Meet Your Gallbladder: The Essential Detox, Hormone, and Digestive Organ Most People Know Nothing About
More than 600,000 people have their gallbladder removed each year in the U.S.
That’s like if every single person in Las Vegas had their gallbladder removed!
Usually, the gallbladder is removed because of painful gallstones. It’s treated as a totally normal, safe procedure with no side effects.
But that’s just not true...
Your gallbladder is actually a crucial part of your digestive, detox, and hormonal systems.
And even if you haven’t had your gallbladder removed, gallbladder dysfunction is becoming more and more common, and can cause symptoms like:
- Digestive issues (pain, bloating, diarrhea)
- Fatigue
- Skin congestion (acne, rashes, eczema, etc.)
- Weight loss resistance
- Hormone imbalance (PCOS, estrogen dominance, etc)
- Fatty liver disease
- And more
Today, I want to explore the role of the gallbladder, common signs and symptoms of gallbladder dysfunction, and steps you can take to heal and optimize your gallbladder function. Learn about hormone imbalance after gallbladder removal.
What and Where Is The Gallbladder?
Your gallbladder is a small organ that sits underneath your liver. Your liver makes bile (the digestive liquid needed to break down and absorb fat) and the gallbladder stores it, concentrates it, and then releases it to the stomach on demand.
The gallbladder plays key roles not just in digestion, but also in detox and hormone balance, as bile is needed both for clearing toxins from the body and for the healthy production of hormones, as well as hormone removal and balance. For that reason, the gallbladder isn’t just a digestive organ - it’s also a hormone and detox organ.
In Chinese medicine, the gallbladder is also attributed with governing decision making and qualities like inspiration, action, and assertiveness (think of the saying “they have gall!”). A strong gallbladder is associated with a quick return to normal after a physical or emotional shock. On the other hand, a weak gallbladder is associated with timidity or hesitation, and problems making decisions or following through. Finally, the gallbladder is also seen as a pivot, a turning point for new decisions and stages of life.
What Bile Does
Although it’s not sexy, the bile created by the liver and then stored, concentrated, and secreted by the gallbladder is one of the most important secretions in your body. Bile consists of ~95% water, in which are dissolved bile salts, bilirubin phospholipid, and cholesterol, primarily.
Here are just some of the many roles of bile:
- Bile emulsifies fat, increasing fat absorption. Bile is an essential “degreaser” and “emulsifier” of dietary fats. Bile is also essential for the utilization of the fat-soluble vitamins A, D, E and K. Bile deficiency leads to vitamin deficiencies.
- Bile prepares nutrients for assimilation in the small intestine. Bile takes food that has been acidified in the stomach and alkalizes it, allowing it to be broken down and absorbed.
- Bile assists in detoxification. Bile contains the conjugated toxins - carcinogens, xenobiotic chemicals, pharmaceuticals, heavy metals like mercury, aluminium and lead, and deconjugated hormones - from the 2 phases of liver detoxification.
- Bile helps modulate the microbiome. It acts as an antimicrobial, keeping the balance of bacteria in check.
- Bile transports excess cholesterol out. In doing so, it prevents cholesterol levels from rising too high.
- Bile lubricates the intestines and plays a regulatory role in motility, allowing food to go through the digestive tract a lot easier and preventing constipation.
- Bile prevents the formation of gallstones by breaking down fats before crystallization, and also digests and dissolves gallstones, which are composed mostly of cholesterol and particles.
- Bile triggers the release of glutathione, which is considered the “master” antioxidant, and helps eliminate bilirubin.
- Bile breaks down fats, and as such, is essential for weight loss!
- Bile controls the rhythm of the gut - the circadian timing of your gut motility is controlled by the gallbladder. Changes in motility (the time it takes for food to move through the digestive system) can lead to issues like Small Intestine Bacterial Overgrowth (SIBO).
