Insulin Sensitivity and Gut Health—A Dynamic Duo
Do you want your skin to look smooth and youthful for as long as possible?
Do you want your brain to be sharp?
What about losing weight and maintaining a slender, sleek body?
These are just some of the reasons to care about keeping your insulin and blood sugar levels balanced—even if you don’t have prediabetes or diabetes. Yet, when many people hear about insulin sensitivity they think it’s only relevant to diabetics.
That couldn’t be more wrong.
There are good reasons for everyone to care about how their body is handling insulin. And surprisingly, it’s your gut that plays a major role in keeping this blood-sugar-balancing hormone in control.
If your gut is unhealthy, your body won’t handle insulin well, which means your blood sugar will get out of whack.
What Is Insulin Sensitivity?
Insulin is a hormone that’s made when our blood sugar (glucose) levels rise. It pushes extra glucose into the cells of our muscles and liver, where it’s stored as glycogen. But when our muscles or liver run out of closet space to store the glucose, the excess is converted into fat and stored in our fat reserves.
When muscles and the liver run out of glycogen they should be able to tap into fat stores to replenish themselves, causing weight loss.
However, if insulin is present in excess amounts, it blocks your body from tapping into those reserves.
What causes high insulin levels? Usually the culprit is high blood glucose in the form of glucose spikes that often happen even in people without diabetes.
Insulin sensitivity refers to the body’s ability to respond to the blood-sugar-lowering signals that insulin is broadcasting. If the body can’t respond to those signals, it starts making more and more insulin to try to “hear” what insulin is saying. Kind of like talking louder when someone can’t hear you. Reduced insulin sensitivity is known as insulin resistance. In other words, your body isn’t as sensitive to insulin anymore so it needs to make more and more.
Why You Should Care About Insulin Sensitivity
Poor insulin sensitivity and glucose spikes are to blame for a number of health problems, not just diabetes. For example, they’re linked to:
- Accelerated skin aging and more rapid development of wrinkles
- Acne and other inflammatory skin conditions
- Adrenal stress
- Arthritis and other inflammatory diseases
- Cravings
- Depressive episodes
- Digestive symptoms like leaky gut, heartburn, acid reflux
- Fatigue/chronic fatigue
- Heart disease
- Increased cancer risk
- Increased risk of Alzheimer’s disease and dementia
- Infertility and polycystic ovary syndrome (PCOS)
- Memory problems
- Migraines
- Non-alcoholic fatty liver disease (NAFLD)
- Poor sleep (waking during the night)
- Suppressed immune response
- Type 2 diabetes
- Worsening of hormonal hot flashes and night sweats
How The Gut Controls Insulin Sensitivity
Problems in the gut lead to problems with blood sugar and the way your body uses insulin. Usually people don’t connect the gut with insulin problems, but there is a HUGE connection between the two.
Here’s the deal: The gut affects insulin sensitivity in five ways. Some of these might sound kind of technical, but bear with me for a moment as I’ll explain them all in a minute.
- Leaky gut
- Endotoxemia
- Production of short-chain fatty acids like butyrate
- Alterations in bile acid metabolism
- Effects on the secretion of gut hormones
The common denominator in all five of these factors is an imbalance in the gut microbiota. The gut microbiota are the little organisms that live in your intestines, both good and bad bacteria, viruses, and fungi. Scientists call an imbalance in the gut microbiota dysbiosis. Dysbiosis is common in diabetes, suggesting the gut microbiota and blood sugar problems are connected. In diabetes, levels of beneficial bacteria are decreased, whereas many harmful bacteria are increased. Small intestinal bacterial overgrowth is also common in diabetes.
Leaky Gut
Gut microbiota dysbiosis can lead to leaky gut, otherwise known as increased intestinal permeability. Leaky gut is the name for what happens when a person’s intestinal lining is weakened. This weakened lining allows toxins and bacteria to slip through into the bloodstream, causing problems throughout the body. Leaky gut creates inflammation and reduces insulin sensitivity. There’s also a link between leaky gut and diabetes.
Low-Grade Endotoxemia
Bacteria in the body produce a type of toxin known as an endotoxin, primarily a bad guy known as LPS. It’s a component of bacterial cell walls found mostly in gram-negative bacteria. When LPS escapes the colon during leaky gut and becomes a fugitive on the run throughout the body, it triggers an inflammatory response known as endotoxemia.
LPS also does a number on the way your body uses insulin. LPS triggers an inflammatory cascade in every type of tissue it comes into contact with in the body. In insulin receptors, this inflammation leads to reduced sensitivity to insulin—or—insulin resistance.
Endotoxemia and leaky gut go hand in hand. Since the intestinal lining is weaker, it allows these toxins to escape into the bloodstream, causing problems that at first glance don’t seem as if they’re linked to the gut.
Butyrate and Short-Chain Fatty Acids
Short-chain fatty acids like butyrate are important for gut health and insulin sensitivity. Bacteria in the gut, especially those that belong to the phylum Firmicutes, make butyrate. If your gut isn’t making enough butyrate it spells trouble for the way your body uses insulin.
In studies of obese mice, butyrate supplementation increased insulin sensitivity and improved weight loss. Fasting blood glucose, fasting insulin, and insulin tolerance remained normal in mice given butyrate.
In humans, if there aren’t enough butyrate-producing bacteria, it boosts the risk of metabolic disorders like diabetes.
Butyrate repairs the intestinal lining and reduces inflammation, helping to get rid of leaky gut, which in turn promotes healthy blood sugar levels.
Bile Acid Metabolism
Another way in which the gut controls insulin sensitivity is by regulating the way the body produces bile acids, which stimulate insulin secretion. People with leaky gut don’t recirculate bile acids efficiently. So they wind up with bile acid deficiency over time, which leads to inefficient detoxification as well as changes in how your body regulates fat and carb digestion.
Secretion of Gut Hormones
A healthy gut equals healthy amounts of gut-derived metabolic hormones called glucagon-like peptides (GLP-1), which are linked to blood sugar balance. GLP-1 boosts insulin levels when there’s glucose in the blood, helping to push glucose into your cells to improve blood sugar levels.
GLP-1 also keeps you feeling full and satisfied after eating so that you can stay away from desserts and other unhealthy foods.
How To Know If You Have Blood Sugar Issues
One of the best ways to monitor your insulin and blood sugar levels is to work with a functional medicine provider, who will order lab tests. The lab tests to measure insulin sensitivity and blood glucose include:
- Fasting glucose, optimal range 70 to 85
- Fasting insulin, optimal below 5
- Fasting uric acid, optimal less than 5.5
- HBA1c (a measure of blood sugar control over time), optimal range 4.8 to 5.2
Also important: Finding out if your gut is healthy by using a stool test. I like the BiomeFX panel.
The second way to see how your body is coping with blood sugar is to monitor glucose spikes. Everybody has glucose spikes to a certain extent. But when insulin sensitivity is low, blood sugar spikes are often too high since insulin is unable to control your blood glucose.
The best way to monitor glucose spikes is by using a glucose monitor for two to four weeks. Monitor readings should be 70 to 120 the majority of the time, but even more ideal is 70 to 100. Lots of people spike above 140, even if they’re not diabetic, but most of us shouldn’t be going over 120 most of the time.
What To Do About Glucose Spikes and Reduce Insulin Sensitivity
Eat Foods That Support Butyrate and Probiotic Bacteria
The main goals of balancing blood sugar and insulin are to raise butyrate levels and to get rid of any gut microbiota imbalances.
From a dietary perspective, there are certain foods you can eat to increase butyrate levels.
Butyrate foods include:
- Apples
- Leeks
- Onions
To support a healthy gut microbiota, eating high-fiber foods rich in prebiotics is a good first step. These types of foods can also help butyrate-producing bacteria flourish. Research has shown that eating fermentable fiber was linked to an increase in the beneficial bacteria Bifidobacteria. This type of fiber also normalized LPS and improved glucose tolerance and insulin secretion, while reducing inflammation.
Prebiotic foods include:
- Apples
- Beans
- Bran
- Chicory root
- Garlic
- Jerusalem artichoke
- Oat bran
- Onions
- Psyllium husk
- Tomatoes
It’s also a good idea to limit sugar and saturated fat, since these can cause butyrate levels to tank.
Butyrate Supplements and Other Solutions
Another way to increase butyrate levels is through using certain dietary supplements. In animal studies, giving mice butyrate supplements blocked the development of insulin resistance caused by eating a high-fat diet.
Probiotics containing Bacillus bacteria endospores such as MegaSporeBiotic can increase butyrate-producing bacteria in the gut.
Certain supplements can also boost butyrate production directly. These include:
- Alanine
- Citrus polyphenols
- Cystine
- Glutamate
- Glycine
- Lysine
- Oligosaccharides (FOS, GOS, XOS)
- Proline
- Sulforaphane
- Threonine
- Tributyrin X by Healthy Gut Company
I have found that it’s possible to boost butyrate by 140% in four weeks using a combo of MegaSporeBiotic and MegaPre—which only feed selectively the keystone bacteria species, not the bad guys—along with MegaMucosa to heal and repair leaky gut with essential nutrients as building blocks.
Balancing Blood Sugar By Improving Gut Health
I have seen so many patients experience an improvement in their health after addressing gut issues, restoring butyrate levels, and balancing insulin and blood sugar levels. They’ll often have improved energy, clearer skin, better sleep, less hot flashes, and many of their other health complaints go away.
You’re going to have the greatest success working with a functional medicine provider who can tackle all the bases. That’s why I invite you to reach out to me for a free 15-minute call to find out the best course of action for you.
If after the call you come on board as a patient, I’ll order the right tests for you. Based on the results and your symptoms, I’ll start you on a protocol to balance blood sugar, improve your gut health, and help you look and feel your best.
How to Heal Ulcerative Colitis: A Case Study
If you have ulcerative colitis, this is a case study you’re going to want to read. It’s about a woman—I’ll call her Sherrie—who suffered from this condition for years—until we were able to make some real breakthroughs in her health.
Ulcerative colitis is a type of inflammatory bowel disease (IBD), a disorder that also includes Crohn’s disease. People who have ulcerative colitis have an inflamed colon and rectum and ulcers on the intestinal lining. Living with IBD can be a roller coaster. Their symptoms worsen during flare-ups and their symptoms go away during periods of remission.
Doesn’t sound like much fun, does it?
Ulcerative colitis is often hard to put into remission. It can take time to pin down and treat the root cause. But I’ve found that ulcerative colitis responds well to functional medicine. Often, we can send its bags packing—or at least put it into a long-term remission.
Such was the case for Sherrie.
Sherrie’s Long-Term Battle With Ulcerative Colitis
When Sherrie first came to see me in January 2018, she had been diagnosed with ulcerative colitis nine years prior at the age of 25. Before developing symptoms, she’d had a stressful few years. She bought a house, got married, was finishing her bachelor’s degree, and became pregnant for the first time.
After her initial diagnosis her symptoms were manageable for years. She responded well to the drugs offered her. Conventional doctors gave her prednisone and Lialda (mesalamine) to lower inflammation. Most of her ups and downs were during pregnancy when she had to get off her meds, and she’d get better when she went back on the drugs.
After her third child was born in 2013, she went into remission and didn’t need to take any UC medications for two to three years. Then she caught a cold while traveling and this turned into an ear infection. She took antibiotics, which led to a UC flare. In the two years before she contacted me, she never came out of the flare, which motivated her to seek my help.
Sherrie suffered from bloody stool and watery, urgent diarrhea six to ten times per day. She couldn’t leave her house for fear of not being near a bathroom when she had to go.
She’d never been hospitalized, but the poor dear had only been in remission for a brief period since giving birth, she told me. Pregnancy and birth can cause an immune shift and had made her ulcerative colitis even more difficult to control.
The lab work ordered by other doctors found:
- Low iron and ferritin
- Low vitamin D
- Low potassium
- Low hemoglobin (she was anemic from blood loss)
- Monocytes and eosinophils very high (suggests a parasitic or other type of infection.)
When she first came to my clinic, she was already on a strict paleo diet. That by itself didn’t do any good.
Treating Stress Hormone Imbalances
The first step? Treating Sherrie’s stress-response system. The hypothalamic-pituitary-adrenal axis (or HPA axis) regulates our circadian rhythm and our stress response. Chronic stress can really throw the HPA axis out of balance, which leads to hormone imbalances. It can cause the adrenal glands to pump out too much of the stress hormone cortisol. Some people call this “adrenal fatigue,” but it’s really a problem with the entire HPA axis.
As Sherrie tapered off the prednisone, I gave her a higher than normal dose of dehydroepiandrosterone (DHEA), a hormone produced by the adrenal glands. Because she had been under stress, her adrenal glands were likely worn out and weren’t making enough DHEA.
In fact, every ulcerative colitis patient I’ve treated has had HPA axis dysregulation. So I typically always address this in my UC patients.
And guess what? Her ulcerative colitis flare regressed for the first time in two years. She now had only minimal rectal bleeding and not every day.
Candida and Intestinal Bugs
While dealing with Sherrie’s adrenals, I ordered a stool test that revealed she had high levels of the following bacteria and fungus:
- Candida
- Klebsiella
- Prevotella
- Proteus
- Pseudomonas
- Salmonella
- Staphylococcus
- Streptococcus
It didn’t surprise me that she had Candida overgrowth. The fact she had gotten worse after taking antibiotics for her ear infection was a BIG clue that fungal overgrowth played a role. Candida is a type of yeast that under the wrong conditions can turn into an invasive fungus in your body.
Plus, we know from studies that almost all cases of ulcerative colitis involve the marriage between a fungal imbalance and a bacteria that either trigger immune dysfunction or worsen it.
In mouse studies, Candida albicans can worsen inflammatory colitis. What’s more, the yeast Candida tropicalis teams up with certain bacteria like E. coli to form a monstrous biofilm larger than any created by just one or two of the species alone. A biofilm is a type of shield that bacteria and fungi can form to protect them from things like antibiotics.
The stool test also detected the presence of an amoeba parasite known as Entamoeba coli. Although many people with this parasite don’t have any symptoms, high amounts are linked to loose stools, gas, and other GI complaints. Amoeba infections in general are also linked to IBD.
Sherrie’s stool test also showed high levels of calprotectin, which is a marker of inflammation in the gut lining. A high calprotectin is a red flag for IBD. Her levels of secretory IgA (SIgA) were also high. SIgA lines your intestines and acts as a gatekeeper, keeping bacteria, parasites, and allergens out of your circulation.
Fancy Footwork and Ulcerative Colitis
I began treating the parasitic infection, balancing the microbes in the intestines, and starting round one of Candida treatment. However, we had to put the brakes on treating the Candida for a little while because before starting treatment for this fungus, Sherrie went into flare mode.
