hormones like testosterone, estrogen, and progesterone. I’m also talking about adrenal hormones like cortisol and DHEA, which play a role in controlling your sex hormones as well.
During perimenopause, hormone levels fluctuate, and it's fluctuating hormones that can cause symptoms like hot flashes, mood swings, and weight gain. Research shows that stress only intensifies this.
Stress triggers the release of cortisol. This is good, as cortisol is the “fight or flight” hormone that helps us respond to danger. But when stress is on-going, it can lead to an on-going state of elevated cortisol. Elevated cortisol in turn depletes the hormone DHEA, which is already in a natural state of decline as we age.
Low DHEA is a problem for anyone, but especially for perimenopausal women because DHEA is a precursor to both testosterone and estrogen. Low levels of DHEA can therefore cause low levels of both testosterone and estrogen, intensifying the already changing hormone levels during this time.
Low DHEA & The Pregnenolone Steal
So far, we’ve covered how stress can lead to elevated cortisol, which causes lower levels of DHEA. Because DHEA is a precursor for testosterone and estrogen, it can impact sex hormones.
But why does elevated cortisol deplete DHEA? That’s thanks to a process commonly called the “Pregnenolone Steal.”
The basic premise of the pregnenolone steal is that pregnenolone - a hormone produced by the adrenal gland - is a precursor for both cortisol and DHEA. When stress is high, the body reacts by producing more and more cortisol, “stealing” all the pregnenolone and leaving none for DHEA production.
That’s a bit of an oversimplification, though. There’s not just one pool of pregnenolone that gets depleted. In reality, pregnenolone is in the mitochondria of each of the cells. Rather than thinking about pregnenolone being stolen, it's more that the body prioritizes some pathways of hormone production that are about survival (cortisol), over reproductive hormones.
That being said, no matter “how” it happens, the decrease in sex hormone production this causes is particularly inopportune during the perimenopause years, when we are already hormonally in shift. It can make it seem like we are more sensitive to stress, or that it takes less stress to cause a noticeable change in how we look and feel. Coexisting issues like blood sugar imbalance or hidden infections - which are other common triggers for cortisol release - might suddenly become a bigger problem, too.
Perimenopause and Low DHEA Symptoms
If you’re dealing with stress related hormone dysfunction on top of perimenopause symptoms, you might feel like you’ve got the worst perimenopause of anyone you know. It can cause an intensification of already-known symptoms like:
- Hot flashes
- Night sweats
- Decreased sex drive (low libido)
- Decreased sexual pleasure
- Weight gain/ weight loss resistance
- Poor sleep
- Increased cravings
- Mood disturbances (depression, anxiety, etc.)
- Low energy
- Overall lack of wellbeing
So that’s the “bad news.” Now let’s talk about the good news - all the things you can do to help rebalance hormones, support your body’s stress response, and get back to feeling like yourself.
In fact, after 1-2 months on a customized plan based on your hormone test results, most of my clients see a 75% or more reduction in symptoms.
Can Hormone Therapy Help Low DHEA and Perimenopause?
For a deep dive into using bioidentical hormones safely during perimenopause, see my blog here.
But in addition to sex hormone replacement therapy, supplementing with hormones like DHEA can be an option too.
When used appropriately - and well monitored - DHEA is a safe way to help increase low testosterone in peri-and menopausal women. (It’s especially great for women with some types of hair loss, too!)
But, DHEA needs to be used carefully. Androgen dominance (too much testosterone) can be a main driver for the development or worsening of insulin resistance in perimenopause.
That’s why I always recommend testing before starting DHEA (even if it is available over the counter where you live) and on-going monitoring. I recommend a comprehensive hormone panel like the DUTCH test.
In the clinic, we also use pregnenolone supplementation when using DHEA. This helps with two main problems with DHEA supplementation. First, it can help offset the tendency of DHEA to lower cortisol levels, which can be a problem if someone is already dealing with low HPA output.
Secondly, DHEA has a tendency to put weight on some people, or cause water retention. Adding pregnenolone can prevent this tendency.
Active Stress Management and Supplements
Supplementing with hormones is just one part of the puzzle - just as, if not more, important are complementary lifestyle practices that help manage stress.
I make a custom plan for each of my clients, but some of the techniques we use include:
- Optimizing sleep hygiene (no blue light before bed, etc.)
- Introducing movement (finding an exercise you actually enjoy– and prioritizing muscle building over cardio)
- Circadian alignment (going to bed and rising with the sunset/sunrise)
- Balancing blood sugar and increasing protein intake
- Eliminating/reducing alcohol and processed sugar
Active stress management - like qi gong, walks in nature, meditation in any form, making time for art, getting involved in your community, and spending time with friends and loved ones - are also key.
And then of course there are the issues that you can control - like your relationships, overall task burden, time management, ability to delegate and ask for support, and cutting out toxic people or activities.
These steps can help you eliminate what stress you can and better tolerate the stress you have to live with.
A final piece of the puzzle are adaptogenic herbs and herbs for supplement symptoms. As a long-time Traditional Chinese Medicine practitioner, I’ve seen the incredible power of herbs for transforming health. But, as with all powerful tools, they should only be used after adequate testing or practitioner diagnosis has identified the imbalances that exist.
Look and Feel Your Best in Perimenopause
Perimenopause has a reputation as the worst time in a woman's life… but it doesn’t have to be that way!
With the right support, you can not just survive perimenopause - but actually enjoy the transition and step confidently into a new chapter in your life.
You don’t have to accept weight gain, low sex drive and lack of pleasure, hot flashes, mood swings, cravings, irritability, and all the other common symptoms of perimenopause.
My passion is guiding women through this change, helping to support their body’s unique needs, and watching them thrive in this phase of life!
If you’re interested in learning more, schedule a free 15 minute call by clicking here. We offer different programs for every need and budget, and would love to help you find the support that’s a perfect fit for you.
Skin from Within: A Unique Approach to Anti-Aging Skin Care
If there is one thing we all can agree on it’s this: we want younger looking skin!
And judging by the myriad face creams, facials, lasers, and injectables on the market, most of us are willing to spend time and a lot of money to get it.
But if you’ve tried a few of these products (or procedures) you’ve likely been underwhelmed. Even the very expensive treatments don’t have the kind of results most people want and expect.
And as a long-time functional medicine practitioner and acupuncturist, I can explain exactly why…
These treatments only go skin deep.
If you want the kind of radical results that get everyone asking “What are you doing differently?!” you absolutely must address your skin’s aging from the inside out.
We need to go beyond topical treatments and take a look at what is happening on a cellular level to actually change the way your skin looks as it regenerates itself. To do this, we need to talk about your mitochondria.
Stick with me - today I will explain what your mitochondria are (in a simple way) and how you can help them function better for younger looking skin from the outside in, no 27-step skincare regimen required!
How the Mitochondria Give You Youthful Skin
Mitochondria are one part of the many cells that make up your entire body. You might remember from high school biology that the mitochondria are like the batteries that charge up your cells. Mitochondria churn out ATP (Adenosine triphosphate), the fuel your cells use for energy.
Research has shown that mitochondria become less efficient as we age. When researchers looked at mitochondria in skin cells from young, middle-aged, and older patients, they found mitochondria function was lower in middle-aged adults and even lower in the older group.
The lower mitochondrial function left the aging skin cells more vulnerable to the effects of damaging compounds known as reactive oxygen species (ROS)—otherwise known as free radicals. Free radicals damage the skin cells, leading to a dry, wrinkly outer layer and premature aging over time.
On the other hand, robust mitochondrial action helps protect skin from damage and recover quickly - think of the way a kid’s skin heals after a cut. That's why, as we age and mitochondrial function naturally decreases, we start to see fine lines, wrinkles, sagginess, and discoloration set in.
Protecting Your Skin From The Sun
One HUGE source of skin damage throughout life is UV radiation from the sun. The problem is twofold. First, too much sun exposure weakens the mitochondria and the energy production in skin cells sputters out. This changes the skin—and not in a good way. The sun damage leads to premature skin aging.
But in addition to this, the mitochondria—when they’re working well—serve as nature’s sunscreen helping to protect your skin from sun damage even when it is exposed. That’s why it can feel like all the sun damage from you teens and twenties finally appeared when you turned 30!
How To Have Beautiful Skin
The healthiest thing you can do for your skin is to rejuvenate your mitochondrial health. One of the best ways to do this is with a powerhouse nutrient called NAD+ (nicotinamide adenine dinucleotide). Your mitochondria use NAD+ in order to make ATP. Without enough NAD+, your cells can’t create the ATP that provides the energy to defend against free radicals, which leads to skin damage.
Plenty of NAD+ equals plenty of ATP, which in turn results in gorgeous skin. Since NAD+ levels drop with age, an NAD supplement is an important part of aging skin care.
NAD+ also boosts levels of sirtuins, a family of proteins that can protect your skin against inflammation. Redness and puffiness are signs your sirtuin levels may have taken a nosedive. Scientists call this inflammaging, meaning the inflammation that happens as you age.
Keeping the mitochondria happy and healthy by using NAD+ also can lengthen your telomeres. These are caps at the end of your chromosomes, just like the caps at the end of your shoelaces that keep them from unraveling.
As you age, your telomeres grow shorter. UV radiation from the sun also shortens telomeres in the skin. The more you can do to protect your telomeres, the healthier your skin will look.
The best bet? Use NAD+ both orally and topically on your skin itself. An oral NAD supplement will include nicotinamide riboside or nicotinamide mononucleotide. In addition, there’s a liposomal NAD+ product, and NAD+ is also included in Thorne Collagen Plus, along with other skin healthy ingredients.
Other Mitochondrial Support Supplements
You’ve probably noticed that many topical skin health product contain antioxidants like vitamins C and E and coenzyme Q10. Antioxidants like these help to protect the mitochondria from free radical damage.
But just using these antioxidants topically misses the mark - it’s when used internally that they can have the greatest anti-aging effect.
However, you don’t want to just start popping tons of mitochondrial support supplements - it’s better to work with a functional medicine practitioner who can isolate the nutrients you’re low in and focus on those.
Having said that, here are some mitochondrial rejuvenators worth talking about with your provider. Each of these supplements either protect the skin against stress, act as antioxidants and defend against too many damaging ROS, and soothe inflammation.
- Adaptogens
- Alpha lipoic acid
- Coenzyme Q10
- Curcumin
- Probiotics
- Carnitine
- Glutathione
- Magnesium
- Omega-3 fatty acids
- Vitamin B12
- Vitamin C
- Zinc
Avoid Things That Damage the Mitochondria
You might have noticed that when you don’t get a good night’s sleep, your skin suffers. Or when you’re going through a lot of stress your skin lacks that healthy glow. Think about how much older presidents look when they leave office compared to when they first took over one of the most stressful jobs around.
Lack of sleep and stress can spell trouble for the mitochondria. In fact, their impact on the mitochondria may be the reason why each of these things can get in the way of healthy looking skin.
The sex hormone estrogen also protects the mitochondria at the same time as it keeps the skin looking young, so as levels start to decline with premenopause, the mitochondria can suffer. This is why it’s a good idea to work with a functional medicine provider to balance hormone levels.
Toxins are another source of mitochondrial damage. Toxins are all over the place: in your food, your water, the air you breathe. We’ll talk more about the role of toxins in mitochondrial health in an upcoming blog post.
The Secret to Gorgeous Skin
Want skin that looks and feels younger and healthier? As a functional medicine provider, I can help you maintain your youthful appearance by ordering the right tests and then choosing the right supplements. That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you. We’ll start there, and if you come on board as a client, I’ll order a full lab work-up. Our strategy is to give you healthy skin from within so your good-health glow will turn heads wherever you go.
What Is Mold Toxicity or Mycotoxin Illness?
Did you know you might have an unwanted house guest?
Sometimes, that “guest” sends out a musty odor, so you know it’s there.
Other times, there are no obvious signs of your visitor’s presence.
In fact, the problem may not have originated in your current home. Your unwanted visitor might have hitched a ride with you when you moved from one place to another.
This visitor is a real troublemaker.
I’m talking about mold. Gross, right? Especially when you discover that it can colonize more than just your house—it can also colonize you.
Mold can wreak havoc on your health. If you suffer from brain fog, fatigue, acne, light sensitivity, sleep problems, or headaches—or one or more of the other symptoms listed later in this article—your unwanted guest could be to blame.
When mold makes you sick, it’s called mold toxicity, mold illness, or mycotoxin illness.
My Personal Experience with Mold
I’m deeply interested in mold toxicity right now. Why? During a recent storm, my neighbor’s hose froze and ruptured. The trouble began when it thawed out, and the water saturated the ground between our homes. Some of that water leaked into my basement—an area already susceptible to mold because it’s foundation is 100 years old.
I woke up on Christmas morning to the sound of water trickling in the basement and spent the day shop-vacuuming up over 30 gallons of water as it flowed down the inside of the dry wall and out across the flooring (and under it!) from under the baseboard. A demo team came pretty quickly to remove the Pergo and linoleum, and parts of the drywall– the bigger problem was that once those were pulled out, there was clear evidence of pre-existing water damage and mold on the surfaces. I immediately had an industrial grade HEPA air filter installed to vent the basement air to the outside as a temporary solution until I could get all the mold removed.
Uh, oh! It was clearly time to take aggressive action or my health, and that of my family, could suffer.
I plan to run mycotoxin testing on myself and journal the results, so stay tuned for updates on my progress. For now, let’s talk about mycotoxin illness and how it may impact your health.
What Is Mold Illness?
Mold is a fungus that’s usually found outdoors, but sometimes it can lurk in your home, office, or even your car or child’s school. When mold invades a water-damaged indoor area, watch out! It can cause mold illness, and you may dismiss the symptoms without realizing they’re causing many of your most bothersome health problems.
Buildings aren’t the only source of mold exposure, though. Did you know that mold can grow inside breast implants in some women?
Mold releases odorless mycotoxins into the air, which can really do a number on your health. Exposure to mycotoxins can cause mold toxicity, also known as mycotoxin illness or mold illness.
Likewise, mold creates other troublemakers known as volatile organic compounds (VOCs). If you notice a musty odor in a water-damaged area, these VOCs are to blame. And if you can smell them—and even when you can’t—you can inhale or swallow them. In some cases, mold can colonize your body, causing you to pump out mycotoxins from within.
Exposure to mycotoxins can trigger chronic inflammatory response syndrome—CIRS, for short. CIRS kickstarts excessive inflammation, which can impact pretty much any organ in the body. CIRS symptoms are the same as those caused by mycotoxins since CIRS is often the culprit behind mold toxicity.
Even in small amounts, mycotoxins and VOCs can harm the body. In fact, they’re considered carcinogens. They create a high level of damaging oxidative stress, which in turn harms the mitochondria of your cells. Think of mitochondria as the powerplant of your cells that fuel your body with energy. If you have a hard time getting out of bed in the morning and are dragging all day, your mitochondria could need some tender loving care.
It's important to remember that mold toxicity and mold allergy are completely different things. During mold allergies, your immune system reacts to mold spores. The result? A runny nose and itchy, watery eyes, etc.
Mold toxicity often affects more than just your sinuses and lungs, and it causes symptoms that can be mistakenly attributed to some other trigger.
Symptoms of Mold Sickness
Different types of mycotoxins can each cause specific symptoms. For example, the mycotoxin ochratoxin A leads to problems with brain or nerve function and may cause nerve pain or a hormone imbalance. This mycotoxin also attacks your immune system.
Whether or not you feel ill varies greatly. Even in the same environment, you may feel sick while your coworker or spouse feels just fine.
So, what causes those reactions? You can thank your genes for an increased vulnerability to mold. Nearly 25% of people living in the U.S. are genetically susceptible to mold toxicity. If you’re one of them, your immune system doesn’t identify and eliminate the mycotoxins as easily as other people’s systems do, so the toxins build up in your body.