The Gallbladder, Bile, and PCOS
The gallbladder’s role in hormone balance deserves special attention, especially in relation to PCOS (Polycystic Ovarian Syndrome).
Dietary fat and bile (to absorb it) are both necessary for the production of hormones. Even more importantly - bile helps your body excrete excess and used hormones, like estrogen. In addition, estrogen dominance (either as a result of hormone imbalance or due to supplemental estrogen, like birth control pills) are known risk factors for sluggish bile (the precursor to gallstones) and gallstones themselves. This is believed to be because estrogen causes an increase in cholesterol levels in the bile, which can then thicken and form stones.
Interestingly, research has shown that in PCOS, bile acid levels are actually significantly elevated, and that high levels of bile acids correlated with higher levels of testosterone levels, meaning worse PCOS.
The exact mechanism is not yet known, but it is thought to be related to sluggish bile, which is more commonly seen in those with hormone imbalance and PCOS. The sluggish bile raises levels of bile acids in the blood. There, the bile acids act on the Farnesoid X receptor, which has hormonal actions throughout the body, and can lead to elevated testosterone.
In addition to increasing testosterone, high levels of bile acids can also contribute to insulin resistance, another major issue in PCOS.
Bile and Leaky Gut
Bile flow issues or lack of bile can also cause or worsen leaky gut (increased intestinal permeability).
While leaky gut is often attributed to toxins produced in the gut or pathogenic bacteria living there, insufficient bile is another major cause.
One role of bile is to bind with toxins and help them be safely excreted from the body. But if there is inadequate bile to bind with the toxins, they can damage the intestinal barrier, allowing toxins and undigested food into the bloodstream… creating “leaky gut.”
Leaky gut causes widespread, multi-system issues and may even be a major part of triggering autoimmune disease. It is common in IBS (Irritable Bowel Syndrome), ulcerative colitis, Crohn’s disease, Celiac disease, and more.
Signs of Gallbladder Dysfunction
The most common type of gallbladder dysfunction is the result of slow or sluggish bile. This can be a result of not enough water (remember, bile is 95% water!), but can also occur when bile is oversaturated with toxins. The sluggish bile is more like peanut butter than water, and is too thick to flow freely.
In addition, the removal of the gallbladder, as well as other conditions, can lead to reduced levels of bile salts in the bile and weakened bile.
Symptoms of sluggish or weak bile include:
- Abdominal tightness
- Bloating
- Difficulty digesting fats
- Diarrhea
- Constipation (fat can build up in the intestinal wall and cause slow movement in the digestive tract)
- Trapped gas
- Bad-smelling gas
- Stomach cramps
- Gallstones
- Fatigue and malaise
- Fatty stool that floats or is light in color or grayish white
- Increase in allergies, chemical sensitivities, or food intolerances
- worsening PMS/Estrogen dominance…
- Hormone imbalances like PCOS
- Heartburn
- Erratic bowel movements
- Weight loss
- Signs of Vitamin A deficiency: Dry eyes, night blindness, red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks), and dry skin
Why Are So Many Gallbladders Removed?
Typically, the gallbladder is removed due to gallstones. Gallstones are crystallized masses of bile and cholesterol. Around 20% of females over the age of 40 have gallstones.
When gallstones become stuck in the duct of the gallbladder, they can cause pain and inflammation called cholecystitis. The most common treatment for gallstones is simply having the gallbladder removed. The surgeon then ‘“reroutes” the bile to go straight from the liver to the stomach.
Risk factors for gallstones include:
- Alcohol
- Excess reproductive hormones from supplementation or steroids (most commonly estrogen dominance)
- Oral contraceptive pills (birth control pills)
- High Endotoxin load causing sludgy bile
- Hereditary disorders like Gilbert's syndrome
- Thyroid issues or thyroid supplementation with T4
- Hepatitis
- Pregnancy
However, without the gallbladder, bile isn’t concentrated and lacks adequate bile salts - leading to the problems discussed above. That’s why gallbladder removal isn’t something you should just jump into.
