The REAL Meaning Behind Adult Acne (And How To Get Rid of It For Good)- Part One
You wake up on the day of your dream-job interview, look in the mirror… and there it is, a big pimple on your chin.
You wish you could blame it on nerves, but the truth is that lately your skin is more broken out than it was when you were a teenager. You don’t know what else to try...
- You’re already spending tons of cash on facials and trips to the dermatologist
- You’ve tried every “miracle” regimen at Sephora
- You even tried cutting back on nights out with your girlfriends!
But here’s what you don’t know… what you think is just “annoying adult acne” might actually be more than that. It could be a sign you have Polycystic Ovarian Syndrome.
I know what you’re thinking - you’ve heard of PCOS and you couldn’t possibly have it! You have normal cycles (well, at least your birth control pill makes them seem normal), you’re not overweight (although you do feel like you carry a bit more weight than you should, given how active you are), and you don’t have any other symptoms (except the acne… and your hair is thinning a bit… and the need to wax your lip every month…).
Listen girl, I get it! When I found out I had PCOS, I was shocked. But it turns out, I actually had a pretty atypical case. And you might too.
Misinformation about what PCOS is and the symptoms it can cause let many women slip through the cracks and never get the diagnosis or treatment they deserve.
Adult acne isn’t normal, and it isn’t something you should have to deal with. Finding the root cause of your acne and addressing it can mean clear skin and better health (because acne is always a sign of a bigger problem). And even if you’re certain you don’t have PCOS, keep reading anyways - you may be surprised by what you learn!
What PCOS Is (And Isn’t)
The #1 misconception about PCOS is that it is simply a condition where cysts develop on the ovaries. So wrong. In fact, some women with PCOS don’t even have cystic ovaries!
PCOS is actually the most common type of hormone and metabolism imbalance. It affects 1 out of 10 women. (Yes, that number is the same as 10% - a huge amount.)
Based on the Rotterdam Criteria from 2003, there are 3 diagnostic criteria for PCOS - and to be formally diagnosed, you have to have at least 2:
- Confirmed androgen excess on labs or androgen excess symptoms
- Ovulatory dysfunction
- Multiple cysts on ovaries (PCOM) diagnosed via imaging ultrasound
If you have at least 2 of the 3 criteria above, your doctor can diagnose you with PCOS.
In 2018 PCOS diagnosis guidelines were updated by a combined counsel of the Australian National Health and Medical Research Council, European Society of Human Reproduction and Embryology, and American Society for Reproductive Medicine.
It was a HUGE step forward in the treatment and diagnosis of PCOS, since the new guidelines (finally!) took into account how different PCOS can be in different women.
Here are their new recommendations:
- Androgen excess can be diagnosed by measuring free testosterone or bioavailable total testosterone. However, elevations in the hormones Androstenedione and DHEAS can also indicate PCOS, even without elevated testosterone.
- When irregular menstrual cycles are present, a PCOS diagnosis should be considered. Irregular is defined as cycles less than 21 days, greater than 35 days, or less than 8 cycles per year. However, ovulatory dysfunction can still occur with regular cycles - this can be confirmed or ruled out with serum progesterone levels taken in the second half of the cycle.
- Ultrasound should not be used for the diagnosis of PCOS in those less than 8 years out from their first period, because many younger women have multifollicular ovaries, even without having PCOS.
The new diagnostic criteria don’t mention weight - and that’s because your weight is not part of the diagnosis for PCOS. Only 30% of people with PCOS are overweight or obese. And pain is not a symptom of PCOS, either.
What Does PCOS Do To You?
The hormone imbalance in PCOS creates problems with how the ovaries function, so the egg that should develop each month may not, or may not be released during ovulation (aka anovulation).
Some women think that if they aren’t actively trying to get pregnant, anovulation is no big deal - but regular ovulation is a sign your body is humming. Many women with PCOS also experience irregular cycles. Again - this is more than just a fertility problem (though it is that too!) A healthy period is a sign your overall health (physical & mental) is good
(Side note - if your doctor prescribed the pill to regulate your cycle, this is still a problem! More on that later, so keep reading).
But PCOS is about way more than just ovulation.
Excess Androgens Are The Real Cause of Adult Acne
Women with PCOS tend to have an excess of androgens. Androgens are male hormones, and an excess can mean high testosterone, high DHEA, or high metabolites of either.
Excess androgens are responsible for some of the most dreaded PCOS symptoms like:
- Acne (especially on the chin, jaw, and back)
- Male pattern hair loss/thinning
- Hirsutism (male-pattern hair growth, like on the face)
- Anger, irritability, mood swings
- Poor stress response
- Increased anxiety and depression
Not every woman with excess androgens has all of the above symptoms - and sometimes one symptom can be severe (like acne!) while other can be more mild (maybe just a bit more hair on your upper lip).
But pay attention here - hormones levels are complex! Many women with PCOS also have symptoms of high estrogen. It commonly happens like this: DHEA is high, but progesterone is low relative to estrogen levels. On top of that, many women have poor estrogen detox because their liver is overburdened.
How PCOS Presents in Real Women
Remember, every woman is unique - but there’s a common scenario I see in my clinic with women with PCOS. And - full disclosure - I was one of these women too!
Here’s a story I hear from a typical PCOS patient with acne in my clinic about her teenage years/early 20s:
- Her period came in her later teens (or never started naturally)….or started “on time” but then had irregular long windows between
- Acne started to develop and so did hair in places she didn’t want it --(like nipples, lip, chin, stomach)
- She may have been put on oral birth control pills to “regulate” her period and help deal with the acne
- And she might have been put on antibiotics like tetracycline or Accutane to further help control the acne
Sound familiar to you?
Then, as she aged into her 20s and 30s:
- As other women’s acne clears up, hers is getting worse than ever
- She may start to gain weight around her middle (even if she remains thin), or struggle to control her weight despite a healthy lifestyle
- Her hair might lose its luster and start to thin
- She may notice more anxiety and depression, trouble recovering from stress
And if she decides to stop taking the pill, here’s what usually happens:
- Her period takes a long time to return after stopping the pill - or it NEVER comes back
- Can’t conceive easily or without intervention
Not all of these symptoms are drastic (although some women do have very dramatic symptoms as a result of PCOS) - they can be subtle annoyances that hint at a bigger underlying problem.
What Not To Do If You Have PCOS & Acne
Most doctors - be they GPs, gynecologists, or dermatologists - only think of acne as a cosmetic issue. They often don’t make the link between acne and bigger issues like PCOS or hormone imbalance - especially if your other symptoms are mild or masked by the artificial hormones in the pill.
So, if you go see your doctor complaining about acne, you’ll probably be given one of these 3 things:
- Oral contraceptives (birth control pills)
- Antibiotics like tetracycline
- Medications like Accutane
While these meds might help short-term for some women, in the long-run they only make PCOS symptoms worse. Research has shown women with PCOS already have a less diverse microbiome than women without PCOS (and, that increasing microbiome diversity may be an essential part of treatment). The pill, Accutane, and antibiotics all only further damage the microbiome (especially when you’re taking them long term!)
Our microbiome (aka all the bacteria living in our gut) are critical for hormone biotransformation - that means they help produce and then clear out hormones. To have healthy hormones, (and clear skin) you’ve got to have a healthy gut - and taking any of these common acne meds can wreck your gut!
(It always comes back to the gut!)
Don’t Panic!
If you’re reading this and thinking you may have PCOS - or are nodding along because you were prescribed the Pill and antibiotics to treat your acne - please don’t panic!
Our bodies are so resilient, and there is a lot you can do to balance your hormones. In Part Two of this article, I’ll explain exactly what you CAN do and how I help women with acne, hormone imbalances, and PCOS in my clinic. Check out Part Two here.
Are Worms The Next Frontier of Health? Everything You Need to Know About Helminth Therapy
I talk a LOT about clearing infections and overgrowths - Small Intestine Bacterial Overgrowth (SIBO), yeast overgrowth (candida), and of course, killing parasites.
So I was shocked when I first heard about a new treatment idea for treating disease and healing damaged gut: worm therapy. Not clearing worms. Giving them to the patient, to help heal disease.
No, I’m not joking. It’s called helminth therapy - named for the type of organism used Hymenolepsis Diminuta Cysticeroids (HDCs). HDCs are the larval form of a very specific type of worm that help to restore immune tolerance and diversity to the microbiome when it’s been damaged.
I was really skeptical when I first heard about this. But then I heard a presentation given by one of my medical heros, Dr. Sidney Baker (former faculty member of Yale Medical School, founder of Defeat Autism Now! and Autism360.org, Linus Pauling Award recipient) and Dr. Yehuda Shoenfeld at the Institute for Functional Medicine conference in May 2018.
They shared the latest research and their experience using helminth therapy - and I went from skeptical to excited. I slowly introduced helminth therapy in my own practice and saw amazing results.
Here’s what I want you to do: suspend all your judgement for the next 10 minutes and read the rest of this post. I promise you’ll be surprised by what you learn - and I bet you’ll want to learn more about helminth therapy.
HDCs Aren’t Just Any Worms
HDCs are the larval form (aka an intermediate life stage between egg and worm) of a small helminth. Helminth grows naturally in grain beetles, which were a common part of our food supply up until about 100 years ago.
HDCs are not a parasite. By definition, a parasite causes harm to an organism - HDCs cause no harm. HDCs stay in the gut - they cannot breach the gut wall.
Really important: HDCs cannot colonize in humans. That means they’ll never go from larvae to worm in a human. For that same reason, HDCs can’t be passed from human to human either. They’re NOT contagious from person to person.
Using helminth therapy is completely different from something like taking a tapeworm from Mexico. It’s produced in sterile lab conditions (just like probiotics are) and carefully controlled.
How Are HDCs Produced - And How Do You Take Them?
Therapeutic HDCs are grown in sterile conditions in a lab - much the same way probiotics or yeast for brewing beer or culturing yogurt are.
First, the eggs are grown in rodents in the lab. If that makes you squeamish, keep in mind that these animals are kept in MUCH more humane & clean conditions than most farm animals! Then the eggs are taken and are bred into larvae in grain beetles which eat only oatmeal. The HDCs are harvested from the grain beetles and suspended in salt water.
HDCs are given orally (again, just like probiotics!) through the salt water solution. You’ll take a tiny vial (about the size of the tip of your pinky finger!) that holds the microscopic organisms. If you hold the vial up to the light, you can just barely see the HDCs as tiny white flecks.
Unlike probiotics - which can contain billions of CFUs per capsule - HDC are given in very precise, small amounts: most people start with 10 HDC per vial and work up to 30 HDC. Strong, therapeutic doses of up to 100 HDC every 2 weeks can be used, too.
If you do ingest HDCs, they can only stay in your body for about 2 weeks.
How Does Helminth Therapy Work?
This is the part that’s really exciting:
Helminth therapy works by promoting microbiome diversity and restoring immune tolerance.
Remember - our body isn’t sterile. Our microbiome is teeming with important bacteria and other organisms that help it function: both flora (like probiotics) and fauna (beneficial things like HDCs). When the gut microbiome doesn’t have enough diversity of both flora and fauna it can’t perform its functions properly.
Our gut microbiome teaches our immune cells how and when to function and it establishes our intestinal barrier (which keeps pathogens out of our bloodstream). Our immune cells are our body’s defense team. Immune tolerance is what our immune cells won’t react to. It’s our body’s bouncer waving something through.
Immune tolerance is a good thing! It means your body won’t wage war on the strawberries you ate, or cause you to sneeze and cough when you’re outside around pollen.
If you have decreased immune tolerance, you’re more likely to experience these conditions:
- Allergies (both seasonal and to foods)
- Eczema
- Asthma
- ALL autoimmune conditions (things like endometriosis, multiple sclerosis, lupus, rheumatoid arthritis, vitiligo, Hashimoto’s, alopecia, ulcerative colitis, Crohn’s and more)
Today, 50 million Americans have been diagnosed with an autoimmune disease. That’s up from 9 million in 1997. (Still a huge leap even when you factor in increased testing/awareness.)
Experts like Dr. Baker and Dr. Shoenfeld agree: the best way to treat ANY chronic illness is to restore immune tolerance.
What Makes Our Microbiome Diversity & Immune Tolerance Decrease?
Up until the very recent past (like the past 100 years) our microbiome diversity was supported naturally by our environment. People interacted more frequently and directly with nature: farming, foraging, etc. They also had less hygiene practice: no antibacterial soap or hand sanitizer.
Worms - both beneficial ones like HDCs and pathogenic ones - were also something more people had when we lived hunter-gatherer lifestyles. (These persist in hunter-gatherer groups like the Hadza tribe today - and they have the most robust and diverse microbiomes of anyone known on the planet… and virtually no IBS, UC, Crohn's, diabetes or other autoimmune disease!)
Other things in the modern world that damage our microbiome diversity:
- Antibiotic use (kill beneficial bacteria in the gut)
- PPIs (impair digestion and promote bacterial and fungal overgrowth)
- Birth control pills (kill beneficial bacteria in the gut and promote yeast)
- C-section births (prevent transfer of microbiome from mother to infant in the vaginal canal)
- Vitamin D deficiency (too much time indoors)
- Chronic stress (go-go-go cultural attitude)
- Contaminated/nutrient poor food (Standard American Diet!)
- Excessive hygiene practices (overuse of antibacterial cleaning agents)
How To Restore Microbiome Diversity & Immune Tolerance
Diet has the biggest influence of all factors on the health of our microbiota. Less diversity in your diet = less diverse gut bugs.
Step 1 has to be eating a nutrient-dense diverse diet with plenty of gut-nourishing foods: fiber, healthy fats, and protein.
Making changes to your lifestyle & hygiene practices is important too:
- Put down the antibacterial soap!
- Get out in nature and interact with the earth
- Get adequate sunlight or supplement with Vitamin D
- Eat fermented foods or supplement with a high quality probiotic
But if you already have all these steps dialed in and are still dealing with symptoms of decreased immune tolerance or chronic illness, helminth therapy that can increase diversity and immune tolerance may be the next step for you.
What The Research Shows About Helminth Therapy (And Results in MY Practice!)
- In the largest randomized control trial in history (!), 1 million children in India were dewormed by researchers who hypothesized it would lead to an improvement in general health. Instead, they found no significant effect on weight, death rate, or health. This drew into question the premise that all worm are always harmful…
- In a 2005 study, 29 patients with Crohn's disease (most of whom were non-responsive to pharmaceutical treatments) were treated with helminth therapy every 3 weeks for 24 weeks. At 24 weeks, 79.3% of the participants had responded favorably and 72.4% had completely reversed their Crohn’s disease!
- In this 2014 study, people with IBD (either ulcerative colitis or Celiac Disease) were treated with either helminth therapy or a placebo for 12 weeks. Although this study was too small and too short to be conclusive, 10% of those who received the helminth achieved remission (compared to 4% in the placebo group).
In my own practice, I’ve seen these results using helminth therapy:
- Normalization of thyroid labs
- Remission of Crohn’s and Ulcerative colitis (when symptoms have already been improved and other co-infections addressed)
- Improvement of GI symptoms (diarrhea, constipation, gas, bloating, etc.)
- Reduction of arthritis symptoms
- Improvement of inflammatory symptoms like skin rashes, insomnia, and mood/brain issues
- Reduction of histamine intolerance symptoms
Other practitioners have reported improvement in children with autism and people with multiple sclerosis.
Who Helminth Therapy Is (And Isn’t For)
There’s no magic potion in medicine that will cure all your problems (i’m sorry!).
If you’re not eating right, moving, finding joy, and managing your stress, helminth therapy won’t work for you.
But if you’ve already got those “core” practices in place and are still struggling (or just want to see how good you can feel!), helminth therapy could be beneficial for you.
Typically people take 6 doses of HDCS 2 weeks apart to initially evaluate if they are or are not going to have a beneficial response. Then, if no benefit is seen, they can increase the dose for. Risk is almost non-existent, and the potential benefits are huge.
(But, anyone on immunosuppressive drugs - like those used in some types of inflammatory bowel disease or other autoimmune diseases - shouldn’t take HDCs. The helminth therapy is not beneficial if your immune system is suppressed by medication.)
What Do You Think?
I am so glad you stayed with me.
I know that “worm therapy” sounds really weird at first- but the idea of taking probiotics was once weird, too! I’m a supporter of anything we can do to improve our gut health - because our gut health radiates out into every aspect of our being.
Want to learn more about helminth therapy (and potentially give it a try?) - book a free 15 minute consult with my team where we can create an action plan for you.
Want to get healthier but NOT ready to try HDCs? That’s OK too - I’d love to teach you about how else you can support your gut. Book a free 15 minute consult with my team here.
