What Your Gut Is Trying To Tell You About Your Thyroid (+ Tests That Can Reveal The Truth!)
Everything is connected.
It’s one of my key beliefs in medicine, and when it comes to your gut health and thyroid problems, it holds true.
If you’re struggling with thyroid symptoms OR gut issues, I want to take a look at both… because where we find one, we often find the other! And if you only try to fix one issue, you’ll wind up spinning your wheels, unable to fully heal.
And if you’re facing a thyroid issue, this is ESPECIALLY true.
Today, I want to explain exactly how gut infections and thyroid health are linked - and what you can do to find and address gut infections to achieve better thyroid health.
You - Yes, YOU - Could Have A Gut Infection
No one wants to think they could have any sort of gut infection or parasite. First of all, there is the “ick” factor associated with parasites and infections. Just talking about it might make your skin crawl!
Plus, most people think that gut infections only happen if they are drinking “dirty” water or travelling to far-flung countries.
But that just isn’t true! Even in North America, Europe, and Australia, gut infections happen all the time! Even very clean and careful people can become infected when doing everyday activities - like swimming, gardening, or eating out. If you have pets, kids, like to hike or spend any time outdoors, and eat or drink ANYTHING… you’re at risk of a gut infection.
So don’t panic… we’re exposed to potential pathogens all the time! You can likely think of one you know you’ve had… food poisoning.
Plus, one of the most common infections is actually overgrowth of commensal bacteria or fungi - which just means bacteria that belongs in the gut naturally either overgrows or grows where it doesn’t belong.
That’s why I bring up the topic of gut infections and parasites with all my patients.
Gut Red Flags To Beware Of
If you come to see me as a patient, I look for these warning signs that could indicate some sort of gut infection could be a factor:
- Diarrhea
- Constipation
- Abdominal pain
- Vomiting
- Gas and bloating
- Ulcers
- Weak immune system
- Autoimmunity
- Extreme fatigue
- Nutritional deficiencies
- Brain fog
- Sugar cravings
- Depression
- Anxiety
- Joint pain
- Obesity
- Food intolerances – especially developing new sensitivities
- Skin conditions – such as psoriasis, rosacea, and eczema
Or, any of these conditions, either diagnosed or suspected:
- Intestinal Permeability (leaky gut)
- Chronic and Acute Gastroenteritis
- Inflammatory Bowel Disease (IBD - Crohn’s or ulcerative colitis)
- Irritable Bowel Syndrome (IBS)
- Autoimmune Disease
- Small Intestine Bacterial Overgrowth (SIBO)
And of course, anyone with any type of hormonal issues - but especially thyroid or sex hormones - gets a closer look, since gut infections and hormones are so closely linked.
These Are The Tests I Order...
Have some red flags? It’s time to test!
First up are stool tests. This is where I start for almost all patients.
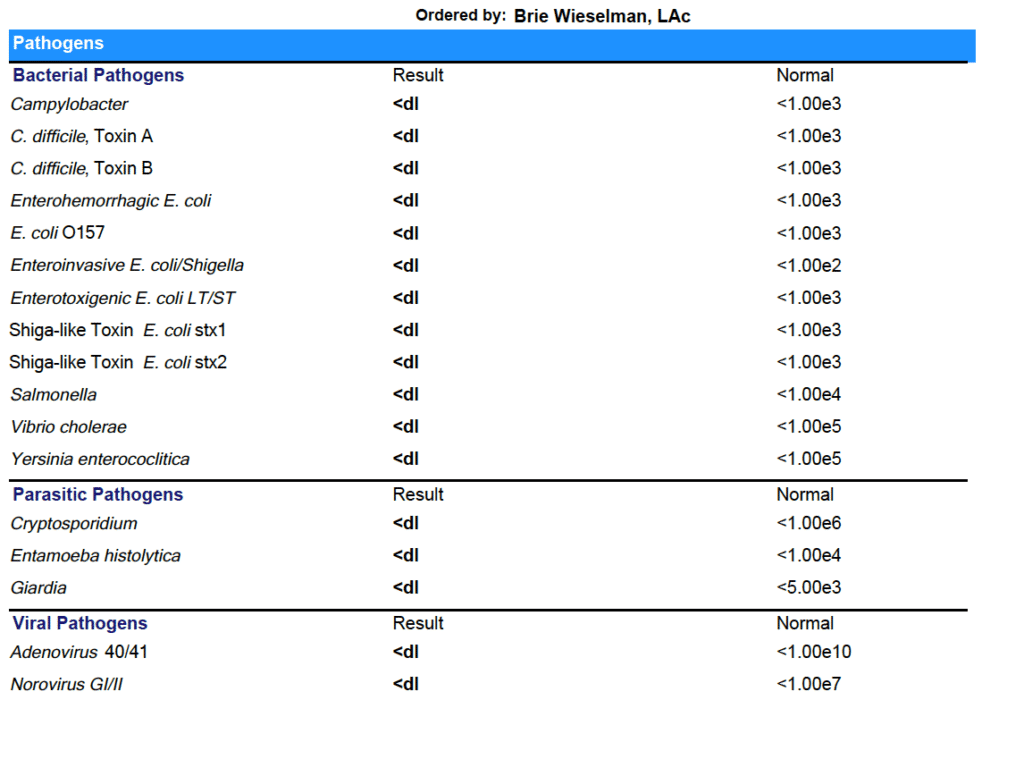
My personal favorite stool test is the GI Map.
Why do I like it? Compared to a regular stool test, the GI Map uses qPCR (quantitative) Technology, which is a more accurate way to detect and quantify organisms compared to more common culture, regular PCR, microscopy or DNA sequencing. qPCR works by amplifying and detecting DNA and RNA sequences, which is key because for results to be clinically meaningful, you need to know how much DNA is in the stool.
The GI Map test is also reproducible, which means that if you run it twice in a row, you get the same results - this is a key quality to look for in any diagnostic test. It’s used in research settings and it is the first pathogen assay that is FDA approved.
Other tests I like and sometimes use are:
- BiomeFx - this is a newer test that uses Whole Genome Sequencing to analyze over 25 pathogens measures their relative abundance as a percentage of your entire microbiome. This is different from traditional stool tests, which only look for any detectable number of pathogens present. While it isn’t uncommon to have a small number of pathogens present in your microbiome, the relative abundance in proportion to your other bacteria is what’s important.
- GI360 by Doctors Data
If you have constipation, diarrhea, gas, significant bloating or a history of food poisoning, I’ll also ask for a SIBO Breath Test.
If you have candida overgrowth symptoms like a history of antibiotic use, yeast infections, urinary tract infections or interstitial cystitis, chronic itching in groin, fungal toe nails, you’re reactive to yeast in foods, have been diagnosed with methane SIBO, have sugar or carb cravings, or stubborn weight issues, but the stool test doesn’t show candida, I will order Organic Acids, and/or Serum Antibodies to further suggest candida overgrowth treatment would be beneficial for you.
What Your Gut Test Results Can Reveal
Once I’ve got your test results back, the real fun can begin: interpretation and treatment!
But I don’t just glance at your results: I comb through all the details, connecting dots to put together a comprehensive picture of what’s happening with your health.