There’s often a lot of fancy footwork needed to treat ulcerative colitis patients. Flares can happen due to stress, seasonal changes, and other reasons. We need to time treatments so that we’re not putting too much stress on the body during flares.
Other issues that showed up in testing also needed attention. For example, her mitochondria—the powerhouses of the cells—were in trouble. This is likely because the Candida produced ammonia and acetaldehyde, both toxins to the mitochondria. She also had high levels of a damaging process known as oxidative stress due to the autoimmune process that had created a years-long raging fire in her body.
Her glutathione levels had also tanked, so her body wasn’t making enough of this antioxidant to fight the oxidative stress. I included liposomal glutathione into her regimen.
Here are some other strategies that worked:
- Adding low-dose naltrexone, an anti-inflammatory drug shown to reduce symptom severity in IBD
- Eating an anti-inflammatory diet and adding in foods like rice and some dairy
- Gut-focused hypnotherapy for her post-traumatic stress disorder (PTSD) response when getting into her car. This was triggered by the fear of needing to poop and not being near a bathroom. This therapy and the progress we were making allowed her to travel far from home.
Big Improvements in Ulcerative Colitis Symptoms, But More to Go
By August 2018, Sherrie was the best she’d been in two years!
In September 2018, I ordered another stool test and some other lab work. Some of her beneficial gut bacteria were low and her calprotectin levels were still high. At the same time, I ordered a food reactivity test. Based on that, I had her avoid eggs, wheat, lentils, peas, cashews, peanuts, tuna, and a few other foods.
Her worst flares tended to happen between Thanksgiving and Christmas. My theory? Holiday stress combined with lack of sun and vitamin D contributed to these flares. I learned to give her proactive support heading into that time of year.
Finally, for the first time, she was able to go through the holidays with only a minor flare. I gave her a Chinese herbal formula known as Yunnan Paiyao, which stopped the flare in three days. The Chinese herbs also firmed up her stool.
In addition, I gave her pre- and probiotics and improved her detoxification and antioxidant levels.
Ultimately, after a period of three steps forward and two steps back, she was able to endure the holidays with zero flares.
By January through May 2019, she was better overall and her stool consistency improved, but she was still bleeding mildly.
So much progress, but there was still a root cause that had not been addressed. At this point, I ordered more testing, including a stool test that found the amoeba parasite Blastocystis. The testing also revealed problems digesting and using fats, so I had her take ox bile and a few other supplements.
What’s more, her zinc levels were low. Zinc is critical for bowel repair and lowering inflammation. Selenium—a mineral critical for autoimmune health and the production of glutathione—was also low.
The testing showed her oxidative stress levels were high and her detox abilities were overwhelmed. Levels of the antioxidant glutathione were better, but still low. She still had some Candida.
How To Stop An Ulcerative Colitis Flare-up
In July 2019, after a stressful event, Sherrie went into another flare. I put her on the Specific Carbohydrate Diet (SCD), a diet that’s free of sugar, grains, starch, and processed foods, which really helped. Butyrate enemas were also helpful. Butyrate is a short-chain fatty acid formed from the fermentation of dietary fiber in the colon. It is the main fuel the cells of our intestinal lining use for repair, and it is known to reduce ulcerative colitis symptoms.
Even before our next appointment, as soon as Sherrie could feel a flare coming on, she immediately followed my advice for reducing a flare. It was a BIG win! She was learning how to manage and stop flares on her own. The flare stopped by August and by the fall she was the best she’d been in four years.
She had another flare at the end of summer triggered by poison ivy while camping, but she was able to stop it within two to three days.
By fall she was feeling amazing. She was having regular, twice daily bowel movements. There was no urgency and the stool was well-formed. At the same time, Sherrie was finishing round two of the Candida program.
From fall of 2019 to January 2020, Sherrie stayed in remission. Right after the holidays were over she had another flare, but she was able to stop the flare almost entirely on her own before our next appointment. Yay!
We tested again. As you can see, this is a process of continually testing, treating, and modifying the protocol until we can get ahead of the disease process. Since her vitamin D levels were very low, I gave her a higher dose supplement. Her gut microbiome was also imbalanced with low levels of a type of bacteria known as Akkermansia. I focused on restoring levels of this important bacteria using specific prebiotics (pomegranate seed husk, matcha, greens powders, red powders for polyphenols, and acacia fiber) in order to repair her gut lining.
She had only a mild flare in the winter of 2019-2020. This happened in February 2020 and drew out with occasional small amounts of blood until April.
Can Mold Toxicity Cause Ulcerative Colitis?
After the flare in February 2020, we discussed some reasons why she kept having flares—and we had a breakthrough.
I knew that there is a link between mycotoxins—toxins produced by mold—and ulcerative colitis. When no obvious lifestyle or nutrition factors could explain Sherrie’s UC flares, I started digging deeper into what might be bothering her in her environment- her house to be exact. The fact she got worse in winter when the environment was more moist also pointed toward mycotoxins as a possible cause.
Even though her home was a new build she knew for certain there was periodically mold in her home. She and her husband often tried to clean it up.
We tested Sherrie for mold and mycotoxins in April 2020. Many markers for mycotoxins were high. An inflammatory marker known as TNF-alpha was also elevated.
Aha! Mold could definitely be the culprit.
She had her home inspected by a professional company that uses indoor mold testing and found the home was contaminated.
I started Sherrie on a treatment regimen for mycotoxins in July 2020 to proactively get her through her vulnerable period in late fall/winter.
At first that strategy paid off. She felt great. Her stool was firm and she had no flares.
She took a break from the mycotoxin program and had a flare between Christmas and New Year’s 2021. She mostly recovered within a month. But since she was still having flares, I decided to retest her for mycotoxin markers in February 2021.
That testing revealed she still had very high levels of the mycotoxin known as ochratoxin. Although these tests aren’t always 100% accurate, Sherrie’s lack of complete progress, her symptoms, and other markers suggested mold could be to blame.
I put her on another round of the mold protocol, and she stayed well through August 2021.
I ordered another mycotoxin test and it was much lower, although still high. This suggested she might be getting re-exposed.
Her husband had done some mold remediation on their home. But another round of indoor mold testing still showed the mold was off-the-charts positive. A mold-testing company found more mold in the utility room behind the water heater, in the shower caulking, and in the air.
They had their home professionally remediated.
I then put Sherrie on another round of mold treatment.
She had COVID-19 in November 2021 but did not experience a UC flare even though her body was under stress from the virus. This showed her intestines were getting stronger.
Stopping Ulcerative Colitis in Its Tracks: Success at Last!
Sherrie had no UC flares through the winter of 2021—the first winter with no flares in nine years. Over the course of treatment, Sherrie would have long periods up to a year with no bleeding, but she might develop loose stools with blood for a few weeks and then go back into remission. But by 2022, she had gone a very long time with no visible blood in her stools. Now we were getting somewhere!
Her mold test came out clear. She felt great—high energy, no anxiety, and able to travel a lot in the winter and spring without fear.
At this point, I put her on a long-term program featuring antioxidants and pre- and probiotics. She’s taking minimal supplements and doing well.
Sherrie’s case shows that ulcerative colitis and inflammatory bowel disease respond well to a functional medicine approach. In IBD, there are many overlapping root causes that must be identified, treated, and modified, all the while working around a person’s flare-ups. Over time, Sherrie and I figured out her triggers and she learned the tools to stop her flares before they started. It may take some time, but ultimately a functional medicine practitioner can dig down to the root problem in order to heal ulcerative colitis.
Heal Ulcerative Colitis with Functional Medicine
Like Sherrie, you can heal ulcerative colitis by working with a functional medicine practitioner. That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you.
If after the call you come on board as a patient, I’ll order the right tests for you and start you on an anti-inflammatory protocol. The goal is to pinpoint your individual triggers and put ulcerative colitis in remission or cure ulcerative colitis altogether.
A Functional Medicine Practitioner’s Approach To Treating IBD
When a patient visits me for the first time with inflammatory bowel disease (IBD)—ulcerative colitis or Crohn’s—they’re usually in bad shape.
They have abdominal pain and cramping, diarrhea, fatigue, and other problems, such as visible blood in the stool.
In other words, they’re experiencing an IBD flare.
People who suffer with ulcerative colitis or Crohn’s experience usually have flare-ups when symptoms are much worse, as well as periods of remission, when their symptoms go away. It can be frustrating and hard to have a “normal” life.
When patients come to me for IBD treatment, the first step is to get the patient out of the flare so we can focus on putting the IBD into remission- for good.
In this blog post I’m going to dive into what I do to treat IBD naturally. We can get lasting remission without the use of medications, as seen in this real-life success story from one of my patients. But, first, a word of caution.
Do NOT try this at home!
There’s a very strategic order of operations. If you do any of the things I mention in this article in the wrong order, you can make yourself worse.
Much worse.
For example, if a patient is in a severe flare I might not throw betaine hydrochloride, a digestive aid, at them until later. If they take betaine hydrochloride during an IBD flare it can make things worse.
That’s why it’s so important to work with a functional medicine provider.
I can’t say it enough: If you have ulcerative colitis or Crohn’s, get yourself a good functional medicine practitioner.
Okay, with that out of the way, let’s briefly recap what IBD actually is and the symptoms it causes.
What Is IBD?
Inflammatory bowel disease refers to conditions like ulcerative colitis and Crohn’s disease. These conditions are linked to ongoing inflammation in the gastrointestinal tract. In ulcerative colitis, patients develop inflammation and lesions on the lining of the large intestine and rectum. Crohn’s disease is a type of IBD that involves the lining of the digestive tract. Crohn’s usually involves inflammation in deeper layers of the digestive tract compared to ulcerative colitis.
What Causes IBD?
IBD is an autoimmune disease believed to be caused by an abnormal immune response to gut microbiota or food in susceptible people. In IBD, the immune system malfunctions and attacks the cells in the gastrointestinal tract. The cells in the intestines are innocent bystanders but the immune system thinks they’re foreign invaders. The primary cause and the triggers of IBD are still unknown.
IBD may have a genetic component, since it occurs in some people who have family members with the disease. However, most IBD patients don’t have a family history of the disease.
IBD risk factors include:
- Younger Age – Most people with IBD are diagnosed before the age of 30, but some patients don’t develop the condition until they’re in their 50s or 60s.
- Family History – People with a close relative who has IBD are at higher risk of the condition.
- Cigarette Smoking – This is a risk factor for Crohn’s disease.
- Nonsteroidal Anti-inflammatory Medications (NSAIDS) – Anti-inflammatory drugs like ibuprofen (Advil, Motrin, etc.) and naproxen sodium (Aleve) as well as others in this class may increase the risk of developing IBD or worsening the condition in people who already have it.
Inflammatory Bowel Disease Symptoms
IBD symptoms are different depending upon how severe your inflammation is and where it’s located. IBD patients usually go back and forth between disease flares and periods of remission.
Symptoms of ulcerative colitis and/or Crohn’s include:
- Abdominal pain
- Blood in the stool
- Constipation, especially when inflammation occurs in the rectum.
- Diarrhea
- Fatigue
- Poor appetite
- Unintended weight loss
IBD Complications
Ulcerative colitis and Crohn’s disease share several complications. These include:
- Increased risk of blood clots
- Increased risk of colon cancer
- Increased risk of primary sclerosing cholangitis, a condition that causes scarring within the bile ducts, leading to liver injury.
- Inflammation of the skin, eyes, and joints
Patients with IBD also take medications that can have side effects. For example, corticosteroid drugs increase the risk of osteoporosis and high blood pressure, as well as other conditions.
Possible complications of Crohn’s disease:
- Anal fissure, a small tear in the tissue lining the anus.
- Bowel obstruction
- Fistulas. Inflammation leads to these abnormal connections between different body parts. In Crohn’s, fistulas can develop near the anal area and may become infected.
- Malnutrition
Possible complications of ulcerative colitis:
- Dehydration caused by frequent diarrhea.
- Toxic megacolon, a condition where the colon rapidly widens and swells.
- Perforated colon, a hole in the colon that often occurs due to toxic megacolon.
Fight The Flare
The first thing I do for a patient who’s in the middle of an IBD flare is to begin an anti-inflammatory protocol while at the same time ordering important tests. The two goals at first:
- Prevent tissue inflammation
- Bring symptoms into remission
One of the best ways to calm the tissue inflammation and get out of flares is the specific carbohydrate diet (SCD). The SCD diet is a whole-foods diet including vegetables, fruit, fish, meat, nuts, beans, and healthy fats and oils. It excludes sugars, processed foods, preservatives, all grains, starchy vegetables, and lactose. In patients with diarrhea, I’ve really seen the SCD make a HUGE difference. The elemental diet is also very useful for seven to 10 days. An elemental diet is a liquid formula providing all of the basic nutritional elements you need for health, in a form that your body can easily absorb. One clinical trial of 23 patients with ulcerative colitis found that 56% went into remission on an elemental diet and nearly half of those remained in remission for 7 to 28 months.
Even if the patient isn’t gluten sensitive, I urge the patient to go on a gluten-free diet. Gluten promotes leaky gut, a condition that will stop a patient from going into remission. Mostly, I encourage any patient in an IBD flare to go on a paleo-type diet, with no gluten and no carbs.
For patients in flare mode, I also recommend a Chinese herbal formula called Yunnan Paiyao. In addition, I put them on high-dose DHEA to support the adrenals as they withdraw from corticosteroid drugs.
It’s also important anyone with diarrhea take electrolytes like magnesium and potassium. And Epsom salt baths and butyrate enemas are a part of my anti-flare strategy.
Interpreting Test Results and Treating Accordingly
While making those initial changes to diet and supplements, I order a number of tests in IBD patients. These include stool tests, as well as tests to find out if a patient is nutrient deficient, and tests for markers of oxidative stress, methylation, and neuroinflammation. Figuring out a person’s specific problem areas helps build a protocol precisely for their needs.
Oxidative stress is what you might know as free radical damage. Oxidative stress happens when free radical production goes out of control. Inflammation from IBD can cause oxidative stress in the colon.
Methylation is an important process that affects many bodily functions. People can have genetic defects in methylation. These defects are linked to the development of IBD. Often the genetic defect involves the inability to metabolize the folic acid form of the B vitamin folate. We get around this by giving patients a special form of folate that can bypass the pathway needed to use folic acid. This special form of folate is called 5-MTHF.
You’re probably wondering what neuroinflammation has to do with IBD. Well, one is inflammation in the brain and the other is inflammation in the gut. I am interested in markers of neuroinflammation in IBD patients because of the gut-brain axis. What’s happening in the brain is linked to the gut and what’s happening in the gut is linked to the brain.