What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
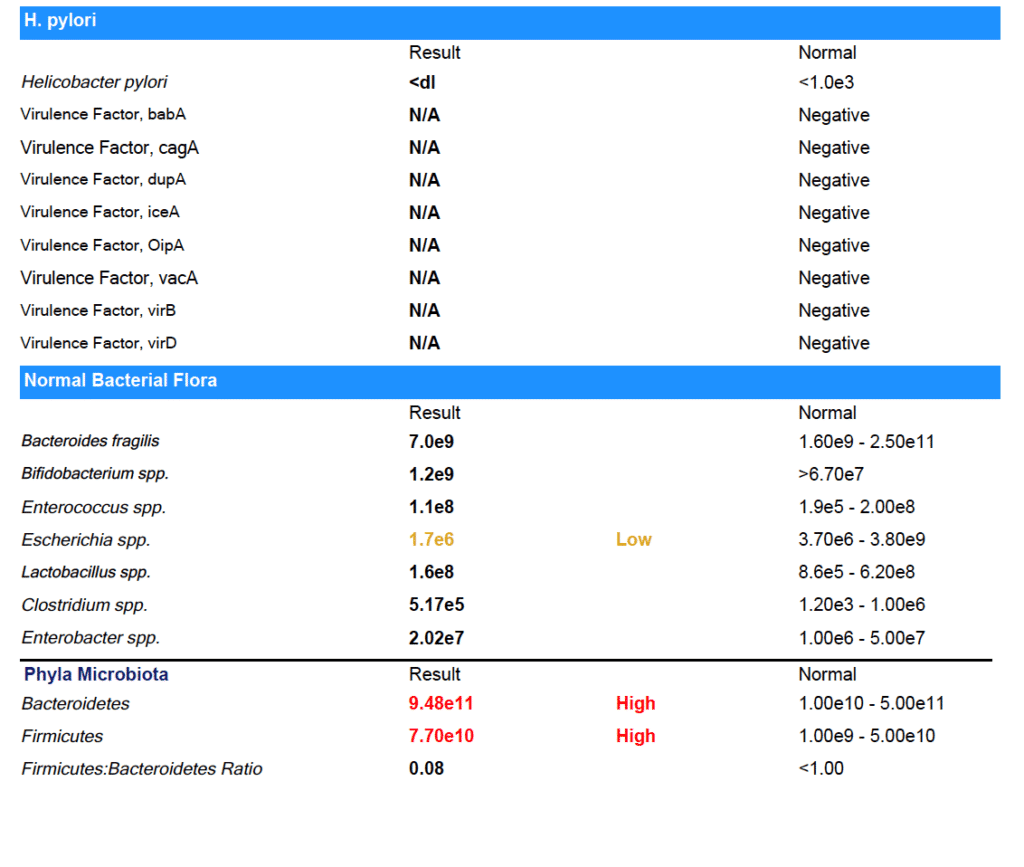
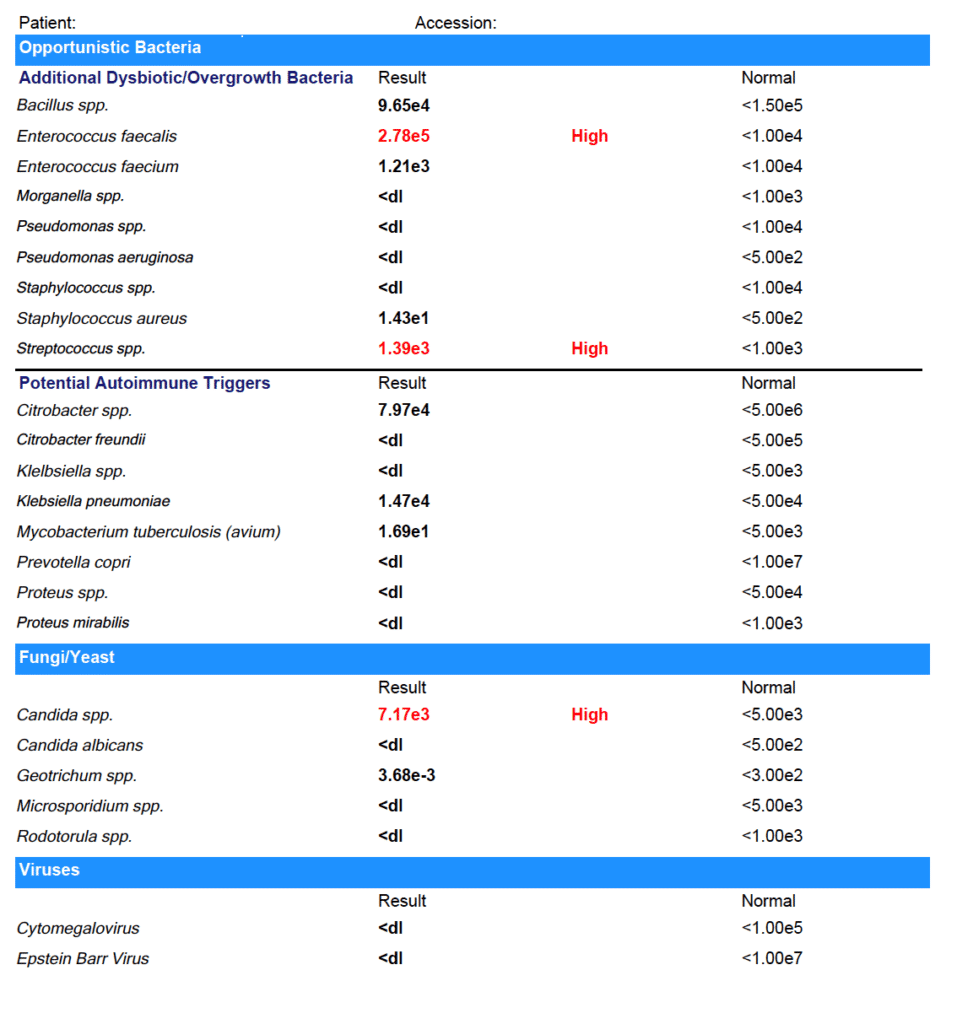
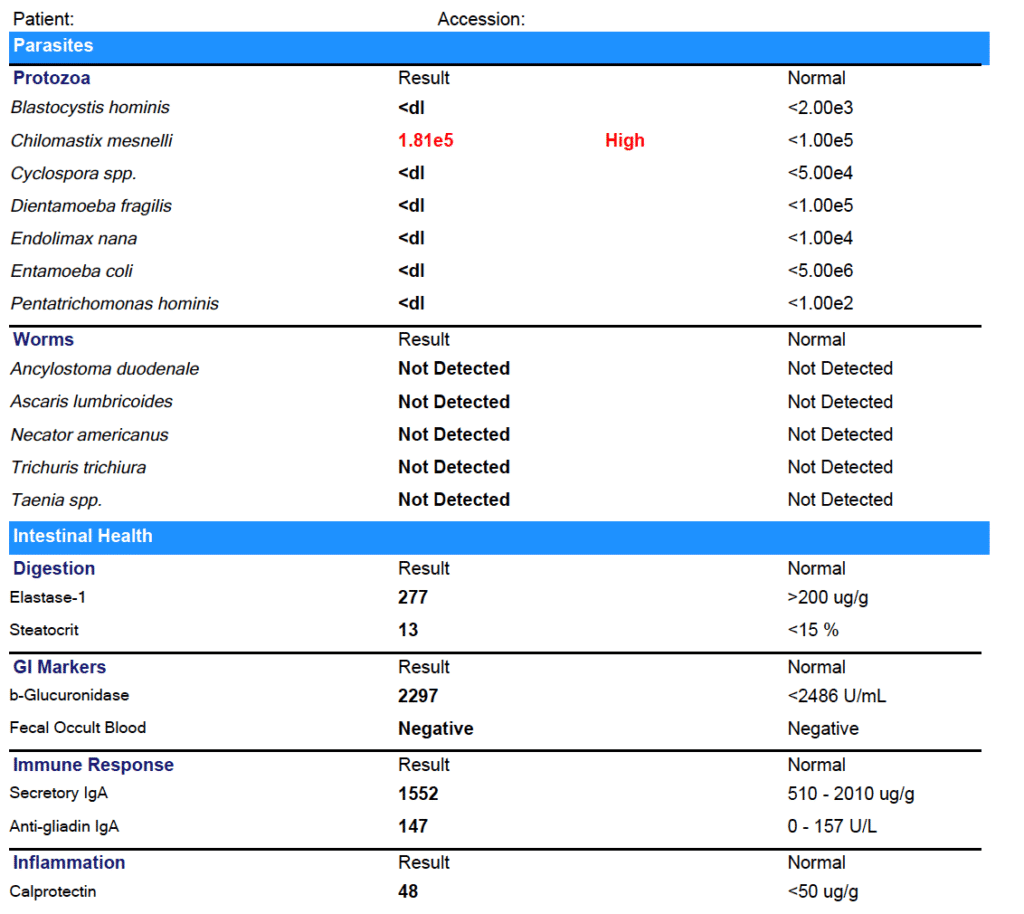
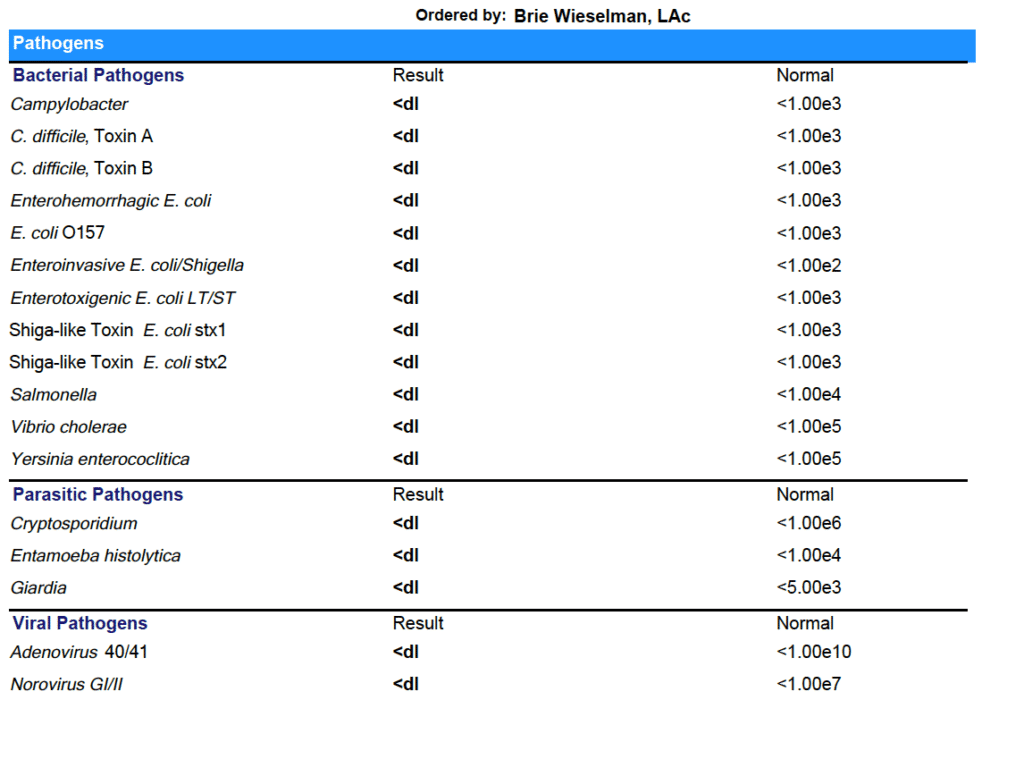
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
Marina agreed to the test, and a few weeks later, results were in:
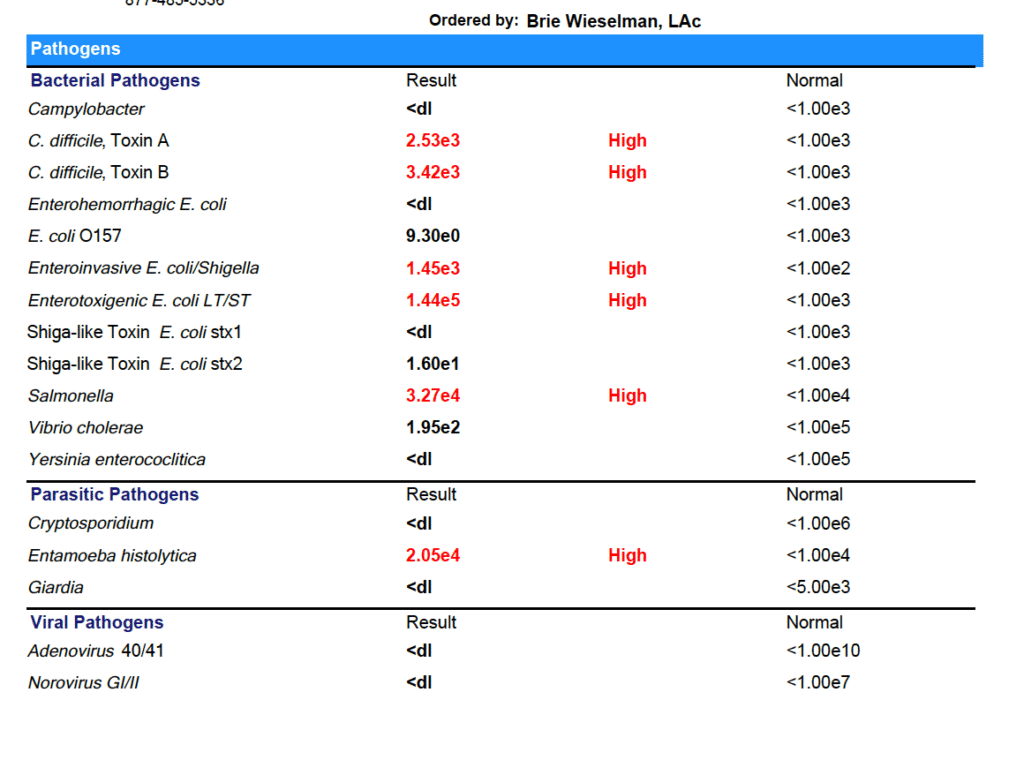
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
Step 3: The Second Test Results:
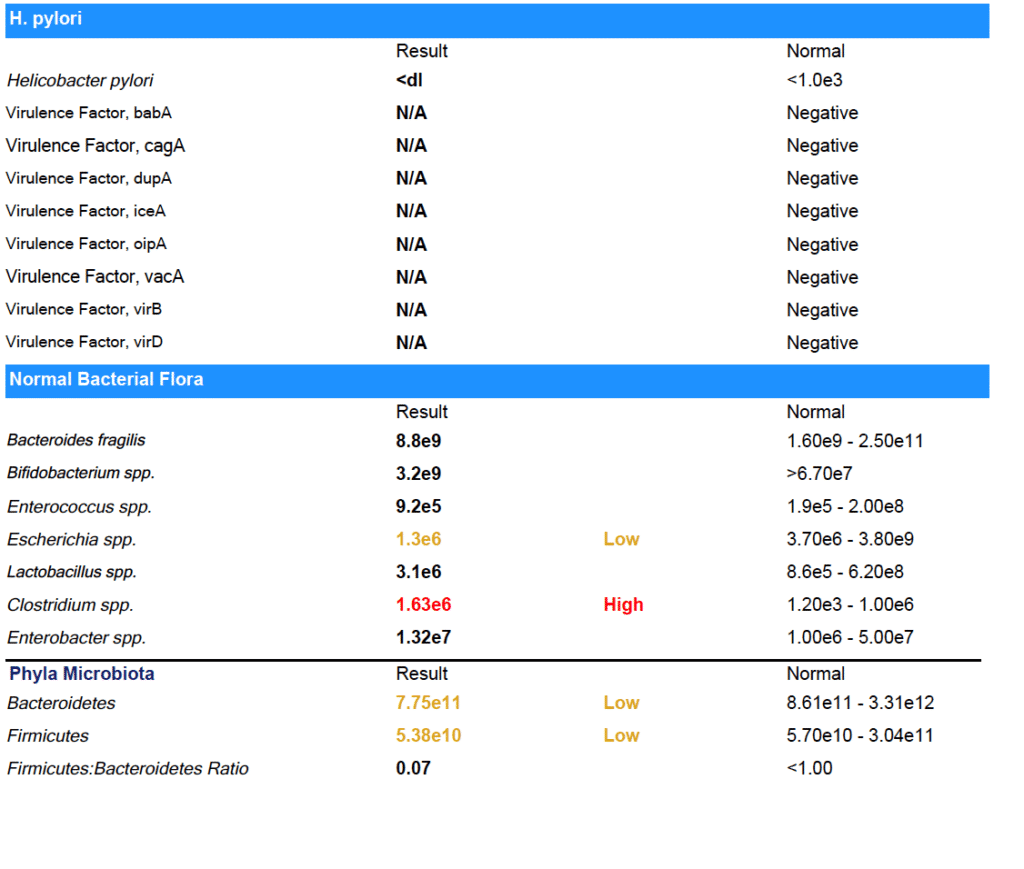
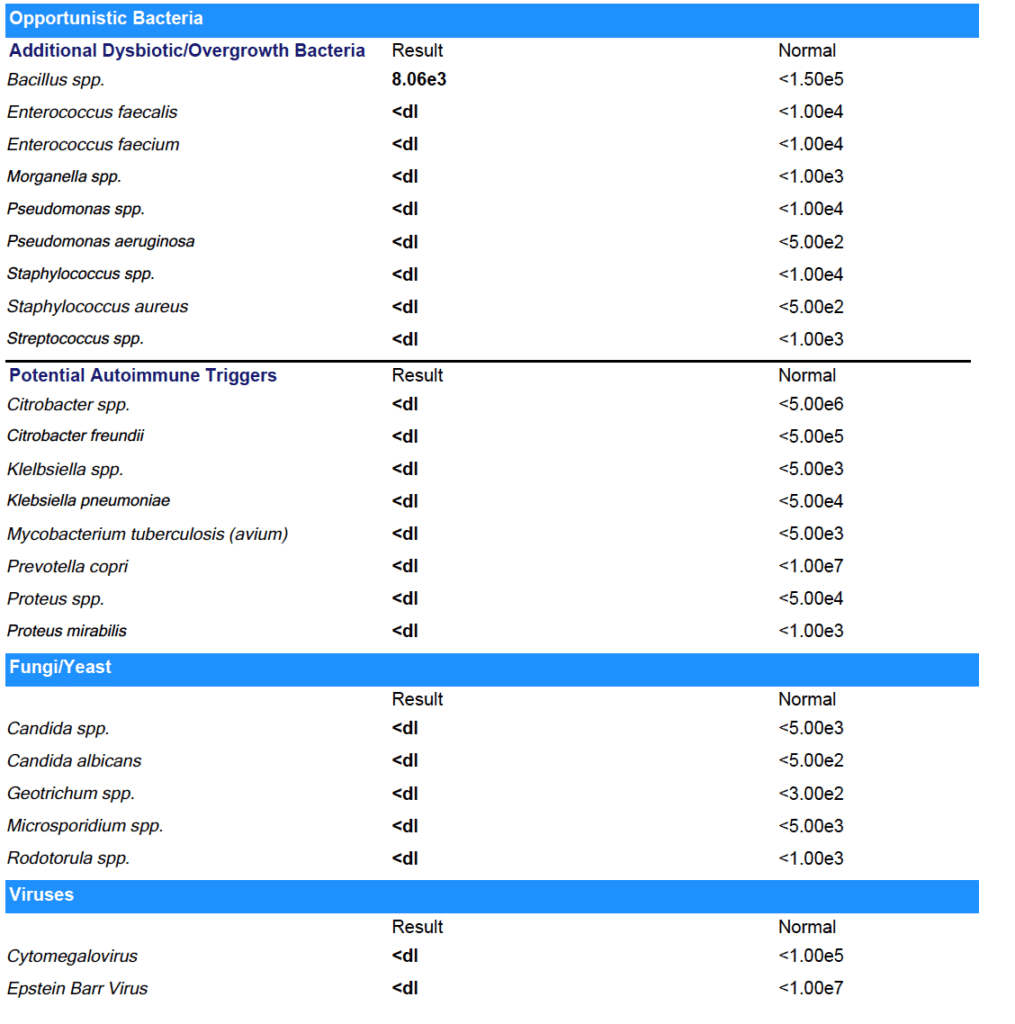
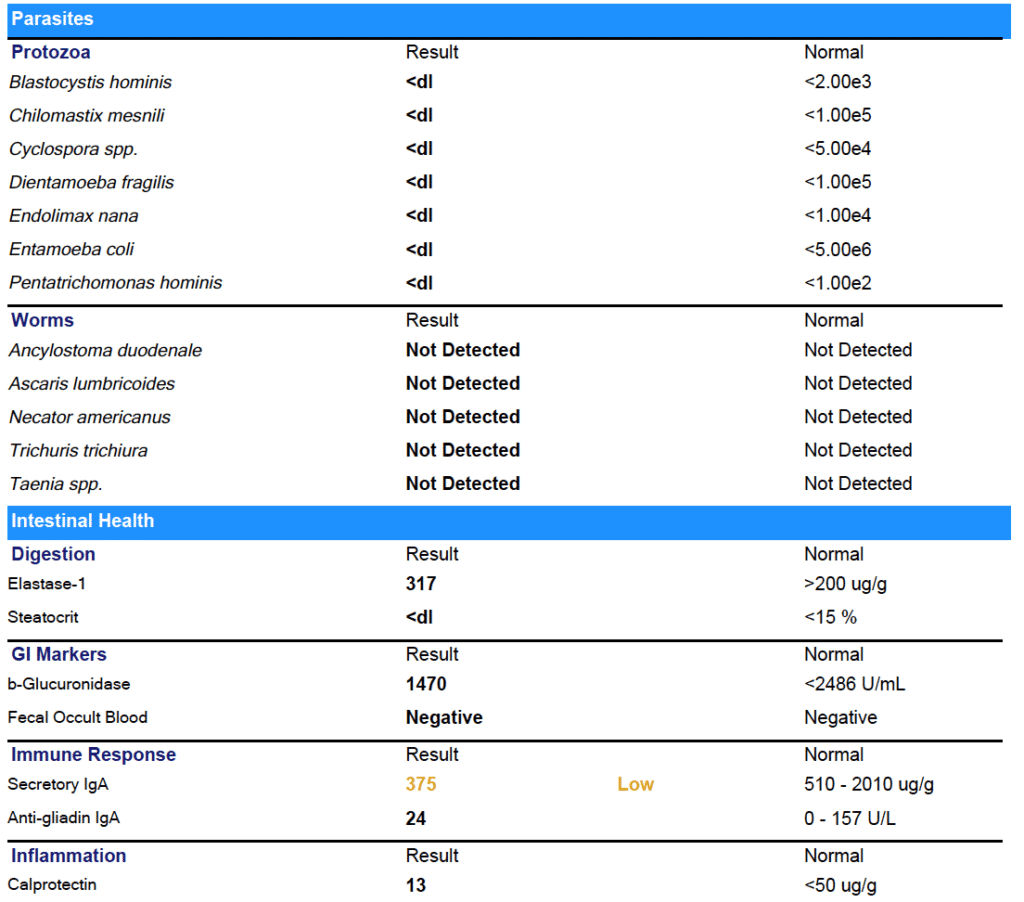
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
The Truth About Hormones & Your Sex Drive
Which of these best describes your sex drive?
“Want it, need it, gotta have it!”
“Could take it or leave it...” or
“Don’t even think about it!”
Whatever you answer, there’s no shame.
Women are pretty reluctant to say our libido (or lack thereof) is one of our top health concerns. But when I dig deep with the women I work one-on-one with in my clinic, I find that almost all of them are struggling with their sex drive.
And personally, when I was struggling with hormone imbalance, my sex drive was non-existent. I thought it was just “normal.” After all, as women we are conditioned to believe we should want sex less than men.
Truth: healthy women have robust sex drives!
Our libido isn’t just dictated by whether our partner brings home flowers or we’ve shaved our legs - it is controlled by a complex group of hormones and neurotransmitters. Too much or too little of one or another can cause our sex drive to dwindle away or get out of hand.
That means that if your libido is lacking, you don’t just need to try lighting candles or new lingerie (although if your sex drive is healthy, that would sound fun instead of like a chore!). Balancing your hormones can restore a healthy libido.
Today, I want to explain how your hormones impact your sex drive. I hope this information empowers you - and if you have more questions or need more support, please reach out to me!
What This Article Can’t Do
Before I dig in to all the juicy hormone info, there are a couple other things I want to get out in the open.
First, most of the research on hormones has been done based on cisgender, heterosexual people and in heterosexual relationships. More research on hormones in other populations is long overdue. If you’re outside this group, some of this information will apply to you and some of it won’t - but I’d love to support you in overcoming hormone issues one-on-one until more inclusive research is available.
Secondly - as you're reading this I know symptoms of too much or too little of various hormones are going to jump out at you. But know this: the only way to diagnose hormone imbalances is with proper testing! That means blood, saliva, and/or urine testing.
Treatment for hormone imbalance is highly individualized, and I always recommend anyone who suspects hormone imbalance work one-on-one with a trained practitioner like myself for accurate testing and treatment! At the end of the article, I’ll share about my favorite hormone tests.
OK - disclaimers done - let’s get to the good stuff!
Estrogen - “The Feminine Hormone”
Estrogen is the hormone we associate with women. It makes women softer - both emotionally and physically. Estrogen is responsible for women’s curves: breasts, hips, and more fat on the butt! In studies of heterosexual men, women with higher estrogen levels were rated as more attractive.
It also increases a woman’s receptive sex drive—the part that makes her interested and open to penetration. Estrogen says “Take me now!” Women with higher estrogen levels may have more of a seductive sex drive - they are more likely to be receptive to sex, more likely to flirt and give “I’m available” signals, than they are likely to initiate it.
Testosterone - “The Masculine Hormone”
What hormone causes horniness? Testosterone is the hormone associated with men - but healthy women have testosterone, too. It helps us build muscle and causes us to feel more competitive and aggressive. In the bedroom, testosterone makes us want to initiate sex and governs the drive for genital sex and orgasms. Women with higher testosterone levels tend to have more of an aggressive sex drive and are more likely to initiate sex than wait for a partner to start things up. Interestingly, some post menopausal women have relatively higher testosterone levels (as compared to other hormones like estrogen) and may notice more of an interest in initiating at this phase in their lives.
Testosterone makes us less interested in relationships and commitment and more likely to want time alone (that’s what the Man Cave is for!). Women with higher testosterone levels tend to masturbate more, too. Too much testosterone can make us feel irritable - but too little can make us feel depressed.