Here’s a peek at what I’m looking for in your test results:
Inflammation/Immune Markers
-
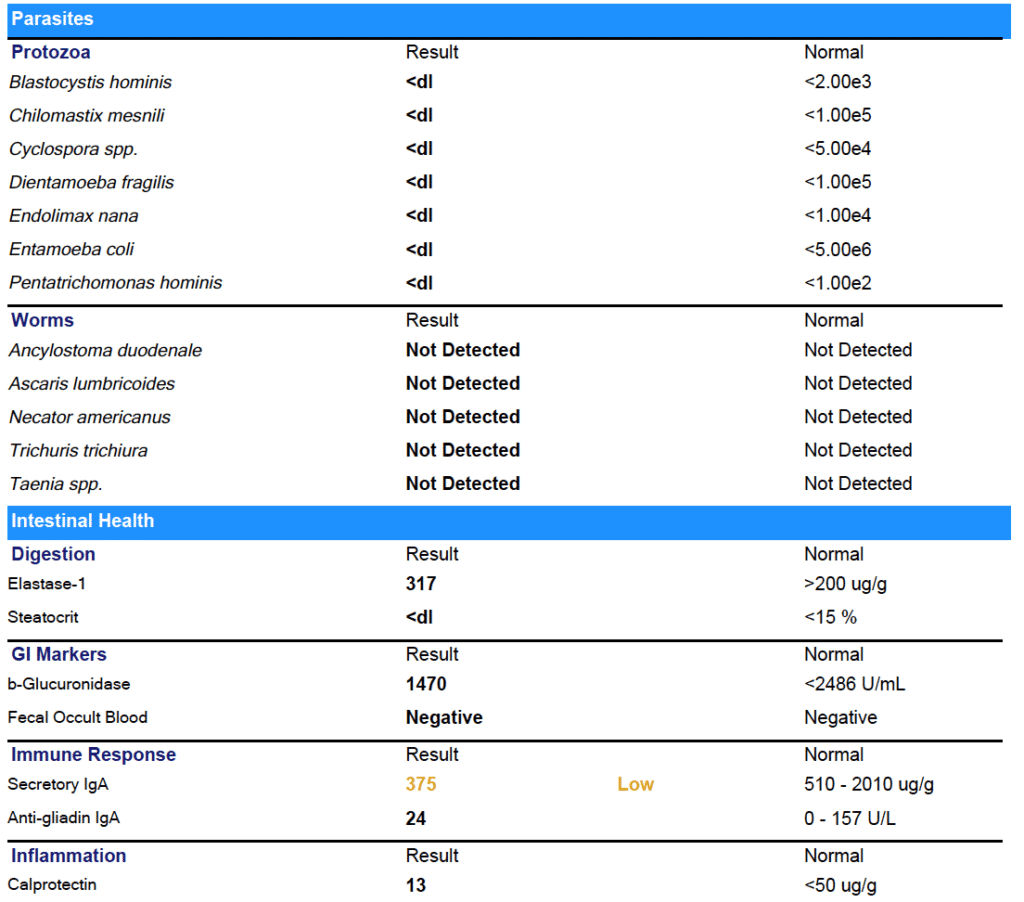
- Calprotectin - this is key for differentiating between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) (some tests also have lactoferrin). If below 120, it suggests infection, chronic NSAID use, or could be polyps, colorectal cancer or IBD. If above 120, it’s a sign of significant inflammation--which may be caused by an infection, but also generally receives a recommendation for referral to a GI doc if you’re working with me, as it can be suggestive of Celiac, or Inflammatory Bowel Disease such as Chrons’ or Ulcerative Colitis. (Gastroenterologists may suggest colonoscopy to rule these out when calprotectin levels cross a particular threshold). Each lab has a different range and sensitivity for calprotectin, so practitioners should use that lab's range. Should be rechecked at 4-6 weeks or after treatment.
-
- Zonulin - this is a keymarker of leaky gut.
-
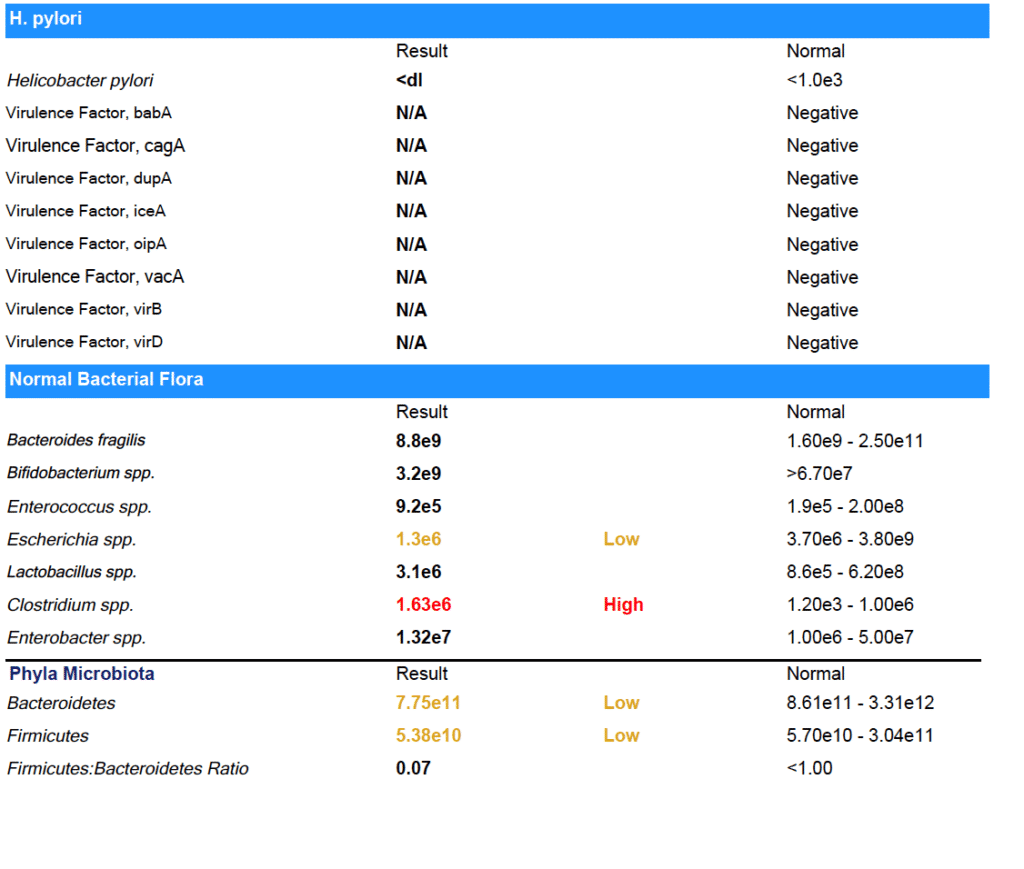
- SIgA - this is a marker of gut secretory immunity and barrier function and can show loss of resilience and tolerance. I look at this for signs of chronic infection, immune suppression, and/or adrenal hormone dysfunction.
Digestion and Absorption
-
- Pancreatic Elastase-1 - this marker reflects levels of pancreatic digestive enzymes present. There are many reasons why someone might have sub-optimal digestive enzymes, but regardless of the cause, we will want to supplement with enzymes at least in the short term.
-
- Fecal Fat - this is a marker of fat breakdown and absorption. If really low, it’s a sign a patient is not eating enough fat (<5%). If high, it indicates fat malabsorption/digestion. I’ll want to consider bile flow/production issues, enzyme deficiency, or SIBO.
-
- Short-Chain Fatty Acids and Beta-Glucuronidase - these are functions of the bacteria in the microbiome that reflects if good bacteria are present in adequate numbers or if less desirable bacteria are overpopulated. SCFA are the main fuel for cellular repair of the barrier membrane. High beta-glucuronidase can be a cause of estrogen dominance, and can also signal overall issues with not just the gut, but liver detox, depending on the level.
Microbiome
-
- Commensal bacteria - these are your “good bacteria” - and this also shows which bacteria are in low number, and which are missing altogether
-
- Parasitology - looking for infections like campylobacter, giardia, Blastocystis hominis, entamoeba histolytica, etc are present.
-
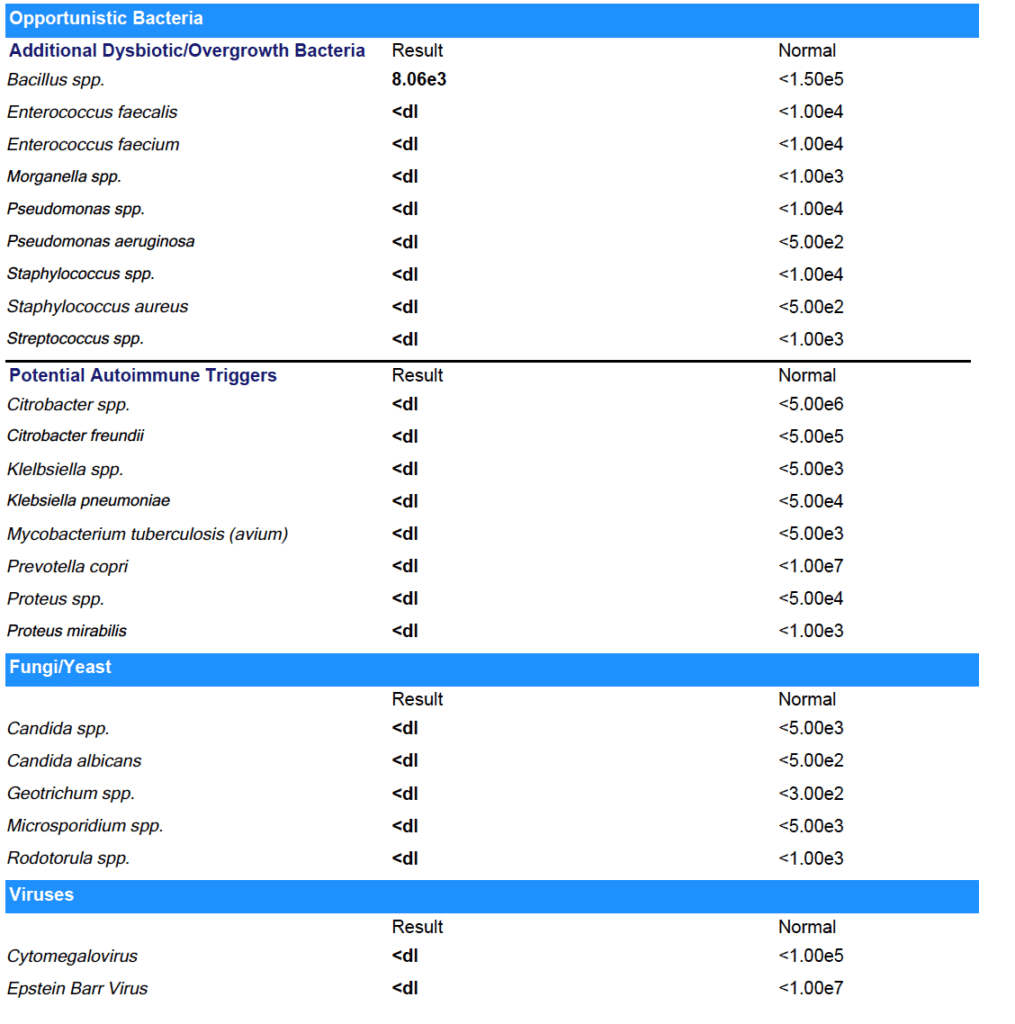
- Mycology - this clues me in to what fungi and yeast are present.