There are more than 100 mold illness symptoms. I can’t list all of them here, but some of the most common ones include:
- Abdominal pain
- Anxiety
- Asthma (new-onset or worsening)
- Autoimmune disorders
- Bloating
- Brain fog
- Chemical sensitivity (symptoms that occur when exposed to chemicals or fragrances)
- Depression
- Diarrhea
- Digestive problems, like irritable bowel syndrome (IBS)
- Dizziness
- Fatigue
- Headaches
- Irritability
- Joint pain or stiffness
- Leaky gut
- Memory loss
- Mood swings
- Muscle pain
- Nausea and vomiting
- Poor immunity
- Sensitivity to bright light
- Sinus problems
- Skin irritation or rashes
- Skin sensitivity, even to light touch
- Sleep problems or night sweats
- Sore throat
- Thyroid problems
- Tremors
- Urinary incontinence
- Weight gain
Your Brain on Mycotoxins
Ochratoxin, the most common mold mycotoxin, greatly reduces dopamine levels, especially in areas of the brain linked to Parkinson’s disease. In addition to Parkinson’s disease, over time, mold toxicity puts you at risk for:
- Alzheimer’s disease
- Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease)
- Autism
- Multiple sclerosis
Tests for Mold Exposure
Just because you don’t live in a warm, humid part of the world doesn’t mean your home is safe from the problem. Mold can occur anywhere. Studies show that half of the buildings in North America may have water damage.
If you have mold toxicity symptoms, don’t write them off because your house is a new build or you can’t smell anything musty. Testing for mold is your best bet.
Because mold can also colonize your body—and especially your gastrointestinal tract—the problem might not even be in your current residence or office. Your previous home or workplace could be to blame. Mold can catch a ride on things like papers, books, and even your clothes. This means it can travel with you from place to place.
Here’s how to test your home for mold: use a do-it-yourself (DIY) mold testing kit, such as this one as a starting place. Want another option? Use a professional home inspector. I love We Inspect, but you can also find mold testing professionals in your area through the National Association of Mold Remediators and Inspectors (NAMRI).
You can also work with a functional medicine provider who will use a mold toxicity urine or stool test to detect the presence of mycotoxins in your body and help you create a personalized protocol to remove them.
Treating Mold Toxicity
Once you’re certain that you’ve been exposed to mold, how do you kick mold illness to the curb? I use this five-step approach:
- Ditch mold exposure either by moving or thoroughly treating and/or revamping your home or office. If you move, be careful what you bring with you. Mold can contaminate furniture, documents, books/bindings, clothing, and fabric.
- Have your functional medicine provider order baseline mycotoxin urine, and sinus testing to gauge your level of exposure. Stool testing for fungal dysbiosis is also encouraged. Your provider can recommend natural antifungals to kill any mold colonizing the GI tract, lungs, or sinuses.
- After six weeks of treatment, your functional medicine provider should retest your mycotoxin levels. If mycotoxins are still present, you may need to try a new antifungal treatment or increase the dosage.
- Help the body chase away the mycotoxins. Using natural binders and using products to boost bile production can help pull mycotoxins out of the body. Liposomal glutathione is a great choice for removing residual mycotoxins. Mold toxicity seriously decreases glutathione levels. As your body’s major antioxidant, glutathione fights the oxidative stress caused by mold. In some cases, you might need to sweat the mold toxins out of your body using an infrared sauna or sauna blanket. Be sure to hydrate and poop one to three times per day.
- Support your mitochondria and energy as well as insulin levels and hormone balance.
Feel Better by Fighting Off Fungus
Is mold toxicity causing your sickness, fatigue, or other health problems? As a functional medicine provider, I’ll find out the answer to that question. The process begins with a free 15-minute troubleshooting call. From there, I can order the right mold toxicity tests and interpret the results to find out whether we need to take steps to get rid of your mold exposure and treat your mold illness. I’ll develop a treatment plan to help you feel more energetic, clear-headed, and better overall. Sign up for a call today, so you can feel like your old self again.
Is Toxin Exposure Aging You Faster?
Is Toxin Exposure Aging You Faster?
Are you looking in the mirror every day and wondering how you can turn back the clock?
You’re in the prime of your life, but you are noticing wrinkles and fine lines where there used to be none.
You can’t seem to squeeze into your favorite jeans.
You feel an energy dip in the afternoon when you want to be present to your kids.
It seems like your mind has lost its sharp edge.
Your muscles are less toned, even when you double-down on your workouts.
After tackling work and home life, does it feel like you have nothing left over for your own enjoyment?
Unfortunately, you’re not imagining things. It’s real. Your cells are aging. You are aging. But it doesn’t have to be that way. Because you can turn back the clock.
I’m inviting you to get off the aging train. Keep reading to find out one of the most important steps you can take to slow the aging process. You can hold on to that youthful glow -and turn heads- now and well into your golden years.
Look and Feel Younger
Did you know that your biological age can be much younger than your chronological age?
Your chronological age is based on how many birthdays you’ve celebrated. Your biological age is based upon how old your cells think they are and how they feel. By turning back the clock on your biological age, you will no longer be a prisoner to your chronological age.
Here’s an example of young biological age…
I’ve taken up social dancing recently, a type called Casino that is from Cuba. Dance is a huge piece of how I stay younger. Dance brings me joy.
When we’re joyful, our cortisol levels are more balanced, our hormones are more balanced, our body functions better and we have more oxytocin, a love hormone that plays a role in social bonding.
Dancing is good for my health. I’m a better person when dance is part of my regular weekly routine.
A couple of weeks ago when I was out dancing, I saw a woman in her mid- to late 70s. Not only was she the life of the party, she was even getting down on the dance floor with the lead singer of the band! She was the poster child for someone who has a young biological age
I will be doing something right if I’m her age and have her energy and her outlook and her mood! I just looked at her and thought #lifegoals.
The point is: there are a lot of ways to be 75 or 80 years old. She’s found what feeds her soul. She found her place, her happy spot. Her chronological age might be chasing 80, but her biological age was much younger.
So what does dancing have to do with environmental toxins? You see, exposure to toxins is one of the most common things that cause our biological age to skyrocket. Your youthfulness—or your biological age—is an equation. You can slow down aging with things that bring you joy, a healthy diet, nutrients, building muscle mass, and more. You can speed up aging with stress, toxins, poor diet choices, drinking, staying up late, smoking, working out too much, radiation, and more.
Toxin exposure can make you look and feel older. Toxins trigger inflammation, damage DNA, shorten telomeres, and get in the way of healthy mitochondrial function.
The good news? There are ways to measure your toxin exposure and to detox your body. Let’s take a deep dive into how toxins age you faster. You’ll find out what you can do to kick toxins to the curb so you can feel and look more youthful.
Lead and Mercury and BPA, Oh My!
Everywhere you go and everything you do exposes you to toxins. They’re found everywhere from canned food to cash register receipts to some personal care products, children’s jewelry and toys, vinyl flooring, dust, and soil. Toxins lurk in the water you drink, the air you breathe, and the food you eat.
For example, lead—a chemical linked to heart disease and other health problems—is found in many places including:
- Electrical cords including Christmas tree lights
- Houses painted (and toys made) prior to 1978
- Imported candies and food
- Lead-glazed ceramics, china, leaded crystal, and pewter
- Some folk medicines, ayurvedic medicines, and cosmetics
- Some children’s jewelry and toys.
This article isn’t meant to go into detail about each and every toxin. Just know that toxins are out there and we’re exposed to them from the time we’re in the womb.
But don’t let this discourage you because there are ways to decrease your toxic burden. I will discuss more on how to detox later in this article.
A Telomere’s Worst Enemy
One reason why toxins age the body is because of their impact on telomeres. The genetic blueprint of our bodies is encoded on double-stranded DNA molecules called chromosomes. Telomeres are protective caps on the ends of chromosomes that make it possible for cells to divide without scrambling that important DNA information. Telomeres are often compared to those hard sections at the end of shoelaces that stop them from unraveling.
Telomeres grow shorter and shorter each time cells divide. Eventually telomeres get so short that cells can no longer divide, and instead they die.
What does telomere shortening mean for your body? The shorter your telomeres, the greater the chance you’ll feel and look older. Short telomeres are linked to a whole host of age-related problems, whether we’re talking about cancer, immune system and memory problems, inflammation and all the diseases that go with it, or skin wrinkling.
Toxins are basically out to get your telomeres. For example, every time you touch a cash register receipt or eat food out of a plastic container or can that’s not BPA-free, your telomeres will need to duck and cover because they might get a hefty dose of bisphenol-A (BPA). Even low-doses of this toxin speed up telomere shortening.
Likewise, lead exposure damages telomeres. This is an important way in which toxins age you faster.
How Toxins Do Their Dirty Work
Environmental toxins damage the mitochondria, the powerhouses that fuel our cells and give them energy to keep working their best. When toxins hurt the mitochondria, cells are injured and stressed, creating molecules that are pro-inflammatory and speed up aging.
Normally, inflammation benefits the body because it helps the body recognize and fight off infections or address naturally occurring damage to our tissues. This type of inflammation is low-grade and should have a beginning, middle, and end.
We have systems in our body that understand when the inflammation is needed and should resolve it in the same way firefighters strive to put out a wildfire before it gets out of control.
But when toxins damage our mitochondria, the checks and balances that the body usually puts in place to stop inflammation from spiraling out of control stop working.
The result? Inflammation rages out of control and goes on and on, causing a shift in the immune system and leading to more tissue damage, cellular aging, and chronic inflammatory diseases. For example, it can cause the immune system to attack itself, causing autoimmune disease.
Are You Suffering from Inflammaging?
As we grow older or are exposed to damaging substances like toxins, inflammation ramps up in the body like a fire that hasn’t been put out. Damaged mitochondria from toxin exposure create pro-inflammatory molecules, which can speed up aging.
Scientists coined a term for the inflammation that goes into overdrive when we age. It’s known as “inflammaging.” Aging plus inflammation is not pretty. It puts you at greater risk for many diseases that disable the elderly including heart disease, diabetes, and dementia. Out-of-control inflammaging can also cause wrinkles to pop up on your face, and you can say goodbye to your youthful appearance.
There’s another damaging process called oxidative stress, which goes hand in hand with inflammation. Reactive oxygen species (ROS) are the culprits behind oxidative stress. Some oxidative stress is healthy, but too much of it hurts your body. That’s why people take antioxidants—to protect themselves against too much oxidative stress.
Oxidative stress builds up in your body for many reasons, but toxin exposure is one of the most common.
Where Are Toxins Lurking?
Toxins are made by harmful bacteria in the gut and those in the water supply. We also can get exposed to toxins when we eat or drink, especially food that’s not organic or when we drink too much alcohol.
We breathe air and dust that contain toxins (such as mycotoxins from mold), which enter the lungs, travel into the mucous membranes in the sinuses, and drip into the throat. When we swallow, the toxins end up in the gut.
If your cells are exposed to lots of toxins—and heavy metals are some of the worst offenders—production of reactive oxygen species goes into overdrive and damages the mitochondria and weakens your body’s ability to protect you.
If the toxic burden is too high your mitochondria can’t repair themselves, which means the mitochondria can’t make enough ATP, the energy molecule that fuels your cells. The result? Feeling tired and dragging as you perform your daily responsibilities.
How Your Body Protects You Against Toxins
So what happens when you’re exposed to these toxins? Nrf2 to the rescue! The Nrf2 pathway in your body soothes inflammation and boosts your body’s production of antioxidants.
Aging, toxins, and infections weaken the Nrf2 pathway, which is why it’s important to increase levels of this powerful protein. I’ll talk more about a substance that activates the Nrf2 pathway later in this article, so you’ll be armed and ready to defend yourself against rapid aging.
Testing for Toxins
The good news? We can measure our toxin exposures by using a number of blood tests such as:
- Genova ION test to measure levels of the antioxidant glutathione, oxidative stress, and different liver detox pathways
- Testing for mycotoxins, or toxins from mold (Mycotox Panel by Great Plains Laboratory)
- Heavy metals testing (Mercury Tri-Test & Blood Metals Panel Quicksilver Scientific test)
- Environmental toxin burden panels (Great Plains Laboratory ENVIRO-Tox Panel).
How to Detox Your Body from Toxins
You don’t have to put up with a toxic brew of chemicals that harm your health and age you faster. Here are some ways to detox your body or avoid toxin exposure in the first place. These strategies can slow aging and lead to younger looking skin and a healthier body.
- Use an Infrared Sauna. Pull toxins out of your body by sweating them out using an infrared sauna or infrared sauna blanket.
- Dry Brushing. This method is thought to open pores and promotes sweating to release toxins through the skin.
- Install a Good Water Filter. To purify the water supply, use a water filter not only in the kitchen but also in the bathroom so you don’t breathe in (or bathe in) toxins while you shower.
- Eat Organic Food. To reduce your toxin exposure in the first place, eat organic food. Researchers have found that people eating an organic diet have lower levels of pesticides in their urine samples.
- Promote Bile Flow. After the liver detoxifies toxins, the byproduct is removed from the body through bile, which is excreted in the intestines. Make sure you’re pooping daily. If not, try eating more fiber, taking a magnesium supplement, and addressing other root causes of constipation.
- Drink Lots of Water and Liquids. You’ll need to drink enough water or other healthy liquids like herbal tea to keep toxins moving through the kidneys and out through the body.
- Support the Nrf2 Pathway. Sulforaphane, which is found in broccoli, is an Nrf2 activator. It’s a good idea to eat lots of this vegetable to reduce inflammation and oxidative stress and to keep the mitochondria healthy. Just make sure you choose the organic variety in order not to expose yourself to even more toxins. Healthcare practitioners may offer supplements that contain other Nrf2 supportive combinations of herbs and nutrients.
- Keep Your Mitochondria Happy. NAD+ is just one supplement that I use in my clinical practice to support mitochondria health. You can read more about this nifty nutrient here:
- Take a Prebiotic and Probiotic. These can protect your gut against bacterial-produced toxins. I recommend Megaprebiotic and Megaspore.
Other Factors That Can Make You Look and Feel Older Than You Are
Many factors besides environmental toxin exposure can age you faster. These include:
- How you sleep or don’t sleep
- Ongoing infections in the gut or bacteria-related toxins known as endotoxins
- Smoking cigarettes
- Solar radiation
- Eating too many processed and artificial foods
- Not spending enough time in nature
- Being under a lot of stress
- Ongoing psychoemotional challenges (experiencing trauma)
All of those things impact how fast or slow we age, more so than the number of years you have on the planet. They’re the driving force behind whether you’re going to be dancing salsa when you’re in your 80s or too tired to get off the couch.
How to Slow Aging with My Help
Are toxins causing you to age faster? That’s what we will find out if you choose to reach out to me for a free 15-minute troubleshooting call. As a functional medicine provider, I can order the right tests and interpret the results to find out which toxins are damaging your telomeres and mitochondria. Then I’ll develop a treatment plan to detox your body and give you a more youthful appearance, increased energy levels, and a sharp memory—to name just a few healthy aging benefits. Sign up for a call today, so you can feel and look years younger.
What is a Functional Medicine Health Coach?
As a Functional Medicine Health Coach, I combine my training and knowledge of Functional Medicine principles and approaches with my expertise in coaching psychology, behavior change and more. My work is aimed at empowering people to take charge of their health, and guide them to make lasting, sustainable changes to optimize their wellbeing.
In my years of working in Functional Medicine, I witnessed a gap that some people experienced. While these folks invested their time and money into meeting with highly qualified practitioners who provided them with very comprehensive treatment plans, they couldn’t figure out how to take that plan and make it work in their lives. They understood the directives they were supposed to follow to get healthier, but they couldn’t figure out how to go about doing it. This gap often resulted in frustration and struggle, impeding their success in reaching their goals for improved health.
This spurred me to create a Functional Medicine Health Coaching practice to address the need for support and guidance on 1.) how to implement treatment protocols, along with 2.) how to make Lifestyle changes that would successfully lead to reaching goals, and 3.) how to cultivate potential for greater fulfillment and wellbeing in life.
What does Functional Medicine Health Coaching offer me?
Studies show that people have much greater success in creating positive, long- lasting changes when they have the support and guidance of a professional wellness coach. Coaching improves the efficiency of your journey and ensures a greater outcome achieved. Athletes and high-performance professionals wouldn’t think of trying to achieve their goals without the guidance of a coach.
What can you expect from Functional Medicine Health Coaching?
- Mentorship and guidance
- Education
- An objective perspective
- Opportunity for self-discovery and growth
- Strategies to support habit changes
- Empowerment to change and progress
- Tools to support motivation
- Accountability
- Individualized action plans, and much more…
These would be difficult to access if trying to do this alone.
* My personal style blends knowledge and science with intuition and wisdom derived from many years of working with patients in healthcare. I employ many holistic tools, modalities and techniques based on individual needs and presentation.