Dopamine - “The Pleasure Chemical”
Dopamine isn’t exactly a hormone - it’s actually a neurotransmitter. Dopamine helps us anticipate pleasure - therefore having the drive and motivation to take action. It’s dopamine that makes us anticipate that sex = pleasure.
People who are low in dopamine tend to seem “flat” - they lack interest, enthusiasm, and get-up-and-go.
Testosterone increases the activity of dopamine in our brains, so supplementing with testosterone is often prescribed for women with low libido. But in my experience, this rarely works - or at least not without other support - probably because the issue isn’t just low testosterone, but also low dopamine. (Just another reason why you have to test!)
DHEA - “The Master Hormone”
DHEA is our most abundant circulating hormone. It’s produced both in the Adrenal glands and in the brain, and most of our other hormones are derived from it. DHEA levels peak in our 20s and start to decline from there - faster for some than others based on factors like your genetics and stress. Oral contraceptives are also know to lower DHEA levels.
Ideally, I like to see DHEA levels on the higher end of the normal range because DHEA can:
- Lower risk of depression
- Provide better function in old age
- Protect against immune suppression when cortisol levels are high (from stress)
- Prevent osteoporosis
- Maintain muscle mass
And of course, DHEA plays a major role in sex drive, orgasms, and sex appeal. Higher levels of DHEA in women correlated with higher rates of sexual desirability in studies. Most of our pheromones are derived from DHEA - scents that in the animal world dictate attraction and mating. Pheromones are often what make us feel an “instant connection” or drawn to someone. When a woman complains of low libido, I always test her DHEA levels first!
In times of stress, DHEA levels decrease significantly -and this can cause a cascade of low hormones throughout your body, since most other hormones are derived from DHEA.
Oxytocin - “The Love Molecule”
Oxytocin is a molecule that is triggered by physical touch. Oxytocin levels increase if you hug, hold hands, have sex, hold a baby - and even if you look at a dog! Levels of oxytocin also spike when you’re aroused and when you orgasm - it’s also what causes the uterus to contract during orgasm. If you’re in love, just thinking about the person can make your oxytocin levels go up.
Oxytocin helps you bond and feel love. It’s especially important for maternal bonding, and oxytocin levels rise during breastfeeding. Higher levels of oxytocin both reduce stress and rational thought - making it easier to “fall in love.”
Progesterone - “The Cock Blocker”
Does progesterone increase libido? In my practice I call progesterone the cock-blocking, (or clam-jamming) hormone. Basically, progesterone stops your sex drive. The effect of progesterone on your sex drive is so powerful, monks used to take the herb Vitex (aka Chaste Tree Berry!) to promote progesterone production and block their sex drive. Progesterone actually numbs the erogenous zones, meaning you’re likely to have dull orgasm with more stimulation - or no orgasm at all.
Many women have high levels of progesterone because they take hormonal contraceptives. The birth control pill contains a synthetic form of progesterone called progestin. Great birth control, right? Just kill your sex drive completely!
Progesterone isn’t all bad though - it promotes maternal behavior and has a mild sedative effect. It can make you feel calm, happy, and that everything is a-okay.
Does ovulation make you horny? In the second half of the menstrual cycle (after ovulation), progesterone is naturally higher. That makes sense biologically - once you’ve ovulated, your body won’t drive you to sex for reproductive reasons. When natural progesterone is balanced with estrogen, the dip in sex drive isn’t as strong and some women don’t notice it at all. Others might just be more interested in cuddling rather than going for an orgasm.
Prolactin - “The Nursing Hormone”
Prolactin is mostly associated with lactating women - it is the hormone that triggers your milk to let down after birth. Prolactin also tends to lower your sex drive - that’s why, in general, women have less sex when they are breastfeeding. Depending on your estrogen levels, you might retain some “receptive” sex drive even when prolactin is higher.
Promoting dopamine opposes prolactin. So if your prolactin levels are high and you’re NOT breastfeeding, using dopamine-promoting herbs can help lower prolactin and improve your sex drive. The only way to accurately gauge your prolactin levels is with testing!
Serotonin - “The Happy Chemical”
Serotonin is dopamine’s partner - together they are the two main neurotransmitters in the brain. Serotonin can impact your sex drive whether it’s too high or too low. Certain medications (like SSRIs) can cause high levels of serotonin. Dieting and chronically low calories can cause low serotonin, too.
Very high levels of serotonin dull your sex drive. That's why SSRI antidepressants have lowered sex drive and delayed/weaker orgasms as a side effect.
Conversely, low levels of serotonin can magnify your sex drive. In people with depression, low serotonin levels can even lead to sex addiction. In women with low serotonin, orgasms happen faster and easier. Men with low serotonin ejaculate right away.
Your Menstrual Cycle - “The Conductor”
Your menstrual cycle is like the conductor of all these hormones and chemicals. As the cycle progresses, hormone levels naturally rise and fall, leading to a shift in your sex drive.
At the beginning of your cycle, all hormone levels are low. Mid-cycle, estrogen and testosterone both spike - leading to an increase in sex drive (you’ll be both more aggressive and receptive to sex).
Many women also notice their libido peaks right before they start their period, as progesterone is naturally falling relative to testosterone. Your genitals will be more sensitive and it’s easier to orgasm during progesterone withdrawal.
During menses, some women have an increased sex drive - again because progesterone is lower relative to testosterone. But because serotonin levels can also drop during this time you might be grouchy too. Grumpy and horny!
The natural shift in hormones throughout the month can explain why sometimes you want sex more for the cuddling, emotional bonding, and skin-to-skin contact, - and why other times you just want an orgasm without all the bells and whistles.
Your Hormones & Your Libido
Our sex drive is completely dependent on our hormones. And as you’ve learned in this article, it’s not as simple as “more testosterone makes you horny!” Balanced hormones are the key to a healthy sex drive.
If your sex drive isn’t how you’d like it to be - either too much or too little - looking at your hormone balance is a great place to start. I know you’re sick of hearing me say this by now, but the ONLY way to accurately diagnose hormone imbalance is with advanced testing. You never want to “guess and check” by starting treatments or supplements for what you “think” is the problem. This can cause even greater imbalances that take more time and work to resolve.
Over the years I’ve used blood and saliva hormone tests - but now I almost exclusively use the DUTCH hormone test. This test is a kit your practitioner orders and you complete at home. It uses dried urine (that’s what the D and U stand for in DUTCH) to accurately test various hormone levels. It’s more accurate than saliva testing, and much simpler than blood testing. You just pee on a stick, let it dry, and mail it back to the lab.
Once I know a patient’s hormone levels, we can work together to come up with a plan to balance them. I never share exact protocols publicly because I’ve never had 2 patients who needed the exact same treatment! Hormones really are that unique.
If this article has resonated with you and you think hormone imbalances could be at the root of your sex drive struggles, I hope you’ll book a free 20-minute exploration call with my team. There’s zero obligation, but we’ll dive deep into your issues and then share what we can do to help.
Having come out the other side of hormone imbalance, I can tell you - having my sex drive back is great! (And my husband loves it too.) I want the health and radiance that comes from balanced hormones for all women. Book a 20-minute call for free here!
My Top Travel Tips for A Healthy Gut
Traveling is one of my biggest passions. When I got married, we chose to do a destination ceremony and reception with all of our friends and family in Sayulita, Mexico, instead of a traditional wedding (no regrets there!).
Traveling hasn’t always been fun for me, though. When I was younger, I felt like EVERY time I traveled, I got sick. And I’m not talking about a cold, folks - I’m talking about the nemesis of every globetrotter: traveler’s diarrhea.
Traveler’s diarrhea, Montezuma’s revenge, Delhi/Bali belly - it’s all caused by food poisoning. And while it will definitely ruin your trip, it also has a more sinister side - food poisoning can cause lasting damage to your digestive system leading to a lifetime of #gutproblems.
Want to know how food poisoning can cause long-term digestive issues - and what I do to avoid traveler’s diarrhea (even in the most exotic locales!)? Keep reading!
(Not interested in the science? Skip here for my travel tips).
How Food Poisoning Can Wreck Your Gut Long Term
I can’t tell you how many patient in my clinic can trace their digestive symptoms back to a case of food poisoning. And the science backs them up! Food poisoning is a known cause of irritable Bowel Syndrome (IBS). IBS after food poisoning is called “post-infectious IBS.”
But this gets a little complex, so bear with me here...
IBS isn’t a disease - it’s a syndrome. That means it’s just a name for a group of symptoms (fun stuff like gas, bloating, diarrhea, constipation, and food intolerances). IBS is a diagnosis of exclusion, meaning your doctor will call your symptoms IBS when they can’t find any other cause for them.
For many people - perhaps as much as 60% - the actual cause of IBS symptoms is something called Small Intestine Bacterial Overgrowth (SIBO). SIBO occurs when bacteria that should be confined to the large intestine migrates up and into the small intestine. A healthy small intestine should have very little bacteria in it!
So how does bacteria get from the large intestine to the small to cause SIBO?
It’s usually do to a problem with the Migrating Motor Complex (MMC). The MMC is what creates movement in your intestines - called peristalsis - and moves food from your stomach down through your intestines and eventually out of your body.
So what can harm your MMC? The most common causes are chronic viruses like Lyme disease, structural abnormalities, high stress levels, and… food poisoning!
Stay with me here - food poisoning can cause your Migrating Motor Complex to malfunction. When the MMC malfunctions, bacteria can move from the large to small intestine and overgrow, causing SIBO - and SIBO is the cause for as much as 60% of IBS!
As you can see, it’s a complex chain of events - and that’s why for years doctors have missed the connection between IBS, SIBO, and food poisoning. Luckily they are catching up now.
Toxins & Autoimmune Responses
So how exactly does the food poisoning cause damage to the Migrating Motor Complex?
Common food poisoning bacterias like E. coli, salmonella, Campylobacter jejuni, and Shigella all produce a toxin called cytolethal distending toxin B. It sounds bad, doesn’t it?
Your body will start producing antibodies against the cytolethal distending toxin B. For some people, they’re able to fight it off over in a few days and move on without long-term problems, but for about 10% of us (raising my hand!) we can’t fight it off as quickly - and therefore we keep producing more and more antibodies.
These antibodies don’t just fight the cytolethal distending toxin B - they also reduce a kind of protein in our intestine called vinculin.
Vinculin is very important in the health of Migrating Motor Complex - vinculin is crucial for proper function of nerve cells in the gut that cause peristalsis. When the MMC isn’t functioning and movement of food through the gut is slowed down, bacteria can overgrow and cause SIBO - plus other symptoms like bloating and gas.
The good news is that your gut can recover vinculin over time. First, you need to heal the SIBO. But it’s also critically important that you don’t get food poisoning again. So if you already have some gut issues, don’t stop reading now!
Here’s What I Do To Avoid Traveler’s Diarrhea
The key to avoiding traveler’s diarrhea is being proactive - think about where you’re going, research, and prepare! There are supplements I take to prevent illness, supplements I bring with me for defense in case I start feeling sick, and hygiene practices I follow, too.
Supplements I Use When Traveling To Keep My Gut Happy
When I’m travelling, I always take a probiotic. My favorites are Floramyces (which contains the yeast Saccharomyces boulardii) or UltraFlora Acute Care (this one blends S. boulardii with Bifidobacterium and Lactobacillus). I take 1 capsule of either, 1-2 times daily.
I also take Biocidin Advanced Formula Liquid to help boost my immunity. I start with 3 drops per day and work up to 5-10 drops twice daily.
Finally, I always take an Adaptogen blend. Adaptogens are herbs that help mitigate the stress of traveling. Yes, traveling is fun - but it is also hard on our bodies! Moving through time zones, awkward sleep schedules, and even just enjoying all the “newness” are all registered as stress to our bodies. I like blends that contain herbs like rhodiola for emotional and mental stress and eleuthero for physical stamina. NanoMojo Liquid and HPA Axis Homeostasis are my two go-tos.
Don’t Eat That!
Hygiene practices are so important for avoiding traveler’s diarrhea.
I always carry hand sanitizer with me - but not the conventional kind! Commercial hand sanitizers are full of BPA and other chemicals. Instead I make my own from aloe vera gel with lavender and tea tree essential oils, plus some Silvercillin. If you don’t want to make your own, this is good alternative. And of course - wash your hands with hot soap and water whenever you can.
Only drink bottled water - and never get ice! (Yes, even on the plane and in fancy restaurants!)
Avoid salad and uncooked veggies - especially lettuce. Cooked veggies (and cooked, hot food in general) are better when traveling. Worried about missing your greens? I bring a greens powder with me and mix it with bottled water. This one is my favorite.
Make sure you wash any produce you buy. As tempting as it is, don’t eat fruit straight from the farmer’s market cart. Wash it with a non-toxic fruit and veggie disinfectant first!
When eating out, look for food carts and restaurants with long line and plenty of locals.
Do This If You Feel Something Coming On
The minute I start to feel “off” - fatigued, grumbling stomach, or even a headache - I switch from my prevention to my treatment protocol.
I up the Biocidin Liquid to 10 drops, 3x per day.
I double up the probiotic.
I add in Oregano Oil Gelcaps for several days - 2 caps 3x daily.
And if diarrhea strikes? I go to a classic Chinese remedy called Huang Lian Su. It’s a blend of berberine-containing herbs that always works for me. I use 4-5 tablets, 3-4 times daily.
Happy Trails To You!
I hope these suggestions helps ease your fears about traveler’s diarrhea - and allow you to travel the world without getting sick!
And if you think food poisoning is at the root of your SIBO or gut problems, I hope you’ll consider working one-on-one with me to get it resolved. There is hope for overcoming gut problems - even one you’ve had for years! You can book a free consult with my team anytime. We’d love to help you!
The Truth About Fertility Apps (And the Exact Ones I Use and Recommend)
In college, I tracked my periods on my wall calendar. A red dot (so subtle!) marked day 1 of my period. It wasn’t very advanced, but it was when I first started paying attention to my not-so-monthly cycle. Back then I also read paperbacks and kept a grocery list on a magnetic notepad on my fridge.
I don’t do any of those things anymore though because - hey, there’s an app for that!
If you’re like me, you keep everything on your phone now, and there are even some amazing fertility tracking apps you can get, too. These apps don’t just help you remember when you last got your period - the best ones can accurately predict when you'll ovulate each month. You can use that information to help you get (or not get) pregnant.
But not every fertility tracking app you can download is actually useful. Some really can help you predict when you’re ovulating, but others are no more sophisticated than my old red-dot method.
Let me explain how and what fertility trackers can and can’t do - and I’ll tell you which ones I use and recommend (even if you have PCOS or irregular periods!).
Why Should I Track My Cycle?
I recommend cycle tracking for all women. Your period is one of the biggest indicators of your overall health - but it’s also really sensitive to changes. Little changes in your cycle can be a clue of a bigger problem, even before any other symptoms show up.
Plus, being aware of your cycle gives you powerful information about your body. As you get more in tune with your cycle, you may even start basing some other patterns around it (like how you eat or your exercise throughout the month).
And of course, the obvious reason to track your cycle is to track your fertility (by knowing when you ovulate). This is not just for women who are trying to get pregnant - you can use this information to help you get pregnant more easily OR to avoid pregnancy without having to use hormonal birth control methods.
Yes - the right fertility tracking app can replace hormonal birth control if it is used correctly!
But if you’re going to rely on cycle tracking to predict your fertility, it’s critical that you use a reliable app - and they aren’t all created equal.
Calendar-Only Apps Can’t Tell You Enough
Unless you are simply trying to get a better sense of cycle length and variations, regular calendar based apps are useless for fertility detection. These are apps like “Period Tracker” that just ask you to track when your period begins and ends.
These apps base their estimation of your fertility on data from your prior cycles, assuming you have a 28-day cycle and Cycle-Day 14 ovulation. But the truth is that fewer than 10% of women actually do. Your cycle length can also vary from month to month. Because most women don’t have this cycle pattern, these apps cannot accurately tell you when you can and can’t conceive.
Which App Should I Use?
If you really want accurate results (and when it comes to getting pregnant or not, accuracy is key) you need a fertility tracker that does more than just count days.
After testing and trying them all, both myself and with my patients, there are three I recommend - one for people whose goal is avoiding pregnancy, and another two for those who are looking to conceive OR who have very irregular cycles (my PCOS sisters, this one is for you!)
Let me break them all down for you.
If You’re Trying To Avoid Pregnancy (And Or Get Pregnant & Have Regular Cycles)
If you want to track your cycle, get a better understanding of your fertile window and monthly rhythms, and/or avoid pregnancy, I think the Kindara Fertility Tracker is the simplest to use and has a great track record.
Kindara is an app that you use along with a basal thermometer (which gives temperature to the second decimal).All you need to do is remember to take your temperature using the thermometer every morning, right when you wake up, and enter that data into the app. You’ll also track changes in your cervical mucus.
Research by the CDC has shown that, when used perfectly, this method of birth control is 99.6% effective!
Kindara reports days to you as either fertile or not fertile, based on your temperature, past cycles, and cervical mucus. If you’re avoiding pregnancy, abstain or use a non-hormonal birth control method when you’re fertile.
At only $4.99/month (and with a free basic version, as well), the Kindara app is a great alternative to hormonal birth control and is a useful tool for tracking your fertility.
If You’re Trying to Get Pregnant - Or You Have Long or Irregular Cycles
If your goal is to get pregnant, or if you have PCOS or irregular cycles (whether you want to get pregnant or avoid pregnancy) I recommend both Oova and the new Priya.
Priya is a vaginal sensor that monitors temperature all day long. It’s a silicone ring that you can wear continuously for up to 29 days - or remove for up to three hours daily - that takes regular temperature readings.
Because it measures core temperature, and because it takes readings all day long, every 6 minutes, the resulting temperature data is much more accurate than taking a single, oral reading.
Priya is able to predict ovulation up to 2.5 days in advance of a LH surge on an ovulation urine test and data in trials suggests it is just as accurate as an ultrasound, which is the gold standard for ovulation testing!
If you have PCOS, or unexplained fertility, using Priya can unlock a huge piece of the puzzle. The same holds true if you have irregular cycles or irregular ovulation from any cause, and are either trying to conceive, or trying to avoid it. It also works if a woman is taking fertility treatments in the form of herbs or medications to promote ovulation.
And if you’re wondering if it’s safe to wear, I have you covered! My first question was about the potential for EMF exposure. What makes Priya cool is that it only connects to the device once an hour for a few minutes, and it’s at a very low power. You can also change the setting and have it connect even less often, 1-2x daily is all that’s needed, and you can remove it before connecting. It will still read and store your temperature, even when disconnected.
I also asked about the potential for biofilm buildup and vaginal microbiome disruption (which is a major issue with other vaginal rings, like Nuvaring). Priya is different because it's made from washable silicone. You can take it out every day and wash it, and it can be removed up to 3 hours per day and still be effective.
Priya is not yet available to the public, but I am testing it with my clients and loving the results. Sign up for pre-orders here.
Another Amazing Option - Especially for PCOS!
Along with Priya, I recommend Oova, which uses urine tests (think pee-on-a-stick pregnancy tests) to track fertility throughout the month instead of temperature. You order a kit with 15 tests, and enter test results into the app for lab-quality results.
Honestly, I love Oova. The technology was developed by a doctor who struggled with fertility herself, and it’s unlike anything else you can buy.
You’ve probably heard of LH tests (AKA Ovulation Predictor Kits) before: you can buy them at the drugstore, and until now they were the best option for at-home ovulation prediction. But the big problem is that LH - luteinizing hormone - is present in your urine all month, and it surges just before ovulation. All an LH test can tell you is that ovulation is coming in the 24 hours or so - and that depends on you taking it at the right time (too early or too late and you’ll miss the tell-tale surge). Plus, interpretation can be confusing: is today the strongest pink line? Was it yesterday? Will it be tomorrow?
If you’re trying to get pregnant, LH tests alone aren’t very helpful because your fertile window is actually 5 days up until you ovulate, and an LH test misses most of that. And, an LH surge doesn’t always mean that an egg has actually been released, as some women don’t release an egg every cycle.
Oova uses super-sensitive, nanotechnology LH tests along with progesterone tests to solve this problem. Progesterone levels rise when an egg is released from the follicle in the ovary where it has been growing. High progesterone levels are also necessary for the vascular development of endometrial lining, and to prevent shedding of the endometrial lining if you are pregnant. By tracking progesterone levels with LH, Oova gets a complete look at your cycle.
You’ll use the Oova tests - which are read by the app, so you don’t have to do any interpretation - to establish your hormonal baseline and then see the changes that indicate your fertile window. It can uncover your exact, unique cycle length, and confirm that ovulation has in fact occurred - so it’s ideal for women with irregular cycles or PCOS!
I love to pair Oova with Priya or Kindara data, too - especially for tricky, irregular cycles who are trying to conceive!
Learn more and get Oova here. Use code BWIH1 for 15% off your Oova order!
Can A Fertility Tracker Really Replace Other Forms of Birth Control?
Like I said before, I recommend tracking your cycle to all women - even if it’s just a simple calendar app for right now.
But the right fertility tracking app CAN replace other forms of birth control as long as you’re doing it the right way. Just like with the pill or condoms, user error is the biggest problem with using fertility tracking as a birth control method.
Before you get started, read all the instructions included with your fertility tracking app - and when in doubt, use a backup method like a condom. My favorite condoms are Sustain Natural Latex Condoms, which are nitrosomine-free (nitrosomine is is a carcinogen that is formed when latex is heated and formed). The rubber they use for manufacturing their latex is also non-GMO and fair trade, which is really significant with condoms, as child labor and harsh working conditions are a big issue in many rubber plantations world-wide.