-
- Pathogenic bacteria - aka bad bacteria, or bacteria that can be either bad or good (like H Pylori)
-
- Worms - Yes it is gross, but it’s not the end of the world!
What Does All This Have to Do with Your Thyroid?
Let’s bring this all back around to your main concern: your thyroid!
Research has actually linked multiple gut infections to thyroid issues. Here’s a breakdown of some of the most common ones:
Blastocystis hominis
This common gut infection (often called Blasto for short), which is spread via contaminated food or stool, can cause symptoms including bloating, diarrhea, nausea, flatulence, variable bowel habits, abdominal pain, hives, and fatigue. Additionally, this pathogen is notorious for causing multiple food sensitivities.
It’s also linked to Hashimotot’s thyroiditis: people with Hashimoto’s are more likely to develop the skin condition chronic spontaneous urticaria (also known as chronic hives), as well as irritable bowel syndrome (IBS). And a study of 54 people in Egypt with chronic urticaria (hives) revealed that Blastocystis hominis was found in 61 percent of them, while only eight percent of the healthy controls had the parasite, suggesting that Blasto could be linked to hives, IBS, and Hashimoto’s.
Epstein-Barr Virus
Epstein-Barr Virus is a common virus best known for causing the disease mononucleosis.
Research out of Poland supports my informed hunch that it’s also linked to Hashimoto’s. A 2015 study done there found the virus in the thyroid cells of 80 percent of people with Hashimoto’s, while controls did not have the Epstein-Barr virus in their thyroid gland.
Yersinia Enterocolitica
This infection is often caused by consuming undercooked meat or drinking contaminated water. There is some evidence that Y. enterocolitica is associated with autoimmune thyroid disorders including Graves’s disease and Hashimoto’s thyroiditis in genetically susceptible individuals because higher antibodies to Y. enterocolitica are often found in these patients.
Helicobacter Pylori
This ultra-common infection/overgrowth, best known as a cause of ulcers, is also linked to autoimmune thyroid disorders. In a Korean study, those who were positive for H. pylori were significantly more likely to also have anti-thyroid peroxidase antibodies present.
Small Intestine Bacterial or Fungal Overgrowth (SIBO or SIFO)
Both bacterial and fungal overgrowth in the small intestine is linked to hypothyroidism - research has shown as much as 54% of people with hypothyroidism also have SIBO or SIFO.
These overgrowths can also deplete iron, which is involved in thyroid hormone synthesis.
In my own clinical experience, many of those with Hashimoto’s often have a high degree of yeast overgrowth and symptoms to go with it: gas, bloating, brain fog, sinus congestion, GI distress, itchy skin or scalp, eczema, vaginal yeast infections, and intestinal permeability.
Giardia
Giardia is another common parasite most commonly caused by drinking contaminated water. Some research has shown it can prevent the absorption of thyroid hormones in the gut, leading to hypothyroidism. (While I don’t have studies to support it-- just my own observation with my clients-- I suspect this could be true for any parasite or overgrowth causing inflammation in the gut, and not just Giardia.) But the good news is clearing the infection reverses hypothyroidism!
Connecting the Dots & Creating Your Treatment
With the right testing, you might finally be able to “see” what caused your thyroid issues - or is exacerbating them: a gut infection.
All the testing and interpretation brings us to the most exciting point: treating your gut issues, And with that information in hand, we can co-create a 100% unique treatment plan for you.
For my clients, I always create a custom protocol based not only on their test results, but also with their budget and lifestyle in mind. I don’t believe in a one-size-fits-all approach to medicine, which means if you have a strict supplement budget to stick with, or really, really, REALLY don’t want to give up a particular food, we try our best to find a way to work with it so that you get the results you want, within your parameters.
If you want to learn more about what it’s like to work with me as a practitioner, sign up for a no-obligation 15-minute Intro Session here.
This is your chance to share your story with my team and get a realistic look at what working with us is like.
>>> Book an Intro Session Here
I hope this information was helpful to you - and you can find tons more over at my blog: https://briewieselman.com/
- Brie Wieseleman, L.Ac
Are Worms The Next Frontier of Health? Everything You Need to Know About Helminth Therapy
I talk a LOT about clearing infections and overgrowths - Small Intestine Bacterial Overgrowth (SIBO), yeast overgrowth (candida), and of course, killing parasites.
So I was shocked when I first heard about a new treatment idea for treating disease and healing damaged gut: worm therapy. Not clearing worms. Giving them to the patient, to help heal disease.
No, I’m not joking. It’s called helminth therapy - named for the type of organism used Hymenolepsis Diminuta Cysticeroids (HDCs). HDCs are the larval form of a very specific type of worm that help to restore immune tolerance and diversity to the microbiome when it’s been damaged.
I was really skeptical when I first heard about this. But then I heard a presentation given by one of my medical heros, Dr. Sidney Baker (former faculty member of Yale Medical School, founder of Defeat Autism Now! and Autism360.org, Linus Pauling Award recipient) and Dr. Yehuda Shoenfeld at the Institute for Functional Medicine conference in May 2018.
They shared the latest research and their experience using helminth therapy - and I went from skeptical to excited. I slowly introduced helminth therapy in my own practice and saw amazing results.
Here’s what I want you to do: suspend all your judgement for the next 10 minutes and read the rest of this post. I promise you’ll be surprised by what you learn - and I bet you’ll want to learn more about helminth therapy.
HDCs Aren’t Just Any Worms
HDCs are the larval form (aka an intermediate life stage between egg and worm) of a small helminth. Helminth grows naturally in grain beetles, which were a common part of our food supply up until about 100 years ago.
HDCs are not a parasite. By definition, a parasite causes harm to an organism - HDCs cause no harm. HDCs stay in the gut - they cannot breach the gut wall.
Really important: HDCs cannot colonize in humans. That means they’ll never go from larvae to worm in a human. For that same reason, HDCs can’t be passed from human to human either. They’re NOT contagious from person to person.
Using helminth therapy is completely different from something like taking a tapeworm from Mexico. It’s produced in sterile lab conditions (just like probiotics are) and carefully controlled.
How Are HDCs Produced - And How Do You Take Them?
Therapeutic HDCs are grown in sterile conditions in a lab - much the same way probiotics or yeast for brewing beer or culturing yogurt are.
First, the eggs are grown in rodents in the lab. If that makes you squeamish, keep in mind that these animals are kept in MUCH more humane & clean conditions than most farm animals! Then the eggs are taken and are bred into larvae in grain beetles which eat only oatmeal. The HDCs are harvested from the grain beetles and suspended in salt water.
HDCs are given orally (again, just like probiotics!) through the salt water solution. You’ll take a tiny vial (about the size of the tip of your pinky finger!) that holds the microscopic organisms. If you hold the vial up to the light, you can just barely see the HDCs as tiny white flecks.
Unlike probiotics - which can contain billions of CFUs per capsule - HDC are given in very precise, small amounts: most people start with 10 HDC per vial and work up to 30 HDC. Strong, therapeutic doses of up to 100 HDC every 2 weeks can be used, too.
If you do ingest HDCs, they can only stay in your body for about 2 weeks.
How Does Helminth Therapy Work?
This is the part that’s really exciting:
Helminth therapy works by promoting microbiome diversity and restoring immune tolerance.
Remember - our body isn’t sterile. Our microbiome is teeming with important bacteria and other organisms that help it function: both flora (like probiotics) and fauna (beneficial things like HDCs). When the gut microbiome doesn’t have enough diversity of both flora and fauna it can’t perform its functions properly.
Our gut microbiome teaches our immune cells how and when to function and it establishes our intestinal barrier (which keeps pathogens out of our bloodstream). Our immune cells are our body’s defense team. Immune tolerance is what our immune cells won’t react to. It’s our body’s bouncer waving something through.
Immune tolerance is a good thing! It means your body won’t wage war on the strawberries you ate, or cause you to sneeze and cough when you’re outside around pollen.
If you have decreased immune tolerance, you’re more likely to experience these conditions:
- Allergies (both seasonal and to foods)
- Eczema
- Asthma
- ALL autoimmune conditions (things like endometriosis, multiple sclerosis, lupus, rheumatoid arthritis, vitiligo, Hashimoto’s, alopecia, ulcerative colitis, Crohn’s and more)
Today, 50 million Americans have been diagnosed with an autoimmune disease. That’s up from 9 million in 1997. (Still a huge leap even when you factor in increased testing/awareness.)