Get Support from a Functional Medicine Health Coach
Functional Medicine Health Coaching is useful whenever you’re attempting to make changes in habits and patterns aimed at improving the quality of your wellbeing. Taking steps to upgrade Lifestyle habits is an investment in your health. Simple changes can lead to huge strides in feeling better, having more energy and vitality, improving the quality of your health, being more content in your life, and ultimately living with greater fulfillment.
What exactly are “Lifestyle Factors?” These are the choices you make every day that define how you live, impacting the quality of your health and your life.
There are nine pillars that lay the foundation for our health and well-being. They include:
- Nutrition
- Exercise and Movement
- Sleep
- Stress Management
- Positive Relationships
- Creativity
- Meaning and Purpose
- Connection to Nature and Environment
- Avoidance of Toxic Substances
If I’m working with a Functional Medicine healthcare provider, why do I need a coach?
Functional Medicine providers are highly skilled at identifying the root cause of your ailments and devise brilliant treatment plans to alleviate your condition. However, they commonly don’t have the bandwidth nor the skills to help guide you on how to make behavior changes or integrate treatment protocols into your life.
Collaboration with a Functional Health Coach expedites the process. When these two professions are employed in tandem, it creates a synergy that makes a recipe for success and the results are beyond impressive.
Changing habits and patterns can be complicated. It becomes easier when you have someone who is knowledgeable on the nuances of your treatment plan - a coach to guide and educate you how to carry it out, support your motivation, provide accountability and help keep you on track. Results are often accelerated, and more lasting levels of change are achieved. It’s your willingness and dedication to the process that brings the alchemy to fruition!
Meet Health Coach: Catherine Willows, RN, BA, FMC-HC, NBC-HWC
Catherine is a Registered Nurse and a seasoned healthcare professional with years of experience in a wide variety of clinical settings. Her long-standing passion for integrative and holistic health practices led her to studying and certifying in many holistic modalities, including herbalism, energy work, somatic therapies, and much more. This eventually led her to serving as a leader in the Obesity Prevention Initiatives in Chicago, and brought her to Functional Medicine where she worked as Clinical Services Director for Dr. Mark Hyman’s clinic, the UltraWellness Center. Catherine is a Functional Medicine Certified Health Coach, and a National Board-Certified Health and Wellness Coach.
If you really know me, you would know that…
I am dedicated to personal growth. I believe we’re all here to become our best version of ourselves. My purpose is dedicated toward helping others become their best version of themselves too!
I deeply value Creativity and Creative Expression. I believe everyone is inherently creative, even though many people have lost touch with it. Through Creativity, we have the opportunity to express our unique gifts in the world. I make it a practice to carve out space for Meditation, personal Freedom, Creativity and Inspiration - as these are essential to my wellbeing.
I love the arts. I love to engage in art-making, painting, fiber arts and more.
I love Nature - the Beauty of Nature - all its seasons and elements, plants and animals alike. I believe that the Essence of Nature has much to teach us about how to live in greater balance, and our individual health is intimately connected with the health of the planet.
I am a life-long learner with burning curiosity that drives me to continuously expand my knowledge in many areas of interest.
I enjoy riding my bike through the backroads of the Berkshires, kayaking, gardening and spending time with my Australian Shepherd.
If I could snap my fingers and be anywhere in the world, I would be
along the coast in Portugal I love to travel, and being seaside is one of my favorite places - among natural beauty, in a place rich in culture and arts, with healthy food, a temperate climate zone, and a more easeful lifestyle.
New Functional Medicine Health Coach Program
Have you heard about my new group coaching program yet? This hour-long virtual gathering will be offered to current clients twice monthly and hosted by Catherine Willows. Its aim is to provide you with greater support in making lifestyle choices and habit changes to bring your health to a better place. Catherine’s next session is February 1st – get the full scoop here.
Always Tired? It Could Be Your Mitochondria
Feeling tired and run down? Girlfriend, I know how frustrating it can be! But don’t accept low energy levels. You can reclaim your youthful energy and conquer the world.
You can wake up refreshed, take care of your home, dominate at work, and crush it at the gym.
And you won’t need three cups of coffee to feel that way!
What do you need to do to have boundless energy? Taking care of your mitochondria is at the top of the list.
Mitochondrial health is the next big thing to think about in regards to getting back your youthful energy. More and more research is published every day on this cutting-edge topic, which is why mitochondrial support is a big part of my treatment for many patients.
Since mitochondrial dysfunction is one of the most common causes of fatigue, this is one of the most important blog posts you’ll ever read.
Mitochondria that aren’t working well can cause all sorts of problems, including weight gain, insulin resistance, skin aging, and much more. I’ll talk more about those problems in a series of blogs coming soon.
Meanwhile, in this article, I’m going to dive into the ways that mitochondrial dysfunction can cause your energy levels to drop—and what you can do about it.
What Are Mitochondria and How Do They Boost Your Energy?
Mitochondria are fascinating little structures. They’re the powerhouses of your cells, manufacturing energy that powers your entire body.
The cellular fuel that mitochondria make is known as adenosine triphosphate, or ATP for short. Without ATP, your cells couldn’t work and you wouldn’t be able to function. With enough ATP, you’ll have lots of youthful energy.
Within each mitochondrion, there is an assembly line that takes proteins, carbohydrates, and fats derived from food, breaks them down, and manufactures ATP. Every cell in the body needs energy (ATP) to do its job. The heart, brain, liver, muscles, and kidneys are high in mitochondria because these organs need lots of energy to work.
When your mitochondria are humming happily along, you have lots of energy and feel like you can take on the world.
Symptoms of Mitochondrial Fatigue
So how do you know if weak mitochondria are the cause of your low energy or other health problems? These symptoms will clue you in:
- Fatigue in general
- Weakness or lack of endurance during exercise
- Excessive body pains or muscle aches after exercise
- Longer than average exercise recovery or feeling wasted the day or two after exercise
- Weight gain, slow metabolism, insulin resistance
- Aging skin and rapid wrinkling
- General all-over body pain, muscle weakness (myopathy)
- Brain fog
- Migraines
- Anxiety and depression
- Difficult to cope with stress
Your Mitochondria During Aging
As you age, the mitochondria can break down and not work as hard. The number of mitochondria actually decreases during aging. This means mitochondria make less ATP, so the body doesn’t make enough fuel to keep it running, just like a car that runs out of gas.
If you want to see young mitochondria in action, watch children run around a room or in the park. They’re little bundles of energy, fueled by their youthful mitochondria.
Unfortunately, mitochondrial problems due to aging cause your body to make too many reactive oxygen species (ROS), also known as free radicals. These chemicals can harm your cells, creating a vicious cycle of yet more damage to the mitochondria. In addition, too many ROS smothers the creation of new mitochondria and stops the body from getting rid of damaged mitochondria.
So what does it mean for you when your mitochondria get messed up during aging? It drops your energy levels and you feel too tired to get things done.
Other Reasons for Mitochondrial Problems
Besides aging, other factors can make the mitochondria scream out for help. These include:
- Alcohol
- Antibiotics
- Environmental toxins
- Hereditary factors
- High-fructose corn syrup
- Inadequate nutrients
- Not enough physical activity
- Overeating
- Smoking
- Statin drugs
- Stress
- Vegetable oils (high in omega-6 fatty acids)
How To Know If Your Mitochondria Are Healthy
Your functional medicine provider can order an organic acids test (OMX Metabolomics or the ION). These tests will tell you whether your mitochondria are happy.
Your functional medicine doctor can also order a test to measure your telomere length. Telomeres are caps at the end of your chromosome—like the ends of shoelaces that keep them from unraveling.
Telomeres become shorter and shorter with age. Your numerical age may not be the age your cells think they are. By measuring telomere length, you can get a good idea about your cellular age.
Finally, testing adrenal function can let you know if your cortisol levels are off. High cortisol can block mitochondria function.
A Secret To Keeping Your Mitochondria Healthy
One of the best ways to give your mitochondria some TLC? Make sure you have plenty of nicotinamide adenine dinucleotide (NAD+).
Your mitochondria need NAD+ to make ATP and to fuel your energy levels. On the other hand, low levels of NAD+ can damage the mitochondria and make you feel like you just ran a marathon even if you haven’t gotten out of bed for the day.
Low NAD+ also shortens your telomeres. Think of NAD+ as the “gas pump” you need to fill your cells’ “gas tank.”
Between the ages of 40 and 50, NAD+ levels drop to 50% of what they were when you were younger. In some organs and tissues, your NAD+ levels can drop by as much as 90% to 100%. This freefall in NAD+ means you’re not making as much ATP, which makes you feel like you’re running on empty.
Because your body needs NAD+ to make ATP, making sure you’re getting enough NAD+ ensures that all areas of your body are healthy including the adrenals, thyroid, brain, and circulatory system. For example, NAD+ protects the neurons in the brain by restoring mitochondrial health. This keeps your brain from feeling worn out.
How do you raise NAD+ levels? You can take one of several different types of NAD+ supplements. I take it in a collagen product called Thorne Collagen Plus. It’s also available as liposomal NAD+. Many people use either a nicotinamide riboside or nicotinamide mononucleotide supplement to boost NAD+ levels.
Other Mitochondrial Support Supplements
Many other supplements support mitochondrial health. Be sure to work with your functional medicine provider to find out which nutrients you really need. By ordering the right tests, your doctor can create a personalized and more effective protocol that includes supplements for mitochondrial support.
Here are the most common and effective mitochondria support supplements:
- Adaptogens – These are botanicals that help the body cope with stress. Stress can cause cortisol levels to go through the roof, and high cortisol is one of the mitochondria’s worst enemies. Stress also shortens telomeres.
- Alpha lipoic acid – An antioxidant that encourages ATP production.
- Coenzyme Q10 – An antioxidant that plays a crucial role in mitochondria’s ability to make ATP. CoQ10 is one of the mitochondria’s best friends. It stops the mitochondria from making too many reactive oxygen species (ROS). CoQ10 is the cornerstone of a mitochondrial support program.
- Curcumin – Improves mitochondrial health by reducing inflammation.
- Probiotics – Probiotics improve mitochondrial function and your body’s ability to make energy.
- Carnitine – This amino acid boosts fatty acid metabolism in the mitochondria. Fatty acids are building blocks for ATP.
- Glutathione – An antioxidant involved in mitochondrial health.
- Magnesium – This mineral acts as an antioxidant in mitochondria, blocking the production of too many ROS and improving mitochondrial dysfunction. An organic acid test can tell you which type of magnesium your mitochondria need the most—for example, magnesium citrate.
- Omega-3 fatty acids – These are an important component of the mitochondrial membrane.
- Vitamin B12 – Your body needs enough of this vitamin to make energy.
- Vitamin C – An antioxidant that promotes the production of carnitine, which in turn keeps your mitochondria in tip-top shape.
- Zinc – Stops the mitochondria from making too many ROS.
Getting Rid of Chronic Fatigue and Mitochondrial Dysfunction
As a functional medicine provider, I can work with you to answer your question: “Why am I always so tired?” I’ll order the proper testing to see if your mitochondria need a boost. Then I’ll let you know what supplements to take and other steps that can get rid of your fatigue and make you more productive and full of energy.
I’ve successfully used this approach in many patients. That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you. We’ll start there, and if you come on board as a client, I’ll order a full lab work-up.
The goal? To boost your energy levels, improve the health of your mitochondria, and give you the stamina to tackle life’s daily challenges.
Weight Gain in your 40s
You’re eating the same as you always have, still getting the same amount of exercise… but your pants are suddenly tight.
Surprise! It’s menopause to blame… again.
Of course there are the night sweats, hot flashes, and mood swings, but gaining weight in menopause (or the 10 years leading up to it!) is one of the most common (and dreaded) signs of this massive hormonal change.
But like any other sign of menopause, just because it’s common, doesn’t mean it has to happen to you.
The first step to preventing or reversing weight gain in peri-menopause is to understand why it happens on a chemical and hormonal level.
From there, we can focus on holistic changes that don’t just make you drop a few pounds - they create an overall feeling of well-being, happiness, and health so you can thrive in this new season of life. Menopause doesn’t have to suck - I promise!
Why Do Women Gain Weight in Menopause?
Menopause isn’t just the end of your period - it’s a massive hormonal shift in your body, only comparable to puberty or pregnancy. As women, hormones are the ruler of almost everything that happens with our bodies, from our energy level to weight to mood.
For a complete explanation of the hormonal changes that occur during menopause, read this blog.
Those hormone changes interact with the various mechanisms that control weight. (Yes, weight is about a lot more than just “calories in and calories out!”)
Here are just some of the mechanism involved in weight changes:
- Gut Microbiome Dysbiosis
- High cortisol (adrenal/nervous system issues)
- Chronic inflammation
- Thyroid disease
- Insulin resistance and fatty liver
- Medications
- Lack of movement
- Mitochondrial dysfunction
- Hormonal changes
In menopause, the major hormonal change is first fluctuating and eventually lower levels of estrogen and progesterone. Those changes impact everything from glucose regulation to sleep, and those, in turn, impact weight.
In particular, the hormone changes of menopause can lead to increased belly fat. That increased belly fat can then fuel excess estrogen progesterone, intensifying the fluctuations that can lead to symptoms.
Sleep, Menopause, and Weight Gain
One well-known side effect of menopause are sleep problems - from trouble falling asleep to waking suddenly with night sweats. Research suggests that the sleep disturbances caused by menopause may also be at least partly to blame for the weight gain common in menopause.
The fluctuating estrogen levels common during the menopausal shift can trigger increased appetite, hot flashes, and night sweats, impacting sleep quality. The late-night combination of increased hunger and inability to sleep is also a perfect set up for late-night binge eating.
Even if your eating hasn’t changed, lack of sleep makes it harder to lose body fat, increases hunger and cravings for carbohydrate foods, and even inhibits muscle gain. Simply sleeping less may impact your body’s ability to manage glucose (blood sugar), promoting weight gain. In one observational study of over 150,000 women, those who had night sweats and hot flashes for a longer period of time (and therefore a longer period of disrupted sleep) also had a greater risk of developing diabetes - as much as 18% higher.
But it’s not just disturbed sleep that can cause issues with glucose levels - the normal hormonal changes of menopause can wreak havoc on your blood sugar as well.
Blood Sugar and Gaining Weight In Menopause
For women, estrogen and progesterone levels impact how we maintain healthy blood sugar levels. Changes in your hormone levels can impact blood sugar and may even contribute to insulin resistance.
Insulin resistance is when the body becomes desensitized to insulin, the hormone that controls blood sugar levels by acting like a key and “unlocking” cells so they can absorb sugar from the bloodstream. When insulin resistance occurs, the “key” stops working, and no matter how much insulin is present, it is unable to do its job. This creates a state of chronic elevated blood sugar, and can even lead to diabetes over time. Signs and symptoms of insulin resistance include weight gain (especially around the midsection), high triglycerides and LDL cholesterol, hypertension, gout, skin tags, and androgen excess, including PCOS.
Estrogen also plays a major role in the production of insulin, and can contribute to both insufficient and excess levels of insulin that contribute to insulin resistance. Estradiol, one type of estrogen, increases glucose sensitivity by enhancing the ability of the mitochondria to turn glucose into energy. Lower estrogen levels may then decrease glucose sensitivity, as well as impair the cells’ ability to convert glucose that has been absorbed into energy, causing a temporary energy crisis, even if enough glucose is being consumed. For you, this can feel like always being hungry, especially for carbs and sweets.
Progesterone, which has an anti-androgen effect, may also be protective against excessive insulin levels, as excess androgens stimulate the production of more insulin. (Overproduction of insulin is one aspect of insulin resistance.) When progesterone levels drop during menopause, this anti-androgen effect is lost. This is why hormone specialists like myself consider progesterone to be a weight loss hormone (just not artificial progestins, which can have the opposite effect).
These hormonal changes can result in elevated blood sugar and insulin resistance. In one study, hormone change symptoms like hot flashes were linked to both increased insulin resistance and higher blood sugar levels. In other research, women were less likely to experience hot flashes when blood sugar was elevated above normal, and more likely to experience them when fasting, showing the extremely complex relationship between menopause symptoms and blood sugar.
In addition, as estrogen and progesterone levels decrease, it can lead to a state of testosterone dominance, which can also contribute to insulin resistance.