Stool testing is another important test in patients with IBD. Stool testing detects parasites, an imbalance in the gut microbiome, and fungal infections—all of which can impact your gut health. This type of testing can let me know if specific types of good bacteria are lacking. In this way, I can build up what’s missing in the gut by giving high-dose probiotics, fiber, prebiotics and more to patients who need them.
Adrenal Testing
I order adrenal hormone testing for my IBD patients. Adrenal testing is important because the adrenals make the stress-hormone cortisol. Many patients with IBD are vulnerable to mental stress, which can make IBD attacks worse or even knock someone out of remission.
Patients who are in a flare and on corticosteroid drugs cannot take the adrenal test right away. This type of drug raises cortisol levels and will throw off adrenal test results. In this case, I may have to wait until symptoms are more controlled and the patient can wean off of corticosteroids. I also take them off high-dose DHEA. Only then am I able to test adrenal function.
Mycotoxins Testing
In the past, I only ordered mycotoxin tests in IBD patients who were not getting results from the usual treatments. But now, after years of treating IBD patients, I’ve noticed there’s a strong connection between toxins made by mold (mycotoxins) and ulcerative colitis.
Yes, this is a thing. Even studies published in medical journals confirm it.
That’s why I no longer wait to test IBD patients for mycotoxins. Instead, my attitude is usually: let’s just get ahead of this and deal with mycotoxins if they are a problem.
Food Sensitivity Testing
Food sensitivities are an important factor in IBD. They can trigger inflammation in the gut. They can stress the immune system so that it malfunctions. They can promote intestinal permeability, or leaky gut.
In IBD patients, there could be two things going on:
- Actual food sensitivities where you have an immune reaction to certain foods.
- Foods irritating the gut without causing any immune reaction. In this case, the irritation and inflammation occurs in a biochemical way. These types of foods are still difficult to digest or are feeding the bad bacteria even if you’re not actually having an immune reaction to them.
The type of food sensitivity testing I like to use not only tests for IgE and IgG but also other aspects of food sensitivities, such as complement. This helps me capture food reactions that are immune-mediated and those that are not.
How To Stay in Remission During IBD
Best Diet For IBD
Conventional “wisdom” says you shouldn’t eat salads and fiber when you have IBD.
Wrong. Very wrong.
You eventually want to emphasize roughage and fiber so you’ll have the prebiotics you’ll need to feed the beneficial bugs in your gut. But timing is everything.
During the remission phase, the goal is to emphasize resistant starch and various types of prebiotics. This type of starch feeds the good bacteria in your colon. I personalize this plan based upon the results of your microbiome testing. The key is to choose prebiotics that only feed the good bacteria, not the harmful ones.
When in remission, expand your diet a little compared to when you were in a flare. Dairy and gluten probably are only going to make things worse. But you can add other things back into your diet one at a time and watch how you react.
The key? Choose foods less likely to cause a flare-up. Avoid gluten, dairy, eggs, nuts, and seeds.
Identify Your IBD Triggers
Another helpful strategy during remission? Focus on preventative management of your stress. For example, if you know you get stressed around the holidays, be proactive and plan ways to reduce your stress such as extra self-care during that time of the year.
The key is to pinpoint your triggers. Do your flares only happen in the winter? Then we need to find out what’s causing them. At that time of year I also want to look at vitamin D levels to make sure yours aren’t too low.
The Best Type of Exercise for IBD
Healthy exercise is also important. By healthy I mean don’t overdo it, especially if you have IBD. Aim for mild cardio three times per week but focus more on weight training, which can help build the microbiome and reduce inflammation.
On the other hand, too much intense cardio (more than 30 minutes), can increase inflammation and spike cortisol levels. Intense cardio can boost levels of an inflammatory protein known as IL-6. High levels of IL-6 are linked to IBD flares.
When you do any cardio exercise, aim for shorter walks or hikes in nature.
Dietary Supplements for IBD
Each of my patients with inflammatory bowel disease has a different supplement protocol customized to their test results and where they are in the course of the disease. Here are some of the supplements I may use in IBD patients:
- Yunnan Paiyao, a Chinese herbal formula for inflammation.
- High-dose probiotics
- Prebiotics
- Liposomal glutathione, which as an antioxidant reduces oxidative stress. In the early stages of treatment, I prefer this over the glutathione precursor N-acetyl cysteine (NAC) because NAC can thin the gut lining.
- Nutrients that show up deficient on testing such as B vitamins.
- Curcumin or turmeric extract to reduce inflammation.
It’s Critical To Work With a Functional Medicine Provider
As I mentioned earlier, if you try to treat yourself you could really make things worse.
Or you could delay your recovery.
There’s an order of treatments that need to take place and this order is unique to each patient.
That’s why I invite you to reach out to me for a free 15-minute troubleshooting call to find out the best course of action for you. If after the call you come on board as a patient, I’ll order the right tests for you and start you on an anti-inflammatory protocol.
The goal is to get you into a long-lasting IBD remission. My protocol has worked on many patients and it’s very effective, but it may take time. At first, you might take one step forward and two steps back. But with persistence, testing, and modifying your protocol, we can find the winning combination to turn off your IBD. In the end, we can calm your gut’s inflammation and get your digestive tract feeling comfortable and healthy again.
If you’d like to see an example of how this approach can bring lasting remission, read a real-life case study of one of my patients with UC (coming soon).
What Causes Restless Leg Syndrome? Natural Remedies for RLS
You’ve just fallen asleep when it hits. That uncontrollable urge to move your legs.
Your legs also ache and throb.
It’s known as restless leg syndrome (RLS), and it makes you feel like you need to put a leash on your legs to keep them from trying to run away. Down boys! Down!
Restless leg syndrome is a condition where your legs are fidgety and uncomfortable, usually at night during sleep. But sometimes it can happen during the day when lying down or sitting for a long time, like when you’re in the car or at the movies.
Symptoms of Restless Leg Syndrome
The main symptom is the urge to move the legs. However, people with restless legs describe other symptoms such as:
- Aching
- An “electric” feeling
- Crawling
- Creeping
- Itching
- Pulling
- Throbbing
The condition is known for:
- Happening when lying or sitting for a long time.
- Relief with movement. The urge usually goes away when walking or stretching.
- Occurring mostly at night.
In some people, the disorder happens together with twitching or kicking of the legs while they’re sleeping. This condition is known as periodic limb movement of sleep.
Causes of Restless Legs Syndrome
There are a lot of reasons why you have restless legs. Since I specialize in treating women with gastrointestinal disorders I’m really familiar with one of the most common causes of RLS—small intestinal bacterial overgrowth, or SIBO for short. An imbalance in the gut microbiome—what scientists call dysbiosis—is also often to blame.
But there are other factors that can cause restless legs. In fact, there might be more than one culprit involved. Let’s dive into all those factors in this blog post and I’ll tell you the natural remedies for restless legs syndrome that have worked for my patients.
SIBO and Restless Legs
In my clinical practice, I see a lot of patients with SIBO who also have restless legs. Studies in medical journals confirm the link between SIBO and restless legs.
If you want to know more about what is SIBO, I recommend you read this blog post I wrote. Meanwhile, in a nutshell, SIBO is an imbalance in the microbes that live in the small intestine.
This can mean that there are too many bacteria or the wrong kind of bacteria that don’t belong in the small intestine.
So what does SIBO have to do with restless legs? A lot.
SIBO causes inflammation in the gut, which leads to the release of hepcidin, a hormone critical in delivering iron to the body and the brain.
Iron is necessary for growth and development as well as supplying the body with oxygen through the blood. But more important for our topic here, iron is a cofactor in the production of dopamine, a brain chemical (neurotransmitter) that tells leg muscles to relax at night. Without enough dopamine, muscles can remain hyperactive. The result? Restless legs syndrome.
When the body releases too much hepcidin, you might not even realize there’s a problem with iron. When you get tested for iron levels or for ferritin, the tests come back normal. And yet your body isn’t able to use the iron that’s available.
Eating enough protein is also critical for making dopamine. The body needs the amino acids tyrosine and phenylalanine from protein as well as iron to make dopamine.
I’m not the only one who connected the dots between SIBO and restless legs. In a small study published in the online version of the journal Sleep, SIBO was found in all seven participants with RLS. Compare this to the general population without restless legs; SIBO occurs in less than 15% of people.
Restless Legs Treatment #1: Work with a functional medicine provider to test for and treat SIBO. Dietary changes, probiotics, fiber, digestive support, and antimicrobials are often used to turn around SIBO. Eat 1-1.2 grams of protein per kilogram of body weight, taken daily in divided doses.
Gut Microbes Gone Bad
Sometimes, treating SIBO isn’t enough and the restless legs continue. There could be many reasons for that, but one of them could involve gut dysbiosis beyond just SIBO. Gut dysbiosis causes inflammation in the gut and the body. In my practice, I don’t just test for SIBO. I use stool testing to look for bacterial overgrowth, fungus, and parasites.
Imbalanced gut bacteria lead to many of the same problems that occur with SIBO, such as the release of hepcidin and the inability of the brain to use iron.
Restless Legs Treatment #2: Balance the gut microbiota through the use of a good probiotic and avoid factors that lead to an imbalance such as eating too much sugar and processed foods and stress. Your functional medicine provider may use antimicrobials, antiparasitics, and/or digestive support to optimize your gut microbiome. Eat 1-1.2 grams of protein per kilogram of body weight, taken daily in divided doses.
High Histamine
Another reason why SIBO or dysbiosis causes restless leg syndrome is because they can lead to histamine excess.
Histamine is a chemical found in many cells of the body. It causes allergy symptoms like itchy, red eyes, runny nose, and sneezing. When the body makes too much of it, it changes how the nervous system functions. This can be a problem for people with restless legs.
People who make too much histamine or who have histamine intolerance often have problems sleeping, since histamine is a brain stimulant.
The catch? Because histamine revs up the brain, people with restless legs who also are making too much histamine can get by on little sleep. They’re not sleepy in the daytime and can function even though they’re exhausted.
Scientists are now beginning to believe that targeting histamine receptors may reduce restless leg syndrome. Histamine receptors are proteins found on the surface of some cells. These proteins are triggered by histamine. Think of receptors like locks on a door and histamine as the key that fits into the lock and gets it to open.
Mast cells are immune cells found in the blood that release histamine as part of an allergic reaction. Now researchers are finding that when mast cells are activated, it may cause restless legs. People who have a condition known as mast cell activation syndrome are more likely to have restless legs compared to healthy controls.
Restless Legs Treatment #3: You can start by supplementing with DAO, an enzyme that breaks down histamine. Two other ways to support histamine levels are Natural D-Hist from Orthomolecular Medicine and quercetin. A low-histamine diet may also help.
But keep in mind that histamine excess is complicated. There are different pathways through which people have problems. It’s best to work with a functional medicine provider to find out if histamine excess is part of your problem and if so, why you’re making too much histamine.
B Vitamins for Restless Legs Syndrome
Vitamins B12 and vitamin B1 (thiamine or benfotiamine) can both fend off restless legs. For example, in patients with inflammatory bowel disease, vitamin B12 deficiency is linked to an increased risk of restless legs syndrome.
Vitamin B1 helps the body make a chemical called acetylcholine, which is involved in motor control. In other words, B1 supports the health of the nerves that control the muscles. So it makes sense that if you’re low in vitamin B1, your legs and body will fidget.
The body also needs vitamin B1 to make dopamine. As I mentioned earlier, dopamine is a brain chemical that says to the leg muscles: “Relax! Relax!”
I’ve had patients tell me that even when other restless legs treatments didn’t help, vitamin B1 worked miracles.
Restless Legs Treatment #4: Start by taking a B complex vitamin or vitamin B1 (up to 100 mg). You may need to go up to 300 mg, which you should only do under the supervision of a functional medicine provider.
Food Sensitivities
Food sensitivities may be to blame for restless legs in some people. A case study of three patients found that food sensitivities caused movement disorders including repeated shrugging of the shoulders. In these patients, milk, coffee, eggs, aspartame (Nutrasweet), tea, chocolate, citrus, raspberries, strawberries, potatoes, beef, and pork caused the most problems. This matches my experience in clinical practice.
Restless Legs Treatment #5: Work with a functional medicine provider, who can order food sensitivity tests to find out which foods don’t agree with you. They may also suggest an elimination diet or just removing the foods that bother you from your tests. After a trial period without the foods, your practitioner will instruct you to introduce one at a time while watching for symptoms. That way you can see which food is causing your restless legs.
Other Causes of Restless Legs
Here are other common reasons why my patients develop restless legs:
- Alcohol, caffeine, nicotine
- Certain medications
- Low vitamin D
- Pregnancy
- Stress/anxiety
- Vigorous exercise
Drugs That Cause Restless Legs Syndrome
Sometimes, the cause of restless legs is a certain prescription medication. Here are some of the most common drugs that cause restless legs.:
- Allergy meds
- Diphenhydramine
- Neuroleptics
- Selective serotonin reuptake inhibitors (SSRIs)
- Tricyclic antidepressants
Getting Rid of Restless Legs
I specialize in treating GI disorders and women’s health. So if you have digestive symptoms and restless legs, I know how to get at the root cause of why your legs are so fidgety.
The first step? Book a free 15-minute troubleshooting call with me to find out the best course of action.
If after the call you come on board as a patient, I’ll order certain tests to show whether your restless legs are caused by nutrient deficiencies, gut dysbiosis, or histamine excess. Whatever the cause, I’ll be on it until I find out what’s wrong. Book a call today so you’ll sleep more deeply tomorrow.
What Causes Diarrhea in Adults and How to Stop It
Diarrhea can take control of your life. I’m not talking about the average tummy bug kind of diarrhea. I’m talking about the type of diarrhea that lasts for days, weeks, months, or even years…chronic diarrhea.
Diarrhea can disrupt the rhythm of your daily life, and take a real toll on your body. But, the good news is that you do not have to live with chronic diarrhea! Diarrhea is a treatable medical condition. Together, we can uncover what’s causing your diarrhea, help to treat your symptoms, and get you back on the road to good health.
Diarrhea Symptoms
Passing loose, watery stools three or more times per day is the primary symptom of diarrhea. Other symptoms can accompany diarrhea including:
- Belly bloating
- Cramping
- An urgent need to use the bathroom
- Nausea
- Abdominal pain
Some people can experience more severe symptoms including:
- Blood or mucus in your stools
- Fever or chills
- Vomiting
- Light-headedness or dizziness
What Causes Diarrhea?
There are a variety of factors that can cause diarrhea. Temporary diarrhea, lasting one to two days, can result from a viral infection, the food you ate or traveling.