Experts like Dr. Baker and Dr. Shoenfeld agree: the best way to treat ANY chronic illness is to restore immune tolerance.
What Makes Our Microbiome Diversity & Immune Tolerance Decrease?
Up until the very recent past (like the past 100 years) our microbiome diversity was supported naturally by our environment. People interacted more frequently and directly with nature: farming, foraging, etc. They also had less hygiene practice: no antibacterial soap or hand sanitizer.
Worms - both beneficial ones like HDCs and pathogenic ones - were also something more people had when we lived hunter-gatherer lifestyles. (These persist in hunter-gatherer groups like the Hadza tribe today - and they have the most robust and diverse microbiomes of anyone known on the planet… and virtually no IBS, UC, Crohn's, diabetes or other autoimmune disease!)
Other things in the modern world that damage our microbiome diversity:
- Antibiotic use (kill beneficial bacteria in the gut)
- PPIs (impair digestion and promote bacterial and fungal overgrowth)
- Birth control pills (kill beneficial bacteria in the gut and promote yeast)
- C-section births (prevent transfer of microbiome from mother to infant in the vaginal canal)
- Vitamin D deficiency (too much time indoors)
- Chronic stress (go-go-go cultural attitude)
- Contaminated/nutrient poor food (Standard American Diet!)
- Excessive hygiene practices (overuse of antibacterial cleaning agents)
How To Restore Microbiome Diversity & Immune Tolerance
Diet has the biggest influence of all factors on the health of our microbiota. Less diversity in your diet = less diverse gut bugs.
Step 1 has to be eating a nutrient-dense diverse diet with plenty of gut-nourishing foods: fiber, healthy fats, and protein.
Making changes to your lifestyle & hygiene practices is important too:
- Put down the antibacterial soap!
- Get out in nature and interact with the earth
- Get adequate sunlight or supplement with Vitamin D
- Eat fermented foods or supplement with a high quality probiotic
But if you already have all these steps dialed in and are still dealing with symptoms of decreased immune tolerance or chronic illness, helminth therapy that can increase diversity and immune tolerance may be the next step for you.
What The Research Shows About Helminth Therapy (And Results in MY Practice!)
- In the largest randomized control trial in history (!), 1 million children in India were dewormed by researchers who hypothesized it would lead to an improvement in general health. Instead, they found no significant effect on weight, death rate, or health. This drew into question the premise that all worm are always harmful…
- In a 2005 study, 29 patients with Crohn's disease (most of whom were non-responsive to pharmaceutical treatments) were treated with helminth therapy every 3 weeks for 24 weeks. At 24 weeks, 79.3% of the participants had responded favorably and 72.4% had completely reversed their Crohn’s disease!
- In this 2014 study, people with IBD (either ulcerative colitis or Celiac Disease) were treated with either helminth therapy or a placebo for 12 weeks. Although this study was too small and too short to be conclusive, 10% of those who received the helminth achieved remission (compared to 4% in the placebo group).
In my own practice, I’ve seen these results using helminth therapy:
- Normalization of thyroid labs
- Remission of Crohn’s and Ulcerative colitis (when symptoms have already been improved and other co-infections addressed)
- Improvement of GI symptoms (diarrhea, constipation, gas, bloating, etc.)
- Reduction of arthritis symptoms
- Improvement of inflammatory symptoms like skin rashes, insomnia, and mood/brain issues
- Reduction of histamine intolerance symptoms
Other practitioners have reported improvement in children with autism and people with multiple sclerosis.
Who Helminth Therapy Is (And Isn’t For)
There’s no magic potion in medicine that will cure all your problems (i’m sorry!).
If you’re not eating right, moving, finding joy, and managing your stress, helminth therapy won’t work for you.
But if you’ve already got those “core” practices in place and are still struggling (or just want to see how good you can feel!), helminth therapy could be beneficial for you.
Typically people take 6 doses of HDCS 2 weeks apart to initially evaluate if they are or are not going to have a beneficial response. Then, if no benefit is seen, they can increase the dose for. Risk is almost non-existent, and the potential benefits are huge.
(But, anyone on immunosuppressive drugs - like those used in some types of inflammatory bowel disease or other autoimmune diseases - shouldn’t take HDCs. The helminth therapy is not beneficial if your immune system is suppressed by medication.)
What Do You Think?
I am so glad you stayed with me.
I know that “worm therapy” sounds really weird at first- but the idea of taking probiotics was once weird, too! I’m a supporter of anything we can do to improve our gut health - because our gut health radiates out into every aspect of our being.
Want to learn more about helminth therapy (and potentially give it a try?) - book a free 15 minute consult with my team where we can create an action plan for you.
Want to get healthier but NOT ready to try HDCs? That’s OK too - I’d love to teach you about how else you can support your gut. Book a free 15 minute consult with my team here.
What Working With A Functional Medicine Practitioner Is Really Like (Patient Case Study)
You’ve been to the doctor. He runs some tests and he says nothing’s wrong.
But you know you’re not you right now. Maybe you’re dealing with digestive problems that have taken the fun out of eating. Every dinner out is a potential threat.
Or maybe it’s your hormones that seem off. Your once predictable cycle is suddenly erratic. You feel like you’re in puberty all over again.
Or maybe you’ve never had a happy gut or healthy hormones. The doctors have thrown up their hands. They can give you The Pill or suggest you try a fiber supplement, but that’s all they’ve got for you.
You’ve always trusted your doctor - but right now it feels like there is nothing they can do to help you.
Where do you turn?
This story is how so many women end up looking for a Functional Medicine Practitioner. I know it well, because this is my story, too.
What Is Functional Medicine?
Functional medicine is an evidence-based approach to health that focuses on finding the root cause of health problems. Functional medicine looks at the body as one system - meaning that is something is “wrong” in one area of the body, it is likely having an impact on other parts of the body, as well.
Functional medicine incorporates both Western and Eastern approaches - the latest technology and ancient wisdom.
The #1 misconception about Functional Medicine is that it denounces modern medicine in favor of healing crystals and water fasts. Not true!
Listen, I won’t knock anything until I try it - including crystals and fasting - but the majority of work I do with clients in my clinic is much different than that. You might not know that though, because you’ve never seen a FMP before!
What Is It Really Like To Work With A Functional Medicine Practitioner?
Today, I want to walk you through the process of working with a Functional Medicine Practitioner. I’ll share one of our amazing patient’s own journey (yes - including test results!) so that you can understand what it’s really like to work with a FMP.
Before anything else, I always do a free 15-20 minute prospective patient interview. This is just a chance for us to connect (without any pressure) and be certain we’re a good fit for working together. From there we’ll go to official first step: the case review appointment.
The case review is like a deep-dive interview. I want to know as much about you as possible. I might even ask some questions about your childhood! Here I’m looking for clues as to the root causes of what is troubling you now.
Next, we’ll order some testing - depending on your unique symptoms and history. I don’t want to waste your time or money, so we’ll only order the tests that are relevant for you.
Once test results are in, we’ll meet again to develop a treatment plan. You’ll implement the plan (usually diet & lifestyle changes, plus supplements) and we’ll have check-ins to see how you’re progressing and if we need to make tweaks to the plan.
Finally, we’ll re-test to check your progress. (This is the best way to know treatments are really working.)
I’m excited to share this story with you - let’s dig in!
Step 1: Marina’s Case Review
Marina met with Amelia, one of the clinicians who works in my practice, in January. At her first meeting, we learned a lot about her!
She was 22 and was working as a paramedic with her local fire department. She wanted to become a helicopter medic (how badass is that?) but was struggling with health problems that were holding her back. Digestive problems and brain fog were zapping her of the energy she needed to go back to school.
First, Marina told us about what was going on right now: serious digestive problems. She was having oily stool, undigested food in her stool, and couldn’t tolerate eating meat at all unless she took her “meat pill” - a prescription anticholinergic medication. The digestive problems were wearing her out, and she was dealing with brain fog.
Then we went back in time: when did her health problems start?
Marina told Amelia that when she was younger, she had developed a cyst on her heart. Her doctors had treated it with back-to-back rounds of antibiotics.
As a side effect of the antibiotics, she developed neuralgias (a kind of nerve pain that causes severe pain) and vertigo. The vertigo led to 3 concussions in a row and she was ultimately diagnosed with a Traumatic Brain Injury (TBI).
It was at this time that the digestive problems started, too. Bloating, nausea, food intolerances, and fat malabsorption (which was causing the oily stool).
Her doctor told her the digestive symptoms were just Irritable Bowel Syndrome (IBS) and gave her the prescription for the “meat pill.” That was all he could offer.
6 years after the cyst on her heart, and Marina was still dealing with the repercussions of it. That’s how she came to see us.
Based on her history of antibiotic use and her current symptoms, we suspected Mishana was dealing with a gut infection. We suggested she start with a GI-MAP - a comprehensive stool analysis that can test for many gut infections at once.