Do You Track Your Fertility?
If you have experience with the Kindara, Priya, or Oova, I’d love to hear how it worked for you! Got another fertility tracking app you love? Leave a comment and let me know.
And if you’re not yet tracking your fertility but want to give it a try using one of the apps I recommend, save 15% on the Oova kit with code BWIH1!
Natural Cold & Flu Remedies
Natural Cold & Flu Remedies (from Chinese Medicine)
It starts in the last weeks of summer with the “back-to-school” cold. By the time fall is slowly starting to turn to winter, it can feel like cold and flu infections are lurking on every door knob and elevator button.
And the truth is, they are! School age kids get 6-8 colds on average per year, and adults get 2-4. Women get more colds than men - probably because they often have more contact with kids. That averages roughly 5.5 missed work days per person, and 150 million workdays missed nationwide, just due to the common cold virus.
But, you don’t have to get sick that often (or stay sick so long)! You can get through the fall and winter without sniffles, runny noses, hacking coughs, and more phlegm than you thought existed in the universe - and you can do it without prescription drugs or over-the-counter cough syrups.
Can You Treat a Cold or Flu Naturally?
Absolutely. If you catch it early enough, nutrients and herbs can cut a virus off before it takes hold. And if you don’t catch it in time to prevent it from taking root, holistic treatment works powerfully to decrease symptoms, shorten the duration, and prevent secondary infections (like bronchitis or pneumonia) from developing later.
And remember: antibiotics do not work for viral infections, so they have no use in treating the common cold. The only time you should use antibiotics is if a bacterial infection sets in on top of a cold or flu.
Herbs, on the other hand, can help treat both bacteria and viruses. One plant can contain thousands of phytochemicals - compounds that are antiviral, help to boost white blood cell sounds, and antibacterial can all be in the same herb! Carefully combining herbs, as has been done for thousands of years, can make them even more powerful!
Why I Use Chinese Medicine to Treat Colds & Flus
When patients (or myself!) come down with the common cold, I always go back to my roots in Chinese Herbal Medicine. Herbs have been used by Chinese Medicine practitioners for thousands of years to treat and prevent colds and flus.
In Chinese Medicine, the common cold is divided into six distinct stages that each have unique herbal treatments. Formulas to treat symptoms of each stage are carefully created with different herbs. Chinese medicine herbalists consider not just what stage of a cold you’re in, but also the properties of the herbs, temperatures, and how a person will interact with the herbs based on their own constitution.
These formulas can give you both quick, short-term relief (by treating your symptoms) as well as help you get better faster (by boosting your immune system).
To really customize an herbal formula to what stage of a cold you are at and your constitution, I would recommend an in-person consult. But even if you can’t see a Chinese Medicine practitioner like me in person, there are some general nutrient and herbal formulas that are balanced enough to be safe and effective in all generally healthy adults who are trying to fend off impending coughing and sneezing.
Prevention First
Hands down, the best way to fight a cold or flu is to not get sick in the first place!
It goes without saying that practising good hygiene is the first step - wash your hands with hot water and soap and cover your nose and mouth when you cough or sneeze. Eating a nutrient-dense diet, getting plenty of sleep, and regular exercise can also help keep your immune system strong so that you effortlessly fight off anything that comes your way.
But Chinese herbs can be a secret weapon in preventing colds, too. Herbs can help strengthen our immune systems and fight off colds before they take root.
My favourite formula for taking throughout cold and flu season to strengthen the immune system is Yu Ping Fen Wan. This traditional Chinese formula contains lots of Astragalus, an herb which helps to increase circulating white blood cell counts and increases cytokines in our immune system that help ward off viral infections. The brand I use calls this formula Astra C, and the dose for adults is 2 tabs 2-3 times daily through cold and flu season.
What If I’m Already Sick?
With any Chinese Medicine formula, the quicker you start to take it, the better results you can expect. Personally, I will sometimes take a few doses of the herbal formulas for the first stage of a cold if I have had significant exposure to someone who is currently sick, just to make sure I don’t come down with the same thing!
But even if you don’t catch it before symptoms set in, the sooner you start treatment, the faster you’ll feel better.
But I know what you’re thinking - the last thing you want to do when you already feel bad from a cold (and maybe have a husband with the man-flu and kids who need your attention, too) is try and decipher labels at a Chinese herb shop!
That’s why I recommend keeping some herbal formulas on hand during the winter months. These are tablets that you can keep in the cupboard, just like you would a bottle of cold syrup. That way, when a cold or flu strikes, you’re already prepared.
I have my exact cold and flu protocols
(yes, even the exact brands of herbs I use!) - the same ones I use for myself and my clients - all in one PDF. You can download a copy for free here
.
When To Get More Help
The common cold, and a low grade version of the annual flu virus, as common as they are, can still make you feel really bad.
Both colds and the flu can usually be treated at home, without needing to see a doctor.
The most common cold symptoms are:
- runny nose and sneezing
- sore throat
- sinus congestion
- mild headaches
- body aches
- chills
- low-grade fever
- generally feeling unwell
A cold should run its course within 7-10 days, in most adults. Herbal treatments (like the ones in my protocol) can help with these symptoms.
But if your symptoms progress to any of these, you should seek medical attention:
- If your fever rises above 101.3 or lasts for more than 5 days
- If your headache, ear, throat, or sinus pain becomes severe
- If you notice wheezing, or have asthma symptoms
- If you get a deep barking cough or bronchitis, especially if you start to feel worse several days into the virus, rather than better.
The influenza virus (aka the flu), has many of the same symptoms as a common cold virus, but it is more likely to include fever (which is frequently over 100 degrees), and tends to have a more abrupt onset. Body-aches are usually more pronounced, and it is not uncommon to also have digestive symptoms like vomiting or diarrhoea.
The flu takes up to 2 weeks to recover from. The warning signs for seeking medical attention are the same as with the common cold, but according the the Mayo clinic, additionally include:
- Difficulty breathing or shortness of breath
- Pain or pressure in the chest or abdomen
- Sudden dizziness
- Confusion
- Severe or persistent vomiting
- Flu-like symptoms that improve but then return with fever and worse cough
Feel Better Soon!
Hopefully you’re reading this article before you get hit with a nasty cold or flu - but if not, I hope you feel better soon! Grab a bowl of bone broth, bundle up, and try some of my cold and flu protocols here.
4 Crucial Steps for Mealtime that can make-or-break your digestion
When it comes to healing digestive issues, it’s certainly true that we need to test to identify and then treat any infections or dysbiosis that may be contributing.
But just as importantly, we need to optimize the environment of the gut. In order to develop infections or overgrowths, the environment has to be right. Otherwise, our healthy gut terrain is inhospitable to the “bad guys”, and nurturing to the “good guys”.
This mainly involves things like optimal digestive secretions (like stomach acid and pancreatic digestive enzymes) that set the pH and fully digest our food. This ensures that we both assimilate the nutrients contained in what we eat, but also prevents other organisms, like bacteria and yeast, from eating it instead.
Other secretions, like bile from our liver/gall bladder, are also super essential. Bile digests fat, but also is a powerful antimicrobial, and regulates the motility of our intestines.
Of all the digestive secretions, Stomach Acid might be the most important when it comes to resilience against infections. Stomach acid (called Hydrochloric Acid, or HCL) is like your first line of defense.
You may know that stomach acid’s main role is to break down the proteins we eat, so that we can absorb the smaller amino acid building blocks to use as nutrition.
But stomach acid is also antibacterial to undesirable strains because of the low pH environment that it creates.
Keeping food in the stomach long enough is critical for the action of stomach acid to control the populations infused into lower regions with each pulsatile release of chyme. This is because food needs to be exposed to stomach acid (HCL) long enough to kill bad bacteria, preventing them from proceeding on into the small intestine.
So, if you have super-rapid motility (this is common in people who have chronic diarrhea), your food may pass too quickly through the stomach and into the intestines, and not have enough exposure to HCL. This equals increased risk of infections, in addition to not enough nutrient digestion.
Due to…
- Stress
- Nutrient deficiencies
- Modern diet and lifestyle
- And even just natural aging!
it’s unfortunately very common for people to produce less than optimal amounts of stomach acid to meet the demands of food intake.
And…..we need enough HCL present to keep the stomach pH below 4 for the entire time the food we are digesting in the stomach. If this doesn’t happen…pathogenic microbes pass unharmed into the intestines where they can take residence! (hello SIBO and parasites!)
Here’s the most important thing I want you to learn today:
HOW we eat our meals is one of the most important factors in optimizing gut environment.
Just becoming aware of HOW we eat, is one of the biggest things you can do to change what is happening with your digestive secretions, and therefore, with your microbiome.
Chewing: Why is chewing your food so important in regards to this?
Yes, chewing breaks your food down into smaller pieces, increasing the surface area, so that digestive secretions in the stomach and small intestines (like pancreatic enzymes, bile, and stomach acid) can further break them down.
But….there are other not so obvious reasons!
Chewing exposes foods to enzymes in the saliva that break down the cell walls of gram positive bacteria, causing them to die.
This means that chewing adequately is really our first weapon against pathogens that might be entering with our food!
Being relaxed while eating: Stress is a big factor that leaves us more prone to getting opportunistic gut infections, because stress shuts down our digestive secretions.
When our brain thinks we need to run from the proverbial tiger, it focuses our body’s energy and attention on surviving NOW, and diverts it from activities that are about long term survival, like digesting our nutrients.
Stress also spikes our cortisol, and this suppresses our gut’s immune system big-time--for much the same reason. And the hormone that our brain uses to signal the adrenal glands to make more cortisol, CRH, can promote leaky gut.
Healthy Meal Hygiene for Healthy Gut Environment:
1) Focus on creating a state of overall calm before, during and after eating to encourage stomach acid and digestive enzyme secretion.
2) Chew adequately—more than you think….keep chewing!-- to reduce particle size and mix enzymes in the saliva.
3) Include balanced fats, carbohydrates and proteins in each meal to encourage food to stay in the stomach long enough.
4) Planning enough time for meals—not eating on the run—is critical, to help allow for parasympathetic (rest-and-digest) nervous system activity. This allows for proper secretion of digestive fluids. Otherwise, if our body thinks we are running from the hypothetical tiger, there’s no digestion being emphasized, and no secretions being made—“Ain’t nobody got time for that”!
Have any questions or comments on this?
Pop on over to my facebook page and ask me anything!
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
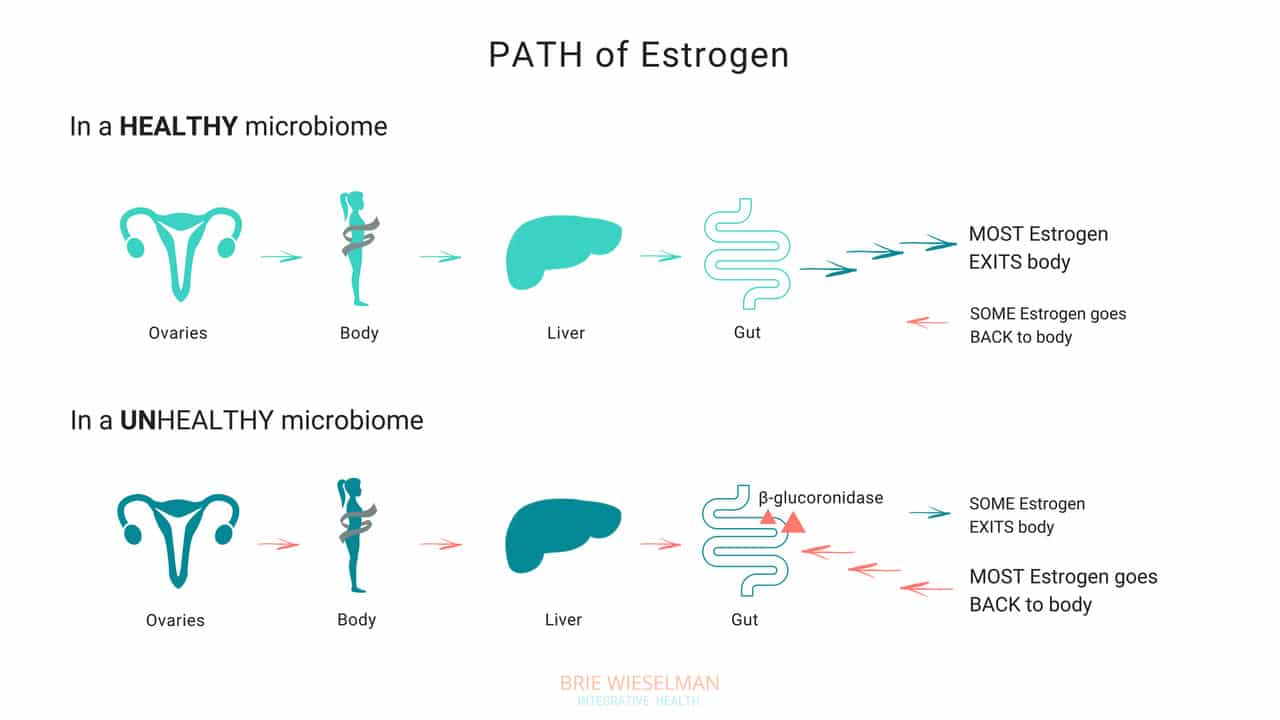
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.
Acid Reflux and Chronic Urinary Tract Infection; Totally 'Unrelated' Symptoms With the Same Root Cause?
One of the principles of Functional Medicine is finding and treating the “root cause.”
But sometimes, it isn’t as simple as finding one root cause and getting rid of it. Most of my clients have multiple health concerns - and multiple causes behind them. Helping them is about peeling back the layers and addressing each one as we go.
For my client Jane, peeling back the layers was exactly what we needed to do! She came in because she was experiencing tightness in her chest caused by acid reflux - and we wound up working through multiple gut infections, addressing vaginal dryness, and putting interstitial cystitis (a condition that causes chronic bladder pain like a urinary tract infection) into remission.
Every time we treated another “layer” Jane felt better than before.
Today, Jane wants to share her story in her own words. If you’re considering pursuing help with a Functional Medicine Practitioner like me, I hope this story helps you better understand the process of working with a practitioner.
Jane’s Story
About three years ago, I started dealing with some bloating. Then, I’d occasionally have constipation - not all the time, but enough that I noticed it. I had a colonoscopy and the results came back normal. I started taking a probiotic. The bloating and constipation just became kind of a general annoyance I was living with.
But then I started feeling tightness and pain in my chest. That was really scary. I went to the doctor right away, but the tightness and pain weren’t heart-related. That’s when I realized they were actually a digestive issue. I decided to go see a physician at my regular clinic, and they told me it was acid reflux, prescribed Prilosec, and referred me to a GI doctor.
Luckily I had read enough about Prilosec to know I didn’t want to take a proton-pump inhibitor. Instead, I decided to get a second opinion from a Functional Medicine Practitioner - that was Brie.
Working With Brie
From the start, Brie was very thorough. She took a really detailed history that helped me connect some dots about what had started all my digestive symptoms in the first place. The past summer, I’d had a urinary tract infection and taken a course of antibiotics. Then in the fall, I went traveled out of the country and had to take a course of the antibiotic Cipro for traveler’s diarrhea. That's when the bloating and constipation became worse and the other acid reflux symptoms started.
But she wasn’t just interested in the acid reflux - Brie asked questions about my overall health. When I told her I was experiencing vaginal dryness, urinary pain, and low libidio, she took me seriously. My doctor had diagnosed my with interstitial cystitis - basically pain in my reproductive organs for no reason.
Brie explained to me how the antibiotics had killed the good bacteria in my gut as well as the bad. She recommended stool testing and a breath test for Small Intestine Bacterial Overgrowth (SIBO), as well as hormone testing. She also recommended I cut out dairy and gluten temporarily to give my system a break, since those foods are common gut irritants. She also recommended some supplement that would soothe my gut and help with symptoms until we got the test results back. All this happened at our very first meeting!
The Test Results Came In
The test results came back a few weeks later - they showed low cortisol, low estrogen, H. pylori, low beneficial flora, and a few overgrown bacteria (citrobacter, pseudomonas). Plus, I had both methane and hydrogen type SIBO and was under-producing pancreatic enzymes.
It was a lot to take in and I was so glad I had Brie to help me understand what the results meant. She saw how everything was connected.
Brie explained that the H. pylori infection was likely causing the acid reflux, and that the SIBO was probably the cause of the constipation and the uti bloating. My hormone problems were tied in to all of it and causing the vaginal dryness, urinary pain, and low sex drive.
It was a relief to know there was a reason I was feeling the way I was feeling - especially because my symptoms had gone into a flare as we waited for the test results. I remember going to visit a friend for a few days and having to come home early because I was just so uncomfortable.
Brie started my on a supplement protocol for 6-8 weeks for both the H. pylori and the SIBO. I kept avoiding gluten & dairy, too.
After I finished the first supplement protocol, we re-tested. The H. pylori was gone! The SIBO levels had come down, but it wasn’t completely gone. On the second stool test, I also had positive results for some other common gut infections and parasites, including candida overgrowth. Brie explained that all of this was normal - the first protocol of supplements had helped destroy the “biofilm” - the protective cover the bad bacteria use to protect themselves and hide. With the biofilm gone now, we could see other parasites and better treat the SIBO, too.
By, then my acid reflux was totally gone and I was feeling pretty good gut-wise. But I was still struggling with the vaginal dryness and hormone symptoms. And, what I initially thought was a bladder infection turned out to be Interstitial Cystitis. The “UTI” pain didn’t respond to normal treatments, and the pain turned chronic. Can a UTI cause bloating and constipation?
Putting Interstitial Cystitis Into Remission
My hormone symptoms were slowly improving as my gut healed - but Brie also suggested using a plant-based bioidentical estrogen replacement. She also had me use vaginal DHEA, a vaginal probiotic, and some herbs. Those helped me feel better right away.
Brie also explained that two of the bad bacteria that the tests had shown were overgrown in my gut - proteus and citrobacter - were related to the Interstitial Cystitis, too. As we treated those, my symptoms disappeared completely.
Brie suggested I work with a pelvic floor therapist, too. That helped me relax some overly tight muscles that were contributing to the pain.
Changing My Diet
Brie suggested I follow a gluten and dairy-free, low-FODMAP diet. It helped me a lot in the beginning, but I was anxious to reintroduce more foods as soon as I could.
After a few months, I was able to reintroduce beans and some other legumes, which I hadn’t been able to tolerate for years, and I really missed. I am now back to eating all fruits and veggies, and I can even add in a little gluten here and there. That makes me feel good!
Where I Am Now
After working with Brie, I feel great for the first time in years.
I came to see her because of the acid reflux - but she opened my eyes to a lot of problems I had been writing off as “normal” or just “part of getting older.”
Gut-wise, I am feeling so much better now! After having given up gluten and dairy for years, I’m finally able to experiment with adding them back into my diet again now.
The interstitial cystitis pain is gone now, too. I didn’t realize how much the pain held me back from enjoying life - I even cancelled an overseas trip because of it!
I’m so happy to be where I am now with my health. I’m following a maintenance protocol now and continuing to meet with Brie occasionally to make sure I’m doing the right things moving forward.
Working with Brie has made a huge difference for me, and I wish more people could have access to it! I hope my story helps to spread the word.
Do You Need Help, Too?
Jane had amazing success - she cleared multiple gut parasites, fixed her digestion, reversed interstitial cystitis, and was even able to reintroduce foods she hadn’t eaten in years.
Why was she so successful? Because she dedicated herself to working through the process of Functional Medicine. She didn’t give up even when it got complicated - and neither did I!
I hope reading Jane’s story has helped you understand better understand the process of working with a Functional Medicine Practitioner like me.
If you’re inspired and ready to start your own journey, you can book a free, no-obligation Prospective Patient Interview with my team. During this 20-minute appointment, we’ll learn about you and discover if you’re a good fit for working with us.
We’re Hiring a Virtual Office Manager!
Hey, guess what!? We’re looking for a Virtual Office Manager to help us manage the every-day details of running our consulting practice. We currently have an absolutely brilliant team member in this role who will be moving onto bigger and better things in the fall.
This is a paid hourly contract position--you work from home and would probably start out as a 12-or-so hour per week role, with room for growth as we grow :-) That said, we are currently growing rapidly, and so the ideal candidate would have room and desire to grow into a 20-30 hour a week position over the next year.
We’re looking for someone who:
- Is highly organized, detail-oriented, and serious about organization and processes (like, you organize-your-closet-by-color-and-alphabetize-your-spices-type-organized). You probably have done event planning or bookkeeping because you’re good at logistics and details, and you like to write lists and work from a checklist at all times.
- Enjoys working alone most of the time. While you will be in communication with Brie and other team members, as well as with clients, regularly, the work you’ll be doing is typically alone. If you’re the type of person who likes to chit-chat with people and interact with friends a lot during your work day, this probably isn’t right for you.
- Has the flexibility to work at least 1-4 hours each day of the week (excluding Saturday and Sunday) - preferably split between the morning and late afternoon/evening. Certain tasks must be done on Friday of each week, requiring several hours.
- Knows their way around a computer, apps, and various cloud-based software. Thinks that “everything is figure-out-able”. Is “tech savvy” with things like Office, Google Docs, Excel sheets, scheduling, email, ordering things online, etc.
- Is extremely dependable... not the “This usually doesn’t happen, but it happened again” type.