Ketones, Menopause, and Your Brain
Weight gain isn’t the only potential consequence of these changes. The brain’s primary fuel source is glucose, and the brain alone consumes more than 20% of the glucose in your bloodstream.
Because estrogen plays a role in the cells’ ability to burn glucose, when estrogen levels drop, cells must switch from burning glucose for fuel to burning ketones, and this may have an impact on brain function if the switch between the two fuel sources isn’t smooth. You might feel this as brain fog, forgetfulness, and fatigue.
To navigate this transition, the brain needs to get better at using ketones. And to do that, you need whole body insulin sensitivity and metabolic flexibility. Let’s talk about how you can achieve those goals.
How To Stop Menopause Weight Gain
The causes of weight gain in menopause are complex, so the solution needs to be multi-faceted. Here are just some of the suggestions I work with my own clients on:
Do Exercise You Love and Build More Muscle
Aim for 3-4 hours per week of muscle-building activity, as well as a mix of high intensity and steady state cardio. For a bonus, incorporate up to two fasted workout sessions per week. After you’ve exercised, refuel with 20-40 grams of protein in the hour after training.
Optimize What You Eat
I recommend a blood-sugar balancing diet, which typically involves lowering carb intake or rotating a keto-style diet with a moderate-carb-intake, mediterranean-style diet rich in above-ground veggies, polyunsaturated and unsaturated fats like olive oil, nuts and seeds, avocado, and leaner proteins. In general, your food should be anti-inflammatory and plant-forward, with a lot of veggies at every meal. Avoid liquid calories.
Optimize When You Eat
A 10-12 hour eating window (followed by at least a 13 hour fast), and 3 meals without snacks is ideal for insulin sensitivity. Focus on eating protein at your first meal, and have it no later than 10 AM. Research suggests eating the biggest meal of the day at breakfast (instead of dinner) can also help promote weight loss.
Test For Food Intolerances
While not a factor for everyone, sometimes removing foods you’re intolerant of can reduce inflammation and clear the path for effortless weight loss. After testing revealed an intolerance, just removing eggs from my diet allowed me to lose 6 pounds without any other changes.
Find Your Carb Sweet Spot
In general, menopausal women need fewer starchy foods than they did when they were younger. (I know, it isn’t fair!) Each individual has their own “sweet spot” for carb intake depending on activity levels and metabolism. Choose complex carbs, and aim for 30+ grams of fiber daily. Eat the bulk of your carbs during your most active part of the day or right after you exercise.
Test For & Treat Insulin Resistance
Signs of insulin resistance include:
- Waist measurement over 33 inches/85 CM
- Elevated C-Reactive Protein (CRP)
- High triglycerides and LDL
- HBA1c above 5.6%
- Continuous Glucose Monitor readings high (above 140)
- HOMA-IR index
- Fasting insulin above 5, especially above 10
For treatment, I like to use organic acid testing with my clients to personalize nutrients that influence insulin sensitivity, such as ALA, magnesium, chromium, bitter melon, cinnamon, and gymnema. Magnesium is one supplement I recommend to almost everyone. My favorite form is magnesium glycinate, which helps calm the brain and promotes better insulin sensitivity.
Stabilize Estrogen
Test your estrogen levels and then use supplements like DIM, CDG, IC3, and phytoestrogen-rich foods like ground flaxseed to stabilize levels if estrogen is high. If estrogen is low, and you’re in perimenopause or early menopause - consider bioidentical replacement.
Use Hormone Replacement Therapy Strategically
Learn about the safety and efficacy of hormone replacement therapy, plus how I use it successfully with my clients, in this blog post.
Get Enough Sleep
Make 7.5-8 hours of sleep a night a priority. If you’re struggling with insomnia, I can help with strategies for increasing melatonin and decreasing nighttime cortisol. Some easy places to start: turn off screens at least 1.5 hours before bed, and consider wearing blue-blocking glasses, too.
Support Your Liver, Thyroid, and Gut
The liver and gut both play a major role in clearing out used estrogens. Lower estrogen levels can also negatively impact the gut microbiome and increase intestinal permeability. Check for signs of fatty liver, and if you aren’t pooping daily, let’s fix that. Test your thyroid function and support it with adequate levels of iodine, which also helps with hormone processing.
Get Expert Help for Gaining Weight in Menopause
Advice to just eat less and exercise more to lose weight gained in menopause misses the mark. Between fluctuating hormone levels, impaired sleep, and blood sugar changes, the causes of weight gain are complex. What you need is a holistic plan that addresses all aspects of weight gain so you can lose weight without starving yourself or feeling miserable.
I mean it when I say that menopause doesn’t have to be a miserable process. Helping women navigate menopause while looking and feeling their best in my passion. If you’d like support, book a free consult with my team. We’ll start with a deep dive into your health history so we can understand the full picture of you. Then, we’ll develop a customized plan for supporting your health goals, and be with you every step of the way.
>>> Book a FREE 15-Minute Consult to Discuss Your Health Goals Today
The Causes of Hair Loss in Women
Your hair is your pride and joy, but lately you’ve noticed hair thinning or hair loss.
It’s heartbreaking, I know.
The bad news? There is never going to be “just take this supplement” kind of answer, because there are so many drivers behind hair loss in women.
The good news? By digging down to the root cause of the issue, in many cases you can have thicker, fuller hair once again.
So what causes hair loss in women? Glad you asked. Because in this blog post, I’m going to answer that question and let you know the natural treatments for this common and frustrating problem.
Searching for Clues
When seeing a patient who complains of hair loss or hair thinning, I look at the symptom picture and history.
Most importantly, I observe the type of hair loss.
If the hair loss is patchy, it could signal autoimmune psoriasis. Patchy hair loss could also suggest alopecia areata, an autoimmune condition that causes hair loss.
Overall thinning tends to be a sign of hormonal hair loss in women, which may be due to high cortisol and stress or estrogen or progesterone imbalances. Overall thinning could also be a symptom of nutrient deficiencies.
What Causes Hair Loss in Women?
There are many reasons for hair loss in women. That’s why it’s important to work with a functional medicine provider to help you figure out the cause (or causes) of your hair loss. (more on functional medicine providers later).
Menopause and Perimenopause
As many as 40% of women notice their hair thinning in the years before and during menopause. This isn’t a given. It’s not like it happens to everyone. But it’s common enough to include it in this blog post.
Hair is vulnerable to falling out after a drop in estrogen and progesterone, which occurs during menopausal stages. When these hormones fall, hair may become thinner and grow more slowly.
Medications
A number of prescription drugs can cause hair loss or hair thinning. Here are a few of the common culprits:
- Birth control pills
- Chemotherapy
- NSAIDS
- Acne medications
Your DNA
Unfortunately, hereditary hair loss is the most common cause of hair loss and the one that is the most difficult to treat. This type of hair loss is typically gradual and involves a receding hairline and bald spots in men and a thinning of hair along the crown of the head in women.
Blood Sugar Issues
Elevated insulin levels in women can cause excessive production of male hormones, excess levels of free testosterone, or increased sensitivity to male hormones. Androgens are a group of sex hormones found in all genders, but men make more of them. Important for bone, muscle, sex drive, and sexual development, androgens include testosterone, androstenedione, dihydroepiandrosterone (DHEA), DHEA-sulfate, and dihydrotestosterone (DHT).
When these male hormones go unusually high in women, it’s called hyperandrogenism and may promote acne, hair growth on the face, or a deep voice. It can cause hair loss at the front and sides, in the male pattern. Women with insulin resistance and/or polycystic ovary syndrome (PCOS), for example, typically have high levels of testosterone (or it’s metabolites) due to high insulin levels. These women are also prone to hair loss.
But testosterone is not the big culprit behind hair loss, it is testosterone’s downstream metabolite- dihydrotestosterone - which is ultimately responsible for hair loss. Testosterone converts to DHT thanks to the enzyme, 5-alpha reductase. Many hair loss supplements try to block this enzyme.
If a woman or a man is insulin resistant, they produce more DHT. DHT can trigger the death of hair follicles. In fact, the main culprit behind hair loss is not testosterone itself but rather the level of DHT binding to receptors in hair follicles.
Hormonal Hair Loss in Women
Imbalances in hormones can lead to hair loss. If any of the following hormones are out of whack, it could lead to losing hair:
- Estrogen
- Follicle stimulating hormone
- Luteinizing Hormone
- Progesterone
- Prolactin
- Testosterone
Another hormonal imbalance that can lead to hair loss is high cortisol levels, combined with low DHEA. High cortisol levels are the main reason why stress is involved in hair loss and thinning.
Low levels of sex hormone binding globulin (SHBG) also can cause hair loss. SHBG is a protein that grabs on to excess hormones. If it is low and your free testosterone is high, your hair loss treatment should include both increasing SHBG and lowering testosterone by balancing all hormones.
Mercury and Other Toxins
Exposure to some heavy metals are to blame for certain cases of hair loss. Hair absorbs metals like a sponge and could affect hair growth. Exposure to these metals also cause symptoms like fatigue, depression, insomnia, irritability, and memory loss.
Thyroid Problems
The thyroid produces hormones that facilitate and regulate cell reproduction, so thyroid disorders—hypothyroidism and hyperthyroidism—can affect hair growth.
Nutrient Deficiencies or Excesses
Certain nutrient deficiencies—including riboflavin, biotin, folate, and vitamin B12—are linked to hair loss. Micronutrients and macronutrients play an important role in follicle development and regulating immune cell function, which is involved in healthy hair growth.
But don’t rush to load up on biotin for hair loss! Biotin levels that are too high, as in people who take biotin supplements, can harm the thyroid gland and interfere with thyroid lab tests. High biotin also can cause insomnia, digestion issues, skin rashes, and problems with insulin release. If you’re going to supplement with biotin, I recommend a supplement that has lower levels of biotin such as Viviscal Pro Hair Health.
To prevent low levels of key nutrients, take a high-quality multivitamin daily and get checked regularly for nutrient deficiencies, including iron and ferritin levels. You can also take a B vitamin complex to make sure you’re not deficient in any of the B vitamins linked to hair loss.
Autoimmune Issues
In autoimmunity, your immune system is triggered and mistakenly attacks a part of your body, a phenomenon called molecular mimicry.
Alopecia can refer to a number of hair loss conditions, but relevant to the discussion on autoimmunity is alopecia areata, an autoimmune disease that causes the body’s immune system to attack hair follicles. In cases of autoimmune hair loss, we have to dig deep for the root causes of autoimmune disease to bring back hair growth.
Other Causes
Other causes of hair loss in women include using harsh chemicals or hairstyles that pull on the hair a lot. Dieting and calorie restriction can cause hair thinning or hair loss. In addition, inflammation of any cause can lead to hair loss or thinning. What’s more, women often lose hair during the postpartum period. Read my blog post on postpartum and hair loss here.
Case Study — Here’s How It Works
This is a recent hair loss case from my clinic. It is still in progress, but I’m including it to show you what it looks like to address the factors involved in hair loss.
The client was a 48-year-old female. I’ll call her Jill. She had put on more weight around the middle, was on a low-carb diet, suffered from insomnia, and had rapid skin aging and hair loss.
Jill’s first test with another practitioner showed she had low estrogen (estradiol), progesterone, and DHEA, as well as relatively high testosterone, although not out of range. The practitioner jumped to address her hormones, but not in a comprehensive way. She was given progesterone, no estradiol, and nothing was done to address her testosterone levels. The practitioner also did not evaluate insulin resistance or glucose sensitivity.
The next test showed low estradiol, progesterone levels through the roof, and very high testosterone. This was likely due to the fact the practitioner had given her too high a DHEA dose, since the body converts DHEA to testosterone.
When she began seeing me, her symptoms had become worse. I didn’t attempt to adjust her hormone protocol right away because it was designed by another provider and she wanted to wait before changing it. She gained more weight and was sleeping worse. Her skin aging also was worse, she had developed mild acne, and was moody and irritable.
I was concerned about her very high hormone levels in relation to a very low estradiol. I tested her for blood sugar balance to see if it might be part of the mix. I thought stress and cortisol might also explain her hormone imbalances and hair loss.
I had her detox for three months to bring down her progesterone levels using herbal detox support to help the liver clear out the excess hormones and lower her SHBG. I also put her on herbal androgen blockers, which protect the body from too many circulating androgens. In addition, I focused on blood sugar control after finding out she was mildly insulin resistant. I tested her SHBG, gave her low-dose estradiol therapy, and began adrenal support. I had her stop taking DHEA at first because her levels were high, but added it back in at a much lower dose at six weeks, when her levels returned to normal.
Hormonal balance is still on the radar. Jill will need progesterone at some point, and I plan on retesting her after the three months’ detox period.
Jill’s making progress. She dropped eight pounds without changing her diet or activity level. She is sleeping better most nights. Her skin has improved moisture and fullness. She still sometimes has a tough time falling asleep at some times of the month, but progesterone treatment should help with that. I anticipate her symptoms—including her hair loss—will resolve after we finish balancing her hormones and eliminating other causes such as insulin resistance.
Helping You Pinpoint the Cause
If you’re losing hair, it’s best to work with a functional medicine provider to identify the root cause of the problem. Toxins, hormonal imbalance, malnutrition, blood sugar issues, or an autoimmune process are just a few of the possibilities that must be ruled out. Your doctor can order the right tests to figure out the reason for your hair loss. Then he or she can recommend potential remedies.
As a functional medicine provider, I’ve successfully used this approach in many patients. That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you. If after the call you come on board as a patient, I’ll suggest ways to balance hormones and address other causes of hair loss. We’ll work together to revitalize your health and get back your magnificent mane of hair at the same time.
Pros and Cons of Hormone Replacement Therapy
Mood swings, hot flashes, nigh sweats, weight gain, loss of libido: these are just some of the most common “symptoms” of menopause.
Is it any wonder most women dread this transition?
But what if there was a way to skirt menopauses negative side effects completely, and sail through this major change without sweating, screaming, or stress? According to some, the secret to making it through menopause is hormone replacement therapy (HRT).
But is hormone replacement therapy right for you? Today, let’s talk what happens in the body on the hormonal and chemical level during perimenopuase and menopause, how hormone replacement can and can’t help, and options you have to support this transition even if you’re not interested in HRT.
Menopause vs. Perimenopause: What’s The Difference?
Menopause is defined as going 12 or more months without a menstrual cycle. Perimenopause is the time period - usually several years - leading up to menopause. It’s a transition period sometimes thought of as “puberty in reverse.”
The average age of menopause in the Untied States is 51, and perimenopause usually stars 4-10 years before that. For some women, perimenopause symptoms begin as early as age 35. And if you need another reason to quit, research has shown smokers reach menopause at a younger age than non-smokers.