On the other hand, chronic diarrhea can indicate a more serious problem. The most common causes of chronic diarrhea include inflammatory bowel disease (Crohn’s disease and ulcerative colitis), chronic infections, and malabsorption syndromes (cystic fibrosis, Celiac disease, lactose intolerance, etc.) in which food is not digested and absorbed.
Chronic diarrhea is a common complaint amongst our patients. Below are seven of the most common causes of chronic diarrhea that we treat including gallbladder removal, IBD, gut dysbiosis or pathogen imbalance, histamine intolerance, gluten intolerance or Celiac, dairy intolerance, and SIBO.
1. Gallstone or surgical removal of the gallbladder
Frequent loose, watery stools after having gallstones or having your gallbladder removed (cholecystectomy) is common. The gallbladder collects bile to release when you eat aiding in the digestion of fats. Removing the gallbladder takes away the main storage site for your bile acid. Instead, the bile acid is stored in the gut causing it to be less concentrated and drain into the intestines. Once in the intestines, it can have a laxative effect making stools looser.
GI transit times can also be altered after gallbladder surgery causing transit times to decrease in the small intestine and accelerate in the colon. This impairs the body’s ability to absorb water from your stool leading to looser, watery stools.
2. IBD
Inflammatory bowel diseases (IBD), including Crohn’s, Ulcerative Colitis, and other types of colitis (microscopic or lymphocytic colitis), are diseases of chronic inflammation. IBD causes tissue destruction and inflammation of the bowel walls limiting the body’s ability to absorb fluids. This results in loose, watery, or even completely liquid stools.
Patients with IBD may experience frequent and urgent bowel movements because fluid moves more rapidly through the intestine. You may also see blood in or on the stool and experience extreme weight loss, anemia, fever, and loss of appetite.
3. Gut Dysbiosis or Pathogen Imbalance
Gut dysbiosis is a generic term for an imbalance in gut flora. Our digestive tract contains a delicate balance of different kinds of bacteria. When one species becomes overgrown or gets wiped out, the balance is thrown off leading to diarrhea along with many other symptoms.
There are several pathogens known to cause gut dysbiosis including bacterial, yeast, parasites, and viral pathogens.
- Acute Bacterial Pathogens: The most common bacterial organisms to cause diarrhea include: e coli, shigella, Campylobacter Jejuni, Citrobacter, yersinia enterocolitica, salmonella, and Staphylococcus aureus. Chronic bacterial toxins like those secreted by C Difficile can also lead to diarrhea. Older adults in healthcare facilities, like hospitals or nursing homes, or who have recently been on antibiotics, are more at risk for contracting C Difficile.
- Yeast and Fungal Overgrowth: Rapid growth of Candida (a yeast) and cryptococcus (a yeast-like fungus) in the GI tract can lead to diarrhea, especially after antibiotic use.
- Parasites: Intestinal parasites including giardia, entamoeba histolytica, Cryptosporidium Parvum, and Protozoan parasites like blastocystis hominis, Cyclospora, Dientamoeba Fragilis, Entamoeba coli, and endolimax nana can cause diarrhea. Parasitic infections are often, but not always, marked by stomach cramps, bloating, nausea, and watery diarrhea.
4. Histamine Intolerance
Histamine is a chemical that notifies the brain when to release stomach acid for digestion. And, it is part of our response to injury or an allergic reaction. Histamine intolerance occurs when the body is unable to break down enough of it in the intestines, causing histamine levels in the blood to rise.
Histamine intolerance can result from a multitude of factors including a combination of genetics, and a leaky gut. This leads to decreased secretion of DAO enzyme (used to break down histamine), liver detox overburden, and dysbiosis.
5. Gluten Intolerance or Celiac
Gluten, a protein found in wheat, can cause inflammation in the gut and can change the structure of the gut wall. For people with gluten intolerance or Celiac disease, gluten can cause chronic diarrhea along with other GI symptoms.
6. Dairy
Dairy products contain three components that can cause diarrhea: lactose, whey, and casein.
Lactose intolerance is an inability to digest lactase, a sugar found in milk products. Lactose intolerance occurs when the small intestine does not make enough of the digestive enzyme lactase. This condition is common in adults with a genetic predisposition or after an injury, disease, or infection of the small intestine. Lactose intolerance causes diarrhea by increasing the volume of water in the colon, which in turn increases the volume and liquid content of the stool.
Casein and whey, the two proteins in milk products, can cause an allergic reaction when the body thinks the protein is harmful. Most people with an allergy to casein or whey have symptoms that appear as infants and outgrow them with age. However, patients with gut wall damage can experience dairy protein intolerance with diarrhea and other GI symptoms.
7. SIBO
SIBO is an overgrowth of bacteria in the small intestine. Normally, the small intestine contains fewer bacteria than the large intestine and is focused on food absorption. For many who have SIBO, diarrhea is a common symptom.
How is Chronic Diarrhea Diagnosed
The key to diagnosing chronic diarrhea is to uncover the underlying root causes so that we can address them and prevent future relapses. Common tests for patients with chronic diarrhea may include:
- Comprehensive Stool Microbiome Testing – A stool sample can be used to evaluate the root cause of digestive tract issues. Functional medicine stool tests provide information about absorption, digestion, yeast overgrowth, bacterial imbalance, parasite infection, inflammation, metabolic activity, and immune function.
- SIBO Breath Testing with both lactulose and fructose for best accuracy
- Blood Test – Specific blood tests can help identify celiac disease antibodies and yeast antibodies.
- Imaging – Imaging can include endoscopy, colonoscopy, or sigmoidoscopy and is generally used to diagnose or rule out Inflammatory Bowel Disease or structural issues as a driver for symptoms.
Natural Remedies and Treatments for Diarrhea
The challenging part of treating diarrhea is that there is not a one size fits all treatment plan. Many mild cases of diarrhea will resolve on their own. But, for more severe, chronic cases of diarrhea there are a variety of natural remedies and treatments available.
Diet
Specific Carbohydrate Diet (SCD):
The SCD diet is incredibly effective at stopping urgent, frequent bowel movements. This is for you if you run to the bathroom 10 to 20 times per day. The SCD diet focuses on removing carbohydrates that are not fully digested and remain in the gut leading to an overgrowth of harmful bacteria. It is particularly helpful for my patients who have Crohn’s disease, celiac, ulcerative colitis, and chronic diarrhea.
Download a free guide to properly starting the SCD diet from the team at Healthy Gut.
Starch and Meat Diet:
A starch and meat diet is an alternative to the SCD diet that works for some people. This whole-food diet is focused on eating foods like white rice, white potatoes, meat, fish, and poultry. Like the SCD diet, this diet limits all processed and canned foods.
Diet Considerations During Flare-Ups:
Curing the cause of chronic diarrhea can take time. And, flare-ups happen. During diarrhea flare-ups keep these diet considerations in mind.
- Be cautious with fruit, except for bananas
- Raw vegetables can be hard to digest and cause GI upset
- High amounts of fats and oils can be difficult for a sensitive digestive system. Limit high-fat foods like egg yolks, cream, oils, and bacon.
Many other diets (low FODMAP, Low Histamine, Low Salicylate, Low Oxalate, or Autoimmune Paleo) can be useful for the treatment of diarrhea depending on the underlying causes.
Stress Reduction
Have you ever had to run to the bathroom before a presentation or a big event? That’s your gut responding to stress! Increased levels of stress can cause changes to your gut motility, which means that your body can slow down or speed up food processing based on your levels of stress.
Active stress relief activities are a critical component of naturally treating diarrhea. Try watching a funny movie, taking an Epsom salt bath, meditating, or practicing moderate exercise daily.
Sleep
Many of your body’s metabolic processes occur during the night, including digestion. And, sleep provides your body the much-needed energy for digestion to happen.
A few nights of poor sleep might not have a major impact on your GI health. But, chronic insomnia or poor sleep can impact your GI and contribute to your chronic diarrhea.
Supplements
Depending on the cause of your diarrhea, a variety of supplements may be beneficial to you. I often incorporate the following supplements into my patient’s treatment plans.
Digestive Enzymes:
After eating, enzymes break down the food so that we can absorb the carbohydrates, fats, and proteins. Without enzymes, larger food pieces remain in our gut and begin to ferment, feeding the bacteria. This can either slow down digestion or speed it way up.
There has been significant research indicating the successful use of digestive enzymes to support patients with chronic diarrhea. The key to digestive enzymes is taking enough with the right balance of acidity for them to work. It may take some time, but my patients who use digestive enzymes report amazing results!
I recommend Holozyme by Healthy Gut.
High Dose Probiotics:
High-dose probiotics have been shown to balance the gut microbiome and improve intestinal permeability promoting intestinal barrier functions and alleviating many inflammatory responses.
Depending on the cause of your diarrhea, I recommend a variety of probiotics usually containing 250 (or more) organisms daily to help control diarrhea. Below are a few of my go-to probiotics:
- S. Boulardii, a probiotic yeast strain, is my number 1 go-to for helping alleviate diarrhea, especially if it was a result of antibiotic use. But, in my clinical experience, patients with IBD should proceed with caution with introducing S. boulardii because Anti-Saccharomyces cerevisiae antibodies (ASCA) have been associated with Crohn’s disease. Saccharomyces Cerevisiae (Brewer’s/Bakers yeast) is similar enough to S Boulardii that the immune systems of sensitive individuals can cross-react, potentially triggering a symptom flare.
- Bacillus Claussi, a spore-forming probiotic, is an effective probiotic for treating diarrhea, preventing antibiotic associated diarrhea, and may be viable as the only treatment in some cases of SIBO where tolerated.
- Bacillus Subtilis is a multifunctional probiotic ideal for preventing the growth of bacteria and enhancing nutrient digestion. HU58, a strain of bacillus subtilis, is used for the management of antibiotic-associated diarrhea in adults.
- Lactobacillus Rhamnosus GG (LGG) is one of the most widely used probiotic strains and it is ideal for patients with histamine driving their diarrhea. In addition, there are many well-documented studies showing that LGG is indicated for the prevention and treatment of gastro-intestinal infections and diarrhea.
- UltraFlora Intensive contains Lactobacillus plantarum 299v, a probiotic strain of lactic acid bacteria that is naturally occurring in the human gut. This probiotic is excellent at decreasing anti-inflammatory symptoms making it ideal for reducing diarrhea in patients with IBS, C. diff, spontaneous colitis, and high E coli levels.
- High-dose lactobacillus, found in TheraLac, promotes healthy, rapid growth of all beneficial bacteria that can boost immune health and promote regularity.
Immunoglobulins or Colostrum:
Immunoglobulins and colostrum help strengthen the body’s natural immune system. While also fighting bacteria and viruses that cause diarrhea. I recommend utilizing a bovine-derived serum that is lactose-free to repair and support healthy gut barrier functions.
Chinese Herbal Formulas:
This is far from an exhaustive list of Chinese herbal formulas for diarrhea, but these are three of my favorites to use with my patients.
- Shen Ling Bai Zhu San – Usee for poor nutrient absorption, bloating, and/or loose stools.
- Raise Qi – Helpful for poor digestion, bloating and gas pain, chronic diarrhea, and loose stools.
- Huo Xiang Zheng Qi San – Ideal for treatment of acute diarrhea or travelers' diarrhea.
Short-Term Support in a Pinch
When you're in a pinch, it’s always helpful to keep a few diarrhea treatments in your arsenal. I recommend keeping these on hand:
- Bismuth Subsalicylate: Also known as Pepto-Bismol, increases the amount of fluid your intestines can absorb while reducing inflammation and overactivity of your intestines. Note that both liquid and chewable Pepto-Bismol may contain fermentable sweeteners. Follow the label for dosage.
- Imodium: Imodium works to slow motility for sudden diarrhea. Follow the label for dosage.
I Can Help Identify the Cause of Your Diarrhea and Get You Back on the Path to Good Health
Are you ready to troubleshoot your chronic diarrhea? Get a better understanding of your digestive health and the natural approach to resolving diarrhea once and for all, by booking a free 15-minute call with me.
If after the call you come on board as a patient, your clinician will order the best tests for your specific situation, and develop a unique treatment plan so that you can get back on the road to good health.
References:
"Symptoms & Causes of Diarrhea | NIDDK." https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea/symptoms-causes. Accessed 31 Mar. 2022.
"GI-MAP® Interpretive Guide - Diagnostic Solutions Laboratory." https://www.diagnosticsolutionslab.com/sites/default/files/u16/GI-MAP-Interpretive-Guide.pdf. Accessed 6 Apr. 2022.
"Histamine: The Stuff Allergies are Made of - MedlinePlus." 1 Apr. 2019, https://medlineplus.gov/medlineplus-videos/histamine-the-stuff-allergies-are-made-of/. Accessed 6 Apr. 2022.
"Enzyme therapy for functional bowel disease-like post-prandial ...." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6910206/. Accessed 12 Apr. 2022.
"Probiotics for infectious diarrhea - PMC - NCBI." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1773578/. Accessed 19 Apr. 2022.
"Bacillus clausii - The Probiotic of Choice in the Treatment of Diarrhoea." https://www.longdom.org/open-access/bacillus-clausii--the-probiotic-of-choice-in-the-treatment-of-diarrhoea-2157-7595-1000211.pdf. Accessed 12 Apr. 2022.
"Bacillus subtilis HU58 and Bacillus coagulans SC208 Probiotics ...." 11 Jul. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7409217/. Accessed 12 Apr. 2022.
"Towards a better understanding of Lactobacillus rhamnosus GG - PMC." 29 Aug. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155824/. Accessed 12 Apr. 2022.
The role of Lactobacillus plantarum 299v in supporting treatment of ...." 25 Jan. 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7882405/. Accessed 12 Apr. 2022.
What Causes Chronic Constipation in Adults and How to Relieve It
You’re all plugged up and can’t poop. You feel more backed up than a rush hour traffic jam.
Maybe it feels like there’s something in there that refuses to budge.
Your stomach is so bloated it looks like you swallowed a bowling ball.
If you have chronic constipation, we’re sure you’ll agree when we say it’s a real pain in the butt.
The good news? There are ways to get things moving again. But before we go into constipation relief, we’ll talk about what constipation actually is and what causes it.
What Is Constipation?
From a conventional medicine perspective, constipation is defined as having less than three bowel movements per week.
Functional medicine providers, on the other hand, usually want patients to have one to three bowel movements per day. That’s because they recognize the importance of bowel movements for removing toxins and other waste products.
Constipation can also refer to unhealthy stool. Doctors use what’s known as the Bristol Stool Chart to determine the health of a patient’s poop. This type of chart describes stool as being one of seven types. Type 1 (separate hard lumps) or type 2 (lumpy and sausage shaped) both indicate constipation.
What Causes Constipation?