Step 2: The Test Results Are In
Marina agreed to the test, and a few weeks later, results were in:
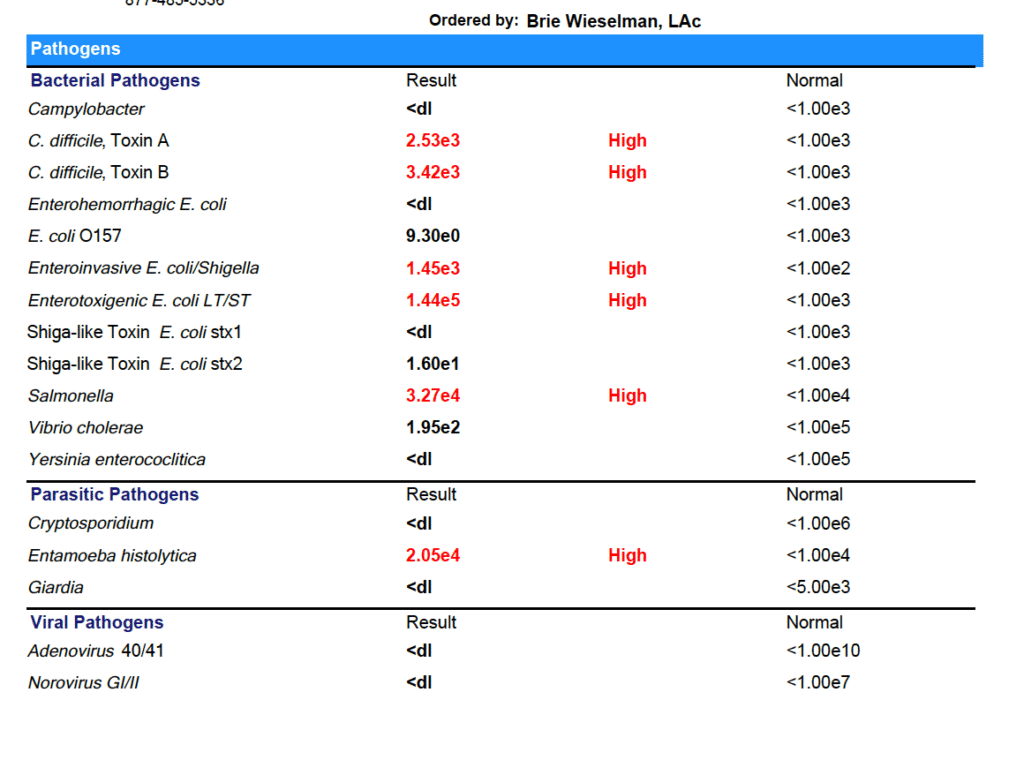
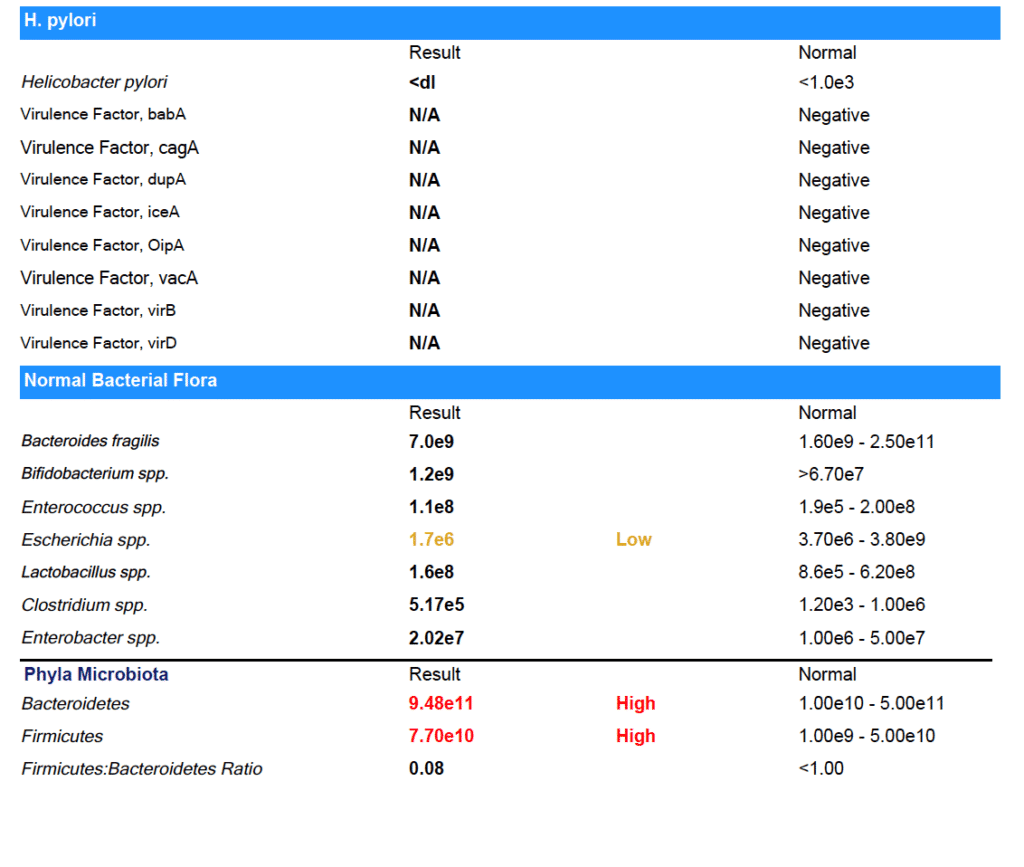
Marina tested positive for:
- C. difficile
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Salmonella
- Entamoeba histolytica
- Enterococcus faecalis
- Streptococcus spp.
- Candida spp.
- Chilomastix mesnelli
- With relative elevations in other markers
You might be thinking these test results are crazy - but it actually isn’t that uncommon! Even in the United States, gut infections and parasites are fairly common. And if you have used antibiotics or have a compromised microbiome for some other reason (like you’ve been eating the Standard American Diet) you are more susceptible to picking up gut infections.
Why don’t doctors test for these infections?
Some Western-medicine doctors do - but many others don’t. They either wrongly believe that gut infections are unlikely or they think they are “non-symptomatic” infections - meaning they don’t cause problems, and don’t need to be treated.
In my experience, (both personally and with my patients) clearing gut infections makes a huge difference in how you feel.
For Marina, we started treatment with a prescription anti-parasitic, alongside a natural bacterial protocol. After she completed those treatments, we used a prescription anti-fungal. Finally, we completed a re-seeding protocol with both probiotics and prebiotics (the most important step after any type of clearing treatment!).
After treatment, I always recommend re-testing to be sure that all the infections have cleared. Feeling better is a great indicator that infections have cleared - but it can’t replace seeing the results on paper!
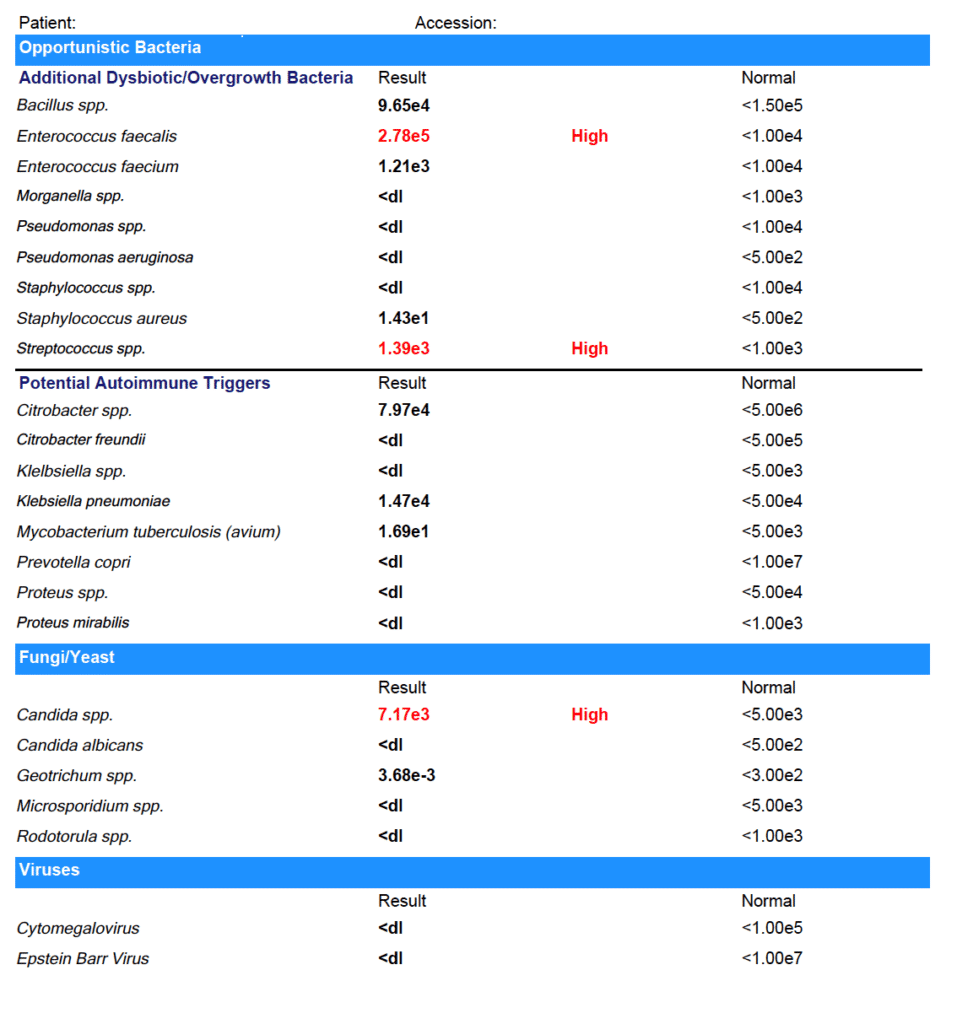
Step 3: The Second Test Results:
As you can see from the results - Marina was able to clear all her gut infections!