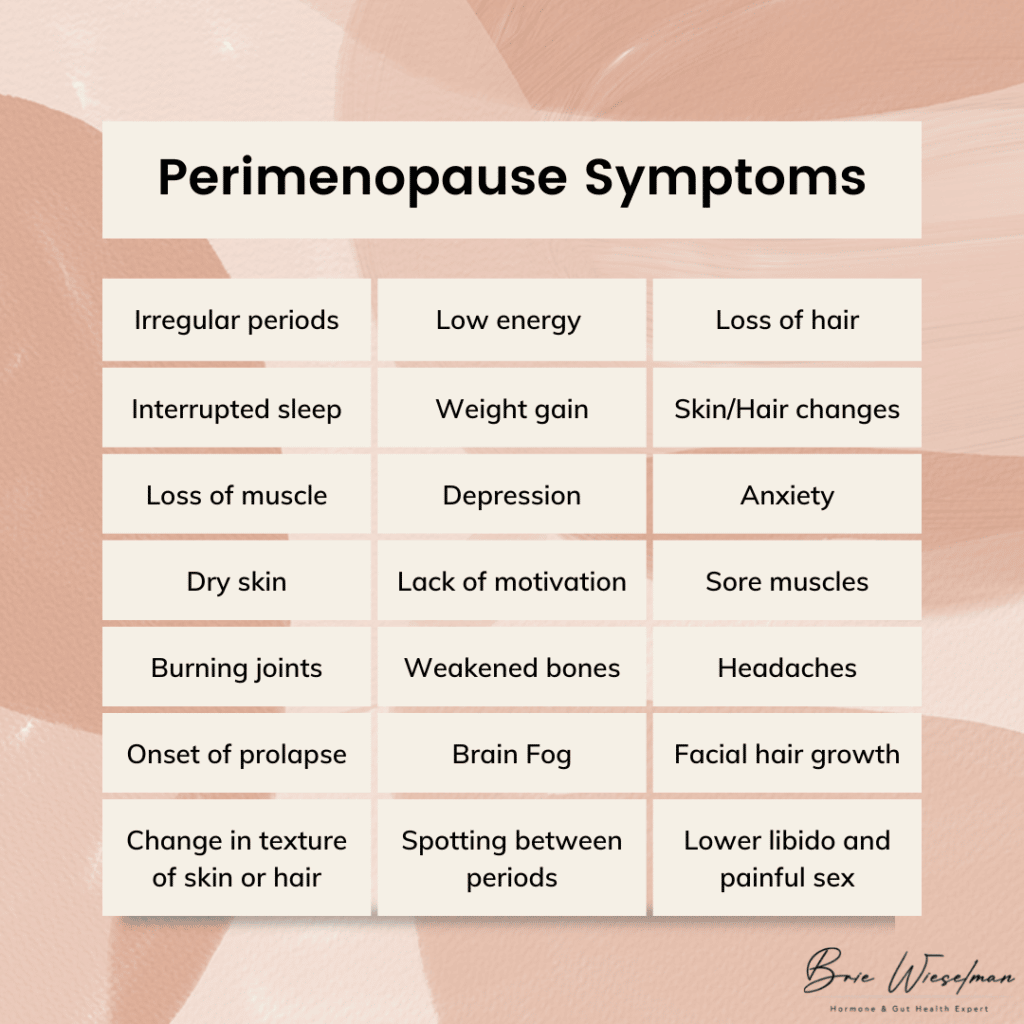 Perimenopause symptoms include:
Perimenopause symptoms include:
- More frequent or heavier periods or missing or less frequent periods
- Interrupted sleep
- Low energy
- Night sweats/hot flashes
- Weight gain
- Change in texture of skin or hair
- Loss of muscle
- Irritability and depression
- Anxiety
- Lack of motivation
- Dry skin
- Sore muscles
- Burning joints
- Weakened bones
- Lower libido and painful sex
- Headaches
- Onset or worsening of prolapse
- Spotting between periods
- Facial hair growth (especially on the chin)
- Loss of hair (on the head)
- Brain fog
Of course, not every woman has every symptom, and it’s not an overnight onslaught. Usually, the first signs of perimenopause are a slightly shortened cycle (think 21-24 days instead of 28) and an increase in PMS symptoms and irritability.
The Hormonal Changes That Cause Menopause
So what is actually happening in the body to cause everything from weight gain to hair loss?
To start, let’s talk about the normal hormone cycle that occurs each month. It all starts in the brain when the hypothalamus signals the pituitary gland via gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In turn, LH and FSH tell the ovaries it’s time to ovulate and release an egg from the follicle. Ovulation triggers the release of estrogen and progesterone. The release of estrogen and progesterone communicate back to the brain that the system has worked, creating a feedback loop.
During the reproductive years, GnRH is produced in a rhythmic cycle, leading to regular cycles. But as we age and enter perimenopause, the release of GnRH becomes more unpredictable. In addition, as we age the ovaries stop responding to LH, leading to erratic ovulation. Because ovulation is what triggers estrogen and progesterone, when ovulation becomes erratic, levels of these hormones drop.
This doesn't happen all at once, though: the changes are often up and down. At first, estrogen levels may shoot up high, then drop back down. Progesterone is only made via ovulation, so it may be irregular in the early stages of perimenopause before beginning a gradual decline. The decline of progesterone often occurs faster than estrogen, leading to temporary estrogen dominance in perimenopause, as well.
The loss of progesterone affects the brain, GABA system, and HPA axis. Allopregnanolone, one type of progesterone, has a calming effect on the brain. Without adequate levels of it, sleep disturbances and reduced ability to cope with stress can occur. The loss of progesterone can also contribute to autoimmunity, especially Hashimoto's thyroiditis. And without the anti-androgenic effect of progesterone, excess androgens can stimulate insulin, contributing to insulin resistance.
In addition to these changes, testosterone, which is produced in the ovaries and adrenal gland, continues to be produced after menopause (though it peaks in the 20s). It is common to go through a phase in perimenopause where testosterone is high relative to estrogen and progesterone, causing symptoms like hair loss, central abdominal weight gain/body shape change, and the onset or worsening of insulin resistance.
Some types of estrogen are produced outside the ovaries. Half of the body’s estrone (one type of estrogen) is made in the fat tissue and adrenal glands, and estrone becomes the predominant estrogen after menopause. This is good for bone density, brain tissue maintenance, and cardiovascular health - we need that estrone! This is why supporting adrenal health is so important for making it through menopause with optimal hormone levels (more on that to come).
The 4 Stages of Perimenopause
From a hormonal standpoint, I like to break perimenopause into 4 stages.
Stage 1: In this stage, estrogen is high, but progesterone levels have started to drop due to an increase in anovulatory cycles (when bleeding occurs and you have a “period” but your body doesn’t ovulate). The luteal phase is often shorter here, but periods might stay regular.
Stage 2: In this phase, estrogen levels are still high but start to fluctuate, causing symptoms associated with estrogen withdrawal, such as hot flashes, migraines, and night sweats. Cycle lengths may vary by as much as 7 days.
Stage 3: Stage 3 is marked by a significant increase in cycle length, going two or more months between cycles. The hormonal changes of Stage 2 remain and/or intensify, and estrogen remains high or rises and drops.
Stage 4: This final stage is often a waiting game: will you get your period again, or are you officially in menopause for good? Estrogen levels are low, unless you get a surprise period, which can raise levels back up temporarily.
Does Menopause Have to Be Miserable?
I could shout it from the rooftops: menopause is not a bad thing, and it doesn’t have to make you feel bad! If there is a menopause problem it’s simply that menopause and modern life are an evolutionary mismatch.
In comparison, the women of the remote Hadza tribe in Tanzania, who still practice hunting and gatherng as a subsistence pattern, don’t experience menopause the way American women do - in fact they report no symptoms associated with menopause, and don’t even have a name for this change.
How can that be? Some of the most important factors might be that Hadza women:
- Have robust gut microbiomes
- Have a strong sense of community and purpose
- Pre-menopausal women rest during their period
- Post-menopausal women eat less and walk more than pre-menopuasal women
- Spend more time pregnant and breastfeeding (and often transition directly from pregnancy/breastfeeding to perimenopause, softening the transition)
- Eat a foraged, high fiber diet without aunty farmed or processed foods
Fortunately, we don’t have to move off the grid to adapt some of these practices to our own lifestyles and reap the benefits. More on my suggestions for how to do this to come.
Understanding Hormone Replacement Therapy for Menopause and Perimenopause Symptoms
Hormone replacement therapy is the use of topical or oral estrogen, progesterone, and sometimes testosterone to temporarily increase hormone levels, treat the symptoms of perimenopause, and improve overall well-being.
Bioidentical hormone replacement therapy (B-HRT) is the use of replacement hormones that are identical to what the body produces. This is in contrast to the use of synthetic hormones, like those found in birth control pills.
As early as the 1930s, women were given placenta as a form of estrogen replacement therapy. In the 1940s, Premarin, a drug made from the urine of pregnant horses, was developed as a HRT. In the 1970s, studies linked estrogen therapy to endometrial cancer, revealing the importance of including progesterone to prevent estrogen-driven cancers.
From the 1960s to the 1990s, hormone replacement therapy grew in popularity. It was marketed as a way to stay youthful and feminine, and was widely used. But then, in the early 2000s, research showed HRT caused a slight increase in the risk of breast cancer, heart disease, stroke and blood clots.
Is Hormone Replacement Therapy Safe?
In 2002, a HRT trial was stopped early because of risks including a small increased risk of breast cancer, heart disease, stroke and blood clots, but fewer cases of hip fractures and colon cancer. This was followed by a 2003 report in the Lancet claiming the use of HRT increased the incidence of breast cancer, even though the data was not strong enough to document a clear harm.
This incomplete information created a change in public opinion that remains today: many women are hesitant to use HRT, even though we now know how to use it safely.
What we now know is that the most important factor for HRT safety is the age at which it is started. HRT is best started as young as possible, while in the perimenopausal window, and ideally continued for no more than 2 years beyond the last period. Starting HRT when older, or after the last period has occurred, increases the risk.
That’s why I’m glad you’re here reading this: if you want to start HRT, starting sooner is safer. But if you feel like you already missed your chance at HRT, and have now “aged out” - don’t give up hope. I have more suggestions for you at the end of this post.
In July 2017, the North American Menopause Society (NAMS) relased thier positon after reviewing the data amassed from millions of women usign HRT over several decades, and concluded the benefits of HRT outweigh the risk for healthy women, when HRT is started at the proper age. They found that being obese or having 4 or more alcohlic drinks per week actually increased the risk of breast cancer more than the proper use of HRT. Women using HRT had a 4 in 1000 chance of breast cancers vs a 3 in 1000 chance in women not using HRT.
In addition, they found there was no increased risk of heart attacks in women using HRT as long as they started taking HRT within 10 years of their last period or started between the age of 50 and 59.
In particular, bioidentical hormones are safer than synthetic hormones. Bioidentical progesterone likely decreases the risk of breast cancer, whereas synthetic progestins increase the risk. If started early in perimenopause, bioidentical hormones are actually heart protective as opposed to a risk factor for heart disease.
Pros and Cons of Hormone Replacement Therapy
When used correctly, the benefits of hormone replacement therapy include:
- Fewer hot flashes
- Improved insomnia & sleep disturbances
- Improved anxiety & depression
- Less brain fog
- Fewer menopausal symtoms in general
The primary cons are the potential slightly increased risk of breast cancer and heart disease.
When deciding to start hormone replacement therapy, there’s a lot to consider. Here’s some of what I go over with patients while developing a treatment plan:
- Age and proximity to menopause (starting earlier is generally better)
- History of breast cancer (self and family)
- Genetic predisposition to hormonal cancers
- Risk of cardiovascular disease (I screen for factor V and prothrombin in all patients before starting HRT)
The type of hormone therapy used matters, too. Options include pills, gels, creams, patches, troche, and liquids. While gels, creams, and patches are common , I actually prefer oral micronized progesterone, or, nanoliposomal topical serum. Most topical progesterones aren’t able to deliver a high enough dose to protect the uterine lining. In addition, there’s no “regular” rate of absorption for creams, gels, or patches. Each woman’s unique physiology determines how much and how fast she will absorb topical hormones. Topical progesterone can also be stored in the fat, then “dumped” by the body, leading to irregular levels in the blood, damaging the sensitive feedback loop in the brain. When used for longer periods of time, I’ve also seen fat-based topical progesterone build up to higher than physiologically normal levels, eventually causing progesterone receptor resistance, much like insulin resistance. When a woman has been using topical progesterone, has normal or even high levels when tested, but still has the symptoms of low progesterone, this is usually the reason.
Whatever form you choose, careful monitoring before, during and after use is an absolute must. After initial testing, hormones should be retested within 3 months of starting HRT to assess if levels need adjusting, as well as how estrogens are metabolized. Women often assume they need estrogen, but actually just need progesterone to start, as progesterone is often low relative to estrogen in early menopause. Progesterone can help with symptoms like night sweats and hot flashes just as much (if not more) than estrogen. When estrogen is needed, estradiol and estriol are both very safe when used in combination with progesterone.
I use the DUTCH Complete Estrogen metabolism test, and look to make 2-OH as high or higher than all types of estrogen and other metabolites, for optimal, safe metabolism.
I also want 4-OH to be moderate to lower, at least not higher than 2-OH.
Alternatives & Complements to Hormone Replacement Therapy
Ready to start hormone replacement therapy? You’ll get the best results when also addressing your glucose, gut, and adrenal health in check, while paying attention to your diet, exercise, social life, and life purpose.
But even if you decide against HRT, addressing these other aspects of your health can have a radical impact on how you feel during perimenopause and menopause.
Eat For Balanced Blood Sugar
Research has linked hot flashes to insulin resistance, finding that glucose levels and the degree of insulin resistance rose as the frequency of hot flashes rose. Glucose levels were 33% higher in women who reported hot flashes 1 to 5 days per week than in those who reported no hot flashes. In another study of 6,000 menopausal women, diets high in fat and sugar led to a 20-percent increase in hot flashes and night sweats. After working with hundreds of women in my clinic, I’ve found that the more stable we keep their glucose levels, the fewer menopause symptoms they have.
Ditch Caffeine
There may be a link between caffeine use and certain menopause symptoms — namely, hot flashes and other symptoms related to the body's regulation of the diameter of blood vessels (vasomotor symptoms).
Avoid Spicy Foods
Like alcoholic beverages, spicy food causes vasodilation of the blood vessels, triggering hot flashes.
Eliminate or Reduce Alcohol
Cut back on drinks to 2 or less per week. When you do drink, expect to see menopause symptms return that night. (And surprisingly, wine is usually worse than clear spirits in this case - so maybe go with the vodka soda!) Cutting alcohol and sugar completely eliminates or minimizes night sweats and hot flashes in most women I see.
Exercise Regularly
Movement is always great, but it's most effective if you’ve been moving regularly in the time leading up to perimenopause, and then keep moving. Too much exercise or high intensity can actually trigger hot flashes because of the influence on blood flow to brain and skin and how the brain regulates body temperature.
Do Active Stress Management Daily
This can look like meditation, relaxation tracks, or hypnosis. CBT has also been shown to be very effective, especially in women who can’t use HRT due to breast cancer.
Support Gut Health
The gut plays a major role in the production and clearance of hormones. I always recommend a comprehensive gut health test and gut health practices like using a probiotic.
Try Phytoestrogen Foods
In some cases, phytoestrogen-rich foods like soy and legumes can be helpful.
Rehab Your Adrenals
Your adrenals are responsible for synthesizing appropriate levels of testosterone, progesterone, and estrogen in the perimenopause transition and beyond. Test your hormones with a DUTCH Complete panel and work with a practitioner who can create a customized protocol to rehab your adrenal hormone function.
Get Personalized Help with Hormone Replacement Therapy & Menopause
If you’re entering perimenopause (or already in the thick of it), hormone replacement therapy can help ease the transition. But even if you’re not ready (or not interested in) HRT, using diet, lifestyle, and herbs can help significantly. Either way, you don’t have to just accept the night sweats, hot flashes, weight gain, and mood swings - we can help!
If you’re looking for support in menopause, perimenopause, HRT, or natural alternatives to HRT, click here to book a free consult with our team.
We’ve helped hundreds of women in this life transition, and we’d be honored to help you, too.
Eating for Balanced Blood Sugar
Every year, various diet theories make their way into popular view on the internet. “Everyone should eat less fat”…. “Everyone should eat low carb”…. “Everyone should go Keto”….. it’s enough to make your head spin! The truth is that we are all biologically and genetically unique, and there is no One Diet that is an ideal match for everyone. That said there are some general principles that hold true across various diet types, and one of those is the importance of maintaining balanced blood sugar
Keeping blood sugar levels stable is critical for hormone balance, lowering inflammation, and optimizing energy levels throughout the day.
Why Balanced Blood Sugar Matters
When we eat carbohydrates, the body breaks them down into simple sugars called glucose. Glucose crosses from the small intestine into the bloodstream where it can be taken up by the mitochondria - the “powerhouses”of our cells - and converted into energy. This energy is called adenosine triphosphate (ATP). However, mitochondria have a limited capacity to convert glucose into ATP: they can only convert as much glucose into ATP as they can use. When more glucose is present than can be used by the mitochondria, it causes “glucose spikes” - also known as elevated blood sugar. To prevent glucose spikes, one of two things happens to extra glucose circulating in the bloodstream: it is either converted by the hormone insulin into fat for storage, or into free radicals.
Free radicals are small, unstable molecules that set off a chain reaction of oxidative stress, inflammation, and aging. Free radicals have the potential to create mutations in our DNA, “turning on” harmful genes and even leading to cancerous cell changes. Oxidative stress caused by free radicals is the main trigger for all types of chronic disease, such as heart disease, dementia and cognitive decline, type 2 diabetes, and accelerated aging of all tissues, including your skin. Free radical damage to mitochondria leads to a loss of endurance for exercise and handling situational stress. A diet that prevents free-radical-creating glucose spikes lowers oxidative stress and the resulting inflammation, thereby reducing the risk of any of these inflammation- based diseases.
