What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
Marina agreed to the test, and a few weeks later, results were in:
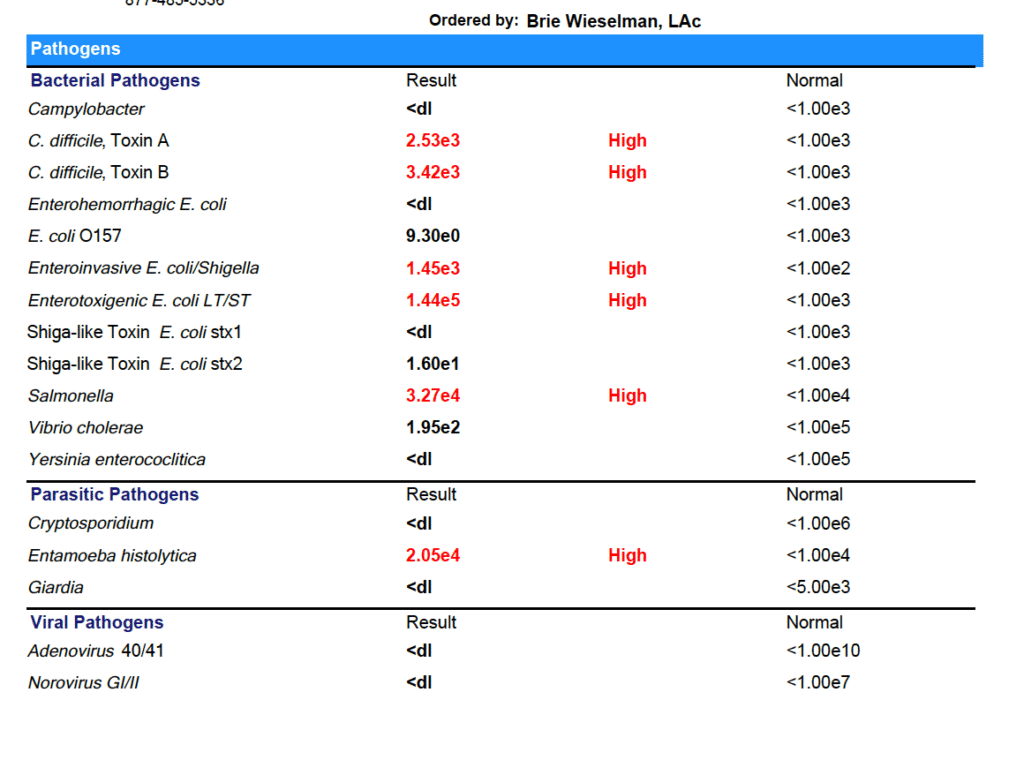
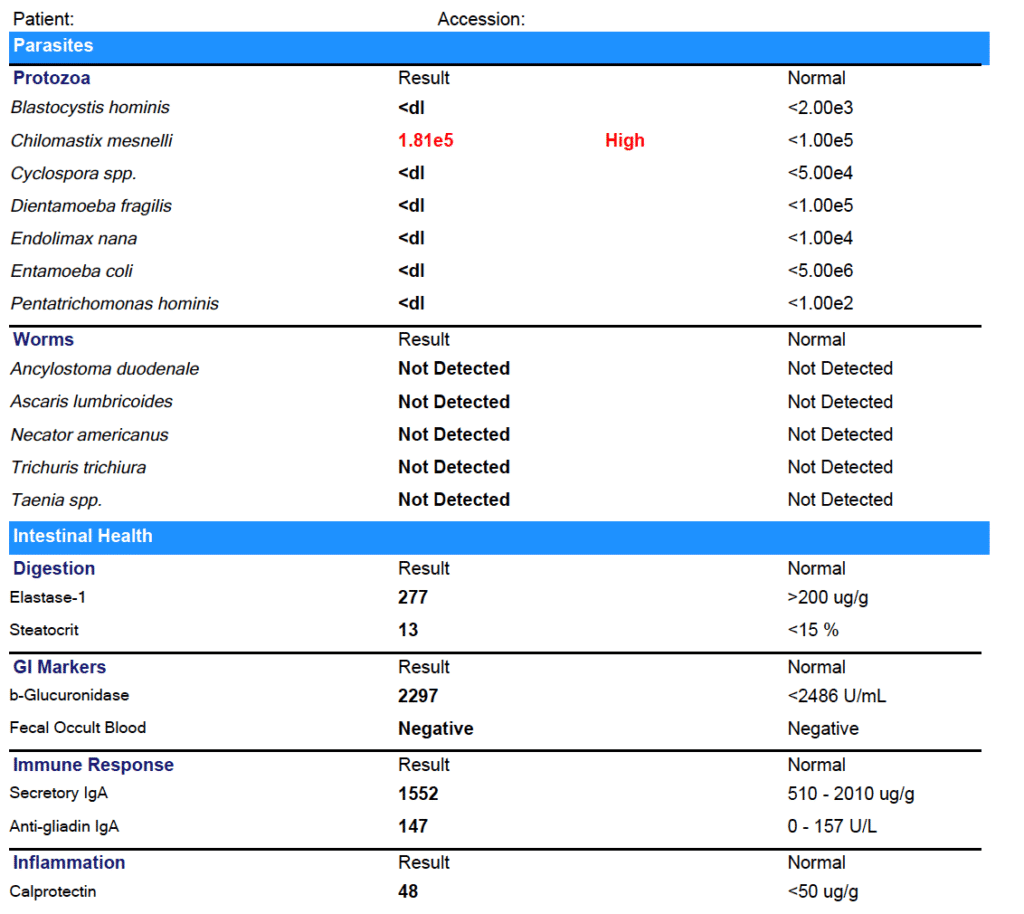
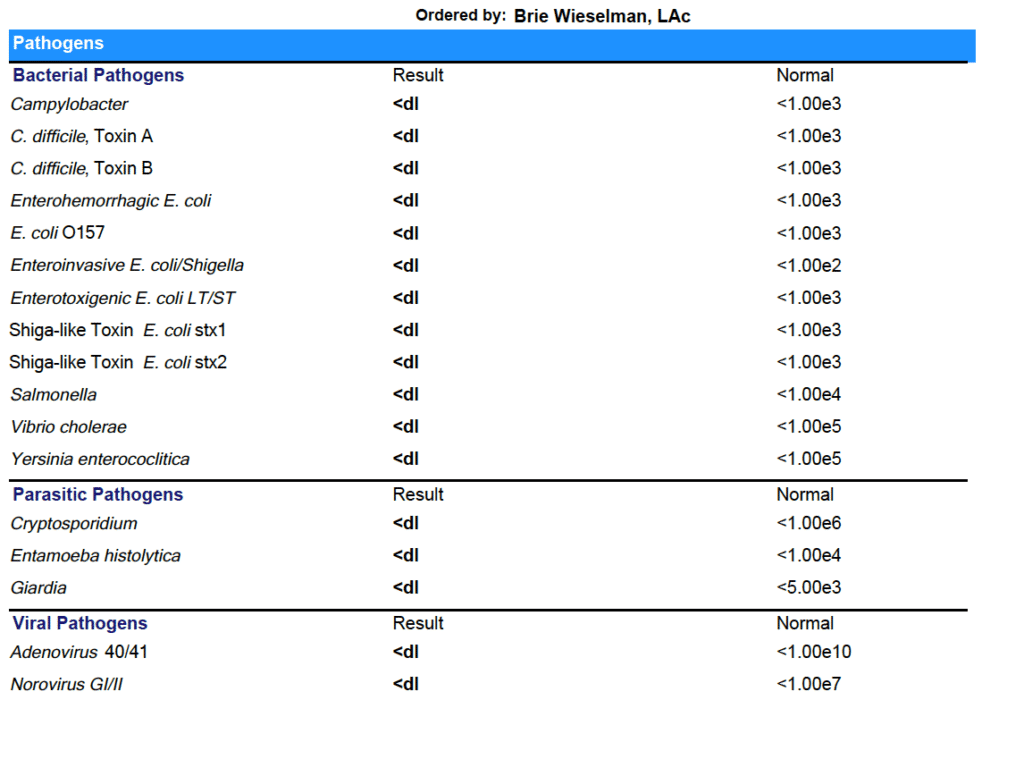