- Doesn’t take things personally, have feelings hurt easily or get offended. Stays objective and likes to always use logic to make decisions. This trait is extremely important for the customer service aspect of this role. Many of our clients just don’t feel so good when they initially start working with us….as a result, they can be slightly less than patient, have a lot of questions, get a bit grouchy, or need things explained to them in more than one way. Having extra patience and compassion, and/or having had experience either recovering from health issues, or living with someone who has, is a plus here.
If you’re the type of person who likes “creative” work, where you interact with a lot of people in a lively physical environment and chit-chat at the coffee machine..... and deal with a lot of different types of complex challenges….. then this probably is NOT right for you. This is more of what we would call “organizer” work, and will require you to keep checklists and work through specific processes.
On the other hand... if you’re the type of person who loves organizing things, operating efficiently and using checklists, and basically becoming better and better at running through a pre-planned process, (or, having the vision to make suggestions for improving upon what we already have developed) then this might be perfect for you!
As the Virtual Office Manager, you’ll be ordering tests, ordering supplements, setting up new patient charts, processing orders, filing test results, etc. This role does involve interaction with our clients or customers via email on a daily basis.
No questions please.
To apply, click below and respond to the questions by WED 9/19.
We can’t wait to meet you! :)
How I healed from 6 years of severe insomnia-- and you can too!
It is estimated that up to 50% of adults in the US are affected by insomnia, with up to 60 million having chronic sleep trouble. Twenty percent of Americans report that they did not wake up feeling refreshed on any of the past seven days. These numbers are staggering, when you think about the incredible number of studies proving that adequate, good quality sleep is essential for disease prevention, mood, and brain function.
I went through a time in my 20’s where I simply couldn’t fall asleep. For hours, I would lay awake, tossing and turning, getting angry and frustrated at my increasing alertness. After a while frustration would turn to worry….. “how am I going to function tomorrow….I need to be up at 7 to make it to work/class/etc”, “Am I ever going to be able to fall asleep naturally again in my life?”
I seriously believed that I had forgotten how to do something that I had taken for granted my entire life up until that point. To just. Go. The. F. To. Sleep.
Sleep Matters
When my clients mention that their sleep is less than optimal, I take it seriously. No matter what the main health issue is, if you aren’t sleeping well, the body and mind just can’t repair fully. Lack of sleep makes us inflamed, stressed, shifts our hormones for the worse, and impairs blood sugar balance. Our levels of patience, concentration, and creativity suffer. That word or name we are grasping for remains elusive as we struggle to communicate our thoughts.
Studies show that we tend to make poor food choices the next day. Poor sleep can even lead to weight gain, without a change in diet. Difficulty falling asleep, or staying asleep, inevitably leads to being less than fully awake and refreshed during the daylight hours— for years; I felt like I was half of myself. And that’s no way to live.
Finding My Root Causes
Resolving my insomnia required a pleiotropic (multi-faceted) approach. Testing and supporting my adrenal hormones was the first step:
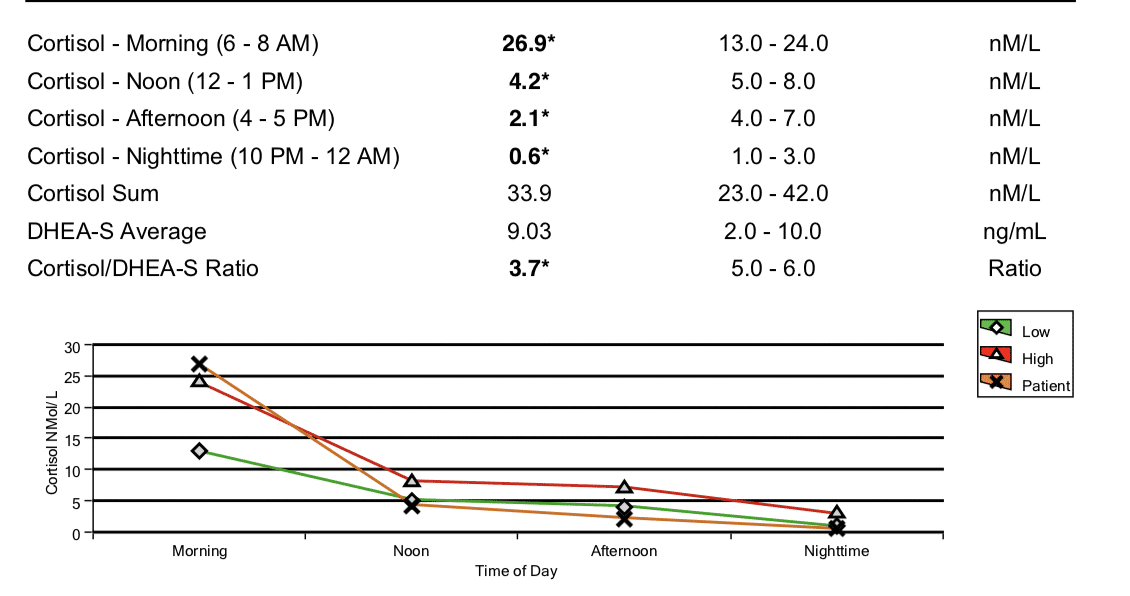
(This is a saliva panel from before I used the DUTCH Adrenal test for assessing the HPA axis in my practice. You can see that my morning cortisol was super high right when I woke up, suggesting that it had been high at night.)
However, it turned out that I also had three parasites and candida overgrowth causing inflammation, which had to be addressed before my adrenal hormones and bio-rhythms could repair. (And this was despite not having many digestive symptoms at the time!)
Test 1
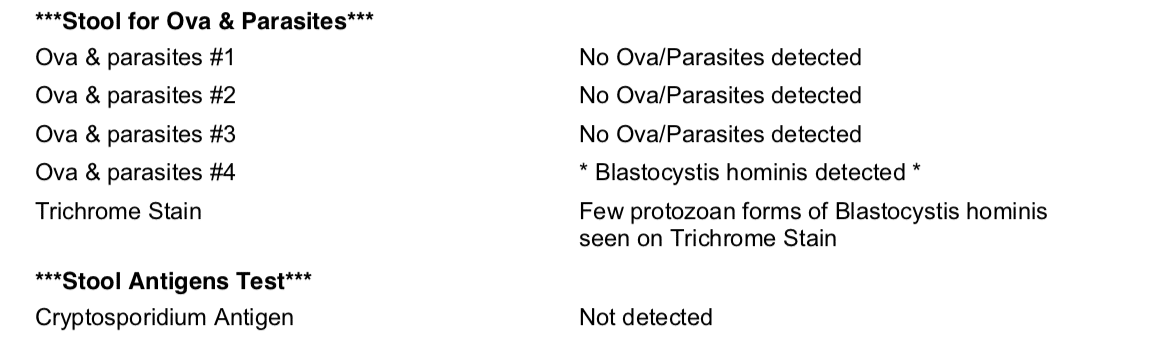
Test 2
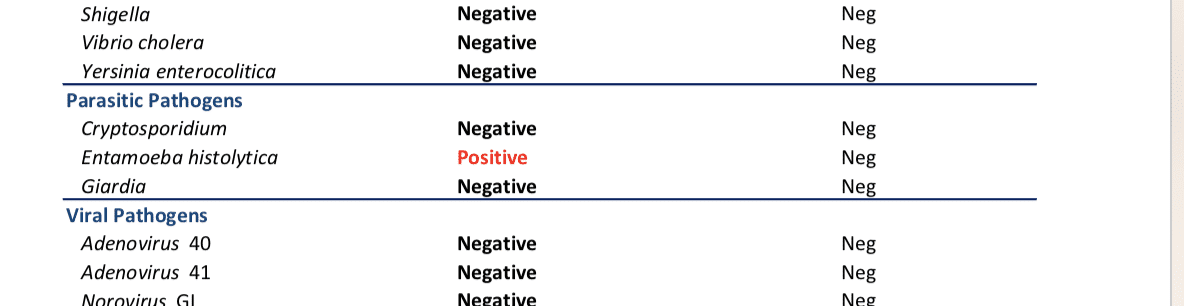
Test 3
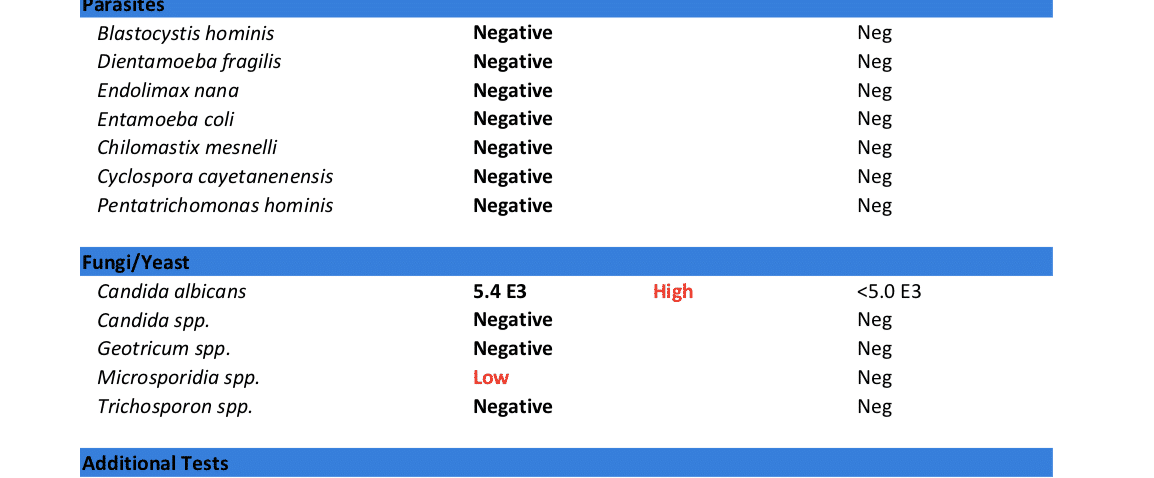
The inflammatory compounds from parasites and yeast in my gut, were neurotoxins. Exposure to these in my bloodstream was creating inflammation and oxidative stress in my brain that contributed to sleep and memory problems.
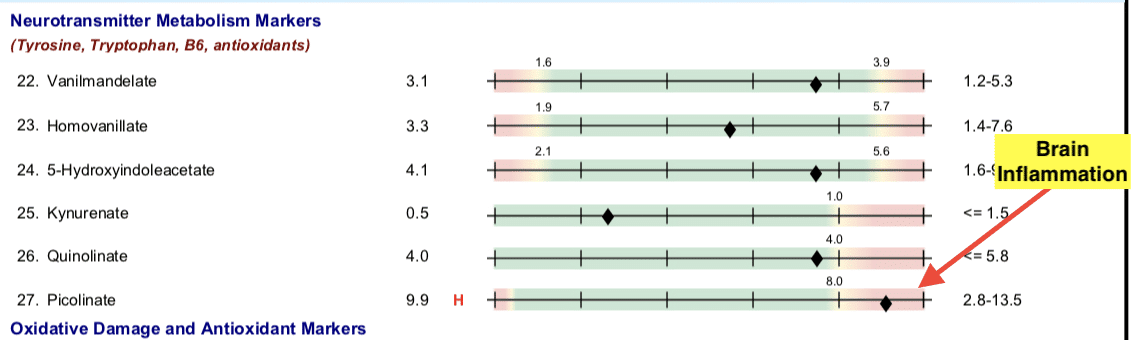
And my progesterone levels were lower than my post-menopausal grandmother’s would have been! (Progesterone production takes a back seat to cortisol production when your body is reading that you are under constant stress... *or inflammation).
To make things worse, my estrogen was through the roof. This relative excess of estrogen to progesterone is called Estrogen Dominance , and can make life in a woman's body fell like...well...a pain in the ass! (Think PMS, breast swelling and tenderness, heavy menstrual bleeding, fibroids and cysts, or weight gain around the hips and thighs....oh, and did I mention insomnia?)
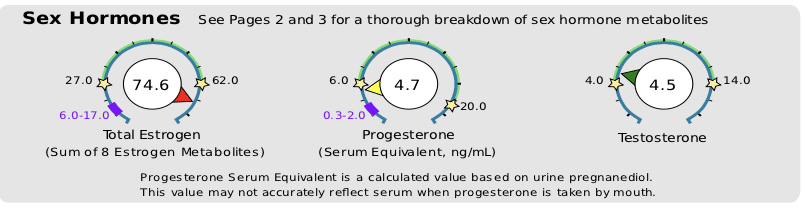
Addressing each of these issues, over a period of about a year, gradually brought about a shift in my insomnia. Even after the first month of treatment, sleep started to come easier and easier. And it just got better and better from there. I felt like I had gotten my life and myself back!
5 Steps to better sleep
Modern life, with our artificial lights, tablets and screens, digital notifications, and indoor living give our bodies the exact opposite of the signals we need to promote sleep. While testing and treating these or other underlying causes for any case of insomnia may be necessary in the long run, we just can’t “out-supplement” diet and lifestyle.
Taking steps to set yourself up for success during the day, and early evening, is essential for anyone who’s sleep is less than optimal. There are many things you can do on your own, to give your body and mind every chance of sinking into a deep, restful sleep, naturally.
Sleep Tips
Sleep is one of the most important aspects of improving hormone balance and repairing body systems, from the brain to the digestive tract. Here are additional tips to facilitate this process:
Tip 1: Train the brain to feel sleepy & awake at regular times:
- Set fixed times for bedtime and rise-and-shine- As much as possible, keep to this schedule, even on weekends, regardless of how much sleep you got the night before.
- Avoid daytime naps- as this reduces your sleep drive at night.
- Keep the lights off -If you have to get up during night to use the bathroom do not turn on the light. Use a small nightlight so that you can see enough to move safely.
- Sunlight Exposure- get at least 30 minutes per day, sunglass free. Even in a cloudy sky, the natural spectrum light is bright enough to trigger your brain with a powerful signal that it is daytime. Natural light exposure helps establish healthy sleep/wake hormonal rhythms—it has only been recently that we’ve spent the majority of our lives indoors, under artificial lights. It’s essential to do this in the morning, within the first hour of being awake. For any kind of insomnia, it’s best to wake and go to bed at the same time every day. However, if you wake at 7 AM most days, but 9 on weekend, set your daily time outside to be 9:15-9:45 to ensure consistency, grab a mug of tea, and head out the door.
Tip 2: Develop a strong mental association between your bedroom & sleep:
- Use the bedroom only for sleep (or sex)- don’t read or watch TV in bed.
- Get into bed only when you are sleepy- If you are unable to fall asleep, get up and go into another dimly lit room, rather than lying in bed awake.
Tip 3: Avoid being over-stimulated at bedtime:
- Avoid Alcohol – it may help you fall asleep, but all the sugar in the alcohol will cause a rapid rise and subsequent drop in your blood sugar which will cause you to wake up. Even low-sugar alcohols like vodka can disrupt your sleep pattern, causing lighter sleep or frequent waking. Avoid alcohol within 3 hours of bedtime, and avoid it completely if you are struggling with insomnia.
- Ditch the Caffeine- Did you know that even a morning cup of joe at 7 AM can disrupt your sleep? This is especially true in people who have genetic caffeine processing issues, due to gene SNPs such as COMT. The “caffeine kick-back effect” is more common than you would think! Avoid caffeine completely if you are having sleep problems. Avoid it after 2 PM as a general rule, even if you don’t suspect you are overly sensitive to its effects.
- Slow Mental activity -stop doing active mental work at least 1 hour prior to bedtime. This includes surfing the web, watching Netflix or movies, emailing, Facebooking, or texting. We all need wind-down activities to switch out of “doing” and “problem solving” mode. Earlier in the evening, meditation, yoga, books, audiobooks, and yes, at the very least, even watching a TV show or playing a game on your Ipad is fine (assuming you are using precautions to avoid blue-light listed below)—anything that helps you switch into relaxation mode and away from the whir of thoughts and pace associated with wakefulness.
- Get Moving!- Exercise at least 30-60 minutes every day. Even walking works.
- Avoid Blue light Exposure— Have you ever noticed that the light near the end of the day, around sunset, is naturally warmer with more reds and pinks? Blue light from screens inhibits melatonin production by signaling that it is day time. Our brains respond to dimmer light and warmer light by winding down activity, but you need at least 2 or more hours of these lighting conditions prior to bedtime for optimal relaxation.
- Install apps on electronic devices that dim blue light and use warmer spectrum tones, such as f.lux on Mac, Nightshift for iPhones, or Twilight on Android.
- Dial down the brightness on dimmer lights, screens, and digital devices.
- These apps do a fairly good job, but if you are more sensitive to light and the apps don’t cut it, also consider buying a pair of blue-blocking glasses (around $10-15—-yep, these come in a ton of super-groovy styles now that they’ve caught on). Some people even install amber-colored light bulbs such as these around the house.
Tip 4: Create an environment supportive to sleep.
Your room should be:
- Dark- cover LED lights on bedside clocks, consider blackout blinds. An eye-mask with cup shaped or curved nose pieces can work just as well.
- Cool- Your body naturally cools off when you sleep, and if your room is too hot, it can be hard for your body to give off its heat. Around -65°F is ideal for most people.
- Comfortable- use a comfortable mattress and pillow that is supportive to your neck, depending on your sleeping position. Consider using a “side sleeper” pillow for under your neck when sleeping on your side. Consider using a body pillow to hug and put between your knees to align your back and shoulders at night. I personally love the PharMeDoc C-shaped body pillow for side sleeping as it supports both neck and hips. Yes, it is marketed for pregnancy (and is a must have for pregnant women!)—but it’s great for non-pregnant people who like to sleep comfortably too!
- Quiet –Some people swear by reusable silicone earplugs like these for the best noise cancellation. I prefer the super soft foam kind so they aren’t uncomfortable. You can use them several times before they lose their “squish” and look a little grubby—then toss ‘em and grab a new pair. These plugs block out even my husband’s snoring on the loudest night!
- You can also use a white noise machine, if you don’t like the feeling of having something in your ears. Different people prefer different sounds. I don’t use one of these, but patients have told me good things about them.
Tip 5: Eating for healthy sleep
- Stop Munching- avoid being too full at bedtime. No food for at least three hours before sleep, unless you suffer from severe hypoglycemic issues.
- Don’t Under-eat: Hunger and low blood glucose can give you insomnia and can wake you up in the middle of the night. Most people’s bodies naturally help them to eat the right amount, but if you’ve been intentionally trying to lose weight, or restricted eating because of digestive or other health issues, your appetite signaling can easily get off, and so can your sense of what is enough food. If you’re not sure that you’re eating enough try this:
- Use an online calculator like this one to figure out your approximate caloric need.
- Use a food tracking app such as MyFitnessPal to keep track of your calories for a few days.
- If you’re under-eating, bumping up your calories may be the silver bullet solution to help you sleep deeper and fall asleep easier.
- Eat high nutrient foods, especially minerals: Mineral deficiencies (like calcium, magnesium or potassium) are a common factor with insomnia. The best way to ensure high nutrient content is to eat a variety foods each week, including fruits, lots of above ground veggies, root veggies and tubers of different colors, animal proteins, liver or other organ meat, seafood, and bone broth. If you don’t eat dairy be sure to get plenty of calcium containing leafy greens, and or herbs that are high in calcium to supplements, Many people need supplemental magnesium as well. Even on an otherwise healthy, whole foods, Paleo type diet, you can still have deficiencies of essential nutrients if you are eating the same foods day in and day out.
- Eat enough carbs: Carbs are super important for sleep, in several ways.
- You need dietary carbohydrate in order to produce melatonin in your brain. Melatonin counters cortisol, among other things. Without enough melatonin in your brain, sleep isn’t happening!
- People with Adrenal Fatigue may have insufficient cortisol levels to stabilize their blood sugar for long periods of time. I notice that people with low cortisol often suffer on low carbohydrate diets, because their body can’t shift into carb generation mode in the liver (which is where your body sources stored carbs between meals). When your blood sugar drops while you’re sleeping, adrenaline kicks in and you wake up out of a dead sleep, wondering what is going on. To avoid this, consume more of your carbs at your evening meal, close to bed time.
- Each person’s carbohydrate need varies widely based on activity level and baseline metabolic rate. It can also differ at different phases in life. Depending on age, gender, activity level, pregnancy status, and weight maintenance goals, people need anywhere from 50-350 grams daily. With sleep difficulty, I recommend that my clients not go below 75 grams daily. The only way to know what is right for you is to experiment and observe.
- Again, take activity level into consideration —if you are training for a triathalon, 50 grams per day is simply not going to cut it. If exercise looks like a walk to the mailbox daily, you aren’t going to need above 150 grams. Adjust these levels until you find the right fit for you.
Tip 6: Develop An evening ritual helps prepare your body/mind for sleep.
Here are some possibilities to choose from:
- Journal- If you are someone who lays awake thinking of your to do list, get it all out on paper before-hand. Planning for the next day by writing a brief list can help short-circuit the mental spinning. Alternately, write down what you are grateful for that day, or journal. Consciously release and hurts or resentments you are feeling.
- Have a cup of herbal tea (e.g. “Sleepy Time”)
- Have a bath with Epsom salts—start with 1 cup in a warm (but not overly hot) bath. Add relaxing essential oils like lavender, chamomile, sandalwood, or vetiver if you enjoy these.
- Use a diffuser in your bedroom & use lavender essential oil before bed.
- Do some gentle stretching, or yoga. I personally love using my foam roller to roll out kinks and knots.
- Try progressive muscle relaxation--this has been shown to help reset cortisol rhythm. There are many version of this available on Youtube, such as this one.
- Do “4-7-8” breathing:
- Breathe in through nose for 4 counts
- Hold your breath for 7 counts
- Exhale through mouth for 8 counts
- This combination of count ratio slows heart rate and relaxes the sympathetic nervous system.