Insulin is the hormone that stashes away glucose that our mitochondria can’t make use of at the moment. Insulin is released when blood sugar levels rise. First, insulin pushes extra glucose into the cells of our muscles and liver to be stored as glycogen. But then, when it runs out of “closet space,” it turns excess glucose into fat and stores it in our fat reserves. When the muscles and liver run out of glycogen, they should be able to tap into fat stores to replenish themselves, causing weight loss. However, if insulin is present, our body is prevented from tapping into these reserves. If levels of glucose are kept stable, insulin levels stay steady, allowing the body to burn fat for energy, thereby decreasing weight.
Excess levels of insulin contribute to adrenal stress, including hypoglycemia, by clearing glucose out of circulation and into fat cells to be stored for later use, causing blood glucose levels to drop. In order to normalize blood sugar, the adrenals have to produce increased levels of cortisol and epinephrine. This often leads to long-term cortisol depletion and ultimately adrenal hormone dysfunction.
The decline of a glucose spike back to normal levels also triggers cravings. Studies show that a decrease in glucose levels, even just a decrease of 1.1 mmol/L, leads to increased cravings for high calorie foods. This can lead to overeating.
Short & Long-term Effects of Glucose Spikes
- Cravings
- Fatigue/chronic fatigue
- Poor sleep (waking during the night)
- Suppressed immune response/more vulnerability to viruses and bacterial infections
- Exacerbation of hormonal hot flashes and night sweats (worse flashes = high levels of glucose and insulin in studies)
- Increased likelihood of migraines
- Memory and cognitive issues
- Increased risk of Alzheimer’s and dementia
- Acne and other inflammatory skin conditions
- Arthritis and other inflammatory diseases
- Increased cancer risk
- Heart disease
- Infertility and PCOS
- Insulin resistance and Type 2 diabetes
- Non-Alcoholic Fatty Liver Disease
- More depressive episodes
- Digestive symptoms like leaky gut, heartburn, acid reflux
- Accelerated aging and more rapid formation of wrinkles
Normal Blood Sugar Levels
According to the American Diabetes Association (ADA), normal fasting blood sugar is below 100 mg/dL. Levels between 100-125 indicate pre-diabetes, and anything over 126 when fasting is considered diabetic. After eating (postprandial), the ADA considers 70-140 mg/dL to be normal.
But, what’s “normal” isn’t necessarily optimal. Fasting glucose can be “normal,” but you may still experience glucose spikes over 140 mg/dL throughout the day. Instead, I prefer to look for these signs of optimal blood glucose levels:
- Fasting: 70-90 mg/dL
- Postprandial: Below 120 with a return to pre-meal glucose levels within 2 hours (ideally below 100)
However, a single blood sugar reading taken alone is not the best way to gauge overall blood sugar health. Instead, I suggest continuous glucose monitoring.
Continuous Glucose Monitoring
A Continuous Glucose Monitor (CGM) is a small device that you wear on the back of your arm for two weeks. They are painless to insert, and once placed, monitor the amount of glucose in your tissues 24 hours a day, sending the data to an app on your smartphone. Though they were originally developed for people with diabetes who need multiple blood glucose readings a day, almost anyone can benefit from the convenience and multiple data points a CGM can provide. A CGM is the best way to understand how specific foods affect your body, and the impact that glucose shifts have on your mood, energy, sleep, inflammation, and more.
Those interested in continuous glucose monitoring may be able to obtain one by prescription from your general practitioner, especially if you’ve had a history of elevated HBA1c, fasting glucose levels, or labs that suggest diabetes, gestational diabetes, or pre-diabetes. Alternatively, you can request a prescription to be filled at a pharmacy of your choosing through the concierge service at www.pushhealth.com. Request the Abbott Freestyle Libre unless you have an actual diagnosis of Diabetes, in which case you should qualify for insurance coverage of the Dexcom G6 CGM, which is more accurate, but more expensive out of pocket.
There are many subscription platforms using CGM, as well. These services come with app interfaces with more bells and whistles, food tracking built in, and generally some type of interactive coaching service available through in-app messaging. January.ai, Nutrisense, and Levels are a few of the better known platforms offering this service.
For more information on how CGMs work and directions on how to calibrate yours, read here.
Are Carbs Bad for Blood Sugar levels?
Since carbohydrates become the glucose that elevates blood sugar levels, it’s only natural to wonder if carbohydrates are something that should be avoided. But in actuality, it’s much more complicated than just “good” or “bad.”
Glucose is essential to life. In fact, in the absence of any glucose in the diet, the liver converts fat into usable glucose via a process called gluconeogenesis. We are also biologically programmed to love sweet tastes. In hunter-gatherer times, sweet flavor meant food was both safe and was rich in energy. Sweet tastes release dopamine in the brain, which registers as pleasurable, prompting us to seek more of it. We are literally designed to consume carbohydrates.
But, not all carbohydrates are created equally. Carbohydrates are made by plants during photosynthesis and consist of starches, fibers, and sugars, including glucose, fructose, and sucrose. These exist in different proportions in different plants: kale has lots of fiber and some starch, while cherries contain mostly sugars, and some fiber. The fiber in plants slows the absorption of the glucose. This is what nature intended. In modern times, we have learned first to breed plants for higher sugar content and sweetness, and then to extract sugar from the fiber in plants and use it to sweeten… everything! It is this that has led to chronic health problems and modern degenerative diseases, not carbohydrates themselves.
How Much Carbohydrate Should I Be Eating?
One of the most effective ways to prevent or reverse the excess production of insulin and cortisol is to balance the amount of carbohydrates and proteins that are eaten with each meal. The amount of carbohydrates that each person needs is highly individual, and is based on several factors: size, activity level, being physiologically male vs female, and biochemical individuality/genetics. For example, an average sized woman who is moderately active, and not trying to lose weight, might need 75-150 grams. If she’s training intensively, she might need closer to 200 grams, or more. An average sized man might need 150-200 grams, or up to 400 grams daily if highly active.
Proper macronutrient ratios (percentage of carb/fat/protein in the diet) vary by health goals as well, for example weight loss vs mood stabilization vs maintaining a healthy pregnancy. Weight loss is generally supported by lowering carbohydrate consumption, whereas some people with insomnia, anxiety, or depression may be better served by slightly increasing carb consumption. If you are only eating 50 grams daily, and not sleeping well, or suffering from energy or mood dips, consider increasing by increments of 25 grams daily up to 100 or 150 grams and noticing what happens.
The only way to know what is right for you is to experiment and observe how you feel. Additionally, wearing a Continuous Glucose Monitor (CGM - discussed above), can provide a sense of your carbohydrate tolerance at various times of day.
Beyond just the amount of carbs eaten, the type and way in which you eat carbs can also have a profound effect on blood sugar stability.
A few simple guidelines:
Include small amounts (1/2 – 1 cup) of starchy veggies (such as root vegetables, squash, or tubers), 1-3 times daily, depending on your personal carbohydrate need. Eliminate or minimize grains. If you do include grains, emphasize whole form, not flours, as flours have a higher glycemic load and will raise blood sugar more rapidly, and to a greater extent than their unprocessed counter-parts.
Include proteins with each meal in a weighted ratio of at least 2:1 of carbohydrate to protein.
Eat 15-20 grams/protein at each meal, unless directed otherwise by your healthcare provider based on specific health goals. This is approximately a palm-sized serving of fish, chicken, or red meat, or 2-3 eggs. You can also get some protein in the form of nuts, seeds, and legumes, just be aware of the carbohydrate load that beans naturally include. While this amount may be fine for some people, for people with blood sugar control issues, beans may be better as a condiment or salad topping.
Eat as many green, and then multi-colored (red, yellow, orange and purple) veggies as possible each day. Strive for 5-10 cups of veggies daily.
Use extra virgin olive oil, coconut oil/coconut butter/coconut milk, ghee, flaxseed oil (do not heat), macadamia nut oil, or avocado. Avoid canola oil and use seed oils sparingly.
Eat 1-2 servings maximum of fruit daily. Always consume fruit with a protein or fat: nuts, nut butter, or other fat/protein source.
If you struggle with elevated blood sugar levels, do not snack between meals, and instead eat at 3 specific times of day, or as your practitioner has recommended for you.
How to Flatten Glucose Spikes
#1 Deconstruct your meal
Instead of grabbing a bite of this and a bite of that, try this: eat veggies first (especially above-ground veggies and anything leafy). The fiber in veggies slows the breakdown and absorption of glucose. After you finish your veggies, eat protein and fat next, as fat slows the absorption of sugar. Save the starchy component of your meal for last.
#2 Add greens to the beginning of every meal
In addition to eating your veggies first, add a small salad or veggie appetizer before the meal, such as spinach leaves with a few artichoke hearts and vinegar and olive oil. Alternately, roast some low carb veggies like cauliflower and broccoli in the oven and store in the fridge to have on hand. Or, try grabbing a few bites of fermented veggies like sauerkraut or kimchi: eating even just a few bites of these prior to your meal lowers glucose spikes.
#3 Stop counting calories
Not all calories are equal. Weight management and health have much more to do with keeping glucose stable (using these techniques) than with sticking to an arbitrary calorie goal.Conventional wisdom says adding oil and vinegar to your salad only adds calories, but in reality those extra calories will keep you full longer, rev up fat burning, blunt the absorption of starches in the rest of the meal, and ultimately contribute to weight loss!
#4 Prioritize a high protein, lower carbohydrate breakfast with plenty of healthy fats
Extra points for fiber from veggies!This will set you up for better glucose control and energy through the day, as we are more sensitive to sugars first thing in the morning after fasting. Plus destabilizing glucose first thing with a high-sugar breakfast makes it very hard to regain glucose stability later in the day. (One note: Avoid smoothies containing lots of blended fruit, as this breaks up the fiber, making the sugar in the fruit more available, yielding bigger glucose swings. Some smoothies easily spike blood glucose as high as drinking a can of soda!
#5 Consume vinegar before a meal
To blunt glucose spikes, dilute 1 teaspoon to 2 tablespoons of any unsweetened vinegar– most people enjoy Apple Cider Vinegar the most– in water and drink before eating. Adding vinegar can reduce glucose spikes as much as 20%. Not a vinegar fan? This blog lists many delicious drink recipes based around apple cider vinegar.
#6 Move your body after you eat
With every movement we make, we burn glucose. If we stay still after a meal, glucose enters the bloodstream and then floods our cells and overwhelms our mitochondria. But, if we use our muscles as the glucose moves from the intestines into the blood, our mitochondria have a higher burning capacity and will use that glucose to make more ATP. This makes a huge difference when tracked using a glucometer or CGM: just adding exercise after a meal significantly lowers glucose levels. For best results, move anytime in the hour after you finish a meal - but it doesn’t have to be a hardcore workout. Just 10 minutes of walking is helpful, and if you can’t go for a walk, doing squats, planks, or lifting something heavy works just as well.
Sweet Foods & Dessert
If you’re going to eat dessert, the best time to eat it is at the end of a meal - meaning green starter, vinegar, then veggie, protein/fat, starches…..and then dessert. When snacking, opt for savory snacks whenever possible. Don’t eat carbs by themselves– always eat them with protein or fat beforehand. This includes fruit.
Replace sweeteners with monk fruit, allulose, or stevia (if you tolerate and enjoy stevia) where possible. Better yet, go sweetener free for a period of time to “reset” your taste buds. Avoid sweeteners like sucralose, xylitol, aspartame, maltitol, and erythritol.
Sample Blood Sugar Balancing Menu
Day 1:
- 8am breakfast: 2-3 egg scramble with 2-4 oz ground chicken or chicken sausage, chopped spinach, onion, garlic, herbs, cooked in 1-2 TBS of grass-fed butter or ghee or coconut oil. Ideally with a few bites of roasted broccoli from the fridge, beforehand.
- 11am snack if needed: 10 nuts or 1 TBS nut butter and 1 cup berries
- 1pm: leafy green salad with 2 cups of chopped veggies, hard-boiled egg, turkey or chicken breast, and salad dressing of fresh lemon juice and EVOO
- 4pm snack if needed: turkey roll-up (2-3 turkey slices rolled around avocado and hummus)
- 6-7pm: oven roasted fish (coconut crusted salmon: rub salmon with olive oil, sea salt and pepper and pat with flaked coconut. Bake at 375 for 20 minutes),1 cup of roasted butternut squash cubes, and 1-2 cups of sautéed leafy greens with garlic. Eat the greens first.
Day 2:
- 8am: Clean protein smoothie w/ 2 cups super greens, 2 TBS tahini, cinnamon, and 1 cup of berries blended in almond milk. Bonus: add 1 TBS of Paleo Fiber
- 11am: raw veggie sticks and guacamole
- 1pm: Lettuce wrapped lamb burger, leftover greens, 1/2 sweet potato with coconut butter
- 6-7 pm: shrimp fajitas (with 1-2 cassava coconut Siete Foods Tortillas) OR ground turkey lettuce tacos with organic pressure-cooked black beans . Eat the beans last!
Day 3:
- 8am: chicken sausage, grated parsnip hash cooked in avocado oil, with spinach and avocado 11am: protein powder smoothie with 1 cup berries and almond milk.
- 1pm: coconut milk soup with chicken, side salad
- 4pm: handful of almonds
- 6-7pm: pesto chicken breast, braised red cabbage (slice cabbage and sauté in olive oil + chicken broth), roasted beets in olive oil with rosemary.
- dessert/snack: dark chocolate (1-2 squares) with whipped coconut cream
Get Your Own Customized Plan
You have the power to take back control and help your body (and blood sugar) get back into balance.
For a customized plan, step-by-step support, and expert guidance, the first step is to book a free, no-obligation discovery call with my health team.
Learn about how we work with clients to achieve their unique health goals and help them step back into radiant health, so they can stop worrying about how they feel and start living a purposeful life.
> Book your free discovery call here
Check Out These Books for Further Reading
- The Glucose Revolution by Jessie Inchauspe
- Drop Acid by David Perlmutter
- Unlocking the Keto Code: The Revolutionary New Science of Keto That Offers More Benefits Without Deprivation by Steven Gundry.
Insulin Sensitivity and Gut Health—A Dynamic Duo
Do you want your skin to look smooth and youthful for as long as possible?
Do you want your brain to be sharp?
What about losing weight and maintaining a slender, sleek body?
These are just some of the reasons to care about keeping your insulin and blood sugar levels balanced—even if you don’t have prediabetes or diabetes. Yet, when many people hear about insulin sensitivity they think it’s only relevant to diabetics.
That couldn’t be more wrong.
There are good reasons for everyone to care about how their body is handling insulin. And surprisingly, it’s your gut that plays a major role in keeping this blood-sugar-balancing hormone in control.
If your gut is unhealthy, your body won’t handle insulin well, which means your blood sugar will get out of whack.
What Is Insulin Sensitivity?
Insulin is a hormone that’s made when our blood sugar (glucose) levels rise. It pushes extra glucose into the cells of our muscles and liver, where it’s stored as glycogen. But when our muscles or liver run out of closet space to store the glucose, the excess is converted into fat and stored in our fat reserves.
When muscles and the liver run out of glycogen they should be able to tap into fat stores to replenish themselves, causing weight loss.
However, if insulin is present in excess amounts, it blocks your body from tapping into those reserves.
What causes high insulin levels? Usually the culprit is high blood glucose in the form of glucose spikes that often happen even in people without diabetes.
Insulin sensitivity refers to the body’s ability to respond to the blood-sugar-lowering signals that insulin is broadcasting. If the body can’t respond to those signals, it starts making more and more insulin to try to “hear” what insulin is saying. Kind of like talking louder when someone can’t hear you. Reduced insulin sensitivity is known as insulin resistance. In other words, your body isn’t as sensitive to insulin anymore so it needs to make more and more.
Why You Should Care About Insulin Sensitivity
Poor insulin sensitivity and glucose spikes are to blame for a number of health problems, not just diabetes. For example, they’re linked to:
- Accelerated skin aging and more rapid development of wrinkles
- Acne and other inflammatory skin conditions
- Adrenal stress
- Arthritis and other inflammatory diseases
- Cravings
- Depressive episodes
- Digestive symptoms like leaky gut, heartburn, acid reflux
- Fatigue/chronic fatigue
- Heart disease
- Increased cancer risk
- Increased risk of Alzheimer’s disease and dementia
- Infertility and polycystic ovary syndrome (PCOS)
- Memory problems
- Migraines
- Non-alcoholic fatty liver disease (NAFLD)
- Poor sleep (waking during the night)
- Suppressed immune response
- Type 2 diabetes
- Worsening of hormonal hot flashes and night sweats
How The Gut Controls Insulin Sensitivity
Problems in the gut lead to problems with blood sugar and the way your body uses insulin. Usually people don’t connect the gut with insulin problems, but there is a HUGE connection between the two.