Testing For Gallbladder Issues
If you suspect gallbladder issues, various tests can help pinpoint the problem:
- Blood test for cholesterol levels - if a person’s cholesterol production is low, bile production is also likely to be low. I look for cholesterol levels lower than 170.
- Digestive stool analysis - can help identify undigested fat in stool, which is caused by low bile availability.
- Bloodwork - to look for changes in serum bilirubin, alkaline phosphatase, serum glutamic oxaloacetic transaminase (SGOT), lactate dehydrogenase (LDH), aspartate aminotransferase (AST) and alanine transaminase (ALT). In early stages of gallbladder dysfunction, these levels might not change. However, functional medicine practitioners like me also use a more narrow interpretation of what normal is.
- A HIDA scan - this imaging test uses a radioactive material to measure the emptying function of the gallbladder, and can help diagnose:
- Gallbladder inflammation (cholecystitis)
- Gallstones, which can’t be seen, but can contribute to reduced flow or blockage to less bile flow if blocking
- Bile duct obstruction
- Congenital abnormalities in the bile ducts, such as biliary atresia
With my own patients, I use the ION panel by Genova (Organic Acids section) to evaluate the various pathways of liver detox and glutathione/antioxidant capacity. These results often illuminate when the liver or gallbladder are overburdened long before we see markers of pathology like elevated liver enzymes in labs. They also give more detail about exactly how the liver or gallbladder are compromised and can best be supported, in each individual.
Support for a Healthy Gallbladder
If you’re having signs of any gallbladder issues, step one is to get tested and find out exactly what’s going on.
In addition, here are some of the steps I turn to again and again with my patients:
- Switching out hormonal birth control (pill, patch, ring, etc.) for non-hormonal to reduce estrogen levels
- Supplements that support healthy gallbladder function
- Digestive enzymes and bitters
- Dietary changes: avoid excessive fried, fatty and greasy food and increase leafy greens
- Cut out alcohol
- Exercise regularly
In addition, addressing the emotional side of gallbladder health can be important. Try to express your emotion freely (journaling is an easy way to get started), address your past traumas (get help from a professional), and forgive.
And if you’ve already had your gallbladder removed? I can help you with strategies to support your digestion and hormones, even without your GB!
Want to learn more? Book a free 15 minute consult with my team now. It’s a zero-obligation opportunity to get a functional medicine opinion on your gallbladder health (and even if removal is something you should consider!).
P.S. Gallbladder issues are more common in women and those on hormones (like HRT or birth control). But if you catch gallbladder issues early on, you can avoid ever developing painful stones. Book a free 15 minute consult now.
The Real Cause of Premature Aging and Dull Skin
I’m not afraid to admit... I'm obsessed with good skin. After my work is done for the day and my daughter is asleep, going through my skin care ritual is how I wind down and relax.
And I know I'm not the only one… Skin care sales have skyrocketed in the last year.
But the truth is that there is a lot more to beautiful skin than expensive creams (or even an acupuncture facial… which I love).
Good skin starts inside… and if you’re having skin issues like dryness, sagging and premature aging… as a practitioner, that puts up major red flags. Today, I want to explore the internal causes of common skin issues.
Good Skin Starts Within
You’ve heard this before I’m sure, but in our current skin-care obsessed world, it bears repeating: the foundation of beautiful, radiant skin is your internal health and well-being.
Your skin care regimen can help, but if something is amiss internally, you’re going to see it on your skin and no amount of products can fix it.
There's actually a lot of good info on the internal link to acne. It seems like there is finally (!) some acceptance and understanding that acne is an internal issue, and usually related to hormones. (More on that here.)
But what most people don't know is that issues like premature aging, wrinkles, sagging skin, dryness, fine lines, discoloration etc… They all have an internal cause, too.