Do the same ritual every night, as you are training your body and mind to unwind from the day and giving it the message that it’s time for sleep.
Tip 7: Supplement Support:
Ideally, supplements should only be used after the above steps are being taken consistently. But tossing and turning night after night can really put a damper on your mood, not to mention your glucose control, sugar cravings, weight, hormone balance, and overall health. There is no one sleep supplement that works for everyone, and these are just several recommendations that are generally safe for people to experiment with on their own.
If you are still struggling, work with your practitioner to identify key issues that are at play with your insomnia, such as hormone imbalances, parasites, inflammation, neurotransmitter issues, toxicity, sleep apnea, or other causes.
Consider:
- L-Theanine- 200-400 mg
- Magnesium- up to 1200 mg, in divided doses daily. Use the chelated forms for best tolerance.
- Liposomal CBD- 1ml-4ml before bed.
- Calming Herbs – Lemon balm, Passion flower, Valerian root (like this blend)
Looking for further help with improving your sleep? We'd love to help you!
Adrenal Fatigue Part 1: Stress and Your Symptoms--What Exactly IS Adrenal Fatigue?
This is Part 1 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it!
Last Sunday evening, I drove across town to meet up with a girlfriend. My husband Jacob and I had driven up the coast from our house in Santa Cruz, on highway 1, to go for a hike that morning. I had just gotten on the road to my friend’s house when I noticed my gas light was on. I drive a Honda Fit, and they never run out of gas. They get incredible mileage, so even when they are “out of gas”, you still have at least 20 miles.
On my way home, I was planning to stop to fill the tank, but decided I’d go first thing in the morning, and headed home instead. Big mistake.
The gas station is less than a mile from my house, but when I went the next morning, I was 100 yards away from it when my car….Slowly….Trudged…To..A. stop.
I was stuck in the middle lane during morning rush hour, people honking at me and yelling out their windows, with my hazard lights flashing, as I tried to push my car to the side of the road. How embarrassing! I haven’t done something like this since I was probably 16 years old!
It was another hour before I’d gotten my tank filled again and was on with my day, running late for my first appointment….sigh…
Not exactly how I wanted to spend my morning. As I rushed non-stop into my full schedule, I noticed that for the rest of the day I felt frazzled. Any capacity deal with an unexpected change of plans, or handle any conversation that required effort or patience went out the window. I wished that I’d had 10-minutes to meditate and re-center myself
When Jacob got home at the end of the day, he took one look at me and just laughed!
"Rough day, Babe?"
Luckily, after a warm bath, some gentle yoga, and a good night’s sleep, I woke up feeling refreshed and ready to charge Tuesday! But several years ago, when my adrenal hormones were on the fritz, a hectic day like Monday would have left me sleepless, exhausted, and stressed out for several days or more…..
It’s well established that all modern diseases and their symptoms are negatively impacted by chronic stress.
From PMS, to susceptibility to the common cold, to an increased tendency to develop chronic diseases like cancer and diabetes, stress clearly promotes the development and prevents healing of a multitude of health concerns.
If we feel stressed out all the time, the impact it has on our physiology can override the benefits that healthy nutrition and exercise provide to your body.
But what exactly is happening in your body when this occurs?
What Is Adrenal Fatigue?
There is a ton of misinformation about Adrenal Fatigue out there in Google-landia. Adrenal Fatigue is not a disease. It’s a syndrome that occurs as a consequence of chronic stress without relief, and is characterized by predictable symptoms like fatigue, poor mood swings, insulin resistance or low blood sugar swings, decreased sex drive, insomnia, increased susceptibility to colds and flus, and worsening PMS or menopausal symptoms. These are just a few of the signs that you might have imbalanced stress hormone levels.
Your adrenals are two small pyramid-shaped glands that sit on top of each of your kidneys. The adrenals are responsible for the production of several types of hormones—glucocorticoids, mineralocorticoids, and androgens. Cortisol, our main adrenal hormone, is made mostly in the adrenal cortex (some is also produced in the mitochondria of cells around the body). Cortisol is often referred to as our “stress hormone”—and it can get a bad rap. More aptly it could be called our “stress response” hormone—and, while we don’t want it to be super elevated for prolonged periods of time, it’s also not great for it to get overtly low.
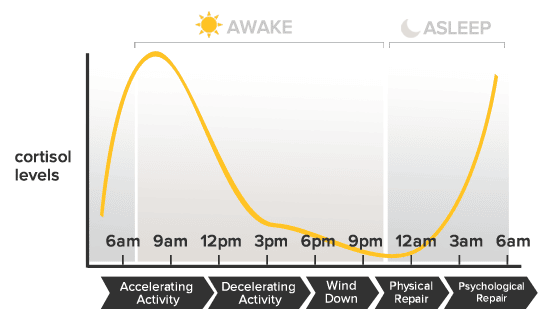
In truth, cortisol (along with meltonin) is one of the primary hormones that establishes our circadian rhythm, or sleep and wake cycle, in response to cycles of light and darkness. We want cortisol to spike highest within the first 30 minutes of opening our eyes in the morning, and then to gradually taper off over the course of the day, hitting its lowest point in the evening when we naturally fall asleep.
We need a moderate amount of cortisol to circulate daily to maintain body tissues, provide energy, put out inflammation, and to serve other vital metabolic functions. When we get in to trouble is when we keep giving our body the message to pump out high levels all the time.
Chronically high cortisol leads to:
-Imbalanced female hormones
-Increased rates of depresssion
-Increased fat storage, especially spare tire, which is good if you are in a famine, in order to survive, but not good if you are trying to look good in that cute new bikini.
-Lower thyroid hormone function and production
-Overall tissue breakdown and poor repair of injuries
-Increased risk of heart attack and stroke
-Increased risk of cancer
-And those are just to name a few...
On labs, Adrenal Fatigue is characterized when the current level of hormones produced by your adrenal glands (like cortisol) are consistently above or below the optimal ranges, or, when the daily circadian rhythm is doing something other than it should be (like being high at night and low in the morning!).
But don’t be fooled. Just because it’s not a diagnosable “disease” doesn’t mean that it can’t have a profound effect on your wellbeing! In fact, Adrenal Fatigue is often an early-warning sign of increased vulnerability to a variety of diseases and conditions such as diabetes, depression, autoimmune disease, thyroid disorders, and more.
The good news is that Adrenal Fatigue is measurable and fixable!
A trained professional can guide you through diet and lifestyle improvements, along with the strategic use of supplement and herbal protocols, to help get you back on the path to wellness.
If you think you might have Adrenal fatigue, (also called "HPA-Axis Dysregulation"--but more about in the upcoming posts) let’s get on the phone and talk about it, so that I can support you!
Click Here for the next section in this series where we’ll talk about what it feels like to have imbalanced adrenal hormones.
Adrenal Fatigue/HPA-D Part 2: How Adrenal Fatigue Feels
This is Part 2 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! To read more about the basics of Adrenal Fatigue, go to part 1, here.
The first time I ran adrenal testing on myself, I was completing my 4th year of Chinese Medicine School. After seeking help from all the best practitioners I knew (Acupuncturists, Herbalists, Ayurvedic practitioners, Nutritionists, and my gynecologist), I was desperately looking for answers to my intractable insomnia. A regular night looked like me getting in bed around 10:30 PM, and then laying awake, frustrated, anxious, and worried, until around 3 AM or later. Beside my bed was an arsenalt of herbs and supplements that at best, helped me fall asleep an hour or two earlier, some of the time.
I still had to be to clinic or class by 8 am most mornings, and prided myself on giving my all to my patients and my studies, and maintaining a workout schedule, even on 3-5 hours of sleep. After 3 years of this, I began to wonder if I was ever going to get a normal, full night of sleep again! It was my own personal kind of hell, and it had gone on waaaaay to long.
If you are living with “Adrenal Fatigue” (also called HPA-Axis dysregulation), you probably live what appears to be a normal life from the outside.
Most people can do the things they have always done and may not have any obvious signs of severe physical illness.
However, you’ll typically have a general overall feeling of burn-out, general fatigue, or a kind of flat tone to their previously vibrant lives. Or, you might not feel fatigued; instead you might feel constantly wired, or even have a hard time winding down at the end of the day.
These people often use mild stimulants like coffee to get themselves going in the morning, and keep themselves going throughout the day. In the more progressed cases, people can be so exhausted that it’s hard to get out of bed for more than a few hours per day.
Some Signs of Adrenal Fatigue Include:
- An overreaction to perceived stressors—like the pressure of writing a school paper.
- An increased susceptibility to colds, flus, and infections
- An inability to regulate blood sugar –getting shakey or spacey between meals.
- An extra 5 pounds of fat that you just can’t lose around your stomach, or 10+ that showed up out of no where and won’t budge no matter what you do!
- Feeling frazzled to the point of road rage, getting easily frustrated or overwhelmed, snapping at your partner or kids, or crying for no particular reason
- Feeling fatigued, especially if you wake up wanting to go back to bed
- Wanting to nap or snack between 3-5 pm—especially if you feel more alert and alive after 6 pm than you do all day
- Difficulty falling asleep or staying asleep
- Worsening PMS, or menopausal symptoms like hot flashes and night sweats
- Nonexistent or decreased sex drive
- Easy bruising, more easily injured, or prolonged healing time
- Lacking the same zest and drive for the things in life that used to drive you
- You want to exercise, but just can’t push it as hard, or, you feel achy or fatigued later.
- Low or high blood pressure
- Difficulty bouncing back from stress or illness
While none of the above symptoms are life-threatening in the immediate, left untreated, imbalanced cortisol levels can lead to chronic disease states down the road.
Some of the risks of untreated HPA-Axis Dysregulation/ Adrenal Fatigue are:
- Greater risk of diabetes
- Increased rates of autoimmune disease
- Increased risk of cancer
- Osteopenia or Osteoporosis
- Increased risk of Alzheimer’s
- Loss of muscle mass
- Increased rates of heart disease
- Greater chance of depression
- Higher overall inflammation.
HPA-Axis Dysregulation/ Adrenal fatigue is defined by abnormal levels or rhythms of cortisol, the main hormone produced by the adrenal glands in response to signaling from your brain. We’ll go into more depth about how this occurs, in my next post. Essentially, testing and treating adrenal hormone imbalances is not just important for feeling better now, it’s also critical for maintain long term health and well-being.
To read more about what happens in your body when stress activates your adrenal glands, click here to read Part 3.
Adrenal Fatigue Part 3: Adrenal Fatigue is actually a BRAIN problem!
This is Part 3 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read Part 1 and Part 2.
In the Parts 1 and 2, we talked about how adrenal fatigue (HPA-D) feels, and associated symptoms and disease states. But what is actually going on in our body when we experience stress, that leads to these changes and symptoms?
(warning: this post gets a bit more technical, so read on if you’re curious…or skip it and click here to get support)
How Your Adrenals and HPA-axis Work:
You are planting a garden outside of your hut, when a hungry bear and her 3 cubs stroll out of the forest. You know a hungry momma bear is not to be messed with.Your brain goes into“high alert” and, in a split second, you decide to run.
The shift into Fight-or-flight mode occurs because your brain perceives some type of danger or stressor.
This decision took you less than 2 seconds, but in that time, a complex chain of events occurred before you were able to get into Go-mode:
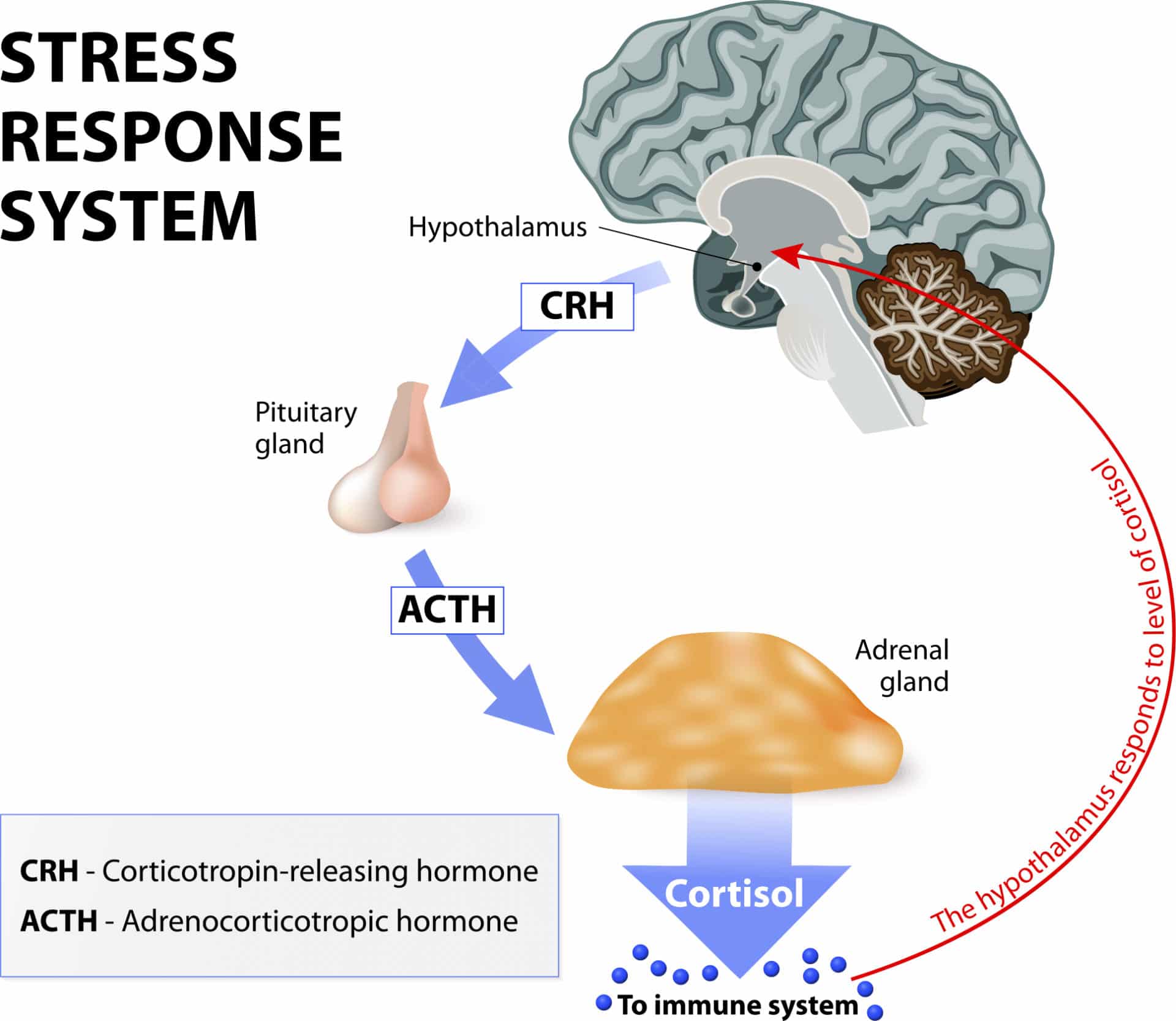
In a big game of physiological telephone, stress registers in the brain, where your hypothalamus signals the pituitary, which then signals the adrenals.
The adrenals release hormones into the blood stream that make their way to the brain. This is the negative feedback loop that lets the hypothalamus and pituitary know the message has been received and the job performed.
Depending on whether the brain is perceiving the level to be high enough to meet the demands of the stress, it will keep signaling the adrenals to produce more cortisol, or stop sending the hormonal signal so that the gland will know it has put out enough.
The stress response happens in 2 phases: First, we release catecholamines (adrenaline and noradrenaline) that prime your body to act immediately. Secondarily, these chemicals trigger a series of neurochemical processes that tell the adrenals, “It’s go time!”, meaning, please make some cortisol--NOW!
Cortisol’s main role here is to increase your heart rate and therefore blood flow to your arms and legs, for running. It also mobilizes glucose to fuel the action.
The flood of cortisol helps to increase your breathing rate, initiate sweating, dilate pupils. It also shuts down movement in your digestive tract, to make sure our muscles have enough fuel to run from the bear, remain alert and keep our bodies cool, among other things. The overall effect is to prioritize energy to the Central Nervous System, Cardiovascular, and musculo-skeletal systems, which are critical to survival in a life threatening situation.
The rest of the body’s systems, such as digestion and reproduction, which are more essential for long-term survival are temporarily reduced in activity.
Priming your body to go into fight-or-flight when under duress is just one of the many hats that Cortisol wears. Cortisol receptors are found on almost every cell in the body—that’s how critical it is to almost every aspect of our metabolism.
Modern Stress
Our bodies were designed to survive and even thrive in situations that are stressful in the short term. For most of our lives as a species, this might have looked like the situation above. It might have been caused by something equally stressful, like falling into a river and having to swim to shore. In situations like these, increased levels of cortisol and adrenaline produce the perfect physiological response to help save your life.
But in our modern industrialized world, we are exposed to a constant barrage of ongoing, sub-acute stress throughout the day. Fighting traffic, meeting work deadlines, parenting issues, relationship glitches, the mortgage, the bills, taxes, and an endless influx of text messages, phone calls, emails, and social media alerts, each add to our stress.
Then there are the stresses that don’t always feel immediately stressful, but that add to our overall stress levels in more subtle ways. These include: sitting all day, lack of exercise, overtraining without enough recovery time, skipping breakfast in favor of coffee, eating processed foods, staying up late to watch one more TV episode, or exposure to lots of artificial light after sunset.
When the stress state is prolonged, cortisol is maintained at higher than normal levels for extended periods of time. Excessive exposure to cortisol actually causes a catabolic metabolic—this causes body tissue breakdown, as opposed to growth and repair. High cortisol levels in the brain permanently burn-out nerve cells in our hippocampus, our center of emotion and memory. So, when stress is too intense, or goes on for too long, our brain down-regulates the production of cortisol, in a disrupted feedback loop.
This is why "Adrenal Fatigue" is more accurately described by the term "HPA-Axis Dysregulation" (Hypothalmus-Pituitary-Adrenal Axis). As the HPA-Axis dysregulation progresses, cortisol production often drops lower and lower, as does the production of other adrenal steroid hormones like DHEA.
Adrenal fatigue is actually a brain problem
When we talk about “adrenal fatigue” and “adrenal repair”, it can give the impression that something is wrong or damaged in the adrenal glands themselves. But issues stemming directly from the adrenal glands are truly only at hand in specific medically diagnosed disease states like Cushings or Addisons diseases.
A more accurate description of what adrenal fatigue really is, is the term HPA-Axis Dysfunction (hypothalamic-pituitary-adrenal dysfunction….say that 3 times fast!). This term describes the breakdown of the communication systems that these three glands use to talk to each other and regulate hormone production and rhythm every day.
The HPA Axis is our central stress response system. When your brain perceives that there is either something stressful or threatening in your environment (or if emotions run high), or if your blood glucose levels get low, or if you have high levels of inflammation, the hypothalamus shouts at the pituitary to do something about it. The pituitary in turn, signals the adrenal glands (by releasing a hormone called ACTH) to crank up the production line on cortisol, to help deal with the situation.
Normally, when the “stressor” is gone, the signaling quiets down, and cortisol levels should return to normal. But if the stress/inflammation/glucose problem is ongoing or severe, sometimes, the levels either stay high, or, alternately, shut down.
When you experience symptoms like fatigue, anxiety, insomnia, or foggy-brain due to imbalanced cortisol levels, it’s because of a breakdown in the signaling from the brain to your adrenal glands. In other words, the problem is in the software or programming, not in the hardware!
When we test with cutting-edge labs, and create treatment protocols, our aim is to reset the rhythm of the output of adrenal hormones. This process is dependent on restoring the feedback loops between the control centers in the brain.
After long term stress or inflammation, we adopt a new normal. Treatment to restore balance is a bit like restarting the computer and rebooting the software.
To learn more about how stress and adrenal hormone dysregulation can throw a wrench in your sex hormone balance (like estrogen, progesterone, and testosterone), continue on to Part 4.
Adrenal Fatigue Part 4: The “Cortisol Steal”—or, How Increased Stress Creates Female Hormone Imbalance
This is Part 4 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read Part one, Part two, and Part three.
Two days ago, I was getting my haircut, and I saw a picture of my hairdresser’s two adorable kids at her station. She told me she’d raised them herself, thankfully with some support from her mother and brother, and that her young daughter was quite a handful these days!
Then she shared with me that she felt like now that she had turned 43, her hormones were “making her crazy” all of a sudden—the other day, she’d snapped at 7 year old daughter about something that would never have been a big deal in the past. This type of short fuse was always worse right before her period was due, but lately, it seemed like her mood, energy, patience, and brain function shifted almost 2 whole weeks before hand! As she remembered it, her mother had gone through a horrible menopausal phase. In fact, she’d had a really tough relationship with her mother during that time because of it, and she was terrified that her menopause was going to turn her into a crazy person too!
I don’t know first-hand, but the stress of being a single parent, even with some close family nearby, just seems like it requires super-powers to withstand. It was no surprise to me that after years of stress, her reproductive hormones were taking a hit.
So how does stress impact our female reproductive hormones?
Our bodies make most of our adrenal hormones and some of our “reproductive hormones” like estrogen, progesterone, and testosterone from the same precursor horomone - pregnenolone.
Ordinarily, pregnenolone is transformed into a multitude of various hormones, in optimal ratios, every minute of every day. But the minute our body perceives it is under stress, it prioritizes cortisol production, at the expense of the other hormones.
This prioritization is elegantly designed. Progesterone, estrogen and testosterone are all hormones designed for the long-term reproductive survival of the species. Cortisol is about rescuing You, Now.