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
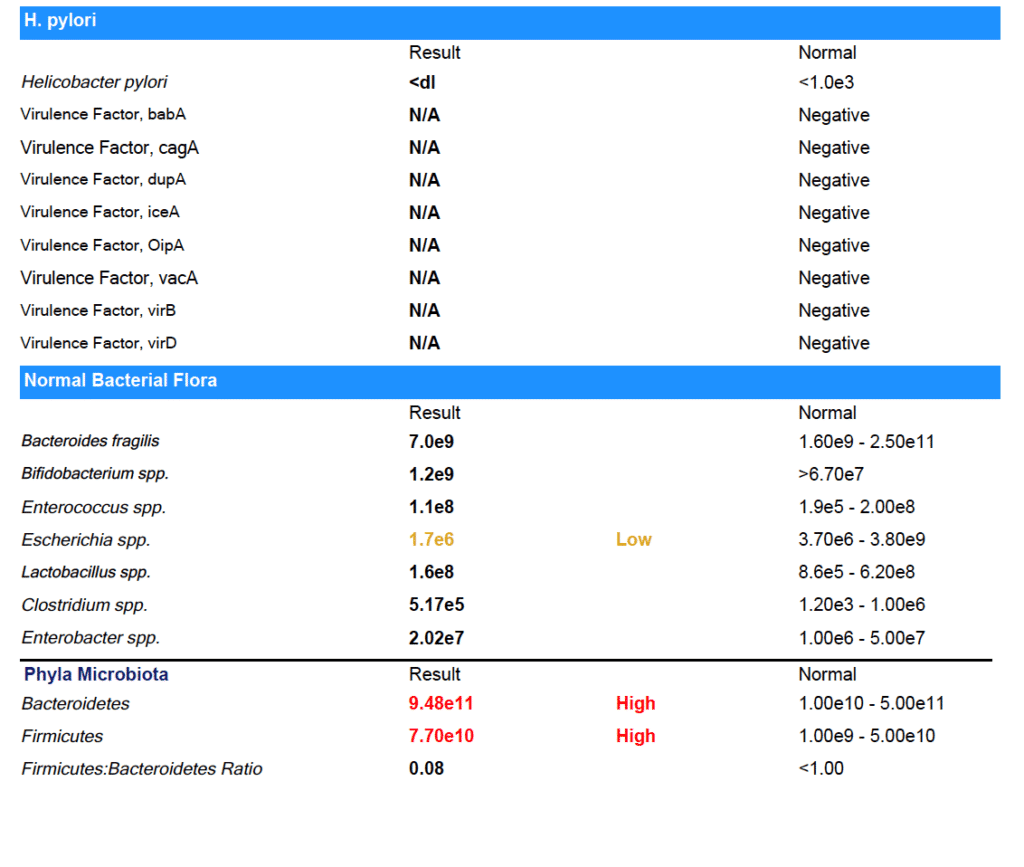
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