Constipation can have a variety of causes, which is why it’s also a good idea to work with a functional medicine provider to find the root cause.
In some cases, people can have structural and anatomical issues that cause constipation. Medications like opioid drugs can also lead to constipation.
When those are not the issue, the most common causes of constipation are:
- Alterations in Gut Microbiology
- Candida or Yeast/Fungal Overgrowth
- Hypothyroidism
- Not Drinking Enough Water
- Parasites
- Pregnancy
- Small Intestinal Bacterial Overgrowth (SIBO)
The Good Bugs vs. the Bad Bugs
The collection of microbes in your gut—both good and bad—are called the gut microbiome. When the microbes that make up the microbiome become imbalanced—either by the bad outnumbering the good or by too much of one type of microbe—it can lead to gastrointestinal problems, including constipation.
Indeed, research shows that an imbalanced gut microbiome can affect how quickly food moves through your bowels and cause constipation. On the other hand, researchers have shown that a healthy gut microbiome prevents constipation. They accomplished this by performing what’s known as a fecal transplant, a procedure where fecal matter from patients who are healthy is transplanted into someone who has gastrointestinal problems. When scientists performed this procedure on patients with constipation, the patients’ gut microbiota and their constipation symptoms improved.
Because constipation is linked to an imbalanced gut microbiota, it’s also linked to other health problems you would never think have anything to do with the gut. For example, people with constipation are at an increased risk of having hay fever.
Candida or Yeast/Fungal Overgrowth
An infection with Candida or any other type of fungus can lead to an imbalance in the gut microbiome. This spells trouble for GI health and stool not moving as smoothly through the intestines.
Sluggish Thyroid
The thyroid gland is important for many processes in our bodies. When it’s underactive—a condition known as hypothyroidism—it causes the body’s processes to slow down. Hypothyroidism slows down the speed at which food moves through the digestive tract.
Dehydration
If you want to know how to relieve constipation in adults, drinking enough water is one of the best solutions.
The large intestine isn’t supposed to be the Sahara desert. It needs fluids to function. When you haven’t had enough water, the colon will grab it from the food, turning stools hard, dry, and more painful to pass. Being well-hydrated also keeps food moving through the intestines.
Parasite Infection
Usually, a parasitic infection starts with acute diarrhea soon after the infection started, like right after returning from a trip. But in my clinical practice I regularly see parasite-caused diarrhea turn into either chronic constipation or constipation alternating with diarrhea.
Patients who have parasite-caused constipation also have bowel movements that feel incomplete.
Pregnancy-Related Constipation
Constipation is a common complication of pregnancy. Nearly half of all pregnant women get constipated at some point during their pregnancy.
During pregnancy, constipation is caused by the dramatic increase in the hormone progesterone, which affects the intestinal muscle and causes food to move through the intestines more slowly.
Small Intestinal Bacterial Overgrowth
Small intestinal bacterial overgrowth—SIBO for short—is another common cause of constipation. SIBO is an abnormal increase in the bacterial population of the small intestines, especially with species of bacteria not usually found in this area of the body.
Diarrhea is a more common symptom of SIBO. When constipation occurs with this condition, it’s usually due to the methane-dominant form of SIBO. In this type of bacterial dysbiosis, there is an overgrowth of bacteria that make methane which can be detected on SIBO breath tests.
How To Relieve Constipation in Adults
It’s no fun being all backed up. Your body can’t get rid of waste and digestion is hampered. You may lose your appetite and when the poop finally comes out, it hurts. While you have probably tried the popular recommendations of drinking water and taking fiber, it may not have been enough. Here are my tried-and-true chronic constipation treatments to get my patients regular again.
Stay hydrated – Drink at least eight glasses of filtered water every day. Coffee and juice don’t count. Neither does tea unless it’s herbal tea. Helpful hint: put a pinch of sea salt in the water. This will help you absorb the fluid better.
Also, sip on warm water with lemon first thing in the morning. Drink this slowly and it will stimulate the gastrocolic reflex, which controls the movement of food through the GI tract after a meal.
Get a good night’s rest – Our bodies have their own internal clocks which control our circadian rhythms. When we ignore our natural circadian rhythms, it can lead to many problems, including constipation. That’s why between 48% and 81.9% of people working either rotating or night shifts have some form of GI problem including constipation.
Researchers also have found that morning IBS symptoms were worse after a night of poor sleep. The IBS symptoms improved after the study subjects slept better.
One reason why lack of sleep causes constipation is because it can affect the gut microbiota.
Get Moving – Walking and yoga are both helpful for constipation relief. Exercise is linked to what scientists call better gut motility—in other words it helps move food faster through your digestive tract.
Use a Squatty Potty – As the name implies, this allows you to squat when you poop. It’s a better, more natural angle and decreases straining.
Biofeedback – Biofeedback is a way to control some of your body’s functions. You can use it to help train your colon muscles to become more coordinated.
Foods to Help Constipation in Adults
I have found that a paleo diet can really get things moving again. This diet mimics a hunter-gatherer diet of meat, fish, eggs, seeds, nuts, fruits, veggies, and healthy fats and oils. In the paleo diet, there is no sugar, refined flour, gluten or dairy.
A low FODMAP diet or specific carbohydrate diet (SCD) has also worked in many of my patients with constipation. FODMAP stands for fermentable oligo-, di-, and monosaccharides and polyols. These are nondigestible carbohydrates which can trigger gut symptoms in some people. The SCD eliminates most carbohydrates including grains, starches, dairy, and sugars with only specific carbohydrates that require minimal digestion allowed. Fresh fruit, most vegetables, grass fed meat, and wild-caught fish are allowed while starches, grains, and processed or canned foods are prohibited. Usually, these types of diets are used for chronic diarrhea, but I’ve seen them kickstart bowel movements, especially when a patient has a chronic infection or an imbalanced gut microbiome.
If you find that your constipation gets worse with starches and sugars, stop eating sweets, which is really a good idea for your health anyway. Avoid using flours. Eat only whole food carbs like root veggies and whole grains if tolerated. Examples of root vegetables are daikon radish, beets, carrots, and parsnips. Beets are the best option especially if you notice that insoluble fiber makes your constipation worse.
Increasing healthy fats from olive oil, ghee, coconut, organic butter, and eggs is also helpful. Make sure you’re getting 2 tablespoons or more per meal—6 tablespoons per day. Fats can increase the rate at which foods move through your digestive tract.
If you tolerate dairy, try making 24-hour yogurt from full-fat cream. Yogurt is a good source of probiotics, which nourish the gut microbiome.
Unless you know or suspect that FODMAP veggies make your constipation worse, get more fiber in your diet by eating seven to 11 servings of vegetables per day.
It’s also a good idea to boost potassium intake. A great way to do this is by making homemade juice with cucumber, tomato, spinach, chard, and melon. Ripe bananas, avocados, and kiwi are also rich sources of potassium.
Fermented foods like chia soaked in kombucha are another ideal choice. These can promote a diverse and balanced microbiome.
Supplements for Constipation
The most common method of constipation relief are laxatives and stool softeners. Warning: these are gut irritants and are not a friend to the gut lining. What’s worse, you can become dependent (otherwise known as habituated) on laxatives so that your gut “forgets” how to poop regularly on its own.
People also often use fiber supplements for constipation, but this can backfire. Fiber supplements can make some people worse. Acacia and partially hydrolyzed guar gum (PHGG) are often the fiber supplements that constipated people can handle the best.
Digestive enzymes and a hydrochloric acid (HCL) supplement are other good choices. Bile support, especially in people who have trouble digesting fats, can help regulate gut motility and transit time (the amount of time food takes to get through your intestines). MegaGuard is a bile support supplement that works well for my constipated patients.
Magnesium oxide or citrate (500 – 2,000 mg at night) can get things moving. Work up to the higher dose slowly. Some people do better with magnesium hydroxide. Magnesium is osmotic, which is just a fancy way of saying it pulls water into the colon. Remember, the colon needs water and magnesium helps there. Natural Calm is a high-dose magnesium supplement you can try.
Another way to increase magnesium levels is to take an Epsom salt bath before bed. This will also soothe away stress.
Buffered vitamin C (2,000 mg) before breakfast and lunch will get your bowels moving. Colon Rx, which includes both Magnesium Oxide and the Ayurvedic herb triphala, has been used for millennia for bowel regulation. Both of these are non-habituating and very safe ways to reduce constipation.
If you have methane-dominant SIBO, Atrantil can treat constipation. It works for many people, but not everyone. It can take up to 21 days to see the full effect.
If you have a severe episode of constipation and nothing else is working, try glycerin suppositories or enemas using water, saline, or coffee. These can make a huge difference to get the gut moving in quick time.
Herbal formulas can work. But be cautious with ingredients like Senna, rhubarb, and aloe. You can become dependent (or habituated) on all of these stimulant laxatives if you use them too often and for too long. If you’ve been taking any of these ingredients, taper slowly while using other support.
Some herbal formulas I like are:
- Bowel Mover
- Digestive Stimulator
- Cleanse More
Smooth Move tea is another herbal option to help with constipation relief. It also contains Senna, so only use it occasionally and work with your functional medicine provider to uncover and address the root causes of your constipation.
Probiotics for Constipation
In choosing a probiotic supplement, avoid formulas that have too high a level of fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), inulin, chicory, or arabinogalactan. These ingredients at too high a level can cause a flare in imbalanced gut microbiota. If you have a gut infection, wait until it is cleared to take any supplements with those ingredients.
Some probiotics for constipation that I like:
Test one species first. Start with about 40 billion and then ramp up as far as 300 billion by doubling your dosage every three days. Stop if your symptoms worsen.
Critical Tests If You Have Chronic Constipation
As you read earlier in this article, there are a lot of causes of constipation. Some of them could be damaging more than just your GI tract. That’s why it’s important to test for parasitic and other gut infections, Candida and fungal overgrowth, and an imbalance in the gut microbiota. Depending on the specifics of your case, we might choose to use the GI-MAP, the Parawellness Stool Pathogen panel, or the BiomeFX panel. We might also include Lactulose and Fructose Breath Testing for gasses that can indicate SIBO.
You really don’t want to tackle these types of gut imbalances on your own. Instead, book a free 15-minute troubleshooting call with me to find out the best course of action. If after the call you come on board as a patient, I’ll order the right tests, recommend a plan customized for you, and put you on the path to feeling like your regular self again.
A Functional Medicine Approach to Healing IBS
So, your doctor says you have IBS - Irritable Bowel Syndrome.
This diagnosis can either feel like a relief or a nightmare.
On the one hand, an IBS diagnosis means some of the causes of digestive issues like Crohn’s, Ulcerative Colitis, and Celiac disease have been ruled out - that’s a good thing.
But on the other hand… IBS is essentially a name for “something’s wrong but we don't know what.”
And in the functional medicine, holistic approach I use - that’s not a good enough answer. In fact, it's not an answer at all!
An IBS diagnosis leaves people to suffer through their symptoms alone - which is bad enough - but even worse, it ignores the root cause of the issue.
And because the gut is so integral to overall health, issues in your gut inevitably lead to more health issues - hormones, mental health, weight concerns, thyroid issues, and more.
So why do we accept this? Why do doctors tell you that you “just” have IBS and send you out the door?
Because treating IBS isn’t easy! There’s no one pill that can fix it, because no two people have the same causes. It requires a multi-step, hands-on treatment approach that usually needs to be tweaked in real time. That’s not the kind of care most standard MDs are able to provide.
Don’t worry - I got you! Today I’m going to share my approach to treating IBS.
But buckle up, because this isn’t a quick 3-step process (sorry!). Today, we’re diving deep into the nitty gritty of treating one of the trickiest conditions out there.
You’re Entitled To More Than One Problem
In Chinese medicine school, I often heard the saying “You’re entitled to more than one problem at the same time.” This was the tongue-in-cheek way of saying it’s the norm, not the exception, for a patient to have multiple contributing factors to any health challenge they faced.
And this is especially true in the case of IBS because the gut is so intricately connected to every part of the body, but also because one gut issue - like inadequate digestive secretions (due to stress, medications, etc.) - can create the environment for another problem to arise.
That’s why the treatment plan I use for IBS has a lot of steps. Because you may have low stomach acid, or bacterial overgrowth, or a parasite… but that’s more than likely not going to be the only issue you’re dealing with. Instead of obsessing over discovering the one root cause of your IBS, my approach works systematically through the most common issues, creating a powerful foundation for lasting health.
So let’s peel back the layers, step-by-step, and tackle this together.
Start From The Top and Work Down
Most people don’t think of it this way, but the mouth is actually the start of the gut. The mouth has its own microbiome that directly influences the composition of the large intestine microbiome. In fact, research has shown that simply brushing your teeth 3x daily can measurably lower levels of candida in the stool.
94% of Americans have some degree of gingivitis and the mouth and sinus are home to fungal strains including Candida species (present in 75% of participants), followed by Cladosporium (65%), Saccharomycetales (50% for both), Aspergillus (35%), Fusarium (30%), and Cryptococcus (20%). In addition, gram negative bacteria such as Enterococcus faecium, E faecalis, Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis are also common in the mouth. These are the same bacteria most commonly overgrown in cases of Small Intestine Bacterial Overgrowth (SIBO).
The best defense is controlling bacteria levels in the mouth with your oral hygiene routine. I recommend Dentalcidin toothpaste and Biocidin Dental Rinse as an important first step for anyone with dysbiosis or candida, SIBO, IBD, IBS, gas that clears the room, or a history of poor dental health.
Optimize Your Gut Terrain
Once you’ve got your new oral hygiene routine in place, the next step is to optimize your gut terrain and environment.
Before we ever run a stool panel, clear a pathogen or take those precious leaky gut supplements, and especially before we start going down side rabbit holes like mold, we need to replace any missing digestive secretions and work on meal hygiene and transit time. This literally sets the stage for a healthy gut.
Digestive secretions include stomach acid (HCL), bile, and pancreatic enzymes. HCL is secreted by parietal cells in the stomach in response to the smell and taste of food, as well as distension in the stomach and small intestine (distention occurs when food enters the stomach).
HCL is particularly important for the breakdown of protein. Most importantly, however, HCL acts as the first domino for all the other digestive secretions. Without adequate HCL, all other secretions will suffer!
The #1 reason for inadequate HCL? Stress. HCL release is triggered via the vagus nerve which connects the brain and the gut. Vagus nerve activation requires a parasympathetic state of the nervous system. You might know this as the “rest and digest” mode. Eating while stressed, busy, or otherwise unfocused is therefore a major cause of low HCL. Other causes include the use of PPIs and other acid-blocking meds, as well as the presence of certain bacteria in the gut like H. pylori, which can denature HCL.