If your body receives a hormonal message that the external environment is threatening, or you’re in a famine and therefore in a fasted, hypoglycemic state, it’s probably not the best environment to bring a new baby into, right?
So, your body focuses its energy and resources on saving you, and diverts its “attention” away from making hormones that are specific to reproduction and other “non-essential” activities. This allows for the production of a huge amount of cortisol, but inhibits the production of virtually every other hormone. When the stress resolves, our brain stops sending the signal to increase cortisol production, and hormone levels return to normal…in theory.
Pregnenolone can convert down either of two main pathways:
- Conversion into progesterone, as a first step on the path to being converted into cortisol, and/or cortisone, our main anti-inflammatory hormone.
- It can be made into DHEA, which is the precursor to all of our sex-hormones.
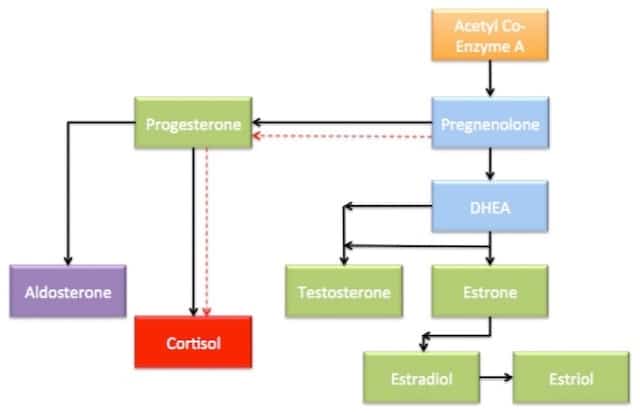
When under stress, the body will decrease DHEA production and prioritize the cortisol production. While the majority of our reproductive hormones are produced in the ovaries and testes, roughly 30-40{0ace9f30246476cbe34912402cc70dd667071e9efa13e47cc458477e17894418} is produced in the adrenals. This amount significantly impacts the maintenance of the overall stable hormone levels in circulation.
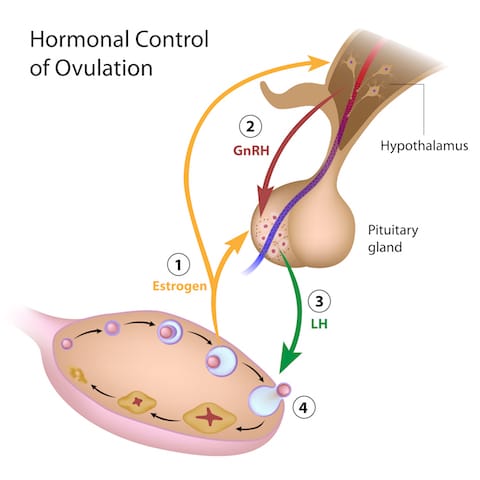
But there are other ways that stress impacts our monthly hormone cycles as well! The HPA axis is closely related to the HPO (Hypothalamic-Pituitary-Ovarian) axis. Just like these glands in the brain have feedback loops and signaling systems that tell the adrenals what to do when, we also have telephone lines between the hypothalamus, pituitary, and ovaries.
High cortisol levels block the HPA axis at each step in the chain. High cortisol stops the secretion of the hormone that our Hypothalamus send to the pituitary (GnRH) that tells it to make LH and FSH. LH and FSH are the hormones that the pituitary makes in order to signal the ovaries to make estrogen and progesterone. When these are suppressed, the ovaries don’t get the message. And, to make matters worse, elevated cortisol levels also interfere directly with ovarian hormone production, which is the bottom line.
This system is meant to protect you, and ultimately, to help your body know when the situation is safe for reproduction. But this brilliant system isn’t built to cope with today’s messy, stress filled world. We used to live in villages where everyone shared the responsibilities of life, food, shelter, and survival. For most of the humans on the planet, most of the time, everyday life was pretty ho-hum, and big stresses only occurred from time to time. Now we’ve each become our own village, wearing all of the hats every day, in industrialized countries. Our lifestyle of convenience and high-speed access to everything may not be so convenient after all.
Worsening PMS, stronger menstrual cramps, increasing hot flashes and night sweats, or periods that go AWOL are some of the red flags that Adrenal Fatigue and stress may be causing female hormonal imbalances!
Read on in Part Five, about the types of Stress (it's not just emotional stress!) that can disrupt adrenal hormones!
Adrenal Fatigue Part 5: When the Bear Isn't Really a Bear—What Causes Adrenal Function to Become Compromised?
This is Part 5 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it! Click here to read part one, part two, part three, and part four.
"Girl, I've had the craziest week!" How many phone calls with my best girlfriends start off something like that?
A lot.
Life happens; kids, husbands/wives, job related stuff, disagreements with other friends, and the stuff that pops up out of left field, like the water heater breaking down. These are the things we call "stressful" in conversation--but there are several other types of stress that our body will respond to in the same way hormonally, even though we don't feel stressed out at the time.
When The Bear Isn’t Really A Bear:
Cortisol increases neurological excitability and heightens sensory perception. This is great for a survival situation, but the same mechanism can cause anxiety, panic –and stress. Good if running from a hungry bear, not so much if you are sitting in a job interview.
Types Of Stress:
Stress is classified in three broad categories:
Emotional or Circumstantial – a few common examples are:
- Grief
- stressful relationships
- a rocky divorce or breakup
- caring for ailing family members
- toxic work environments
- Starting a new job or moving to a new place
- post-college graduations expectations
- starting a new business, while buying a house and having a kid, all in the span of a few years
- lack of regular movement, or excessive exercise & overtraining, (especially too much endurance cardio)
- Inadequate sleep depth or not enough hours
- overwork
- keeping late hours
- having a constant feeling of having too much on the "To Do" list and never quite keeping up
Obviously not all of these “stressors” are unpleasant or traumatic. Just being in “Go-mode” all the time is enough to dysregulate stress hormones!
Dietary:
- Skipping meals
- overeating sugar and processed carbs
- too much carb intake for your body in one sitting
- alcoholism/drug abuse
- restricting calories
- eating poor quality food with lack of nutrient density (like snack food, fast food, or frozen dinners)
Eating pastries at the coffee shop, or even bowl of oatmeal with raisins elevates your blood sugar. As a result, insulin rises to help the glucose get into cells to be used for fuel. But the residual insulin from the surge can easily drop your blood sugar levels too low, so you crash a few hours later.
Your adrenals then pump out cortisol to try to level out the glucose levels.
Going excessively long without eating also causes the body to secrete cortisol, due to stress, just as if the bear jumped out of the forest. Except we don’t register starvation as “stressful” mentally because the stress takes a different form. High sugar, high carb, and high grain diets, especially those low in fats and protein, act on our bodies in the same manner. Ever found yourself in an argument (about nothing important) with your spouse or friend, and had it occur to you that you were "hangry"? Blame it on cortisol!
Chronic Pain & Inflammation
Pain is obvious: migraine headaches, knee problems, bad backs, old unresolved injuries from sports or accidents, severe menstrual cramps every month are just a few common examples.
But people are rarely aware that they are inflamed.
Inflammation is anything that ends in “it is” - arthritis, colitis, gingivitis, etc.
Inflammation can also come on after an acute infection that is severe, such as influenza or pneumonia, appendicitis, etc. But the majority of inflammation is caused by one of 4 things:
- Chronic low grade Infections (such as parasites, yeast overgrowth, SIBO, mold/biotoxin illness, or chronic viral infections)
- Exposure to foods or chemicals that we are “sensitive” or “intolerant” to.
- The toxicity of heavy metals trapped in the body’s tissues after exposure
- Too much sugar or too much Omega 6 (from industrial oils) in the diet.
Emotional stress, dietary stress, pain/inflammatory stress. Think about this for a minute: We’ve all gotten in a fight, or had some really bad news, or lost a pet or someone we love, and felt the immediate impact of the stress and high emotions.
But our body responds in the same way to chronic pain (like migraines and unresolved injuries), or chronic low-grade inflammation from undiagnosed gut infections, food reactions, or chronic viral infections. We have the same hormonal/chemical response. We don’t feel it on a conscious emotional level, yet it impacts our body just as profoundly.
Read part Six to find out if cortisol imbalance is to blame for your blood sugar issues or weight gain.
Adrenal Fatigue Part 6: Is Cortisol to Blame For Your Blood Sugar Balance or Weight-Loss Resistance?
This is Part 6 of an 8-part series about Adrenal Fatigue (HPA-Axis Dysregulation), how it relates to your health, how to know if it’s impacting you, and what you can do to fix it!. Click here to read parts one, two, three, four, and five.
When Mary came to see me, she was extremely frustrated because, despite cooking most meals at home, and exercising most days of the week, she just couldn't’ seem to get rid of the 10 extra pounds that she was carrying, mostly around her hips and stomach.
“I get it,” I told her. Hey, I’m a woman too, and while my priority is to be healthy and to feel good, I’m not gonna lie, I want to stay fitting into my date-night jeans too!
In post number 3 in the series, I mentioned how one of cortisol’s main roles in Fight-or-flight is to keep higher levels of circulating glucose in the blood for fuel. It does this by inducing a process known as gluconeogenesis, where fatty acids and amino acids are converted into useable blood glucose in the liver.
Generally, when our blood glucose levels rise, our pancreas secretes insulin to move the glucose into cells for storage, so that it can be used later during periods of activity. Having elevated cortisol long term leads to consistently higher glucose levels, which leads to consistently elevated insulin levels, as the body attempts to get glucose out of the blood and into storage. The purpose of the stored carbs is to generate a source of rapid fuel for the body. This is required if you, say, need to run from a bear.
But what if the bear isn’t a bear, but is rush hour traffic that‘s making you late for an important presentation. Rather than running down the highway to burn off some of your excess adrenaline, you’re forced to sit there and feel anxious as the minutes tick by. Now you’re just sitting still, with high blood sugar levels circulating, and no good use for them.
After a while, your body recognizes that you’re not using the liberated glucose. Your body then pumps out higher levels of insulin, to transport the glucose into fat cells to be stored. When you have high insulin and high cortisol levels your body typically stores this energy in fat cells located around the midsection or belly. Overall weight gain, or weight loss resistance are also common. To add insult to injury, adipose tissue can actually generate it's own cortisol, jump-starting a vicious circle of chronically elevated cortisol that makes fat just impossible to budge.
Chronically high levels of insulin can also lead to a pre-diabetic condition called metabolic syndrome (or insulin resistance) and type 2 diabetes, which also leads to increased weight gain. Because of the relationship to blood sugar regulation, anyone with diabetes, pre-diabetes, whether overweight or thin, should have their adrenals tested and seek treatment if necessary.
Chronic stress also impacts appetite-regulating hormones like ghrelin and leptin, affecting our levels of hunger and satiation, as well as food preference.
If you’re struggling to lose weight, despite your best efforts, testing your cortisol levels may provide you with valuable insights into what’s getting in the way of your weight loss, and how to fix it!
Stay tuned for the final posts in the series, where I'll discuss different types of testing, and some simple-but-powerful steps you can take to start to heal adrenal fatigue on your own.
Recipe: The Best Waffles in the World! (Cassava Flour Waffles)
A large percentage of my patients have SIBO and are on Low Fodmap diets, are on a version of AIP (Autoimmune Paleo), or a paleo diet. So I’m always looking for safe starches to include to ensure proper carbohydrate intake and to act as food for their good gut bugs. Squashes, sweet potatoes, and root veggies make up a good amount of the carb sources in my diet as well as many of my clients.
But once in a while, I want something with that perfect amount of CRUNCH.
Something that you can slather with grass-fed butter when you need some comfort food from childhood....
Growing up, my house was a waffle house, at least on some weekends. Now, since we have (mostly) eliminated grains in our house, bread-like things happen less frequently, and waffles were unheard of.
But then I fell in love with Cassava.
Many of you know next to practicing Functional Medicine, my biggest passion is dancing, specifically dances of the African and afro-brazilian diaspora. On my last trip to Brazil, I realized how many things are made with cassava/tapioca, and also how absolutely delicious it is! Besides frying the chunked root, it is made into cakes, mashed, and (my personal favorite) miniature cheese-bread rolls called “pao de quiejo” (cheese bread).
Cassava (also known as yuca) is a starchy tuber, and is a staple for millions of people in South America, Asia, and parts of Africa. This plant can be processed into both tapioca starch as well as cassava flour (which maintains the fiber content), each of which have slightly different properties when it comes to using them in cooking and baking.
And, it can be used to make, hands down, the best waffles in the world.
I made these at a birthday breakfast for my extended family recently, and no one could believe they were grain-free. Even the pickiest eaters downed at least 2
Cassava is naturally gluten, grain, and nut-free, and is also low FODMAP. But somehow, it’s a pretty close replacement for wheat flour in terms of texture, and can be used as a replacement in most recipes 1:1.
One thing to note before going on a cassava binge: it is very high in carbohydrate per gram, compared to other roots like sweet potatoes or beets. This can lead to glucose/insulin spikes in those who are sensitive, or if you eat too much. If you’re on a low carb diet, or have diabetes or other blood-sugar issues, avoid cassava, or save it for the occasional treat.

The only brand I use is Ottos Naturals, as I’ve heard of other people having less-than-stellar results with other brands. There are tons of great recipes out there for tortillas, breads, naan and other treats out there in the inter-webs if you do a quick google search. But this waffle recipe takes the cake, IMHO! (Credit to Laura Franklin of Fresh & Frank)
Crispy Cassava Blender Waffles
Makes about 10 standard square waffles
Ingredients
1 cup Otto’s Cassava Flour
1/2 tsp Himalayan salt
2 tsp baking powder
1/2 tsp cinnamon
1 ripe banana
2 organic eggs
1-2 tsp real vanilla extract
2 Tbsp organic virgin unrefined coconut oil
1.5 cups coconut or almond milk
Directions
1. Preheat waffle iron.
2. Throw all ingreidnets into blender.
3. Blend all for about 30 seconds to 1 minute.
4. Check batter; if it seems too thick still, add a splash more almond/coconut milk or water. You want it thick but still able to pour.
5. Pour onto waffle iron. Depending on the integrity of your waffle iron, you may need to cook these twice to make sure the inside cooks through.
6. Remove when crispy and golden brown on the outside. (I know it’s hard to wait, but don’t remove too early!) Top with desired ingredients.
Waffles freeze well and can be thrown directly in the toaster to crisp up!
10 Common Signs & Symptoms of Polycystic Ovarian Syndrome
If you've ever struggled with infertility, irregular menstrual cycles, or other reproductive problems, please know that you're not alone. Thousands of women out there are striving for help and healing in the face of such frustrating health issues.
One relatively unknown yet common cause of reproductive health problems is a condition known as Polycystic OvarianSyndrome, or PCOS for short. PCOS is so common that it affects as many as 1 in 10 women of child-bearing age, although even girls as young as 11 can be affected. Considered a hormonal and metabolic imbalance, PCOS is the leading cause of infertility worldwide.
10 Top Signs & Symptoms of PCOS
By definition, PCOS is a syndrome, not a specific disease. This means there is no one test or procedure that can confirm a diagnosis. Instead, clinicians must rely on a thorough evaluation of each individual woman's signs, symptoms, lab markers, and patient history in order to determine if PCOS is the cause of her symptoms.
Effectively, PCOS is a diagnosis of exclusion. That is, a woman may receive a diagnosis only if and when other diseases that could explain her symptoms have been ruled out. As the most common hormonal disorder in women of reproductive age, PCOS impacts over 100 million women around the world, and has impacts on health that extend beyond the reproductive system to cardiovascular health, metabolic and immune health.
So, what are the indicators of this syndrome? Could you or someone you know be affected? Take a look at the following 10 signs and symptoms. They could suggest the presence of PCOS:
1. Irregular ovulation and/or menstrual cycles.
Women with PCOS may experience long or irregularly timed menstrual cycles, sporadic or missing ovulation (oligo-ovulation or anovulation, respectively) amenorrhea (absence of a period), or dysfunctional uterine bleeding (spotting). Additionally, a pelvic ultrasound may show increased thickening of the endometrial lining of the uterus. Ultrasound imaging can also show enlarged ovaries covered with a series of cyst-like formations which often resemble a "string of pearls."
2. Infertility.
This may be one of the most stressful and troubling symptoms for many women with PCOS who are otherwise trying or would like to become pregnant.
3. Hirsutism. (Excess hair growth)
This is a medical term that refers to male-patterned hair growth in women, including excessive hair on the upper lip, chin, chest, abdomen, and/or back—exactly where most women don’t want it.
4. Hair loss.
A bit of a double-edged sword, isn't it? In addition to excessive hair growth in unwanted places, PCOS can also cause thinning of hair on the scalp and in some cases male-pattern baldness. It’s just not fair.
5. Acne.
Breakouts can be moderate to severe, or newly developing in adulthood, when everyone else’s teenage-acne is ancient history.
6. Obesity and overweight.
Weight gain is common, as is the increased likelihood of related metabolic disturbances including pre-diabetes and diabetes. Interestingly, not every woman with PCOS will be overweight—in fact up to 50% of women affected by this syndrome may be normal weight or even underweight.
7. Darkening of skin.
This hyperpigmentation, called acanthosis nigricans, is usually the most obvious around the groin, underneath the breasts, and in the creases of the neck.
8. Skin tags.
These small flaps of excess skin typically grow around the axilla (armpits) and/or neck area.
9. Depression.
The distress caused by other symptoms can lead many women with PCOS to feel depressed, although depression or anxiety can be symptoms in and of themselves. Additionally, women with PCOS often experience a low or absent sex drive, and a lower stress tolerance.
10. Abnormal lab tests.
Blood work and other tests may indicate elevated levels of male hormones such as Testosterone (also known as androgens), and a ratio greater than 2:1 between two hormones known as the lutenizing hormone, or LH, and follicle stimulating hormone, FSH (a normal ratio is around 1:1). There are other lab markers that can further characterize PCOS, and I will discuss these in the next article in this series.
Recognize any of these symptoms in yourself or another woman in your life?
If so, be sure to consider requesting screening with labs and ultrasound. If you're looking for a holistic, effective, and individually-tailored approach, I invite you to consult with myself (PCOS whisperer) and the rest of my integrative team. We're here to help you heal, and it's my honor to join you on your journey toward better reproductive health.
To learn more about the role of Functional Medicine in the treatment and management of PCOS, schedule your initial consultation or a FREE 15-minute Consultation today.
Recipe: Grandma Fleischer’s Chopped Liver
Liver.
You either love it or you hate it. Or you're too scared to find out.
If you ask someone who grew up in a family where you regularly ate liver, or other organ meats, they'll inevitably grin with deliciousness. But for those of us who didn't dish up liver and onions regularly, the idea can be a bit foreign.
Given the opportunity, most little kids that get introduced at an early age actually LOVE liver.
Personally, I grew up on the east coast, near lots of kosher delis, and ate my fair share of chopped liver. I remember being held in my grandfather's arms, at the fridge, eating it on a spoon out of a deli container and begging for more. Somewhere in my later childhood years, it stopped being something we had around, and by the time I was 23, (after a 15 year stint as a vegetarian), you couldn't pay me to touch the stuff.
A few years ago, with the bone-broth-slurping, organ-meat-eating trends that came with the advent of the Paleo movement, I started really looking at nutritional content of organ meats. Bite for bite, liver holds it's own against virtually anything you can call food, when it comes to nutrient content. Liver is particularly high in Vitamins A, C, Biotin, Folate, and B12, as compared to other foods that are considered to be good sources of these nutrients. In Chinese medical nutrition, liver has been touted for centuries as the best "blood builder" and fertility food-- and indeed, with high levels of iron, folate and b12, it's a sure fire way to help alleviate anemia.
Armed with this knowledge, I was determined to re-learn to eat liver.
If my 3-year-old self could do it, so could my 38-year old self!
Now I learn a lot from my patients. And on my mission to love liver, it was one of my long time patients, Adam, who came to my rescue. After a discussion about this in my office, about once a month or so, Adam brings me a little glass jar with his grandma's chopped liver, and some celery sticks or Mary's Crackers.
And as I sit and munch, it's like I'm 4 all over again....