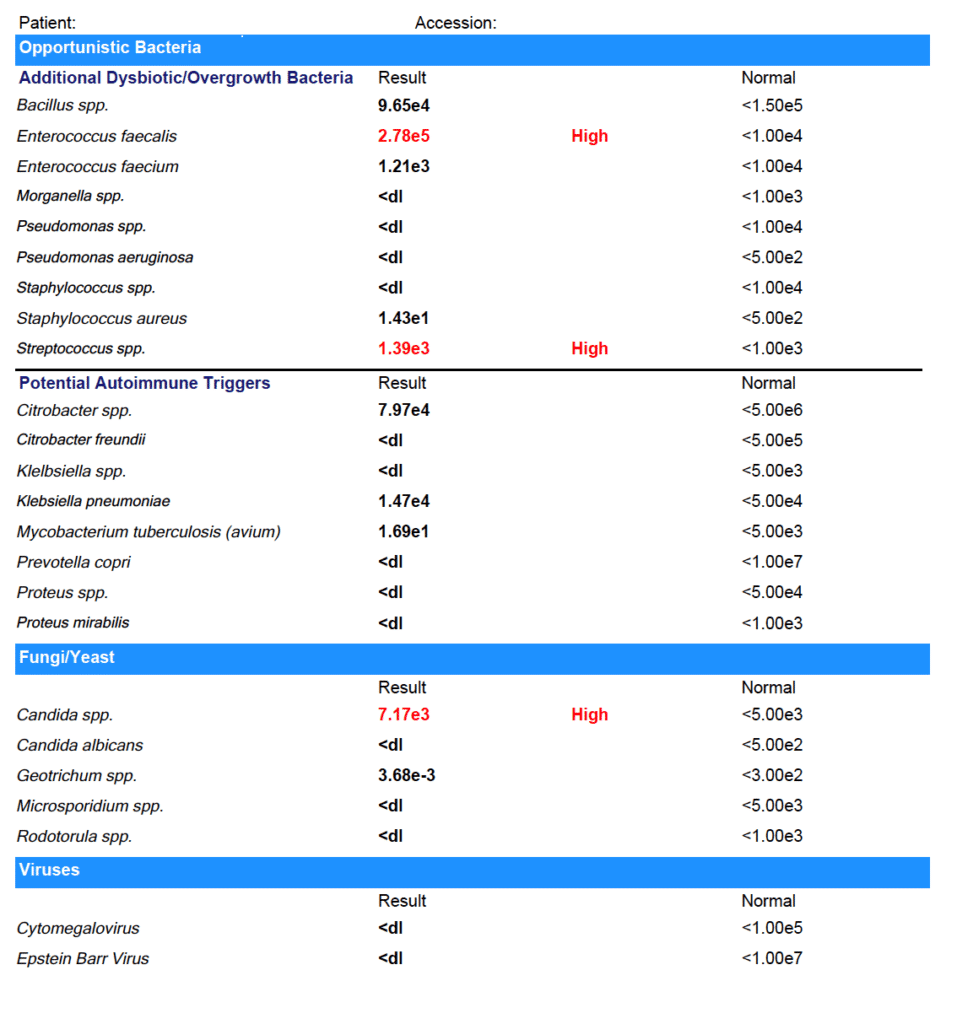
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
Step 3: The Second Test Results:
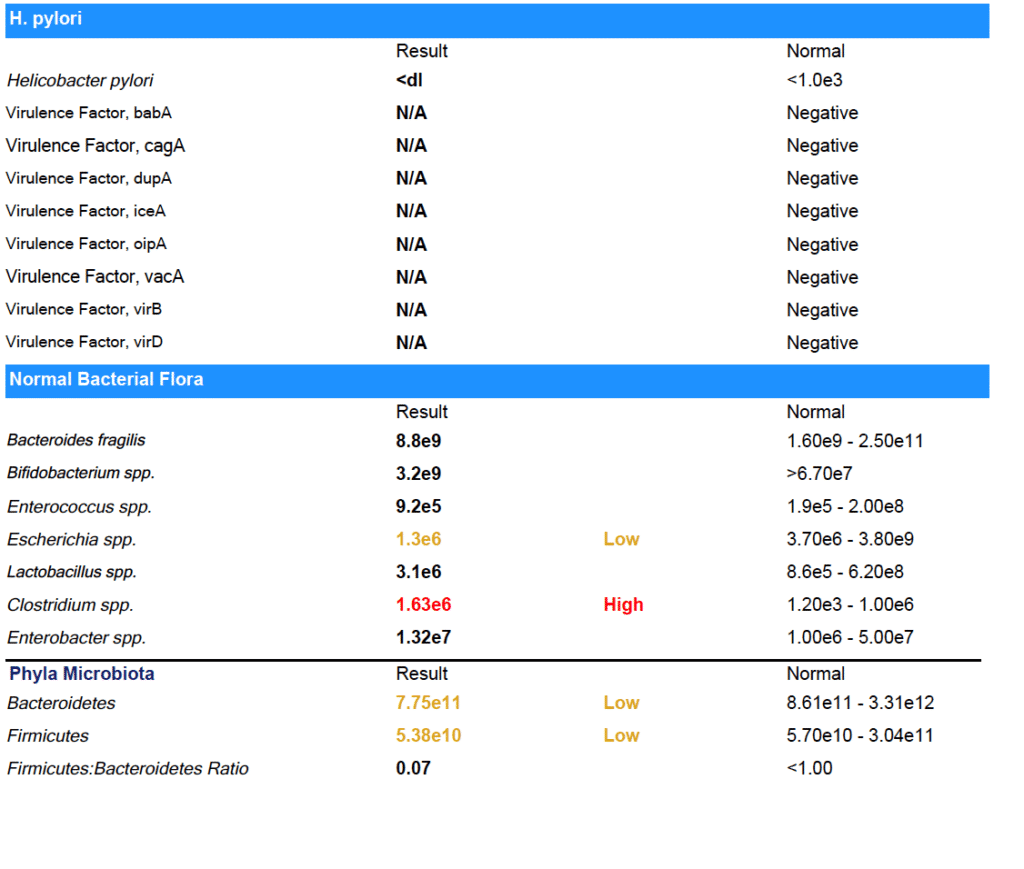
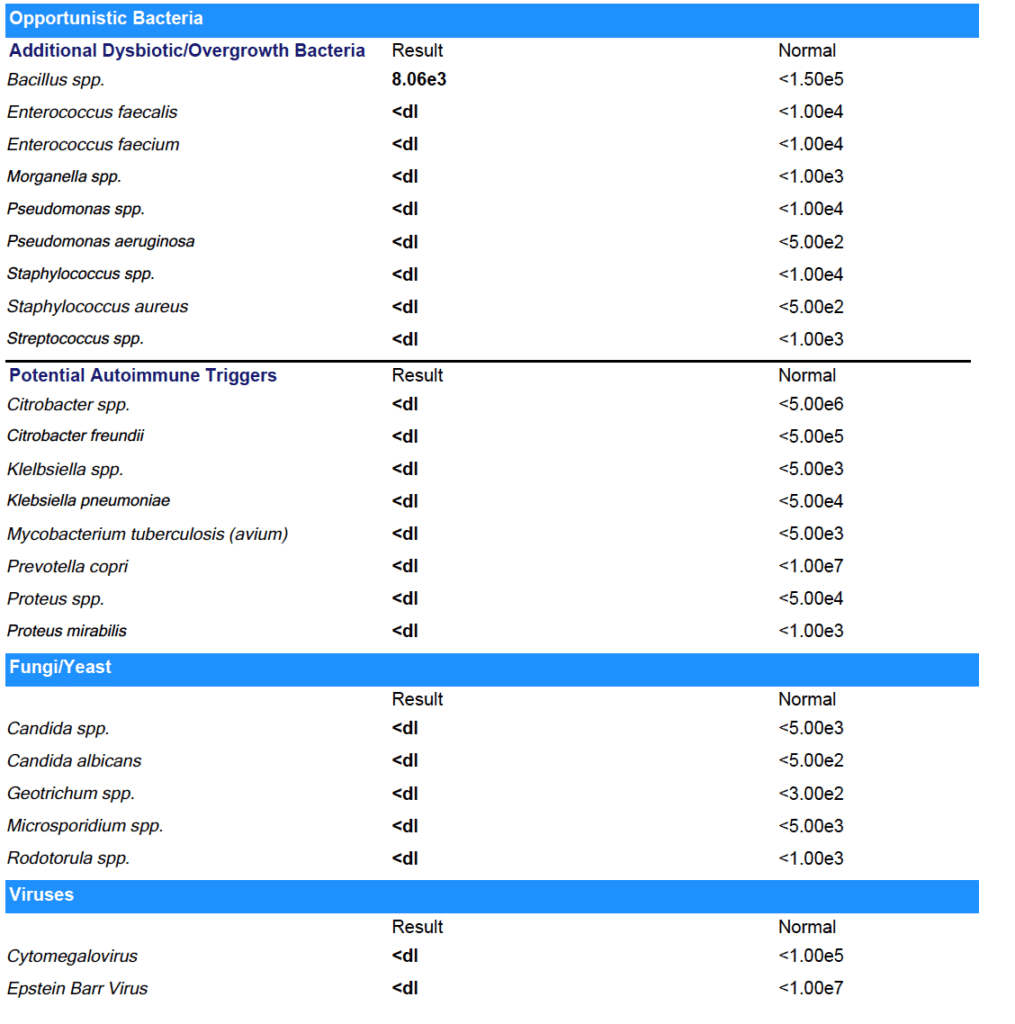
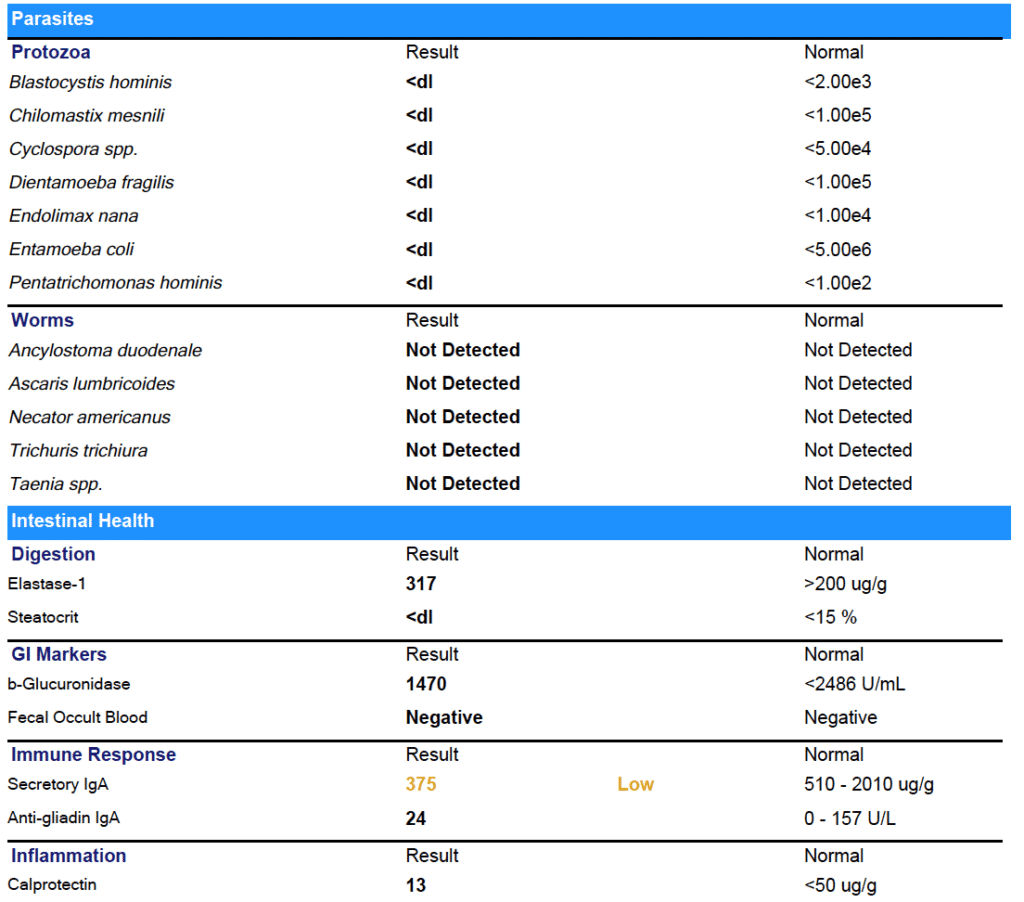
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
Acid Reflux and Chronic Urinary Tract Infection; Totally 'Unrelated' Symptoms With the Same Root Cause?