You’re not just getting old or overdue for a facial… there are real issues that could be causing these symptoms, and one of them is thyroid issues.
The Thyroid-Skin Connection
The thyroid is a butterfly-shaped gland at the base of the neck that produces key hormones for the healthy functioning of the body: triiodothyronine (T3) and thyroxine (T4).
Women are 8x more likely than men to develop a thyroid issue… and a key symptom of thyroid issues is changes in skin.
Thyroid dysfunction may present on the skin as:
- Dryness and dullness
- Rashes
- Premature aging (sagging, wrinkles, fine lines, loss of elasticity)
- Cyclical acne
- Facial puffiness
- Slow healing
- Hyperpigmentation
That’s because the hormones produced by the thyroid are responsible for growth, energy, and repair of cells of the body.
On top of these skin issues, thyroid dysfunction has tons of other subtle symptoms that you may have no idea are connected, like:
- Feeling cold, or having cold hands/feet
- Hair loss
- Sudden weight loss OR weight loss resistance
- Fatigue
- Constipation
- Trouble sleeping
- And more
How Your Thyroid Messes With Your Skin
Thyroid dysfunction can either present as an overproduction of thyroid hormones or an underproduction.
Hyperthyroidism is an overproduction of thyroid hormones and is less common. It is caused by the autoimmune condition Graves’ disease, in which the body attacks the thyroid gland. Symptoms include weight loss, sensitivity to heat, and higher heart rate. In the skin, hyperthyroidism can cause:
- Hyperpigmentation, like melasma, which is darkened patches of skin. This is caused by increased pituitary ACTH in compensation for cortisol being degraded and processed at an upregulated rate.
Hypothyroidism is the underproduction of thyroid hormones, and it is more common than hyperthyroidism. It can have many causes, including autoimmunity, which causes Hashimoto’s. Symptoms include weight gain, cold sensitivity, constipation, hair loss, fatigue, and these skin symptoms:
- Slow cell turnover: if your thyroid hormone levels are low, you will have a lower rate of repair of cells all over your body - but it is especially noticeable in the skin cells, which should have a fast turnover rate. This might present as skin taking longer to heal, dullness (as the old layer of skin hangs out too long), or dry and flaky skin
- Increased wrinkles and sagging: In those with hypothyroidism, a decrease was observed in type-IV collagen and hydroxyproline during the proliferative phase of wound healing. But collagen isn’t just for wound healing - it’s also what stops aging and sagging skin.
- Puffiness: less thyroid hormones cause increased polysaccharides, which causes more water to be held in the skin, and also lowers mitochondrial respiration efficiency, causing poor blood circulation. All this = puffiness.
- Hyperpigmentation: the exact mechanism isn’t well understood, but hyperpigmentation (dark marks and melasma) is also associated with hypothyroidism, probably due to reduced blood flow and slower cell turnover.
In addition to these, conditions like vitiligo and alopecia are also warning signs that the thyroid may be struggling.
Save Your Skin!
If any of what I just described sounds like it could be affecting you… here’s what to do next:
Step 1: Get Your Thyroid Tested
A specialized practitioner like myself or your general doc can order blood work to check for thyroid issues. But be sure to get a FULL thyroid panel: many docs only test T3 or T4, and exclude TSH (thyroid stimulating hormone).
I also recommend cortisol testing. Cortisol is the “stress hormone”and it is closely linked to thyroid function.
If you have mild thyroid dysfunction, just making some key lifestyle changes may be all you need.
For more severe thyroid issues, I highly recommend working with a trained practitioner (book a free consult with my team here.) Treating thyroid issues is multifaceted, and you likely don’t need to be on thyroid meds the rest of your life.
At-Home Ways To Support a Healthy Thyroid
- Switch to natural products, many of the chemicals - PCBs, Phthalates, BPA, flame retardants and more - used in conventional beauty and home products can actually harm thyroid health. Switch them out for natural alternatives. (There are so many great, clean skin care brands now!)