(Note: She did have some low beneficial flora that we worked on next.)
The results on paper back up what Marina experienced day to day: her digestion has improved. No more bloating or food intolerances.
Not just that, but after years of brain fog, Marina is finally thinking clearly again. She was even able to pass her paramedic cardiac program and enroll in medic school.
Now that the infections are cleared, Marina is working on improving her habits - especially around eating foods that support gut health and getting enough sleep - so that the infections don’t have a chance to come back. I’ll keep working with her to make sure she keeps improving.
It’s Black, White, & Gray
I like to say that I look for “black, white & gray” results with my clients.
I want the black and white stuff - the test results that prove the treatments we’re using are working. And I know those results are important to you, too.
But I also want the “gray” - I want to hear that you’re going out to dinner with your boyfriend and you don't get sick, that you’re finally able to be back in school, that you don’t have to press snooze five times every morning before you drag yourself out of bed.
For Marina, we definitely got the black and white and the gray - and I am so thrilled to see her thriving again after years of struggle.
I hope this has helped you understand what it really is like to work with a Functional Medicine Practitioner. And if you’re ready to take the next step forward in your health, I’d be honored to work with you. You can book a free prospective patient interview anytime here.
How I healed from 6 years of severe insomnia-- and you can too!
It is estimated that up to 50% of adults in the US are affected by insomnia, with up to 60 million having chronic sleep trouble. Twenty percent of Americans report that they did not wake up feeling refreshed on any of the past seven days. These numbers are staggering, when you think about the incredible number of studies proving that adequate, good quality sleep is essential for disease prevention, mood, and brain function.
I went through a time in my 20’s where I simply couldn’t fall asleep. For hours, I would lay awake, tossing and turning, getting angry and frustrated at my increasing alertness. After a while frustration would turn to worry….. “how am I going to function tomorrow….I need to be up at 7 to make it to work/class/etc”, “Am I ever going to be able to fall asleep naturally again in my life?”
I seriously believed that I had forgotten how to do something that I had taken for granted my entire life up until that point. To just. Go. The. F. To. Sleep.
Sleep Matters
When my clients mention that their sleep is less than optimal, I take it seriously. No matter what the main health issue is, if you aren’t sleeping well, the body and mind just can’t repair fully. Lack of sleep makes us inflamed, stressed, shifts our hormones for the worse, and impairs blood sugar balance. Our levels of patience, concentration, and creativity suffer. That word or name we are grasping for remains elusive as we struggle to communicate our thoughts.
Studies show that we tend to make poor food choices the next day. Poor sleep can even lead to weight gain, without a change in diet. Difficulty falling asleep, or staying asleep, inevitably leads to being less than fully awake and refreshed during the daylight hours— for years; I felt like I was half of myself. And that’s no way to live.
Finding My Root Causes
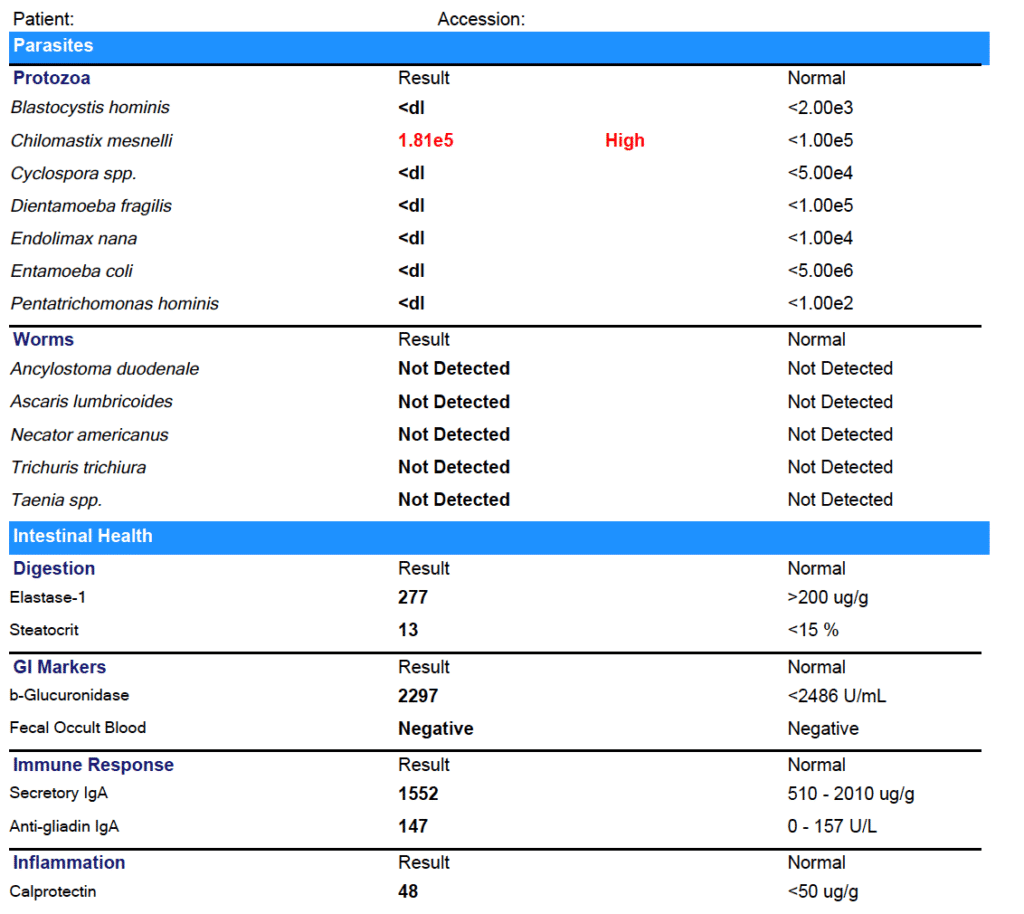
Resolving my insomnia required a pleiotropic (multi-faceted) approach. Testing and supporting my adrenal hormones was the first step:
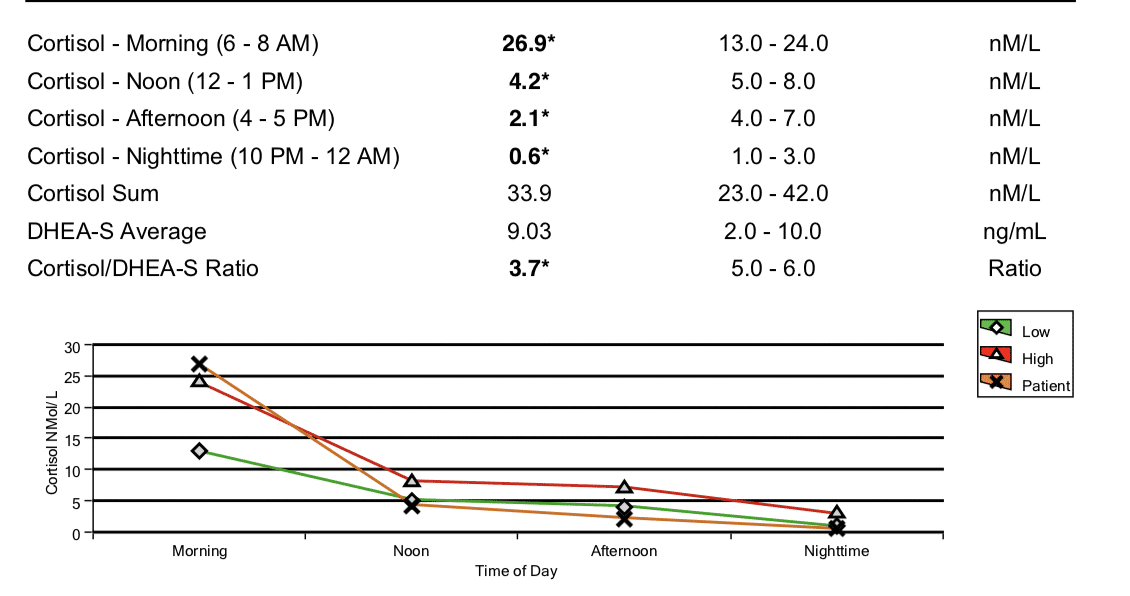
(This is a saliva panel from before I used the DUTCH Adrenal test for assessing the HPA axis in my practice. You can see that my morning cortisol was super high right when I woke up, suggesting that it had been high at night.)