One of the principles of Functional Medicine is finding and treating the “root cause.”
But sometimes, it isn’t as simple as finding one root cause and getting rid of it. Most of my clients have multiple health concerns - and multiple causes behind them. Helping them is about peeling back the layers and addressing each one as we go.
For my client Jane, peeling back the layers was exactly what we needed to do! She came in because she was experiencing tightness in her chest caused by acid reflux - and we wound up working through multiple gut infections, addressing vaginal dryness, and putting interstitial cystitis (a condition that causes chronic bladder pain like a urinary tract infection) into remission.
Every time we treated another “layer” Jane felt better than before.
Today, Jane wants to share her story in her own words. If you’re considering pursuing help with a Functional Medicine Practitioner like me, I hope this story helps you better understand the process of working with a practitioner.
Jane’s Story
About three years ago, I started dealing with some bloating. Then, I’d occasionally have constipation - not all the time, but enough that I noticed it. I had a colonoscopy and the results came back normal. I started taking a probiotic. The bloating and constipation just became kind of a general annoyance I was living with.
But then I started feeling tightness and pain in my chest. That was really scary. I went to the doctor right away, but the tightness and pain weren’t heart-related. That’s when I realized they were actually a digestive issue. I decided to go see a physician at my regular clinic, and they told me it was acid reflux, prescribed Prilosec, and referred me to a GI doctor.
Luckily I had read enough about Prilosec to know I didn’t want to take a proton-pump inhibitor. Instead, I decided to get a second opinion from a Functional Medicine Practitioner - that was Brie.
Working With Brie
From the start, Brie was very thorough. She took a really detailed history that helped me connect some dots about what had started all my digestive symptoms in the first place. The past summer, I’d had a urinary tract infection and taken a course of antibiotics. Then in the fall, I went traveled out of the country and had to take a course of the antibiotic Cipro for traveler’s diarrhea. That's when the bloating and constipation became worse and the other acid reflux symptoms started.
But she wasn’t just interested in the acid reflux - Brie asked questions about my overall health. When I told her I was experiencing vaginal dryness, urinary pain, and low libidio, she took me seriously. My doctor had diagnosed my with interstitial cystitis - basically pain in my reproductive organs for no reason.
Brie explained to me how the antibiotics had killed the good bacteria in my gut as well as the bad. She recommended stool testing and a breath test for Small Intestine Bacterial Overgrowth (SIBO), as well as hormone testing. She also recommended I cut out dairy and gluten temporarily to give my system a break, since those foods are common gut irritants. She also recommended some supplement that would soothe my gut and help with symptoms until we got the test results back. All this happened at our very first meeting!
The Test Results Came In
The test results came back a few weeks later - they showed low cortisol, low estrogen, H. pylori, low beneficial flora, and a few overgrown bacteria (citrobacter, pseudomonas). Plus, I had both methane and hydrogen type SIBO and was under-producing pancreatic enzymes.