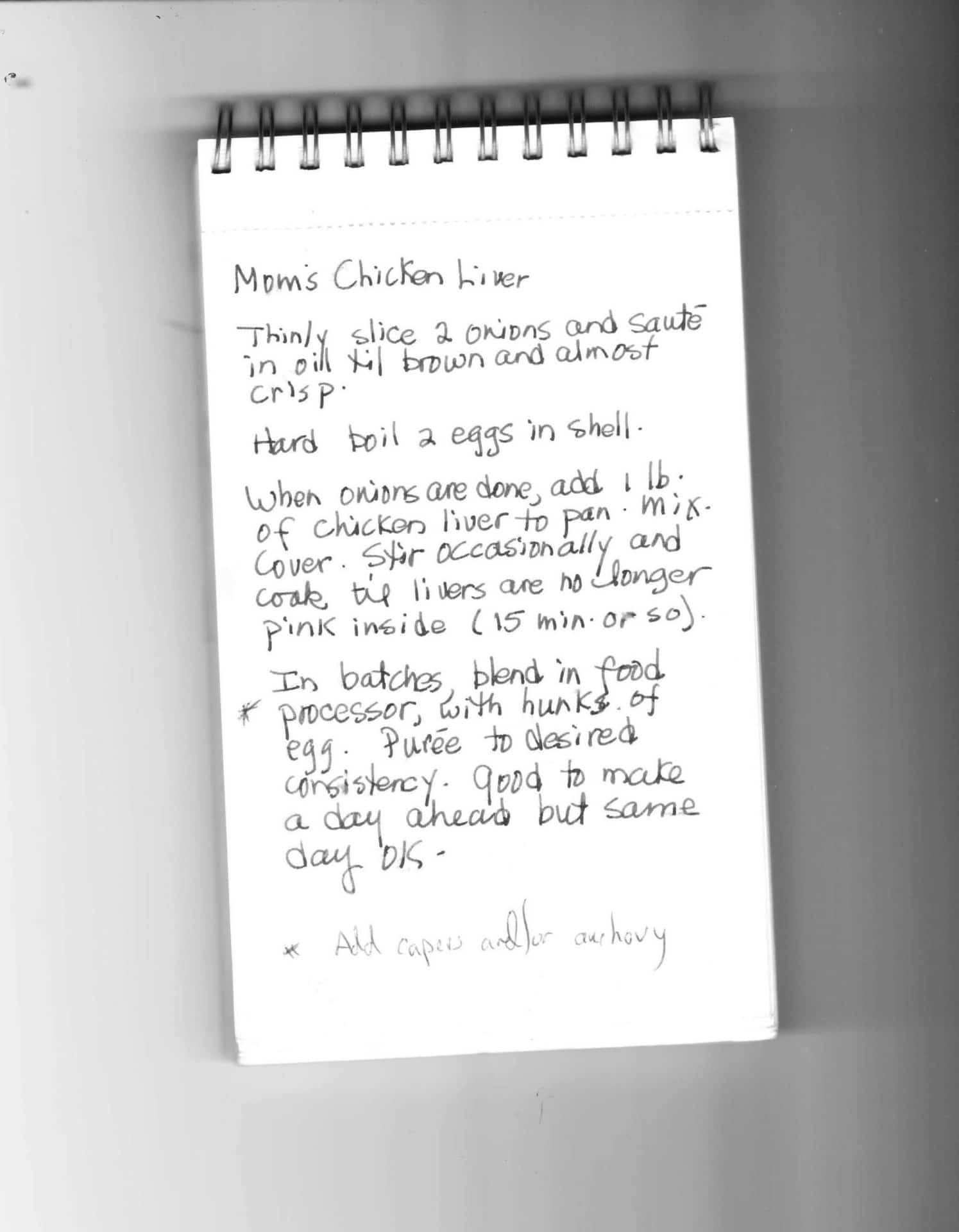
Grandma Fleischer’s Chopped Liver
(With huge gratitude to Adam F)
Ingredients
1 Lb Pasture Raised/Organic Chicken Livers
2 Yellow Onions
2 Eggs, hard boiled
Salt
Pepper
Optional: 2-4 slices of Bacon, Anchovies and/or Capers
- Thinly slice 2 onions and sautée in oil until caramelized brown and almost crisp. Be sure to salt and pepper liberally as you sautée. You can use avocado oil or grass-fed butter for sautéeing, or you can start with 2-4 chopped up pieces of bacon in the pan, and then use that fat to sautée the onions. Cooking time for the onions is 10-20-mins.
- When the onions are done, add 1 LB of chicken livers to the pan, salt and pepper again. Cook 8-12 minutes, on medium (not high) heat, turning or stirring every few minutes (but not too much stirring).
- Very important! DO NOT OVERCOOK THE LIVER--The livers should still have a little pink in the centers when done.
- In batches, remove livers and onions from the pan and transfer to a food processor with chunks of the hard boiled egg. Puree until it reaches the desired consistency. For an added kick, toss in a handful or two of capers and/or some small anchovy fillets. It just takes a few pulses in the food processor, don’t overdo it.
Serve with celery sticks, crackers, or other veggies and enjoy. This is best prepared a day in advance and then served the next day, but is still delicious when made the day of!
Top 3 Uses for This Amazing Probiotic Yeast
In the world of natural health, yeasts get a bad rap. But one of my favorite probiotics, Saccharomyces boulardii, is actually a beneficial medicinal yeast!
Commonly referred to as S. Boulardii, it was originally found on lychee fruit in the 1920s. When taken as an oral supplement, it colonizes the gut within three days. But the colonization is temporary—S. Boulardii disappears from stool within five days of discontinuing supplementation. Interestingly, the health benefits that it provides last beyond the time of oral consumption—which means that, like most other probiotic supplements—the benefits are not due to the probiotic strains taking root and colonizing.
Used for prevention and treatment of diarrhea
Many types of diarrhea are caused by dysbiosis (bad organisms living in the gut). When this occurs, the healthy microbial population takes a significant nose dive--especially important species like Bacteriodies, Ruminococus and Prevotella.
At the same time, the gap formed by the notable decrease in these beneficial bacteria, creates a void-like vulnerability that allows for increases in opportunistic bacteria like Enterobacter and less desirable Clostridia strains—these are aptly referred to as “pioneer bacteria” because they migrate to an area when there is an opportunity!
In this situation, Saccharomyces Boulardii has been shown to help in several ways:
- S Boulardii actually helps to bind pathogenic bacteria and carry them out of the digestive tract, especially Staphylococcus aureus, Klebsiella, Candida, and Salmonella
- Several human studies have demonstrated that S boulardii supplementation leads to faster re-establishment of a healthy microbiome, when recovering from infectious diarrhea.
- It increases the population of specific types of bacteria that are known to produce short chain fatty acids (SCFAs) by fermenting dietary fibers (prebiotics) and resistant starch. SCFAs are the energy substrate of cells in the gut lining that allow it to constantly heal and regenerate, preventing Leaky Gut. They also directly support some of the commensal (or good) bacteria as well.
S Boulardii is most notably useful in infectious Clostridium difficile infection. Clostridium Difficile (also called “C Diff”) is the primary cause of acute diarrhea after antibiotics, and it not an infection to take lightly. In extreme cases, it can even be life threatening. When 124 patients on high dose vancomycin (an antibiotic) for C. difficile related colitis were given S. boulardii, rates of recurrence plummeted from 50% to 16.7%.
But bacteria are not the only micro-organisms that can cause diarrhea. Overgrowth of yeasts like Candida Albicans can also induce diarrhea by causing inflammation of the gut lining. S boulardii has been shown to decrease tissue inflammation in the gut caused by colitis from Candida overgrowth, alleviating diarrhea from this cause.
Disrupts candida colonization in vaginal and other tissues
Candida albicans is the most common opportunistic fungal pathogen found in the human body. It has many tools at its disposal that allow it to thrive and take root; the ability to adhere to tissues and even penetrate them, biofilm formation and the ability to transformation into different forms at various stages of its life cycle.
In order to get an overgrowth in the first place, adherence is the first necessary step. Candida albicans is capable of adhering to the inside of cheeks, labia, vaginal and intestinal epithelial cells, as well as catheters, dental implants or artificial joints.
Not only has it been shown to interrupt Candida’s adherence, but S. boulardii is uniquely able to stimulate Secretory IgA (SIgA), our first line of defense against invading microbes. SIgA is essential to maintaining intestinal mucosal integrity, preventing leaky gut, and ensuring a stable, diverse microbiome—which is key to bulletproofing your gut. This is the main immune agent found in mucous membranes, saliva, tears and vaginal secretions, as its main function is to help protect you against pathogens.
Prevention
Perhaps the best use of S Boulardii is prophylactically.
With Antibiotic use: Since it yeast are not killed by antibiotics (only bacteria are susceptible to antibiotic drugs) you can (and should) take S boulardii during antibiotic therapy to prevent Candida overgrowth and other diarrhea-inducing opportunistic pathogens. Several studies have demonstrated that in patients with known H. pylori infection, S Boulardii supplementation improved eradication rates and reduced treatment-related side effects.
You can also take it before, during, and after travelling—it helps prevent traveler’s diarrhea! Meta-analysis of probiotics used preventatively for travelers diarrhea all showed significant reduction in the risk of traveler’s diarrhea when probiotics are used—but two randomized control trials showed a significant reduction in traveler’s diarrhea in the S. boulardii group compared with other types of probiotics used as controls.
For this particular purpose, I suggest 1000 mg daily. Should you get sick while travelling, you can continue to take it during traveler’s diarrhea, or ongoing diarrhea, to shorten the duration and promote recovery.
A word of caution
S Boulardii has been shown in studies to be helpful helping improve symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome. For example, in a 6-month study of patients with Chrons Disease, the relapse rate was significantly lower in patients treated with mesalazine plus S. boulardii (6%) than in those treated with mesalazine alone (38%).
That said, in my clinical experience, people with Inflammatory bowel disease should proceed with caution, when initially introducing S boulardii. The reason for this Anti-Saccharomyces cerevisiae antibodies (ASCA) have been associated with Crohn's disease (CD). Saccharomyces Cervisiae (Brewer’s/Bakers yeast)—used in baking as well as in brewing beer and wine—is similar enough to Saccharomyces Boulardii that the immune systems of sensitive individuals can cross react, potentially triggering a symptom flare. If any flare in symptoms is noted with oral consumption, discontinue use. Like other probiotics, S boulardii is also not appropriate in severely immunocompromised individuals.
To buy Saccharomyces Boulardii, click here!
Have you ever used this probiotic yeast for your gut health? What was your experience?
11 Ways to Minimize Toxic Estrogen Exposure
It’s a fact of modern life that environmental estrogens are everywhere these days.
These estrogenic chemicals (estrogen mimickers) are endocrine disruptors (they disrupt hormone signaling) and can also mimic estrogen in their structure. Toxic estrogens can take the place of your healthy estrogens in your estrogen receptor sites, yielding an overall more powerful net estrogenic effect in your body. We love healthy estrogen levels, but more of a good thing isn’t always better!
This phenomenon is one of the biggest factors impacting our hormonal health, increasing rates of health concerns like infertility, breast cancer, and PCOS (Polycystic Ovarian Syndrome). Even without causing a namable syndrome or disease, xenoestrogen exposure can still promote estrogen dominance, a common condition where the levels of estrogen in the body outweighs the relative amount of progesterone available to balance it. Estrogen dominance commonly shows up in your body as things like PMS, breast swelling and tenderness, heavy menstrual bleeding, fibroids and cysts, or weight gain around the hips and thighs.
Xenoestrogens can be found in shampoo, conditioners, lotions, air fresheners, household and industrial cleaning agents, and even in your food!
Here is how to reduce estrogen exposure and estrogen mimickers:
1 Filter your drinking water
Trace amounts of estrogens from Oral Contraceptive Pills have been found in city water supplies, but over 90% of the estrogen found in drinking water actually comes from run off from animal manure. These make it to your tap, so unless you filter your water, you may be drinking a dose of estrogen daily. Bottled water isn’t any better, especially if it’s in BPA containing plastic. In other hormonal news, chemicals like Organochloride and Fungicide in water have also been shown to cause hypothyroidism.
2 Limit processed foods
As though we needed one more reason to ditch processed foods, estrogen-laden BPA is a common ingredient in found in the lining of packages which can soak into the foods stored inside of them. BPA is found in the linings of cans (including canned beverages), plastic windows on food boxes, hot beverage lids, and others types of food packaging.
3 Limit dairy and choose wisely
All dairy contains hormones, naturally—think about it, this is breast milk used to feed baby cows, so just like post-partum human breast milk, it is naturally chock full of hormones. If you tolerate dairy, choose organic since this ensures that no hormones or antibiotics were used to treat the cows. Choose grass-fed for an extra nutritional bonus.
4 Use glass, stainless steel, or silicone food storage containers and drinking vessels
Plastic food containers may contain bisphenol A. Never heat plastic containers or wraps in the microwave; heating plastic causes estrogens to leach into your food. But so does freezing food in plastic, so avoid that also.
5 Choose organic when possible
Fruits and veggies grown with pesticides are literally sprayed with estrogen. If you can’t buy all organic, prioritize organic for the foods found on the “Dirty Dozen” list.
6 Minimize soy products
A few of the proven health risks that soy-researcher Kaayla Daniel mentions in her extensive book on the subject, The Whole Soy Story are:
- Soy formula contains as much estrogen as 4 birth control pills, which can vastly alter hormone balance in babies and can predispose them to cancer later in life.
- Soy consumption has been linked to infertility, breast cancer, kidney stones, and immune system impairment.
- Soy isoflavones can lower thyroid function.
7 Eat brassicas and flax seed every day
Flax seeds contains powerful little plant chemicals called lignans that are actually phytoestrogens (plant-based estrogens). Phytoestrogens have a weaker overall effect than the estrogens that we produce in our body, so they can be used to help block excess estrogen from estrogen receptors in women with estrogen dominance. In women with low estrogen, flax can help boost levels. Flax also has anti-cancer properties and supports digestive and cardiovascular health. Broccoli, bok choy, Brussel sprouts, cabbage, cauliflower and collard greens are all Brassica family vegetables. Brassicas contain a natural compound called IC3 that is a potent antioxidant and helps clear excess estrogen from the body.
8 Avoid using chemical pesticides and fertilizers
In studies, Women who used pesticides experienced 60-99% increased odds of longer menstrual cycles, missed periods, and mid-cycle bleeding compared with women who never used pesticides. Using non-toxic products for household cleaning is similarly important.
9 Ditch your nonstick pans
The perfluorooctanoic acid (PFOA) used to make products grease- and waterproof is an environmental estrogen. When the cookware is heated, PFOA can seep into your food. Nonstick pans also release chemicals that block thyroid hormone receptors.
10 Avoid phthalates in your cosmetics and body-care products
Phthalates disrupt both estrogen and testosterone receptors. These are mainly used in fragrances, and the FDA doesn’t require them to be labelled on personal care products. Using fragrance-free and organic products helps to limit exposure. While these are still allowed to be sold in the US, the EU has banned their use proactively since 2004.
11 Avoid hand sanitizers and handling receipts.
Both contain BPA that can absorb through your skin. Hand sanitizer contains alcohol which helps the BPA to absorb in greater rates.
Are you concerned that you have symptoms of Estrogen Dominance and estrogen mimickers or looking for information on how to reduce estrogen? Let's talk about it!
All About Food Sensitivities - New Cutting Edge Test Available! (KMBO FIT Test)
One of the primary tenants of Functional Medicine is to identify triggers for inflammation and reduce exposure. Sometimes, this looks like parasites or yeast overgrowth, sometimes it looks like an imbalance in amounts of Omega 6 to Omega 3 in the diet. And other times, this has to do with otherwise healthy, everyday foods that we eat, that simply aren’t a good fit for us at the time.
In theory, this should be simple. But historically, identifying food sensitivities accurately has been a challenge. Hundreds of tests exist for evaluating your immune systems reactions to food. But it has been shown time and time again that many of these tests are inaccurate, either under diagnosing, or over-reporting sensitive foods.
This makes it really difficult to know what to eat and what to leave behind. When a client’s test comes back with 30 reactive foods, it just leads to overwhelm for both the patient and the practitioner.
If your immune system is our planet, then your gut is like the water. Everything that you feed or put into the water is going to circulate, universally, affecting everything else on that planet. The air, the soil, the vitality of anything that grows. Knowing the foods that trigger decay and disease on your planet is essential to the overall health and vibrancy of your body.
You have far greater quantities of gut immune molecules, than you do in the entire rest of your body. Your gut immunity “scans” more in one day than is scanned by the systemic immune system in a lifetime!! Gut issues are so important to overall health, for this reason.
The truth is that food sensitivities are an underlying problem for every condition that I see.
And I mean everything:
- Arthritis
- Weight Gain
- Insulin Resistance
- Eczema, acne, and other skin conditions
- Fatigue
- Reproductive Hormone imbalance (PMS, PCOS, Menopausal symptoms)
- Infertility or recurrent miscarriage
- Autoimmunity of any kind
- Thyroid imbalances
- Adrenal issues
- Migraines
- Digestive issues ranging from IBS to Chrons or Ulcerative Colitis
- Depression, anxiety, insomnia, and brain fog
- and even addiction
Basically, any health concern where having increased inflammation would worsen symptoms or the disease process, can be worsened by exposure to foods that trigger your immune system. And inflammation is the bottom line in the vast majority of illness!
Even without illness or symptoms, anyone looking to live a long healthy life should run this panel, to prevent the development health issues later! I’m so excited to announce that it’s never been an easier or more reliable process to learn which foods are triggers for YOU! The FIT (Food Inflammation Test) by KMBO Diagnostics is cutting-edge lab testing that provides anyone who wants to rid their body of inflammation the information they need to avoid the foods that cause it! (***cut here for email, “read more”)
So, if it’s not an “allergy” what exactly is Food Intolerance or Sensitivity?
Hold up—let’s break this down a bit.
A whopping 85-90{0ace9f30246476cbe34912402cc70dd667071e9efa13e47cc458477e17894418} of our total immunity resides in the gut. There are several potential ways that you can have an immune reaction to a food. When we talk about Food “Allergy” and Food “Intolerances” or “Sensitivities”, these are very different things.
Our immune system is our bodyguard, working to protect us from “invaders” (like viruses and bacteria) that can cause us harm, 24/7. It works by tagging identifying proteins on the surface of the “invader” to mark it as a “bad guy” that should be attacked and eliminated.
Most of the time, this helps us. However, our immune system can also tag pollens, mold, toxins or chemicals, and other things we are exposed to. In the case of food allergies and sensitivities, a specific type of immune compound overreacts to the presence of a protein marker on the surface of a food molecule. The type of reaction is determined ultimately by type of immune compound that is doing the attacking in each reaction.
In a true food allergy, an immune compound called Immunoglobulin E (IgE) over-reacts to a certain food and causes a reaction within minutes or seconds. You can think of immunoglobulins like soldiers enlisted in our own personal immune army. Substances like egg, corn, or apples are normally harmless or healthy, but if you have an allergy, your body sees the food as a threatening invader!
In mild reactions, we might get histamine-driven symptoms like sneezing, runny nose, or itching, like with seasonal allergies. In a more aggressive reaction, you can develop hives, swelling, and even go into anaphylactic shock, which can be life threatening.
IgG is another type of immunoglobulin. IgG is produced by cells in the gut, in response to protein markers on substances like foods and bacteria. While IgE causes reactions within minutes, IgG causes reactions in 2 hours to 4 days or more!
Unlike true food allergy (IgE), IgG reactions are responsible for most of the symptoms that we associate with being “intolerant” or “sensitive” to a food. While the symptoms from an IgG response typically won’t include risk of death, they can still be uncomfortable and dangerous. For this reason, food intolerances are often dismissed as less significant, but in truth they can have serious consequences, especially with regard to your long-term health!
Food Sensitivity, leaky gut, and symptoms outside of the gut:
Logically, food intolerances can cause digestive symptoms. But how do these reactions cause symptoms all over the body like headaches or acne? If you have some degree of Leaky Gut, your immune system can react to the given food protein, forming immune-antigen complexes. When food proteins get through the gut lining, (through structures known as “tight junctions” in the intestinal wall), the resulting inflammation and immune activation causes further break down of the gut barrier. This in turn causes more leaky gut, and allows more food proteins in, creating a vicious cycle or increasing gut permeability and worsening food intolerances.
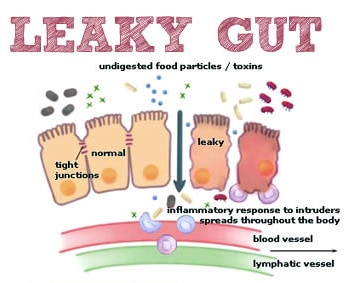
The over-activated immune system attacks local sites in the gut, but can also circulate in your bloodstream to tissues in distant locations around the body, such as joints, skin, your thyroid, or neurological tissue. Virtually any tissue in the body can be effected.
IgG-mediated symptoms can show up from 4 hours to 4 days after exposure to the reactive food. Clearly, this makes it difficult to identify what food caused what symptom!
Enter the FIT test!
The KBMO Fit Test is a revolution in food sensitivity testing. Like its ancestors, it still tests for IgG reactions to 132 different foods.

So, what’s so different and great about this test?
The main advantage that the FIT test offers, is that it screens for IgG types 1-4 (most IgG testing only looks at 1-2 types), and more importantly, screens for something called “complement”. When it comes to generating inflammation, complement is even more important than the level of IgG response to a food.
Let’s say that the initial IgG reaction is like the fire alarm going off at the fire station, and the first responders showing up at the scene. Compliment is like the rest of the squad showing up to help handle the situation…..they show up a bit later, but often create much larger hubbub at the scene of the accident or fire. The alarm (IgG) had to sound in the first place, to trigger the chain of events, but the responding teams (complement) were really what caused the biggest stir in the end. Foods that activate compliment can cause both local and systemic destruction of tissue by increasing inflammation.
In other words, you might have 10 or more foods with a significant IgG reaction, but the ones with complement are the ones that are significant in terms of boosting your inflammatory response. Knowing this information confirms which foods are most important to eliminate, instead of having a list of 40 foods to avoid! No other food sensitivity test currently available screens for IgG 1-4 and complement levels.
But there’s more…how the FIT Test can confirm if you have leaky gut
The FIT test is also a test for leaky gut, so you don’t need second test! If you show up as having a positive Candida antibody, it doesn’t mean that you have candida overgrowth. Candida is present in everyone’s gut, in low levels. A positive reaction to candida means that it is getting through the gut barrier, where it can present to your immune system. This confirms the presence of a leaky gut. The higher the reaction level, generally the worse the leaky gut. Having a high number of food reactions show positive (20 or more) also suggests leaky gut.
The best part is that this test is a blood spot panel. This means that we can mail it to you to do in the comfort of your own home– no blood draw needed! Based on your results, we design a 6-12 week elimination of your trigger foods, and then a systematic reintroduction to check for reactions. In most cases, antibody production in response to a given food will decrease or be eliminated within that time. When that happens, you may be able to reintroduce the food again without symptoms.
