Adequate HCL then triggers the release of bile from the gallbladder. Bile is necessary for the digestion of fats, but bile also acts as an antimicrobial in the small intestine, helping to prevent bacterial overgrowth. Bile also collects toxins for the liver to secrete. Bile levels can be impacted by inadequate HCL, dehydration, gallbladder issues or removal, and exposure to high levels of toxins. If bile is inadequate it can lead to dysbiosis of the microbiome and deficiencies in fat soluble vitamins like A, D, E, and K and nutrients.
Pancreatic enzymes are secreted by the pancreas and play key roles in breaking down carbs like sugar and starches as well as fats. Pancreatic enzymes allow starches to be broken down in the small intestine, rather than fermented, preventing bacterial and fungal overgrowth. Pancreatic enzymes act as a bactericidal against Escherichia coli, Shigella species, Salmonella species, and Klebsiella pneumoniae, and have fungistatic activity against Candida albicans. The release of pancreatic enzymes is dependent on adequate HCL.
HCL, bile, and enzymes can all be supplemented if needed, but there are other things you can do as well. First up, make sure you’re hydrated. Proper hydration is necessary for the production of digestive secretions - think of water as the key ingredient. Secondly, slow down and really chew your food. Thorough chewing allows time for the brain to signal the gut that food is coming, and the gut to secret HCL and bile in response.
With my one-on-one clients I utilize gut testing to check enzyme levels, and often supplement HCL, bile, and enzymes as needed.
What About Probiotics?
I tell my clients to introduce fermented foods as tolerated - even if that’s only a single strand of sauerkraut to start.
Beyond that, certain probiotics can be really helpful. Some strains support secretory IgA, which protects the mucosal barrier of the gut. Those include spore based probiotics, S. boulardii, L. plantarum, L. Reuteri, and B. lactis.
Generally well-tolerated probiotics include OrthoSporeIG, or MegasporeBiotic. For those who are highly sensitive, you may want to start with HU58 instead, which is a single spore organism.
Probiotics can also support specific symptoms of IBS. For diarrhea, S. boulardii works well. I like Floramyces. For constipation, Optibac (1-4 doses per day) or HN019 strain of Bifidobacterium lactis (Xymogen’s Probiomax) are my favorites. BioGaia Protectis drops, which contain Lactobacillus reuteri DSM17938, are my favorite for bloating. And in general, many IBS patients benefit from Ideal Bowel Support which contains L.plantarum 299V.
Address Motility & Transit Time
Addressing motility and transit time goes hand-in-hand with optimizing the terrain of the gut. Bacteria in the gut bloom like a coral reef after meals. If food and bacteria are moving through the gut and into the large intestine, that’s a great thing. But if food isn’t moving as it should, bacteria can bloom in the small intestine, and that’s a problem.
Bacterial overgrowth in the small intestine (SIBO) is a factor in as many as 80% of all IBS cases. (That being said, it’s not the only cause of IBS. I see it more often as a contributing cause - more the “branch” than the “root” of IBS!)
Motility is controlled by the migrating motor complex (MMC), an electrical wave that originates in the brain via the vagus nerve. The MMC acts like a broom, sweeping food and bacteria through the small intestine and into the large. Many factors can contribute to a deficient MMC, including bacterial overgrowth itself, which can secrete toxins that disrupt the vagus nerve.
To improve motility, I use prokinetics (not to be confused with laxatives), which help trigger normal MMC function, as well as other approaches to keep bowels moving regularly. But if motility issues are chronic, it’s a sign of an impaired gut-brain axis. Modalities that can heal the gut-brain axis include:
- Neuroplasticity
- Biofeedback
- Frequency Specific Microcurrent
- Vagal nerve stimulation
- Acupuncture
- Therapy like EMDR, or somatics for trauma
Nutrition Based On Symptoms
Once the gut terrain and motility have been addressed, it’s time to look at your diet. For all my clients dealing with IBS or other gut issues, I have some basic diet recommendations:
- Paleo or Autoimmune Paleo as a foundation
- Focus on nutrient dense foods, including gut-healing foods like bone broth, 24-hour yogurt, and sauerkraut (just start small)
- Gluten, dairy, and added sugar-free
- Avoid eating the same foods day after day - variety is key
- Stay well hydrated
- Practice good meal hygiene (sitting down to eat, avoiding screens while eating, slowing down, chewing thoroughly)
- Incorporate fermented foods as tolerated (start really small)
- Incorporate fiber-containing plants as much as tolerated
While many people want to skip these simple diet changes, they matter. It’s a foundation, not an aside. You will not get better if you’re only eating gluten free toasted waffles, even if you tolerate them well! By the same token, if you’ve found you can stay symptom-free by eating a very limited diet, we eventually need to expand your phytonutrients and nutrients in general if you want to actually get better (and enjoy eating again!).
For those patients with more specific concerns, I do often trial special therapeutic diets like the Specific Carbohydrate diet (SCD), low-FODMAP, or low histamine. Having diarrhea 15 times per day? Try the SCD Diet. (Just make sure you don’t skip the essential Intro phase!) Tons of bloating, belching, and some loose stool or constipation? I’d suggest a low-FODMAP trial. And for those with lots of rashes, headaches/migraines, hives, itching, anxiety, insomnia, brain fog, sudden episodic diarrhea after meals, and allergies with foods, I will try a low histamine diet. (And some may need to take it a step further and follow low nickel - especially if rashes or eczema are present - or have salicylate or oxalate intolerances as well.)
And Now We Test
You might be surprised to see that only now am I considering testing - stool testing, breath tests, or even hormone panels. The truth is that there is so much to work on long before any labs need to be ordered. And for some people, simply improving the health of the oral microbiome, optimizing the gut environment, and making some nutrition changes are all that is needed to completely resolve symptoms! I too often see people on fancy gut protocols, who aren’t getting results, simply because they have addressed the foundation first! Bottom line: don’t skip ahead!
But once we’ve covered the basics, testing can provide invaluable information that leads us forward in the right direction and saves you a ton of wasted time, energy, and money.
My two essential tests are multiple stool panels and hormone testing. In addition, I often find breath testing for SIBO, organic acids tests, and food sensitivity testing to be valuable tools, as well.
Why You Need Hormone Testing for A Gut Problem
It might seem odd if your symptoms are all in your gut, but hormone testing is a must-have tool for treating IBS. Why? Because your struggle with inflammation in the gut, and your ability to resolve it, is to some extent limited or empowered by how harmonious and optimized your hypothalamic–pituitary–adrenal (HPA) axis is. Cortisol, the primary “stress hormone” whose production and release is controlled by the HPA axis, is like your own endogenous prednisone. If cortisol levels are sky high, or have tanked and are too low, the body can’t repair tissues (like leaky gut) or resolve inflammation. Trophic hormones like DHEA are also essential for tissue repair. Stress and cortisol also inhibit secretory IgA, the most important immunoglobulin for repairing the mucosal barrier of the gut. I think of secretory IgA like the immune system of the gut.
Most of my clients have some level of hormone dysfunction - but once we know what it is, we can take active steps to mitigate it. I recommended actively addressing stress and trauma with tools like therapy, EMDR, vagal nerve stimulation, and tools like the Gupta Program or the Inaura platform.
Order These 2 Stool Tests
I always use two stool tests to detect pathogens like H. pylori, fungal overgrowth, and parasitic infections. Right now my favorites are GI Map and Parawellness. To get started, I prefer to use tests that focus on identifying pathogens vs. microbiome tests like BiomeFx or the Genova Panel. While general microbiome wellbeing is incredibly important, if pathogens aren’t first tested and cleared, they will usually impede any improvements to the health of the microbiome. (That said, I do love the BiomeFX for really targeted rebuilding of the beneficial microbiome after we’ve “weeded” the garden!)
That being said, the microbiome is essential in understanding why pathogens are a problem for some people but not others. It’s not just about what pathogens are present, but how your body responds to the pathogen. This is akin to the concept in Chinese medicine of Wei Qi. Wei Qi has its roots in the Kidney Qi (your core energy, or how strong you were when you came in, based on genetics, and how well you’ve nurtured that with nutrition, lifestyle, and exposure).
Wei Qi is the concept that the hand of cards you were dealt (genetics), under the influence of the exposures you’ve had or lifestyle you’ve chosen or been able to afford = your resilience. You might have also heard of this concept as “epigenetics.” Chinese medicine practitioners have been talking about it for 5,000 years!
Pathogens can shift or suppress the immune system, increasing susceptibility to SIBO and other opportunistic dysbiosis. Parasites and gut infections degrade the protective lining of the gut, called the mucin lining, to decrease secretory IgA levels. They do this to stay alive: they need to degrade the immune system in the gut to prevent being destroyed.
In addition, many parasites can mimic or directly trigger IBS or Inflammatory bowel disorders including Giardia lamblia, Entamoeba histolytica, Cyclospora, and Cryptosporidium. In one study, blastocystis infection was found in 67% of IBS patients, and other research found that the prevalence of blastocystis, cryptosporidium and giardia is higher in IBS patients than in controls, and likely play a role in the development of IBS.
If you’re thinking, “There’s no way I have a parasite,” think again! Risk factors include simple things like travel outside the U.S. and swimming in lakes/oceans/rivers. Lots of food intolerances - or food intolerances that change frequently - are also a warning sign for parasites, as parasites are able to “switch” the immune system from innate immune response (the TH1 immune system) to the “food allergy” response (TH2 immune system). Many people report no obvious symptoms. That’s why I test everyone, across the board.
Creating Your Custom Treatment Plan
One we have test results in hand, it’s time to create your customized healing strategy. While no two cases of IBS are the same, there are some general rules I follow:
#1 Start With H. Pylori (If Present)
Because H. pylori breaks down stomach acid, as well as “partners” with and encourages other pathogens, if it is present, it’s where I start. (H. pylori also promotes histamine synthesis and can contribute to histamine induced symptoms).
#2 Clear Other Pathogens
Once H. pylori has been addressed I move down the list of parasites such as Endolimax nana, Giardia, Entamoeba coli, Entamoeba histolytica, etc.
#3 Candida & SIBO
Next, I like to tackle candida overgrowth and SIBO. I often clear candida first, especially in the case of methane-dominant SIBO, because there is a strong association between candida and methane SIBO, and the SIBO often won’t respond to treatment unless the candida is cleared first.
#4 Find & Treat Other Factors (If Needed)
If candida is not clearing after appropriate clinical steps, or, if SIBO won’t resolve after appropriate treatment, I look “further down the rabbit hole” for other things that could serve as impediment to those resolving like:
- Heavy metals burden
- Mycotoxins (Mold exposure)
- Other biotoxin issues like Lyme and tick-borne diseases, chronic viral infections
(And if a patient has a known history with these - like a mouthful of mercury amalgam fillings, or once lived in a moldy apartment, or known tick bites - I skip ahead and test for these issues earlier.)
Let’s Talk About SIBO
Like I mentioned earlier, SIBO is an underlying cause of IBS in as much as 80% of cases. But that doesn’t mean SIBO is the only cause of your IBS. SIBO is often just one aspect of a bigger set of issues. In fact, I often see patients who have had four or more rounds of SIBO treatment and still have symptoms. Why?
Often it’s because they have other parasites or pathogens that haven't been treated. Another common reason is that they actually have SIFO - small intestine fungal overgrowth. A 2015 study showed 25% of patients with unexplained GI issues actually had SIFO. SIFO symptoms are the same as SIBO symptoms, but common SIBO treatments like rifaximin and neomycin are just fuel on the SIFO fire. SIFO can be treated, too - it just requires a different treatment.
Exceptions to the Rule
Now you know my basic treatment approach for IBS - but there are some exceptions. If someone is too overburdened, run down, or “weakened”, by what they’ve endured in body burden, often combined with a lifetime or period of high stress, sleep deficit, limited nutrition (because of what they can’t tolerate, or what is available), and poor assimilation, and are running on a deficit - they may need a different approach.
In these cases, a person may be too vulnerable to tolerate pathogen removal, either because it would leave them more vulnerable to another pathogen, or damage the microbiome itself. (Even natural agents can cause damage - looking at you, Oregano oil!)
A few weeks of support for healing gastritis, esophagitis, or leaky gut prior to digging in to increasing enzymes or HCL levels or endeavoring to clear a pathogen can make all the difference. They may also need several weeks of gentle detox support. I might use Chinese herbs, immunoglobulins and/or probiotics for secretory iGA support, or treatments aimed at supporting HPA Axis normalization. I think of this as strengthening Spleen (digestive) Qi and Wei Qi.
Retest, Rebuild, Revitalize
We’ve already covered a lot, but we’re not done yet. In fact, these three final steps might be the most important. Please don’t skip them!
#1 Retest
Once we’ve completed our first round of treatment, it’s time to retest. Failure to retest is the most common reason people relapse after treatment. Yes, it really is worth the time and money! Retesting gives us insight into how you responded to treatment, if further treatment is needed, or if problems have been resolved. The only exception to this is SIBO testing: if your SIBO symptoms are 90% or more resolved, we often don’t need to retest, because SIBO doesn’t always look perfect on paper.
#2 Repair & Rebuild
We have already started the process of improving the gut terrain and environment. Now is the time to kick it into high gear and increase both probiotic and prebiotic foods. These help “bulletproof” the microbiome, preventing future infections and problems. Now is also the time to add supplements for anti-inflammation and leaky gut repair (butyrates, glutamines, curcumins, immunoglobulins, prebiotics, probiotics, nutrients like vitamins A, D etc).
This is also the right time to utilize advanced microbiome testing like BiomeFX. We can use that information to focus on further diversifying the microbiome, because diversity is strength.
#3 Revitalize
Finally, I focus on detox support, nutrient replacement, and optimization of other systems that may have been impacted as innocent bystanders of the gut issues. Using an organic acids panel like ION, I take a look at liver detox, antioxidant status, amino acid status, neurotransmitter status, leaky brain, skin, and lungs, mitochondria and metabolism, and inflammation throughout the body.
Even if you do every other step in the process, missing this one is like missing the icing on the cupcake. (I know, bad analogy for someone practicing nutritional medicine, even if it’s a gluten free, sugar free cupcake!).
This step is WHY we bother doing the rest. You set out to clear your IBS because you don’t want to run to the bathroom 10 times per day. You don’t want to struggle to get to sleep, stay asleep, think clearly, or deal with rashes or autoimmunity. You don’t want an overburdened detox system and excess oxidative stress to cause you to age prematurely. But clearing the gut and supporting the microbiome will only get you part way to relief (very far, but not entirely).