- Remove processed foods both to lower your toxin exposure and to give your body the nutrients it needs for healing
- Prioritize good sleep
- Detox if needed - especially consider your exposure to heavy metals, mold, parasites, and chemicals. Some of my favorite detox-supporters are saunas!
- Exercise to promote healthy cortisol levels
- Find healthy stress outlets
- Try ashwagandha - this herb can help manage cortisol levels
And if you have any signs of autoimmune-related thyroid issues, like Graves’s disease, or a coexisting condition like rosacea, alopecia, vitiligo, or eczema - you might need more specialized support and guidance. Consider booking a free consult with my team here.
Thyroid Tests Normal?
Thyroid issues are one potential cause of premature aging and other skin issues, but they aren’t the only potential underlying cause. If your thyroid function is normal, here are some other potential causes I would want to investigate:
- Leaky gut
- Oxidative stress
- Toxicity
- Genetic (but don’t worry -this doesn’t mean you’re doomed, just what you need to work with your genetic predispositions)
- Poor nutrition and lifestyle habits
And you might have several of these factors happening at the same time - that’s when working with an experienced practitioner who can tease it all apart and help you manage each piece becomes so valuable.
Get Help With Your Skin Health
If you’ve tried all the serums and moisturizers… and you’re still not happy with the way your skin looks, it might be time to dig a little deeper.
My practice specializes in working with women with gut, hormone, and fertility issues, and we’d love to support you, too!
>>>> Click here to schedule a no-obligation, free consult
How To Treat Depression & Anxiety Holistically - Part One
Butterflies in your stomach before a first date. Sweaty palms before asking your boss for a raise. Grief when your dog dies. Crying over a breakup.
These are all normal and healthy moments of nervousness and sadness.
But then there’s a shift….
Laying awake at night with a pit in your stomach… when tomorrow’s just another Tuesday. Overwhelming sadness when everything is going OK. A feeling of despair you can’t shake…
These are signs of a more serious issue: anxiety and depression.
If you’ve ever experienced anxiety or depression, you’re currently dealing with them, or are supporting someone you love with one of these conditions all you care about is getting rid of them.
But it’s not always simple. Anxiety and depression are multifaceted issues. And that’s where the problem starts.
Doctors and practitioners want to put you onto one 2 paths:
- Treat the brain. This is everything from antidepressants and anti-anxiety meds to talk therapy with a psychologist. On this path, anxiety and depression are seen purely as a mental health issue - so treatment focuses on your brain.
- Treat the body. On this path, anxiety and depression are seen as symptom of a problem somewhere else in the body. Treatment often focuses on changing your diet (especially avoiding certain foods) and adding in exercise.
This gets me so frustrated!
Like nearly EVERY health condition, depression and anxiety are not problems of JUST the brain or JUST the body. There is a definite mind-body connection, and the best treatments (and prevention) for depression and anxiety treat both.
In this series, I want to do some real talk about anxiety and depression. We’re going to dig into the root causes - everything from childhood trauma to candida - and the solutions that might be able to help you.
Nothing is off limits and I’m not going to vilify any one kind of treatment.
I hope this can be an open and honest discussion about anxiety and depression like you’ve never experienced before.
Trauma, Circumstance, and Perception in Anxiety and Depression
Before I dive into some of coexisting conditions I see around anxiety and depression (and the steps you can take to help treat it), I want to make a very important distinction. While I believe (and the research shows) things like compromised gut health and hormone imbalance can cause anxiety and depression, it’s not the case for everyone.
Trauma, circumstance and perception can all be root causes of anxiety and depression.
And even if eating a blood-sugar balancing diet DOES help you manage anxiety and depression, it doesn’t mean that your anxiety was just caused by eating too much junk food. The trauma was real. This is a very sensitive issue, so I want to make sure this is clear.