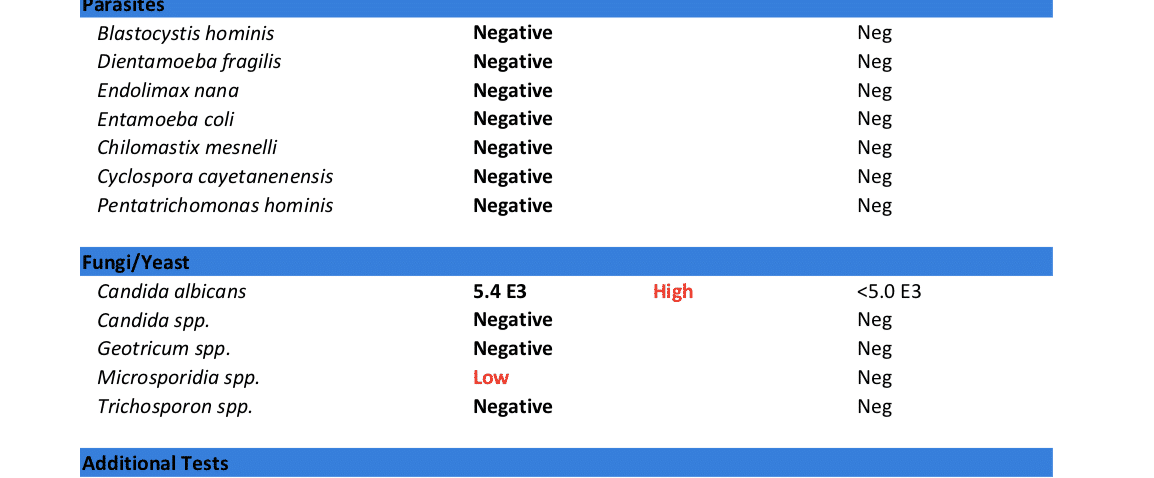
However, it turned out that I also had three parasites and candida overgrowth causing inflammation, which had to be addressed before my adrenal hormones and bio-rhythms could repair. (And this was despite not having many digestive symptoms at the time!)
Test 1
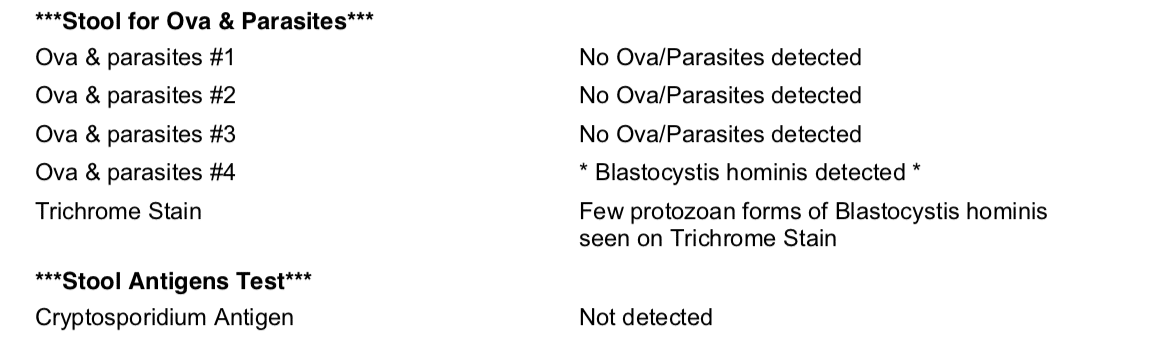
Test 2
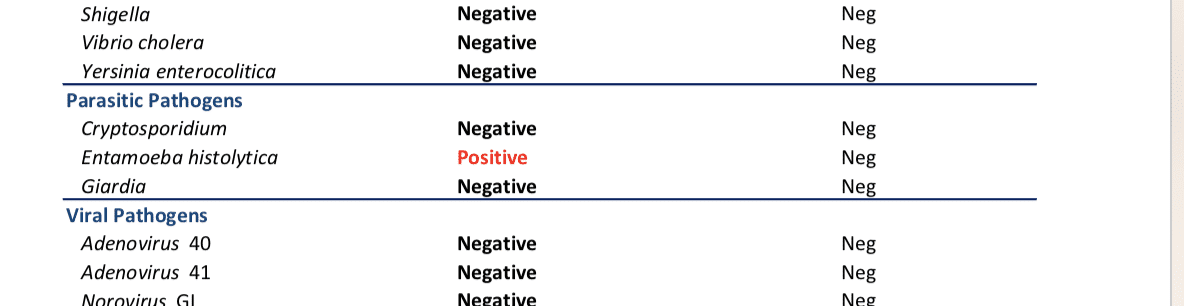
Test 3
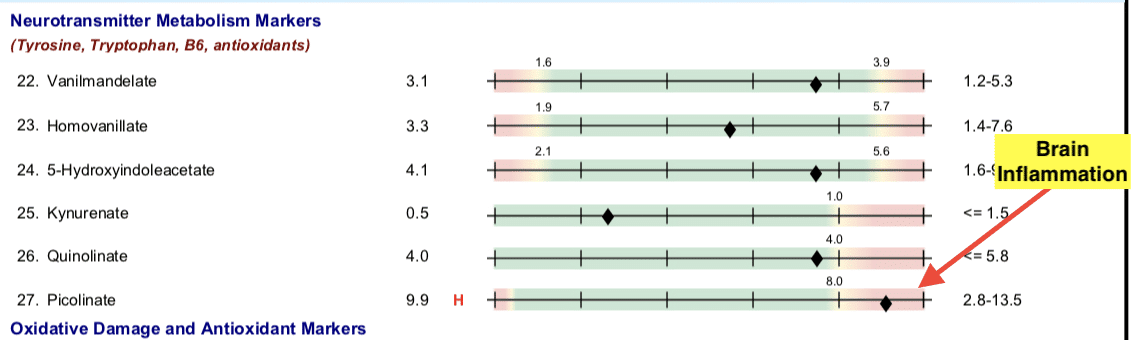
The inflammatory compounds from parasites and yeast in my gut, were neurotoxins. Exposure to these in my bloodstream was creating inflammation and oxidative stress in my brain that contributed to sleep and memory problems.
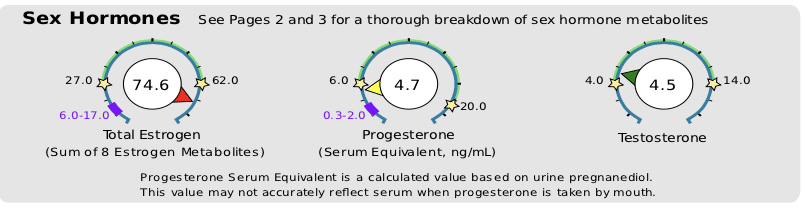
And my progesterone levels were lower than my post-menopausal grandmother’s would have been! (Progesterone production takes a back seat to cortisol production when your body is reading that you are under constant stress... *or inflammation).
To make things worse, my estrogen was through the roof. This relative excess of estrogen to progesterone is called Estrogen Dominance , and can make life in a woman's body fell like...well...a pain in the ass! (Think PMS, breast swelling and tenderness, heavy menstrual bleeding, fibroids and cysts, or weight gain around the hips and thighs....oh, and did I mention insomnia?)
Addressing each of these issues, over a period of about a year, gradually brought about a shift in my insomnia. Even after the first month of treatment, sleep started to come easier and easier. And it just got better and better from there. I felt like I had gotten my life and myself back!
5 Steps to better sleep
Modern life, with our artificial lights, tablets and screens, digital notifications, and indoor living give our bodies the exact opposite of the signals we need to promote sleep. While testing and treating these or other underlying causes for any case of insomnia may be necessary in the long run, we just can’t “out-supplement” diet and lifestyle.
Taking steps to set yourself up for success during the day, and early evening, is essential for anyone who’s sleep is less than optimal. There are many things you can do on your own, to give your body and mind every chance of sinking into a deep, restful sleep, naturally.
Sleep Tips
Sleep is one of the most important aspects of improving hormone balance and repairing body systems, from the brain to the digestive tract. Here are additional tips to facilitate this process:
Tip 1: Train the brain to feel sleepy & awake at regular times:
- Set fixed times for bedtime and rise-and-shine- As much as possible, keep to this schedule, even on weekends, regardless of how much sleep you got the night before.
- Avoid daytime naps- as this reduces your sleep drive at night.
- Keep the lights off -If you have to get up during night to use the bathroom do not turn on the light. Use a small nightlight so that you can see enough to move safely.