For long term resilience and vitality, here’s what else I’m looking at:
- Replacing missing nutrients
- Supporting detox pathways
- Glutathione status
- Ability to optimally metabolize (aka use for energy) carbs, fats, and proteins,
- Omega fatty acid balance
- Mitigating inflammation
- Supporting mitochondrial function
- Lowering oxidative stress
- Optimizing brain function
Healing IBS Is A Journey
In case you haven’t picked up on it yet… healing IBS isn’t a “quick and easy” process. But most things that are really worth it in life take time and effort. You likely are not going to see impressive results by just taking a few supplements or cutting gluten from your diet.
But that’s not a reason to get discouraged. Trained practitioners like myself have years of experience, working with thousands of clients.There’s nothing more gratifying than helping a patient - especially if that patient feels they have tried “everything” - peel back the layers of their IBS one by one and finally find relief!
If you need support healing IBS, I want to invite you to book a complimentary, no-obligation chat with my team. We’ll hear your story and let you know how we think we can help.
>>> Schedule your free consultation here
Living with IBS is hard. You don’t just have to accept this as your normal. We would love to help.
How to Prevent SIBO (Small Intestinal Bacterial Overgrowth) Relapse
You have SIBO (Small Intestinal Bacterial Overgrowth) and you completed all the necessary steps in the “kill phase” of treatment. You run a follow-up breath test and your gas levels have normalized! Or, you didn’t retest, but your symptoms are 90% better! This is great progress and it feels like you are finally moving forward!
But, if you’re just killing the bacteria – you’re only halfway there!!
Many SIBO patients get their initial SIBO treatments and feel good for a while. But then, all the bloating, gas, cramping, constipation, or diarrhea begin to make a very unwelcome comeback. For various reasons, too much bacteria will once again start colonizing the wrong part of the GI tract leading to SIBO relapse.
Unfortunately, it’s common to have SIBO relapse. But, don’t get discouraged. You’re not wading through the murky waters of SIBO treatment alone.
Let’s break down if your symptoms are IBS or SIBO, why SIBO relapse might happen, what you can do, and how to help prevent a relapse in the first place.
Are my symptoms IBS or SIBO?
When it comes to gut issues, it can be difficult to identify and understand your symptoms. In general, there are two common conditions of the intestines that can present very similarly: Irritable Bowel Syndrome (IBS) and SIBO.
IBS is a functional gastrointestinal disorder. It affects the two-way communication between your digestive system and your brain. When this communication system malfunctions it can throw off your entire digestive tract. Leading to symptoms like abdominal pain, bloating, and altered bowel habits such as constipation or diarrhea. Sounds a lot like SIBO, doesn’t it?
A single underlying cause of IBS has not been identified. But honestly, there are many factors that could lead to IBS including food sensitivities, severe infections, stress, or intestinal muscle issues. What’s interesting is that up to 78% of patients diagnosed with IBS have SIBO.
IBS and SIBO are complex conditions. But, since these conditions can present so similarly it’s important to rule out SIBO with a breath test so that we can customize your treatment plan.
What causes SIBO relapse?
I know what you’re asking…if I’ve done the work to identify the cause of SIBO and the SIBO treatment…why on earth is my SIBO coming back?!
Unfortunately, approximately 45 percent of all SIBO patients will experience a SIBO relapse. There are three primary reasons that my patients experience SIBO relapse: diet, underlying gut conditions, and medications.
Diet
Let’s call it like it is, diet changes are never a quick fix, they are a lifestyle change. A diet that is high in sugar, refined carbohydrates, FODMAP vegetables, or alcohol can make SIBO symptoms like gas, bloating, constipation or diarrhea worsen or relapse. It’s important to introduce foods like starchy veggies in the long run because it feeds the good gut flora. But introducing too much too soon is when you run into issues.
Underlying Gut Conditions
A physical obstruction in the gut can be both a cause of SIBO and subsequently the cause of SIBO relapse. Crohn’s disease, celiac, diabetes, and leaky gut are the four most common gut conditions that can cause SIBO.
Medications
Some medications may help with certain issues while wreaking havoc on others. Medications like antibiotics, antihistamines, NSAIDs, acid-blocking drugs (PPIs), and steroids all disrupt your normal gut flora. Some kill healthy bacteria and others increase the permeability of your gut. But, they all increase your chance of SIBO relapse.
How To Prevent SIBO Relapse
Preventing SIBO relapse starts during the “kill” phase of your SIBO treatment. There’s a lot you can be doing during and after SIBO treatment to prevent SIBO relapse. Here are a few things I like to include in SIBO treatment plans:
- Address Low Stomach Acid and Pancreatic Digestive Enzymes – These antimicrobial enzymes help enhance nutrient absorption and assimilation.
- Support your Oral Microbiome – 94 percent of Americans have some levels of gingivitis or bacteria in their oral cavities that can impact gut health. I recommend Blocidin toothpaste and dental rinse. Plus, don’t forget about flossing. Sorry, no water picks.
- Liver Support – The toxins from SIBO have inundated your liver. The endotoxins (the toxic substances bound to bacterial cell walls) from having SIBO saturate the bile and add to your total liver toxic burden. These systems need their own love to get back up to speed. Resolving the excess gram-negative bacteria is the first step. My favorite for bile support is MegaGuard by Microbiome Labs. Learn more about bile support and gut health.
- Repair Leaky Gut/Mucosal Inflammation and Damage – SIBO has likely led to an inflamed gut and has damaged the cellular walls and lining. Not only do you need to kill off harmful bacteria and rebuild healthy gut flora, but you also need to repair any structural damage. I recommend Super Curcumin by Apex, with either MegaMucosa by Microbiome Labs, or GI Balance by Xymogen.
What To Do After You’ve Cleared the Bacteria Causing SIBO
The first phase of SIBO treatment is tough and you’ve survived it. Congratulations! But now what?
Great question! There is a lot you can do after SIBO treatment to prevent relapse and stay healthy.
- Stay on a modified low FODMAP or SIBO Biphasic. To allow your microbiome to heal, I recommend following one of these diets for two to three months, followed by gradual reintroduction of foods that you have omitted.
- Add a Prokinetic to address gastroparesis and support the Migrating Motor Complex (MMC). Gastroparesis slows your stomach’s motility preventing it from emptying properly. MMC sweeps residual bacteria and leftover carbohydrates and protein particles out of the small intestine. Waiting 4 hours between meals allows MMC to work because it is only triggered during a fasted state. So, if we snack all the time or chug large amounts of liquid, we’re inhibiting the MMC housekeeping wave. Limit snacks and sip, don’t chug, your fluids. So remember, eat, stop, eat.
- Restore your vagal tone and your MMC by retraining your nervous system signaling. All of the approaches to restoring vagal tone for improved digestion focus on promoting your parasympathetic nervous system activity, over your sympathetic activity. The parasympathetic nervous system helps restore the body to a calm and composed state and prevents it from overworking. Sympathetic activity, on the other hand, prepares the body for a stress-related activity. Depending on what may be causing your sympathetic activity several techniques can be personalized based on your symptoms. This includes vagal nerve stimulation, gut-focused hypnotherapy, Frequency Specific Microcurrent, acupuncture, or the Gupta Program. And, if there has been a big stress or trauma other treatments like EMDR can be considered. Check out inaura.com to identify additional personalized therapy options.
- Add single-strain probiotics and prebiotics to your daily routine. Probiotics and prebiotics, added slowly to your diet, can help to rebuild and maintain your healthy gut flora. Because multi-strain probiotic blends are not generally tolerated by SIBO patients I recommend several single strain options based upon your specific symptoms and tendencies (i.e. bloating, constipation, diarrhea, histamine intolerance, etc.). I personalize your routine with some of my favorites including HU 58 (Microbiome Labs), BioGaia Protectis, probiomax by Xymogen, and Ideal Bowel Support (L Planetarium 299V). I start all my patients on a partial dose and work up to help bulk the stool without triggering SIBO. Once you are tolerating partial doses, we can reintroduce most FODMAP foods along with other strains of probiotics for continued gut repair. The key is going slow and steady. Adding any probiotics too soon or too quickly can flare SIBO.
To get you started, let’s focus on diet, probiotics, and prebiotics.
SIBO Treatment: Low FODMAP Diet and SIBO Biphasic Diet
Many of my SIBO patients hit the internet and find a lot of information on the “SIBO diet”. The SIBO diet is also known as a low FODMAP diet.
I recommend following a low FODMAP diet during SIBO treatment and for a short time after. But, in the long haul, a low FODMAP diet can be too restrictive. It does not offer you the necessary food diversity required for a robust and diverse microbiome. But, after the initial treatment, you can slowly reintroduce foods that will support your gut health and regularity.
Some patients also have a lot of success with a SIBO biphasic diet. This diet plan is as restrictive as the low FODMAP diet to start. But, it slowly reintroduces the most tolerated and least fermentable foods back in overtime. The foods eliminated don't change on the biphasic diet. Instead, it provides more guidance on what foods to reintroduce and when.
In reality, diet does not cause SIBO. Period. Diet can cause many other things like candida and poor microbiome health, but SIBO isn’t caused by diet. Instead, a highly-processed, low-quality diet tends to lead to increased symptoms and SIBO relapse. Diet is simply a way to manage your SIBO symptoms during the kill phase and long-term. And, it’s unique to each patient. Whether you follow a low FODMAP or biphasic diet, your SIBO treatment should include a full evaluation of your diet to help manage and control your symptoms.
Benefits of Probiotics and Prebiotics
I know it sounds strange, but utilizing probiotic and prebiotic supplements in the treatment of SIBO can be beneficial. It seems counter-intuitive. If excess bacteria in the small intestine cause SIBO, why would you want to add more?
Probiotics help to reduce bacterial overgrowth and hydrogen concentrations. And, probiotic supplements can help improve symptoms and restore a healthy gut microbiome. Which in turn increases your resilience against SIBO or general dysbiosis by promoting healthy expression of gut immunity and maintaining a strong and resilient mucosal membrane.
Prebiotic supplements, on the other hand, essentially provide the nutrients needed for healthy bacteria to flourish in your gut.
Ongoing research shows that probiotic and prebiotic supplements can be very effective in the treatment of SIBO. They can help improve symptoms, improve lab values, and support long-term gut restoration. Yet, not all probiotics and prebiotics are equal. It’s important to introduce the right supplements to focus on helping resolve your specific issues slowly and only as tolerated. Too much, or the wrong things can lead to SIBO relapse if the body isn’t ready. Generally, I start with PHGG (Partially Hydrolyzed Guar Gum) and Acacia.
Get Help With SIBO Relapse
SIBO is an incredibly complex condition that requires a great deal of time and energy to resolve.
Every case of SIBO requires personalized treatment. And as your health guide, we're here to put the pieces of your puzzle together and get you back on track. You deserve to live your life freely and feel well every day!
So, if you find yourself feeling defeated in your journey to better gut health, we are here to help!
Start by scheduling a no-cost, no-obligation 15-minute consultation call to regain control of your health.
References
"Probiotics for Preventing and Treating Small Intestinal Bacterial ...." https://pubmed.ncbi.nlm.nih.gov/28267052/. Accessed 10 Feb. 2022.
Is Toxic Mold Illness to Blame for Your Digestive Problems?
It’s frustrating. You’ve got digestive problems but you’ve hit a roadblock in the healing process.
Maybe you have irritable bowel syndrome (IBS).
Or maybe you have small intestinal bacterial overgrowth (SIBO).
But you’re not getting any better.
Newsflash: there’s one thing you probably haven’t tried to get rid of your digestive problems. I’m talking about toxic mold exposure.
The Fungus Among Us
Mold is a type of fungi and it’s everywhere around us. It’s in water-damaged homes, on the tiles of our showers, in the soil of potted plants—even in some of the foods we eat.
Really gross, isn’t it?
Well, yes and no. Molds certainly won’t win any beauty contests. Yet, they serve their purpose on this planet. They’re essential to the breakdown of organic matter like fallen leaves or dead trees.
There are thousands of species of molds. Many of them are harmless to your health. But some molds produce health-harming mycotoxins.
I have made great strides with my IBS and SIBO patients once I realized many of them have symptoms of mold sickness. This isn’t the root cause for all of my patients, but in the people who have mold exposure, resolving the problem can lead to major breakthroughs in their health.
In this article, I’ll dive deeper into the issue of mycotoxin exposure and how it can wreak havoc on your digestive health. I’ll also give you some suggestions on what you can do about it.
What Are Mycotoxins?
Mycotoxins are substances produced by some molds, usually when the mold feels as if it’s in danger. Kind of like the way a spider or snake shoots out venom when threatened.
While mycotoxins are good for the fungus, they’re not so good for our health. Mycotoxins are to blame for mold symptoms and are real troublemakers for digestive health.
Some mycotoxins are found in foods and beverages:
- Mycophenolic acid, found in Bleu cheese
- Ochratoxin, found in cereals, cocoa, coffee, wine, beer, spices, dried fruit, and grape juice.
- Aflatoxin, found in cereal crops like corn, wheat, and rice, peanuts, eggs, meat, and milk from animals fed contaminated grains.
One of the most common sources of exposure is from coffee mold, which produces mycotoxins in coffee. Ochratoxin A and aflatoxin B1 are the main mycotoxins that might be found in your daily cup of Joe.
Some mycotoxins are found in buildings, especially those produced by black mold:
- Trichothecenes made from the mold called Stachybotrys (black mold)
- Ochratoxin, which may hide out in wallpaper, furniture, and fiberglass insulation.
Research suggests that up to 50% of buildings in North America and Europe have water damage that can lead to mold infestations. This has to do with how we build buildings. We wrap them in plastic and use materials that are susceptible to water damage and mold growth.
What’s more, the mold could be lurking in your home without you even knowing it’s there. Creepy, yes? It’s sometimes good at hiding because not all mold causes that yucky musty smell.
Black mold is the one many people think about when they hear about toxic indoor mold. That’s because it’s one of the most common toxin-producing molds. Black mold symptoms include those mold toxicity symptoms I mention later in this article.
Black mold may be one of the most common — and grossest – molds many people are exposed to, but it’s not the only one that causes issues in people with digestive problems.
Here are some other mycotoxin-producing molds that can cause mold toxicity symptoms:
- Aspergillus
- Chaetomium
- Cladosporium
- Fusarium
- Mucor
- Penicillium
- Rhizopus
- Wallemia
When inhaled or ingested by humans, mold-made toxins can do a real number on the health of susceptible people.
When Mold Meets Your Immune System
When exposed to mold, your body can react in one of two ways:
- Mold allergy – This is a reaction by the immune system to the mold itself. Think runny nose, red eyes, itchy skin.
- Mold illness – Unlike mold allergies, mold illness causes problems throughout your body. Mold illness can cause widespread inflammation called chronic inflammatory response syndrome (CIRS), otherwise known as biotoxin illness. CIRS can be caused by other factors, but when it occurs together with a known history of mold exposure, odds are mycotoxin exposure is playing a role in this inflammatory illness.