Here’s what I see a lot in my practice: when a woman has co-existing conditions like leaky gut or a hormonal imbalance, when trauma happens (and it happens to almost all of us to varying degrees), it’s more likely that the temporary stress of the trauma develops into the long-term problems of anxiety and depression.
How you perceive trauma is important too. What qualifies as a trauma to one person wouldn’t be for another person - and neither one is right or wrong. Your perception is YOUR perception. But, you can learn tools that can help change the way you perceive things.
(It’s the difference between seeing your mother-in-law’s comments as a personal attack against you or just a manifestation of her own insecurities that you can brush off.)
If you’re equipped with self-care practices and coping mechanisms before the trauma happens, you’re much more likely to avoid depression and anxiety.
This is where “treating the brain” is so important.
For those of you who are dealing with past trauma or very difficult circumstances, I’d suggest looking into EMDR and Brainspotting in addition to everything else I lay out in this post.
- EMDR is shorthand for Eye Movement Desensitization and Reprocessing. It’s a kind of psychotherapy that combines aspects of traditional talk therapy with eye stimulus. Research has shown it helps you process through trauma much faster than talk therapy alone (think the work of 8 years of talk therapy in just a few EMDR sessions). It’s a recognized treatment by the World health Organization, the Department of Defense, and the American psychiatric Association. Learn more about it and find a clinician here.
- Brainspotting is a therapeutic tool that can be used in conjunction with other forms of therapy. It works by accessing the autonomic and limbics within the central nervous system to help work through traumas - especially those that are not in the conscious mind (and therefore hard to talk about and treat). Learn more about Brainspotting and find a clinician here.
And I encourage everyone - whether or not they’re dealing with anxiety and depression - to get started on the inner-work that makes you more resilient to trauma. It can be as simple as beginning a meditation practice or finding a counselor.
A note on antidepressants and anti-anxiety medications: I believe antidepressants and antianxiety medications can be life saving for some people. They also have serious side effects and address the symptoms over the root cause. No one other than you and your doctor can decide if medication is the right step for you. But, whether or not you use medication as part of your treatment, I encourage you to explore treating the coexisting conditions and root causes I share about in this post.
Gut Health and Depression
When I hear about depression and anxiety, I immediately think about gut health. I rarely (I mean rarely!) see a patient with symptoms of depression and anxiety who doesn’t have some sort of gut health problems.
And intuitively, it makes sense. We feel our emotions in our guts just as much as we feel them in our mind - the “stomach in your throat” feeling, butterflies in the stomach, a “gut punch” when you get bad news, needing to go to the bathroom when you’re anxious or nervous.
We also know that 90% of the body’s serotonin is actually produced in the gut - not the brain - and that other important mood chemicals are made in the gut, too.
Irritable Bowel Syndrome (IBS) is also closely associated with depression and anxiety.
In my practice, I see 2 kinds of gut health problems contributing to anxiety and depression over and over again: leaky gut and candida overgrowth.
How Leaky Gut Leads To Depression & Anxiety
One of the most famous studies on gut health and depression was conducted in 2008: “The gut-brain barrier in major depression.”
This study is famous (and still cited all the time) because the researchers made some amazing discoveries.
First, they concluded that “There is evidence that depression is accompanied by an activation of the inflammatory response system and that proinflammatory cytokines and lipopolysaccharide (LPS) may induce depressive symptoms.”
In layman’s terms, that means:
- Inflammation is one cause of depression
- There is evidence that leaky gut may cause symptoms of depression
The study measured antibodies produced by the body’s immune system against lipopolysaccharides (LPS) in depressed patients and in controls (without symptoms of depression). LPS are large molecules of dead cell wall of the gram-negative enterobacteria - also called endotoxins. LPS should NOT be in the bloodstream. If LPS are present in the bloodstream, it means the tight junction of the gut have become loose (aka leaky gut).
The researchers found that the immune markers against the LPS bacteria in the gut were much higher in depressed patients than in the control group.