Here’s the deal: The gut affects insulin sensitivity in five ways. Some of these might sound kind of technical, but bear with me for a moment as I’ll explain them all in a minute.
- Leaky gut
- Endotoxemia
- Production of short-chain fatty acids like butyrate
- Alterations in bile acid metabolism
- Effects on the secretion of gut hormones
The common denominator in all five of these factors is an imbalance in the gut microbiota. The gut microbiota are the little organisms that live in your intestines, both good and bad bacteria, viruses, and fungi. Scientists call an imbalance in the gut microbiota dysbiosis. Dysbiosis is common in diabetes, suggesting the gut microbiota and blood sugar problems are connected. In diabetes, levels of beneficial bacteria are decreased, whereas many harmful bacteria are increased. Small intestinal bacterial overgrowth is also common in diabetes.
Leaky Gut
Gut microbiota dysbiosis can lead to leaky gut, otherwise known as increased intestinal permeability. Leaky gut is the name for what happens when a person’s intestinal lining is weakened. This weakened lining allows toxins and bacteria to slip through into the bloodstream, causing problems throughout the body. Leaky gut creates inflammation and reduces insulin sensitivity. There’s also a link between leaky gut and diabetes.
Low-Grade Endotoxemia
Bacteria in the body produce a type of toxin known as an endotoxin, primarily a bad guy known as LPS. It’s a component of bacterial cell walls found mostly in gram-negative bacteria. When LPS escapes the colon during leaky gut and becomes a fugitive on the run throughout the body, it triggers an inflammatory response known as endotoxemia.
LPS also does a number on the way your body uses insulin. LPS triggers an inflammatory cascade in every type of tissue it comes into contact with in the body. In insulin receptors, this inflammation leads to reduced sensitivity to insulin—or—insulin resistance.
Endotoxemia and leaky gut go hand in hand. Since the intestinal lining is weaker, it allows these toxins to escape into the bloodstream, causing problems that at first glance don’t seem as if they’re linked to the gut.
Butyrate and Short-Chain Fatty Acids
Short-chain fatty acids like butyrate are important for gut health and insulin sensitivity. Bacteria in the gut, especially those that belong to the phylum Firmicutes, make butyrate. If your gut isn’t making enough butyrate it spells trouble for the way your body uses insulin.
In studies of obese mice, butyrate supplementation increased insulin sensitivity and improved weight loss. Fasting blood glucose, fasting insulin, and insulin tolerance remained normal in mice given butyrate.
In humans, if there aren’t enough butyrate-producing bacteria, it boosts the risk of metabolic disorders like diabetes.
Butyrate repairs the intestinal lining and reduces inflammation, helping to get rid of leaky gut, which in turn promotes healthy blood sugar levels.
Bile Acid Metabolism
Another way in which the gut controls insulin sensitivity is by regulating the way the body produces bile acids, which stimulate insulin secretion. People with leaky gut don’t recirculate bile acids efficiently. So they wind up with bile acid deficiency over time, which leads to inefficient detoxification as well as changes in how your body regulates fat and carb digestion.
Secretion of Gut Hormones
A healthy gut equals healthy amounts of gut-derived metabolic hormones called glucagon-like peptides (GLP-1), which are linked to blood sugar balance. GLP-1 boosts insulin levels when there’s glucose in the blood, helping to push glucose into your cells to improve blood sugar levels.
GLP-1 also keeps you feeling full and satisfied after eating so that you can stay away from desserts and other unhealthy foods.
How To Know If You Have Blood Sugar Issues
One of the best ways to monitor your insulin and blood sugar levels is to work with a functional medicine provider, who will order lab tests. The lab tests to measure insulin sensitivity and blood glucose include:
- Fasting glucose, optimal range 70 to 85
- Fasting insulin, optimal below 5
- Fasting uric acid, optimal less than 5.5
- HBA1c (a measure of blood sugar control over time), optimal range 4.8 to 5.2
Also important: Finding out if your gut is healthy by using a stool test. I like the BiomeFX panel.
The second way to see how your body is coping with blood sugar is to monitor glucose spikes. Everybody has glucose spikes to a certain extent. But when insulin sensitivity is low, blood sugar spikes are often too high since insulin is unable to control your blood glucose.
The best way to monitor glucose spikes is by using a glucose monitor for two to four weeks. Monitor readings should be 70 to 120 the majority of the time, but even more ideal is 70 to 100. Lots of people spike above 140, even if they’re not diabetic, but most of us shouldn’t be going over 120 most of the time.
What To Do About Glucose Spikes and Reduce Insulin Sensitivity
Eat Foods That Support Butyrate and Probiotic Bacteria
The main goals of balancing blood sugar and insulin are to raise butyrate levels and to get rid of any gut microbiota imbalances.
From a dietary perspective, there are certain foods you can eat to increase butyrate levels.
Butyrate foods include:
- Apples
- Leeks
- Onions
To support a healthy gut microbiota, eating high-fiber foods rich in prebiotics is a good first step. These types of foods can also help butyrate-producing bacteria flourish. Research has shown that eating fermentable fiber was linked to an increase in the beneficial bacteria Bifidobacteria. This type of fiber also normalized LPS and improved glucose tolerance and insulin secretion, while reducing inflammation.
Prebiotic foods include:
- Apples
- Beans
- Bran
- Chicory root
- Garlic
- Jerusalem artichoke
- Oat bran
- Onions
- Psyllium husk
- Tomatoes
It’s also a good idea to limit sugar and saturated fat, since these can cause butyrate levels to tank.
Butyrate Supplements and Other Solutions
Another way to increase butyrate levels is through using certain dietary supplements. In animal studies, giving mice butyrate supplements blocked the development of insulin resistance caused by eating a high-fat diet.
Probiotics containing Bacillus bacteria endospores such as MegaSporeBiotic can increase butyrate-producing bacteria in the gut.
Certain supplements can also boost butyrate production directly. These include:
- Alanine
- Citrus polyphenols
- Cystine
- Glutamate
- Glycine
- Lysine
- Oligosaccharides (FOS, GOS, XOS)
- Proline
- Sulforaphane
- Threonine
- Tributyrin X by Healthy Gut Company
I have found that it’s possible to boost butyrate by 140% in four weeks using a combo of MegaSporeBiotic and MegaPre—which only feed selectively the keystone bacteria species, not the bad guys—along with MegaMucosa to heal and repair leaky gut with essential nutrients as building blocks.
Balancing Blood Sugar By Improving Gut Health
I have seen so many patients experience an improvement in their health after addressing gut issues, restoring butyrate levels, and balancing insulin and blood sugar levels. They’ll often have improved energy, clearer skin, better sleep, less hot flashes, and many of their other health complaints go away.
You’re going to have the greatest success working with a functional medicine provider who can tackle all the bases. That’s why I invite you to reach out to me for a free 15-minute call to find out the best course of action for you.
If after the call you come on board as a patient, I’ll order the right tests for you. Based on the results and your symptoms, I’ll start you on a protocol to balance blood sugar, improve your gut health, and help you look and feel your best.
How to Heal Ulcerative Colitis: A Case Study
If you have ulcerative colitis, this is a case study you’re going to want to read. It’s about a woman—I’ll call her Sherrie—who suffered from this condition for years—until we were able to make some real breakthroughs in her health.
Ulcerative colitis is a type of inflammatory bowel disease (IBD), a disorder that also includes Crohn’s disease. People who have ulcerative colitis have an inflamed colon and rectum and ulcers on the intestinal lining. Living with IBD can be a roller coaster. Their symptoms worsen during flare-ups and their symptoms go away during periods of remission.
Doesn’t sound like much fun, does it?
Ulcerative colitis is often hard to put into remission. It can take time to pin down and treat the root cause. But I’ve found that ulcerative colitis responds well to functional medicine. Often, we can send its bags packing—or at least put it into a long-term remission.
Such was the case for Sherrie.
Sherrie’s Long-Term Battle With Ulcerative Colitis
When Sherrie first came to see me in January 2018, she had been diagnosed with ulcerative colitis nine years prior at the age of 25. Before developing symptoms, she’d had a stressful few years. She bought a house, got married, was finishing her bachelor’s degree, and became pregnant for the first time.
After her initial diagnosis her symptoms were manageable for years. She responded well to the drugs offered her. Conventional doctors gave her prednisone and Lialda (mesalamine) to lower inflammation. Most of her ups and downs were during pregnancy when she had to get off her meds, and she’d get better when she went back on the drugs.
After her third child was born in 2013, she went into remission and didn’t need to take any UC medications for two to three years. Then she caught a cold while traveling and this turned into an ear infection. She took antibiotics, which led to a UC flare. In the two years before she contacted me, she never came out of the flare, which motivated her to seek my help.
Sherrie suffered from bloody stool and watery, urgent diarrhea six to ten times per day. She couldn’t leave her house for fear of not being near a bathroom when she had to go.
She’d never been hospitalized, but the poor dear had only been in remission for a brief period since giving birth, she told me. Pregnancy and birth can cause an immune shift and had made her ulcerative colitis even more difficult to control.
The lab work ordered by other doctors found:
- Low iron and ferritin
- Low vitamin D
- Low potassium
- Low hemoglobin (she was anemic from blood loss)
- Monocytes and eosinophils very high (suggests a parasitic or other type of infection.)
When she first came to my clinic, she was already on a strict paleo diet. That by itself didn’t do any good.
Treating Stress Hormone Imbalances
The first step? Treating Sherrie’s stress-response system. The hypothalamic-pituitary-adrenal axis (or HPA axis) regulates our circadian rhythm and our stress response. Chronic stress can really throw the HPA axis out of balance, which leads to hormone imbalances. It can cause the adrenal glands to pump out too much of the stress hormone cortisol. Some people call this “adrenal fatigue,” but it’s really a problem with the entire HPA axis.
As Sherrie tapered off the prednisone, I gave her a higher than normal dose of dehydroepiandrosterone (DHEA), a hormone produced by the adrenal glands. Because she had been under stress, her adrenal glands were likely worn out and weren’t making enough DHEA.
In fact, every ulcerative colitis patient I’ve treated has had HPA axis dysregulation. So I typically always address this in my UC patients.
And guess what? Her ulcerative colitis flare regressed for the first time in two years. She now had only minimal rectal bleeding and not every day.
Candida and Intestinal Bugs
While dealing with Sherrie’s adrenals, I ordered a stool test that revealed she had high levels of the following bacteria and fungus:
- Candida
- Klebsiella
- Prevotella
- Proteus
- Pseudomonas
- Salmonella
- Staphylococcus
- Streptococcus
It didn’t surprise me that she had Candida overgrowth. The fact she had gotten worse after taking antibiotics for her ear infection was a BIG clue that fungal overgrowth played a role. Candida is a type of yeast that under the wrong conditions can turn into an invasive fungus in your body.
Plus, we know from studies that almost all cases of ulcerative colitis involve the marriage between a fungal imbalance and a bacteria that either trigger immune dysfunction or worsen it.
In mouse studies, Candida albicans can worsen inflammatory colitis. What’s more, the yeast Candida tropicalis teams up with certain bacteria like E. coli to form a monstrous biofilm larger than any created by just one or two of the species alone. A biofilm is a type of shield that bacteria and fungi can form to protect them from things like antibiotics.
The stool test also detected the presence of an amoeba parasite known as Entamoeba coli. Although many people with this parasite don’t have any symptoms, high amounts are linked to loose stools, gas, and other GI complaints. Amoeba infections in general are also linked to IBD.
Sherrie’s stool test also showed high levels of calprotectin, which is a marker of inflammation in the gut lining. A high calprotectin is a red flag for IBD. Her levels of secretory IgA (SIgA) were also high. SIgA lines your intestines and acts as a gatekeeper, keeping bacteria, parasites, and allergens out of your circulation.
Fancy Footwork and Ulcerative Colitis
I began treating the parasitic infection, balancing the microbes in the intestines, and starting round one of Candida treatment. However, we had to put the brakes on treating the Candida for a little while because before starting treatment for this fungus, Sherrie went into flare mode.
There’s often a lot of fancy footwork needed to treat ulcerative colitis patients. Flares can happen due to stress, seasonal changes, and other reasons. We need to time treatments so that we’re not putting too much stress on the body during flares.
Other issues that showed up in testing also needed attention. For example, her mitochondria—the powerhouses of the cells—were in trouble. This is likely because the Candida produced ammonia and acetaldehyde, both toxins to the mitochondria. She also had high levels of a damaging process known as oxidative stress due to the autoimmune process that had created a years-long raging fire in her body.
Her glutathione levels had also tanked, so her body wasn’t making enough of this antioxidant to fight the oxidative stress. I included liposomal glutathione into her regimen.
Here are some other strategies that worked:
- Adding low-dose naltrexone, an anti-inflammatory drug shown to reduce symptom severity in IBD
- Eating an anti-inflammatory diet and adding in foods like rice and some dairy
- Gut-focused hypnotherapy for her post-traumatic stress disorder (PTSD) response when getting into her car. This was triggered by the fear of needing to poop and not being near a bathroom. This therapy and the progress we were making allowed her to travel far from home.
Big Improvements in Ulcerative Colitis Symptoms, But More to Go
By August 2018, Sherrie was the best she’d been in two years!
In September 2018, I ordered another stool test and some other lab work. Some of her beneficial gut bacteria were low and her calprotectin levels were still high. At the same time, I ordered a food reactivity test. Based on that, I had her avoid eggs, wheat, lentils, peas, cashews, peanuts, tuna, and a few other foods.
Her worst flares tended to happen between Thanksgiving and Christmas. My theory? Holiday stress combined with lack of sun and vitamin D contributed to these flares. I learned to give her proactive support heading into that time of year.
Finally, for the first time, she was able to go through the holidays with only a minor flare. I gave her a Chinese herbal formula known as Yunnan Paiyao, which stopped the flare in three days. The Chinese herbs also firmed up her stool.
In addition, I gave her pre- and probiotics and improved her detoxification and antioxidant levels.
Ultimately, after a period of three steps forward and two steps back, she was able to endure the holidays with zero flares.
By January through May 2019, she was better overall and her stool consistency improved, but she was still bleeding mildly.
So much progress, but there was still a root cause that had not been addressed. At this point, I ordered more testing, including a stool test that found the amoeba parasite Blastocystis. The testing also revealed problems digesting and using fats, so I had her take ox bile and a few other supplements.
What’s more, her zinc levels were low. Zinc is critical for bowel repair and lowering inflammation. Selenium—a mineral critical for autoimmune health and the production of glutathione—was also low.
The testing showed her oxidative stress levels were high and her detox abilities were overwhelmed. Levels of the antioxidant glutathione were better, but still low. She still had some Candida.
How To Stop An Ulcerative Colitis Flare-up
In July 2019, after a stressful event, Sherrie went into another flare. I put her on the Specific Carbohydrate Diet (SCD), a diet that’s free of sugar, grains, starch, and processed foods, which really helped. Butyrate enemas were also helpful. Butyrate is a short-chain fatty acid formed from the fermentation of dietary fiber in the colon. It is the main fuel the cells of our intestinal lining use for repair, and it is known to reduce ulcerative colitis symptoms.
Even before our next appointment, as soon as Sherrie could feel a flare coming on, she immediately followed my advice for reducing a flare. It was a BIG win! She was learning how to manage and stop flares on her own. The flare stopped by August and by the fall she was the best she’d been in four years.
She had another flare at the end of summer triggered by poison ivy while camping, but she was able to stop it within two to three days.
By fall she was feeling amazing. She was having regular, twice daily bowel movements. There was no urgency and the stool was well-formed. At the same time, Sherrie was finishing round two of the Candida program.
From fall of 2019 to January 2020, Sherrie stayed in remission. Right after the holidays were over she had another flare, but she was able to stop the flare almost entirely on her own before our next appointment. Yay!