It was a lot to take in and I was so glad I had Brie to help me understand what the results meant. She saw how everything was connected.
Brie explained that the H. pylori infection was likely causing the acid reflux, and that the SIBO was probably the cause of the constipation and the uti bloating. My hormone problems were tied in to all of it and causing the vaginal dryness, urinary pain, and low sex drive.
It was a relief to know there was a reason I was feeling the way I was feeling - especially because my symptoms had gone into a flare as we waited for the test results. I remember going to visit a friend for a few days and having to come home early because I was just so uncomfortable.
Brie started my on a supplement protocol for 6-8 weeks for both the H. pylori and the SIBO. I kept avoiding gluten & dairy, too.
After I finished the first supplement protocol, we re-tested. The H. pylori was gone! The SIBO levels had come down, but it wasn’t completely gone. On the second stool test, I also had positive results for some other common gut infections and parasites, including candida overgrowth. Brie explained that all of this was normal - the first protocol of supplements had helped destroy the “biofilm” - the protective cover the bad bacteria use to protect themselves and hide. With the biofilm gone now, we could see other parasites and better treat the SIBO, too.
By, then my acid reflux was totally gone and I was feeling pretty good gut-wise. But I was still struggling with the vaginal dryness and hormone symptoms. And, what I initially thought was a bladder infection turned out to be Interstitial Cystitis. The “UTI” pain didn’t respond to normal treatments, and the pain turned chronic. Can a UTI cause bloating and constipation?
Putting Interstitial Cystitis Into Remission
My hormone symptoms were slowly improving as my gut healed - but Brie also suggested using a plant-based bioidentical estrogen replacement. She also had me use vaginal DHEA, a vaginal probiotic, and some herbs. Those helped me feel better right away.
Brie also explained that two of the bad bacteria that the tests had shown were overgrown in my gut - proteus and citrobacter - were related to the Interstitial Cystitis, too. As we treated those, my symptoms disappeared completely.
Brie suggested I work with a pelvic floor therapist, too. That helped me relax some overly tight muscles that were contributing to the pain.
Changing My Diet
Brie suggested I follow a gluten and dairy-free, low-FODMAP diet. It helped me a lot in the beginning, but I was anxious to reintroduce more foods as soon as I could.
After a few months, I was able to reintroduce beans and some other legumes, which I hadn’t been able to tolerate for years, and I really missed. I am now back to eating all fruits and veggies, and I can even add in a little gluten here and there. That makes me feel good!
Where I Am Now
After working with Brie, I feel great for the first time in years.
I came to see her because of the acid reflux - but she opened my eyes to a lot of problems I had been writing off as “normal” or just “part of getting older.”
Gut-wise, I am feeling so much better now! After having given up gluten and dairy for years, I’m finally able to experiment with adding them back into my diet again now.
The interstitial cystitis pain is gone now, too. I didn’t realize how much the pain held me back from enjoying life - I even cancelled an overseas trip because of it!
I’m so happy to be where I am now with my health. I’m following a maintenance protocol now and continuing to meet with Brie occasionally to make sure I’m doing the right things moving forward.
Working with Brie has made a huge difference for me, and I wish more people could have access to it! I hope my story helps to spread the word.
Do You Need Help, Too?
Jane had amazing success - she cleared multiple gut parasites, fixed her digestion, reversed interstitial cystitis, and was even able to reintroduce foods she hadn’t eaten in years.
Why was she so successful? Because she dedicated herself to working through the process of Functional Medicine. She didn’t give up even when it got complicated - and neither did I!
I hope reading Jane’s story has helped you understand better understand the process of working with a Functional Medicine Practitioner like me.
If you’re inspired and ready to start your own journey, you can book a free, no-obligation Prospective Patient Interview with my team. During this 20-minute appointment, we’ll learn about you and discover if you’re a good fit for working with us.