This means that the depressed group had more leaky gut and gut microbiome dysbiosis than the control group.
In fact, researchers concluded that patients with major depression should be tested for leaky gut. (And I’d argue, anyone with any symptoms of depression or anxiety - not just major depression!)
What causes leaky gut?
LPS are dead bacterial cell walls - and generally having high levels of them in the bloodstream indicates dysbiotic flora in the gut in addition to leaky gut. This can too much of the wrong bacteria, too little of the right bacteria, or too much or too little bacteria in the wrong place.
Leaky gut can also be caused by parasites, SIBO (Small Intestine Bacterial Overgrowth), yeast overgrowth (more on that to come), and untreated food sensitivities and intolerances.
Food sensitivity symptoms are usually an immune system response to foods we eat. The reaction creates inflammatory compounds that get into the bloodstream, circulate, and can create anxiety, brain fog, depresion, and fatigue.
Low nutrient status can also contribute to depression. When food isn’t properly absorbed in the gut (due to dysbiosis or leaky gut) the body doesn’t have the “nutritional building blocks” like amino acids, folate, vitamin B6 and more it needs to create the chemicals to control mood. This can cause depression and anxiety.
Yeast Overgrowth, Depression
Other than leaky gut, the most common gut health problem I see in relation to anxiety and depression is candida overgrowth. Candida is a kind of yeast that almost all people have present in their body. Candida is responsible for thrush in babies and yeast infections in women. In normal amounts it is healthy - but it’s when it overgrows that it causes problems. And the way candida impacts depression is especially interesting!
Candida is a yeast - which means it produces alcohol (ethanol) and acetaldehyde (the chemical responsible for the main symptoms of hangovers!) Both these chemicals are toxins to the body.
In a normal healthy person, (who hasn’t been drinking!), there should be little to no alcohol in the bloodstream. But if that person has an overgrowth of Candida, the alcohol produced by the yeast is entering the bloodstream - we call this “auto brewery syndrome” and it literally makes you drunk.
In a study conducted by doctors at Biolab in London, UK, a number of chronically unwell patients were tested for blood ethanol levels an hour after ingesting a sugar solution. The study found the patients consistently had high blood levels of ethanol which the researchers concluded came from small intestinal yeast overgrowth.
And - even worse - when candida is well established, it transform into the fungal form its branching (hyphae) “feet” can penetrate the intestinal wall.This creates literal holes in the gut, enhancing leaky gut syndrome and allowing more alcohol and acetaldehyde into the bloodstream.
What does that do to you?
Ethanol metabolism…
- Interferes with energy metabolism; this results in fatigue & muscle aches
- Causes hypoglycemia or "low blood sugar"
- Creates nutritional deficiencies
Then the ethanol is converted into acetaldehyde which…
- Is responsible for most of the symptoms of a hangover
- Causes dilation of blood vessels in the brain which result in the characteristic severe headaches
- Is toxic and inflammatory to the brain’s neurons
- Binds glutathione - the body's main antioxidant - thus increasing oxidative stress and allowing free radicals to damage cells throughout the body. Without enough glutathione, the liver can’t detox properly
- Increases the release of adrenaline, causing heart palpitations, anxiety etc. Panic attacks become more common.
What causes candida to overgrow?
All of these factors make your body more hospitable to the overgrowth of candida:
- Antibiotics
- Oral contraceptive pills
- High sugar/starch alcohol diets
- Stress
- Having other GI infections, or
- Having immunosuppression related to adrenal fatigue
Candida overgrowth can be treated - but the root cause that began the overgrowth must also be addressed!
Action Steps For Healing Gut Issues
The first step to healing gut issues is to find out exactly what is going on.
I don’t like to “guess and check.” For patients in my clinic, I always start with specific stool tests for parasites, dysbiosis, and yeast overgrowth. For SIBO, I test using a lactulose breath test.