We tested again. As you can see, this is a process of continually testing, treating, and modifying the protocol until we can get ahead of the disease process. Since her vitamin D levels were very low, I gave her a higher dose supplement. Her gut microbiome was also imbalanced with low levels of a type of bacteria known as Akkermansia. I focused on restoring levels of this important bacteria using specific prebiotics (pomegranate seed husk, matcha, greens powders, red powders for polyphenols, and acacia fiber) in order to repair her gut lining.
She had only a mild flare in the winter of 2019-2020. This happened in February 2020 and drew out with occasional small amounts of blood until April.
Can Mold Toxicity Cause Ulcerative Colitis?
After the flare in February 2020, we discussed some reasons why she kept having flares—and we had a breakthrough.
I knew that there is a link between mycotoxins—toxins produced by mold—and ulcerative colitis. When no obvious lifestyle or nutrition factors could explain Sherrie’s UC flares, I started digging deeper into what might be bothering her in her environment- her house to be exact. The fact she got worse in winter when the environment was more moist also pointed toward mycotoxins as a possible cause.
Even though her home was a new build she knew for certain there was periodically mold in her home. She and her husband often tried to clean it up.
We tested Sherrie for mold and mycotoxins in April 2020. Many markers for mycotoxins were high. An inflammatory marker known as TNF-alpha was also elevated.
Aha! Mold could definitely be the culprit.
She had her home inspected by a professional company that uses indoor mold testing and found the home was contaminated.
I started Sherrie on a treatment regimen for mycotoxins in July 2020 to proactively get her through her vulnerable period in late fall/winter.
At first that strategy paid off. She felt great. Her stool was firm and she had no flares.
She took a break from the mycotoxin program and had a flare between Christmas and New Year’s 2021. She mostly recovered within a month. But since she was still having flares, I decided to retest her for mycotoxin markers in February 2021.
That testing revealed she still had very high levels of the mycotoxin known as ochratoxin. Although these tests aren’t always 100% accurate, Sherrie’s lack of complete progress, her symptoms, and other markers suggested mold could be to blame.
I put her on another round of the mold protocol, and she stayed well through August 2021.
I ordered another mycotoxin test and it was much lower, although still high. This suggested she might be getting re-exposed.
Her husband had done some mold remediation on their home. But another round of indoor mold testing still showed the mold was off-the-charts positive. A mold-testing company found more mold in the utility room behind the water heater, in the shower caulking, and in the air.
They had their home professionally remediated.
I then put Sherrie on another round of mold treatment.
She had COVID-19 in November 2021 but did not experience a UC flare even though her body was under stress from the virus. This showed her intestines were getting stronger.
Stopping Ulcerative Colitis in Its Tracks: Success at Last!
Sherrie had no UC flares through the winter of 2021—the first winter with no flares in nine years. Over the course of treatment, Sherrie would have long periods up to a year with no bleeding, but she might develop loose stools with blood for a few weeks and then go back into remission. But by 2022, she had gone a very long time with no visible blood in her stools. Now we were getting somewhere!
Her mold test came out clear. She felt great—high energy, no anxiety, and able to travel a lot in the winter and spring without fear.
At this point, I put her on a long-term program featuring antioxidants and pre- and probiotics. She’s taking minimal supplements and doing well.
Sherrie’s case shows that ulcerative colitis and inflammatory bowel disease respond well to a functional medicine approach. In IBD, there are many overlapping root causes that must be identified, treated, and modified, all the while working around a person’s flare-ups. Over time, Sherrie and I figured out her triggers and she learned the tools to stop her flares before they started. It may take some time, but ultimately a functional medicine practitioner can dig down to the root problem in order to heal ulcerative colitis.
Heal Ulcerative Colitis with Functional Medicine
Like Sherrie, you can heal ulcerative colitis by working with a functional medicine practitioner. That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you.
If after the call you come on board as a patient, I’ll order the right tests for you and start you on an anti-inflammatory protocol. The goal is to pinpoint your individual triggers and put ulcerative colitis in remission or cure ulcerative colitis altogether.
Natural Solutions for Hypoglycemia, Hyperglycemia and Insulin Resistance
Do you reach for a snack when you feel your energy levels drop mid-afternoon? Or maybe you’re just the opposite: lunch makes you so sleepy, you feel like curling up under your desk for a nap?
I’m going to let you in on a little secret…
The only thing eating should make you feel is not hungry.
If meals either give or drain your energy, that’s a sure sign you’re dealing with blood sugar dysregulation such as hyperglycemia, hypoglycemia, and insulin resistance.
Unstable blood sugar causes everything from cravings to mood disorders. It can hold you hostage from your ideal weight, cause inflammation, and even impact fertility. Not to mention, it can be the start of blood-sugar related diseases like Type 2 diabetes and Alzheimer’s (which is sometimes called Type 3 diabetes!).
On the other hand, stable blood sugar is the secret to reducing inflammation, having stable energy, better sleep, a better mood, and balanced hormones. I’ve even seen stable blood sugar have a positive impact on relationships (that’s why I always carry snacks for my toddler… and my husband!)
The bad news is that blood sugar issues are one of the most common problems I see in practice… but the great news is that there is an entire suite of things we can do to bring blood sugar back into balance.
What Are Normal Blood Sugar Levels?
Blood sugar is exactly what it sounds like: the amount of sugar in our blood. When we eat carbohydrates, they are broken down by the body into a simple sugar called glucose. Glucose crosses from the small intestine into the bloodstream where it can be taken up by the mitochondria - the “powerhouses''of our cells - and converted into energy, called adenosine triphosphate (ATP).
This process is helped along by key hormones like insulin and glucagon. Insulin is released by the pancreas and helps lower blood sugar levels by allowing sugar to enter the mitochondria, as well as be stored in the liver and muscles as glycogen, or stored in fat. Glucagon works in the opposite direction: it helps free stored glucose to raise blood sugar levels when they drop too low.This give and take is extremely important, as the body thrives when blood sugar remains stable - not rising too high or dropping too low.
When blood sugar levels are chronically low, it is called hypoglycemia. People with hypoglycemia often feel tired, anxious, or unfocused when they are hungry - and a meal helps energize them and allows them to focus. On the other hand, those with hyperglycemia (also called insulin resistance) have blood sugar levels that are too high. They feel tired after eating. Many people have symptoms of both hypo- and hyperglycemia at different times.
According to the American Diabetes Association (ADA), normal fasting blood sugar is below 100 mg/dL. Levels between 100-125 indicate pre-diabetes, and anything over 126 when fasting is considered diabetic. After eating (postprandial), the ADA considers 70-140 mg/dL to be normal.
But, what’s “normal” isn’t necessarily optimal. Fasting glucose can be “normal,” but you may still experience glucose spikes over 140 mg/dL throughout the day. Instead, I prefer to look for these signs of optimal blood glucose levels:
- Fasting: 70-90 mg/dL
- Postprandial: Below 120 with a return to pre-meal glucose levels within 2 hours (ideally below 100)
(For how to find your blood sugar levels, see “Testing Your Blood Glucose and the Benefits of Continuous Glucose Monitoring” below.)
What Is Hypoglycemia and What Causes Hypoglycemia?
Hypoglycemia is low levels of blood sugar, generally less than 70 mg/dL when fasting.
A Lactate dehydrogenase (LDH) level below 140 is also a sign of hypoglycemia.
Clinically, a person with hypoglycemia is often on the thinner side, and a “healthy” eater. However, they may skip meals (or just never feel hungry - only realizing they need to eat when they are shaky, foggy, or depressed), then have a mid-day crash, anxiety, and irritability. They often have strong sugar cravings in the afternoon or after dinner. When they do finally eat, they have improved energy and mental function- but it doesn’t last long! They also often struggle to stay asleep, as they don’t have the necessary glycogen stores.
The main complaints I see with hypoglycemia are:
- Fatigue, especially an afternoon or mid-day crash, or between or after meals
- Insomnia, trouble staying asleep or falling asleep
- Mood swings
- Anxiety
- Depression
- Hair thinning
- Infertility and hormone imbalances
- Impaired metabolism or weight gain
What causes hypoglycemia? The main culprits I see are a habit of missed meals, high-sugar snack, using caffeine or nicotine to suppress appetite, eating sweets or snacks instead of meals, and overtraining without properly replenishing glucose.
Low blood sugar can also be the first step toward developing insulin resistance and hyperglycemia. Low blood sugar causes a stress response, where cortisol rises and catecholamine spikes, to “save'' low blood sugar, which can cause nervousness, shakiness, and anxiety. Catchelomanes also suppress appetite, masking hunger and leading to more hypoglycemia.
What Is Hyperglycemia and What Causes Hyperglycemia?
Hyperglycemia is elevated blood sugar levels, with a morning fasting glucose above 99 mg/dL (though I prefer to see it below 92!), and levels after meals rising above 140 mg/dL. It is also signaled by an HBA1c above 5.6, though this marker isn’t always accurate. Fasting insulin levels above 5 indicate mild hyperglycemia, while levels above 10 indicate pre-diabetic levels of hyperglycemia.
If not addressed, hyperglycemia can intensify into diabetes, where fasting glucose is above 126, HBA1c is above 7, and fasting insulin is above 20.
Clinically, people with hyperglycemia often complain that after they eat, they feel fatigued, have impaired mental function, and often crave sugar. Chronic inflammation is another hallmark of hyperglycemia, and may present as anything from chronic joint pain to acne to autoimmune disease. Frequent urination is another key sign of hyperglycemia I look for. Finally, those with hyperglycemia often have a very hard time exercising, but once they do, have notable improvements in energy levels.
Hyperglycemia and insulin resistance are often used interchangeably. Hyperglycemia is simply the state of having high blood sugar - it could be a one-time thing due to a particularly high-carb or sugary meal. Insulin resistance, on the other hand, is a result of ongoing, sustained high blood sugar, which tells the pancreas to constantly make more insulin to help lower blood sugar levels back down. Over time, the body becomes less sensitive to elevated levels of insulin, and essentially “stops listening” - keeping blood sugar levels high.
What Are the Root Causes of Insulin Resistance?
Chronic stress, eating too many highly processed carbs, and lack of exercise all play a role in the development of hyperglycemia and insulin resistance. However, there are other factors at play that aren’t as simple to control as skipping the bun on your burger.
For instance, people with polycystic ovarian syndrome (PCOS) are genetically prone to be less insulin sensitive, even with a “perfect” diet.
In addition, the normal phases of the menstrual cycle can have a major impact on blood sugar levels. As progesterone rises in the week before your period starts, insulin resistance also increases, leading to elevated blood sugar levels. In addition, progesterone can also increase cravings for carbs and sugary foods, intensifying the problem. (It can also tank workout performance and hinder proper recovery!) On the other hand, estrogen, which rises during the follicular phase, actually increases insulin sensitivity.
For these reasons, I recommend people workout harder and eat more whole-food carbs during the follicular phase, then reduce carbs and do lighter training in the luteal phase. Use the last week of your cycle as a recovery period, and prepare to bounce back hard right after your period ends.
Testing Your Blood Glucose and the Benefits of Continuous Glucose Monitoring
You might have some symptoms of hyper or hypoglycemia, but the only way to know for certain is with blood glucose monitoring. I recommend continuous glucose monitoring with a monitor like NutriSense. This little device is convenient, painless, doesn’t require any finger sticks, and gives you 24-hour-a-day data on your glucose levels. Plus, you can wear it during workouts, sleeping, and everything in between.
Continuous glucose monitoring allows you to see the impacts of everything you do on your blood sugar levels - these are just some of the things I like to pay attention to:
- The types of carbs you eat whole food vs. processed)
- Eating carbs with or without other foods
- The time of day you eat carbs
- Workouts
- Sleep
- Menstrual cycle
- Stress
- Meditation and stress management techniques
You can use this information to optimize your lifestyle for wellbeing and glucose control. You may have never guessed that eating an apple alone at 10 AM would give you a crazy blood sugar spike - but now that you know it does, you can make a point to pair it with almond butter.
One other test I use with those with hyper or hypoglycemia concerns is the ION panel. This gives us a look at nutrient levels, so that we can make personalized supplement recommendations - like adding key blood-sugar control nutrients like magnesium, folate, and other B vitamins.
Elevated levels of Pyruvate, L-Lactate, and/or B-Hydroxybutyrate on an organic acids panel (like the ION/Organix or the OMx) are also potential signs of impaired insulin metabolism. But, because other things - like a strict ketogenic diet or deficiencies of specific nutrients such as CoQ10, B1, or pantothenic acid - can cause elevations in these markers, I only consider them in the context of other symptoms or lab markers.
Food, Fiber and Supplements to Help Stabilize Blood Sugar Levels
Fortunately, if your blood glucose levels aren’t stable, there is a lot you can do about it!
First up, let’s talk about what you can do at meals. Start with a glass of water with 2 teaspoons of apple cider vinegar mixed in. Next, take a look at your plate. Start by eating the greens on your plate - and if there aren’t greens (ideally you’re having greens with every meal) - instead grab a serving of fiber like PureLean Fiber, or Glucomannan Caps if you are on the go (I prefer powder in water as it works better!).
Once you’ve had your greens/fiber, move on to eating your protein and fat. Make sure you’re prioritizing eating enough protein - especially early in the morning. Finally, go ahead and eat your carbs as the last component of your meal. Bonus points if you eat meals containing carbs earlier in the day, as most people are more insulin sensitive in the morning and early afternoon. (And avoid refined carbs and added sugars, in general). If you find that you’re sleepy after meals, it's simply a sign you ate too many carbs at one time.
When you’re done eating, go for a walk. And if you don’t have time to walk, even just doing a few squats can really help. And when you’re done with dinner, be done, and skip those bedtime snacks. A 12-hour fast (from dinner to breakfast) is an easy goal to aim for. But just be aware: fasting longer than your body likes can actually backfire and drive cortisol levels up, so stick to 12-13 hours to start. If you’re not sure about the ideal fast length for your body, a continuous glucose monitor can help clue you in.
Away from the table, actively minimizing stress is key. Stress causes increases in cortisol, and cortisol spikes also spike glucose. If you don’t believe me, just look at your continuous glucose monitor. My glucose has gone up during a couple’s therapy appointment! Sleep is also essential: getting less than 6 hours of sleep per night increases insulin resistance.
I also encourage all my clients to fix any underlying gut health issues, especially an imbalanced microbiome. A lack of butyrate-producing bacteria decreases insulin sensitivity, which many of the proteolytic bacteria are gram-negative and contain pro-inflammatory LPS, which causes or increases insulin resistance.
Hormones play an important role, as well. In women, getting support for hormone balance early on in the peri-menopausal window (after around age 35 for most of us) is essential. Keeping levels of progesterone and estrogen adequate maintains insulin sensitivity. The decline in estrogen that eventually occurs can push up to 40% of women into pre-diabetes or diabetes at menopause. Alternately, having too much testosterone as a woman can make you more insulin resistant (like in many cases of PCOS). Progestin-containing birth control pills have the same effect, as they convert into androgen-like substances in the body. In men the opposite is true: too little testosterone can cause insulin resistance.
And finally, grab some weights: research has shown that building muscle is one of the best tools we have for improving insulin sensitivity.
For my clients, I also like to create custom supplement plans utilizing these nutrients:
- Alpha LIpoic Acid - one of the only substances actually known to recondition insulin receptors to make them more sensitive over time!
- Vitamin B1 (Thiamine) - shown to improve glucose tolerance.
- Chromium - regulates and enhances the effects of insulin.
- Myo-inositol and D-Chiro-Inositol- reduces glucose variability and improves fasting blood glucose.
- Berberine - lowers blood sugar comparably to the drug Metformin, increasing insulin sensitivity and production.
- Magnesium - low consumption of this mineral is associated with poorer blood sugar regulation and a higher risk of type 2 diabetes.
Other herbs I use include fenugreek, cinnamon, bitter melon, pycnogenol, and gymnema, among others.
Get Personalized Help with Your Blood Glucose Levels
Whether you’re dealing with hyperglycemia or hypoglycemia, insulin resistance, or even a diagnosis like diabetes, you have the power to take back control and help your body (and blood sugar) get back into balance.
For a customized plan, step-by-step support, and expert guidance, the first step is to book a free, no-obligation discovery call with my health team.
Learn about how we work with clients to achieve their unique health goals and help them step back into radiant health, so they can stop worrying about how they feel and start living a purposeful life.
>>> Book your free discovery call here