- Sunlight Exposure- get at least 30 minutes per day, sunglass free. Even in a cloudy sky, the natural spectrum light is bright enough to trigger your brain with a powerful signal that it is daytime. Natural light exposure helps establish healthy sleep/wake hormonal rhythms—it has only been recently that we’ve spent the majority of our lives indoors, under artificial lights. It’s essential to do this in the morning, within the first hour of being awake. For any kind of insomnia, it’s best to wake and go to bed at the same time every day. However, if you wake at 7 AM most days, but 9 on weekend, set your daily time outside to be 9:15-9:45 to ensure consistency, grab a mug of tea, and head out the door.
Tip 2: Develop a strong mental association between your bedroom & sleep:
- Use the bedroom only for sleep (or sex)- don’t read or watch TV in bed.
- Get into bed only when you are sleepy- If you are unable to fall asleep, get up and go into another dimly lit room, rather than lying in bed awake.
Tip 3: Avoid being over-stimulated at bedtime:
- Avoid Alcohol – it may help you fall asleep, but all the sugar in the alcohol will cause a rapid rise and subsequent drop in your blood sugar which will cause you to wake up. Even low-sugar alcohols like vodka can disrupt your sleep pattern, causing lighter sleep or frequent waking. Avoid alcohol within 3 hours of bedtime, and avoid it completely if you are struggling with insomnia.
- Ditch the Caffeine- Did you know that even a morning cup of joe at 7 AM can disrupt your sleep? This is especially true in people who have genetic caffeine processing issues, due to gene SNPs such as COMT. The “caffeine kick-back effect” is more common than you would think! Avoid caffeine completely if you are having sleep problems. Avoid it after 2 PM as a general rule, even if you don’t suspect you are overly sensitive to its effects.
- Slow Mental activity -stop doing active mental work at least 1 hour prior to bedtime. This includes surfing the web, watching Netflix or movies, emailing, Facebooking, or texting. We all need wind-down activities to switch out of “doing” and “problem solving” mode. Earlier in the evening, meditation, yoga, books, audiobooks, and yes, at the very least, even watching a TV show or playing a game on your Ipad is fine (assuming you are using precautions to avoid blue-light listed below)—anything that helps you switch into relaxation mode and away from the whir of thoughts and pace associated with wakefulness.
- Get Moving!- Exercise at least 30-60 minutes every day. Even walking works.
- Avoid Blue light Exposure— Have you ever noticed that the light near the end of the day, around sunset, is naturally warmer with more reds and pinks? Blue light from screens inhibits melatonin production by signaling that it is day time. Our brains respond to dimmer light and warmer light by winding down activity, but you need at least 2 or more hours of these lighting conditions prior to bedtime for optimal relaxation.
- Install apps on electronic devices that dim blue light and use warmer spectrum tones, such as f.lux on Mac, Nightshift for iPhones, or Twilight on Android.
- Dial down the brightness on dimmer lights, screens, and digital devices.
- These apps do a fairly good job, but if you are more sensitive to light and the apps don’t cut it, also consider buying a pair of blue-blocking glasses (around $10-15—-yep, these come in a ton of super-groovy styles now that they’ve caught on). Some people even install amber-colored light bulbs such as these around the house.
Tip 4: Create an environment supportive to sleep.
Your room should be:
- Dark- cover LED lights on bedside clocks, consider blackout blinds. An eye-mask with cup shaped or curved nose pieces can work just as well.
- Cool- Your body naturally cools off when you sleep, and if your room is too hot, it can be hard for your body to give off its heat. Around -65°F is ideal for most people.
- Comfortable- use a comfortable mattress and pillow that is supportive to your neck, depending on your sleeping position. Consider using a “side sleeper” pillow for under your neck when sleeping on your side. Consider using a body pillow to hug and put between your knees to align your back and shoulders at night. I personally love the PharMeDoc C-shaped body pillow for side sleeping as it supports both neck and hips. Yes, it is marketed for pregnancy (and is a must have for pregnant women!)—but it’s great for non-pregnant people who like to sleep comfortably too!
- Quiet –Some people swear by reusable silicone earplugs like these for the best noise cancellation. I prefer the super soft foam kind so they aren’t uncomfortable. You can use them several times before they lose their “squish” and look a little grubby—then toss ‘em and grab a new pair. These plugs block out even my husband’s snoring on the loudest night!
- You can also use a white noise machine, if you don’t like the feeling of having something in your ears. Different people prefer different sounds. I don’t use one of these, but patients have told me good things about them.
Tip 5: Eating for healthy sleep
- Stop Munching- avoid being too full at bedtime. No food for at least three hours before sleep, unless you suffer from severe hypoglycemic issues.
- Don’t Under-eat: Hunger and low blood glucose can give you insomnia and can wake you up in the middle of the night. Most people’s bodies naturally help them to eat the right amount, but if you’ve been intentionally trying to lose weight, or restricted eating because of digestive or other health issues, your appetite signaling can easily get off, and so can your sense of what is enough food. If you’re not sure that you’re eating enough try this:
- Use an online calculator like this one to figure out your approximate caloric need.
- Use a food tracking app such as MyFitnessPal to keep track of your calories for a few days.
- If you’re under-eating, bumping up your calories may be the silver bullet solution to help you sleep deeper and fall asleep easier.
- Eat high nutrient foods, especially minerals: Mineral deficiencies (like calcium, magnesium or potassium) are a common factor with insomnia. The best way to ensure high nutrient content is to eat a variety foods each week, including fruits, lots of above ground veggies, root veggies and tubers of different colors, animal proteins, liver or other organ meat, seafood, and bone broth. If you don’t eat dairy be sure to get plenty of calcium containing leafy greens, and or herbs that are high in calcium to supplements, Many people need supplemental magnesium as well. Even on an otherwise healthy, whole foods, Paleo type diet, you can still have deficiencies of essential nutrients if you are eating the same foods day in and day out.
- Eat enough carbs: Carbs are super important for sleep, in several ways.
- You need dietary carbohydrate in order to produce melatonin in your brain. Melatonin counters cortisol, among other things. Without enough melatonin in your brain, sleep isn’t happening!
- People with Adrenal Fatigue may have insufficient cortisol levels to stabilize their blood sugar for long periods of time. I notice that people with low cortisol often suffer on low carbohydrate diets, because their body can’t shift into carb generation mode in the liver (which is where your body sources stored carbs between meals). When your blood sugar drops while you’re sleeping, adrenaline kicks in and you wake up out of a dead sleep, wondering what is going on. To avoid this, consume more of your carbs at your evening meal, close to bed time.
- Each person’s carbohydrate need varies widely based on activity level and baseline metabolic rate. It can also differ at different phases in life. Depending on age, gender, activity level, pregnancy status, and weight maintenance goals, people need anywhere from 50-350 grams daily. With sleep difficulty, I recommend that my clients not go below 75 grams daily. The only way to know what is right for you is to experiment and observe.
- Again, take activity level into consideration —if you are training for a triathalon, 50 grams per day is simply not going to cut it. If exercise looks like a walk to the mailbox daily, you aren’t going to need above 150 grams. Adjust these levels until you find the right fit for you.
Tip 6: Develop An evening ritual helps prepare your body/mind for sleep.
Here are some possibilities to choose from:
- Journal- If you are someone who lays awake thinking of your to do list, get it all out on paper before-hand. Planning for the next day by writing a brief list can help short-circuit the mental spinning. Alternately, write down what you are grateful for that day, or journal. Consciously release and hurts or resentments you are feeling.
- Have a cup of herbal tea (e.g. “Sleepy Time”)
- Have a bath with Epsom salts—start with 1 cup in a warm (but not overly hot) bath. Add relaxing essential oils like lavender, chamomile, sandalwood, or vetiver if you enjoy these.
- Use a diffuser in your bedroom & use lavender essential oil before bed.
- Do some gentle stretching, or yoga. I personally love using my foam roller to roll out kinks and knots.
- Try progressive muscle relaxation--this has been shown to help reset cortisol rhythm. There are many version of this available on Youtube, such as this one.
- Do “4-7-8” breathing:
- Breathe in through nose for 4 counts
- Hold your breath for 7 counts
- Exhale through mouth for 8 counts
- This combination of count ratio slows heart rate and relaxes the sympathetic nervous system.
Do the same ritual every night, as you are training your body and mind to unwind from the day and giving it the message that it’s time for sleep.
Tip 7: Supplement Support:
Ideally, supplements should only be used after the above steps are being taken consistently. But tossing and turning night after night can really put a damper on your mood, not to mention your glucose control, sugar cravings, weight, hormone balance, and overall health. There is no one sleep supplement that works for everyone, and these are just several recommendations that are generally safe for people to experiment with on their own.
If you are still struggling, work with your practitioner to identify key issues that are at play with your insomnia, such as hormone imbalances, parasites, inflammation, neurotransmitter issues, toxicity, sleep apnea, or other causes.
Consider:
- L-Theanine- 200-400 mg
- Magnesium- up to 1200 mg, in divided doses daily. Use the chelated forms for best tolerance.
- Liposomal CBD- 1ml-4ml before bed.
- Calming Herbs – Lemon balm, Passion flower, Valerian root (like this blend)
Looking for further help with improving your sleep? We'd love to help you!