Once we identify exactly what issues are occuring, we tackle them - treating parasites and pathogens, and then using diet and supplements to heal leaky gut. Gut mucosa heal rapidly when the aggravating factors are resolved! On average, my patients see big changes in as little as 3 weeks.
Coming Up: Hormones & Toxins
I hope reading Part 1 of this post has left you feeling empowered - and maybe even hopeful. If gut issues are contributing to your anxiety and depression, treating them can help you take a big step forward.
In Part 2 of this post, I’m going to address two other major factors in anxiety and depression: exposure to toxins and hormone imbalances. There’s still a lot left to cover!
I’m passionate about helping women uncover the root causes of their health problems and address them naturally. If you’re dealing with anxiety or depression, I’d love for you to book a free 20-minute root cause symptom analysis consultation with my team. These appointments are TOTALLY free, and there’s no obligation to book any further appointments. See what time slots we have open here.
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
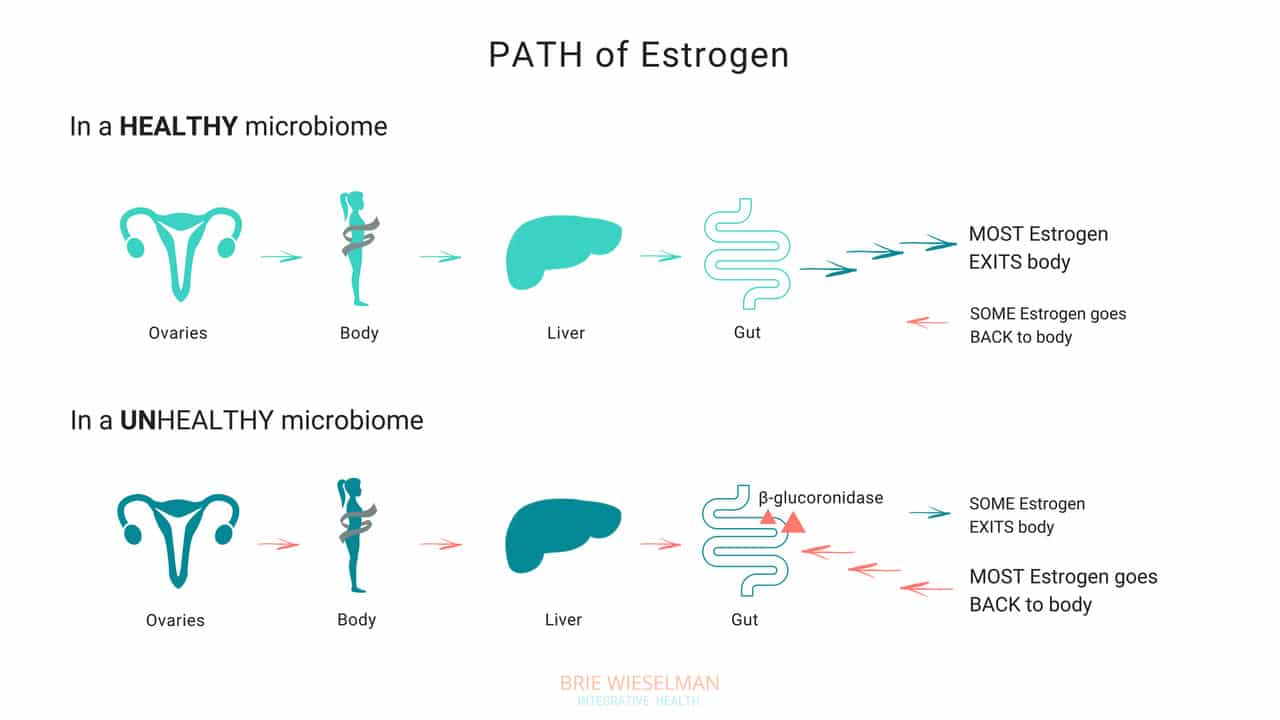
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.