CIRS is also linked to food sensitivities and intolerances. There’s also a connection between CIRS and hypersensitivity to chemicals and other substances that never bothered you before you were exposed to mold.
Symptoms of Toxic Mold Exposure
After exposure to toxic mold, your body may react by developing certain symptoms. In some people, these can be crippling. I’ve treated people exposed to mold who almost couldn’t function. Often, they couldn’t think straight to the point it was very hard for them to even follow my protocol for healing. Many of them had severe pain, nervous system, and/or immune system problems.
Other mold-exposed people have vague symptoms that are milder or come and go.
Here are some of the common symptoms of mold exposure:
- ADD/ADHD
- Anorexia
- Asthma
- Body aches and pains
- Chronic fatigue syndrome
- Depression
- Digestive problems
- Headaches, especially migraines
- Histamine-related symptoms
- Hives
- Hormone imbalances
- Hypersensitivity to foods, chemicals, and other items that didn't previously bother you
- Insomnia
- Immune system dysfunction
- Memory/learning problems
- Mood disorders
- Poor word recall
- Pulmonary diseases
- Rashes
- Sinus symptoms
- Unwanted weight loss
- Weight gain
Are You Susceptible to Toxic Mold Syndrome?
Just because you’re exposed to mold doesn’t mean you’ll develop any symptoms of mold poisoning.
Some people can live in a super moldy home, where the mold is actually visible, and yet not experience a single symptom.
So you’re wondering why you’re not one of those lucky people. Maybe you’re extremely sensitive to mold exposure. You live in the same building with others who are perfectly healthy, yet you’re sick. This can be because:
- You’re exposed to more mold (you have a higher body burden or toxic load).
- You’ve been exposed for longer.
- Your genetic makeup. Some genes boost the susceptibility to mold toxicity by 24%.
- Your immune system doesn’t identify and clear mold toxins as easily as someone else’s does. In this case even smaller overall exposure levels can harm your health.
Other reasons why some people are more susceptible to mold sickness than others:
- Type of mycotoxin you’re exposed to
- Age
- Gender
- Health status
- Nutritional status
Mold and IBS
Digestive problems don’t always come to mind when thinking about mold toxicity. Yet, mold exposure can cause major problems in your digestive tract.
Mycotoxins can declare all-out war against the good bacteria in your intestines. This causes the bad bacteria to take over.
The result? Constipation, diarrhea, and abdominal pain. Leaky gut also often develops when mycotoxins damage the gut barrier. In leaky gut, undigested food particles or toxins from the outside world leak through your gut lining into your circulation, causing problems not only in your gut, but also throughout the body.
The opposite of this is also true. If your gut microbiome – the population of good and bad microorganisms that live in your intestines – is well balanced with just the right amount of good little guys, it will make you less susceptible to mold-related digestive problems. They can also protect you from mycotoxins.
Mold Makes Life Easy for SIBO
Mold can open the door to infections of the gut by reducing immunity. Toxins from black mold are linked to a drop in levels of a substance called IL-8 in the intestine that helps remove pathogens. This leads to infections in the gut.
SIBO happens when there is an abnormal rise in the overall bacterial numbers of the small intestine – especially types of bacteria not usually found in that part of the body.
In fact, many cases of SIBO are really post-infectious IBS that occur after a person has experienced food poisoning. If mycotoxins are present, your small intestine is even more vulnerable to this type of infection.
That means mycotoxins can make you more likely to develop SIBO. And they get in the way of healing this disorder.
Your functional medicine provider can order the right tests to diagnose whether you have SIBO.
Testing for Mold Exposure
If a patient with digestive problems has symptoms of mold exposure or has a known exposure to mold, we will order the Great Plains Laboratory or RealTime Labs Mycotoxin Panel.
There’s also visual contrast sensitivity testing (VCS), which was originally created by the department of defense to find out if soldiers had been exposed to biotoxins. You can take a VCS test online. It costs only $15.
If the mycotoxin panel indicates you have mold exposure, we’ll order blood work to measure how much inflammation the mycotoxins are causing in your body. We’ll order the same blood work to monitor and measure your progress with treatment.
Treatments for Mold Exposure
Here is what we do to treat IBS and SIBO patients who have mold toxicity. With this protocol, we’ve had excellent results clearing roadblocks to healing.
- We urge patients to leave the mold-contaminated environment for several weeks, or until the area can be decontaminated or remediated….lots of outside time is helpful!
- Remediate your home or office. Use a professional IEP (independent environmental professional) and make sure they check the HVAC system for mold.
- Have your home/car/work spaces assessed by trained professionals and also use an ERMI test to make sure your spaces have low enough mycotoxin levels to allow you to start treatment.
- Treat and clear GI parasitic pathogens first and improve the health of the microbiota through the use of probiotics. These beneficial bacteria are your gut’s best friend. Many strains of probiotics can reduce the level of mycotoxins by binding to the toxins and boosting the immune system.
- Usually wait to treat SIBO or Candida-type fungal dysbiosis until after mycotoxin treatment is underway.
- Eat a low-mold diet, including a mold-free diet brand of coffee such as Bulletproof.
- Take binder supplements that help bind and remove mycotoxins. We can help you choose the right ones for the mycotoxins that are present. We commonly use activated charcoal, chitosan, silica, and BioAloe.
- Agents such as liposomal glutathione to coax mycotoxins out from the intracellular space and help remove them.
- Sauna and sweating [check out HigherDose] helps detoxify mycotoxins—especially ochratoxin - but all mycotoxins to some extent.
- Neuroplasticity techniques can be extremely effective in helping to minimize symptoms and regulate hypersensitivity in people with mycotoxin issues. My go-to is the Gupta Program.
Say Goodbye to the Root Cause of Your Digestive Problems
Is your IBS, SIBO, or other stubborn digestive problems caused by mold toxicity? The first step to finding out is to book a free 15-minute troubleshooting call.
If after the call you come on board as a patient, I’ll dig down deep to discover the main reason why you have digestive problems – whether it’s mold sickness or some other cause. Then I’ll recommend the right tests and treatments to start you on your healing journey. We’ll remove the roadblocks that hold you back from optimum gut health and get you feeling your best again.
Eat What You Love Again This Holiday Season and Beyond
Everyone is gathered around the holiday table eating pumpkin pie. But not you. You know how you’ll feel after eating it.
Bloated.
Your tummy will hurt.
Lots of gas.
Maybe your skin will break out or start itching or you’ll be overwhelmed by fatigue.
Such a beautiful-looking pie and you can’t even have a bite. You sigh. It’s like the culinary equivalent of the Grinch Who Stole Christmas. You’re a mean one, Mr. Pie.
And the problem isn’t just the pumpkin pie. It’s all the carbs served with a traditional holiday dinner.
That’s how my patient, who I’ll call Jane, felt. When she first arrived in my office, she dreaded Thanksgiving and the holidays. She knew that if she touched any of the sweet treats or high-carb foods she’d pay the price.
That was until I pinpointed the root causes of her problem. Now, she actually looks forward to the holidays because she can indulge in the edible offerings of the season while still feeling healthy and well.
Yes, it’s possible. How did we do it? And how can you get rid of bloating, abdominal pain, gluten intolerance and more? You’ll discover the answers to these questions and more in this blog post.
A Frustrating Time in Jane’s Life
When Jane first arrived in my office in 2019, she was 12 weeks pregnant with her fourth child. She was having a super hard time and needed relief asap.
For starters, she was exhausted. She’d been pregnant or breastfeeding for the last seven years. She also homeschooled all of her children.
Her tummy hurt, she had near-constant gas, she was bloated and constipated. As if that wasn’t enough fun, she also had gnarly acne, painful canker sores, and regularly itchy ears, scalp, arms, and legs. Her eyes often crusted over in the morning.
She had been barely getting by eating a basic diet. She could only eat clean proteins with olive oil and salt along with above-ground veggies. If she ate anything else her symptoms flared. She couldn’t eat starches and only a little, if any, fruit. Eating nuts gave her canker sores.
As you can imagine, she dreaded Thanksgiving and the holidays. She couldn’t eat turkey if the brine had even a little sugar in it. She couldn’t have stuffing, even if it was gluten-free. And forget about anything high-carb.
No mashed potatoes and gravy. No grains. No dairy.
Can you relate?
Nothing Seemed To Work For Good
It had been six years since she felt “good.” Back then, she was on the Gut and Psychology Syndrome (GAPS) diet. This type of diet addresses the connection between the gut and brain and is often used to heal the gut. It includes meat, fish, eggs, fruit, non-starchy vegetables, and fermented foods.
But Jane had to stick with the GAPS diet religiously, and even then some of her symptoms lingered. After being on the diet, her digestion wasn’t painful anymore and she stopped catching every cold and flu that went around, but she still suffered from daily bloating and constipation.
Jane’s problems actually dated back to before the age of 10. Back then, she had frequent tummy pain. Her parents took her to the doctor a bunch of times, but no one could figure out what was wrong.
In college, doctors put Jane on the drug Accutane for her acne. If I had a dollar for every patient of mine who told me this was part of their history! Accutane devastates the gut microbiome and detoxification. The gut microbiome is the collection of bacteria, both good and bad, that live in your intestines and tune your metabolism, brain, gut health, and immune system.
Even worse, doctors make women take birth control while on Accutane because it can cause birth defects. The birth control sends women into a state of estrogen dominance, which only makes their problem worse.
Not surprisingly, Jane’s stomach pain got worse over the years. In her early 20s, Jane went on a gluten-free diet and the pain went away for a while. But it ultimately came back.
The First Red Flag
During our first appointment, Jane mentioned she had a front-loading washer. It smelled musty and she’d seen mold in it. Gross, right?
In her old house, the washer was in the basement and she could leave the door wide open to reduce the mold. Now the washer was on the main floor in her new house and there was foot traffic, so she had to keep the door closed. The musty smell grew worse.
Helpful hint: get rid of your front-loading washer, like yesterday!
The presence of the moldy washer led me to order a mycotoxin test, which identifies toxins from mold. The result? Jane had HUGE amounts of a type of toxin known as ochratoxin, which are produced by some Aspergillus species of black mold.
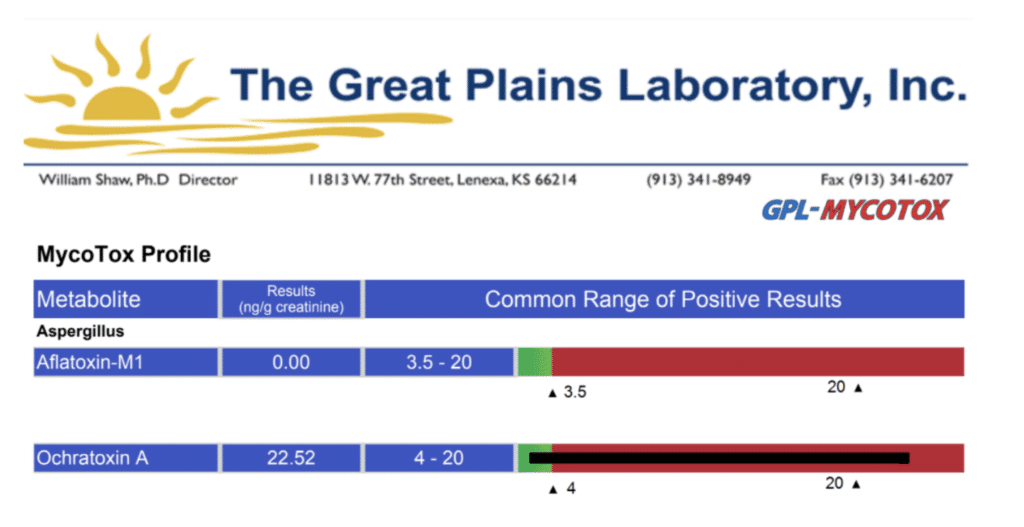
Other tests I ordered were:
- GI-MAP stool panel, which detects parasites, bacterial and viral dysbiosis, and Candida
- Organix panel, which identifies nutrient deficiencies and metabolic imbalances
- Small-intestinal bacterial overgrowth (SIBO) breath test, to determine if she had SIBO, a condition where there is an abnormal increase in the bacteria population of the small intestine, which can cause diarrhea, weight loss, and malnutrition. Jane actually requested this test, after reading about SIBO symptoms in a blog post I had written.
A Trio of Test Results
The GI-MAP stool test revealed Jane had an amoeba parasite called Dientamoeba fragilis, which can live in the large intestines of people. This little bug often causes no symptoms, but in some people it can lead to diarrhea and abdominal pain, as well as loss of appetite, nausea, and fatigue.
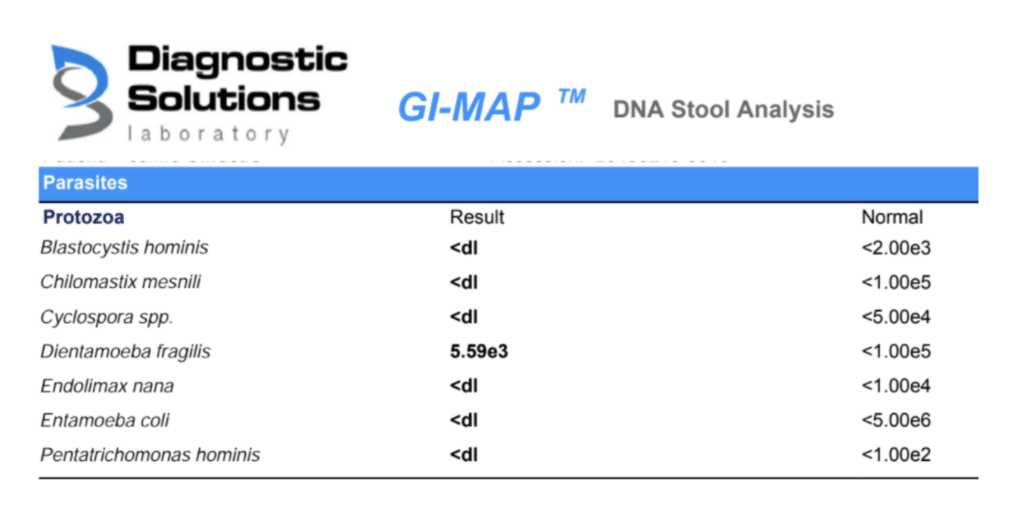
Jane’s Candida levels were through the roof. And her SIBO test came out positive. She had a type of SIBO known as methane dominant (IMO). This type of SIBO is caused by an overgrowth of single-celled organisms called archaea. It can cause constipation as well as bloating and gas.
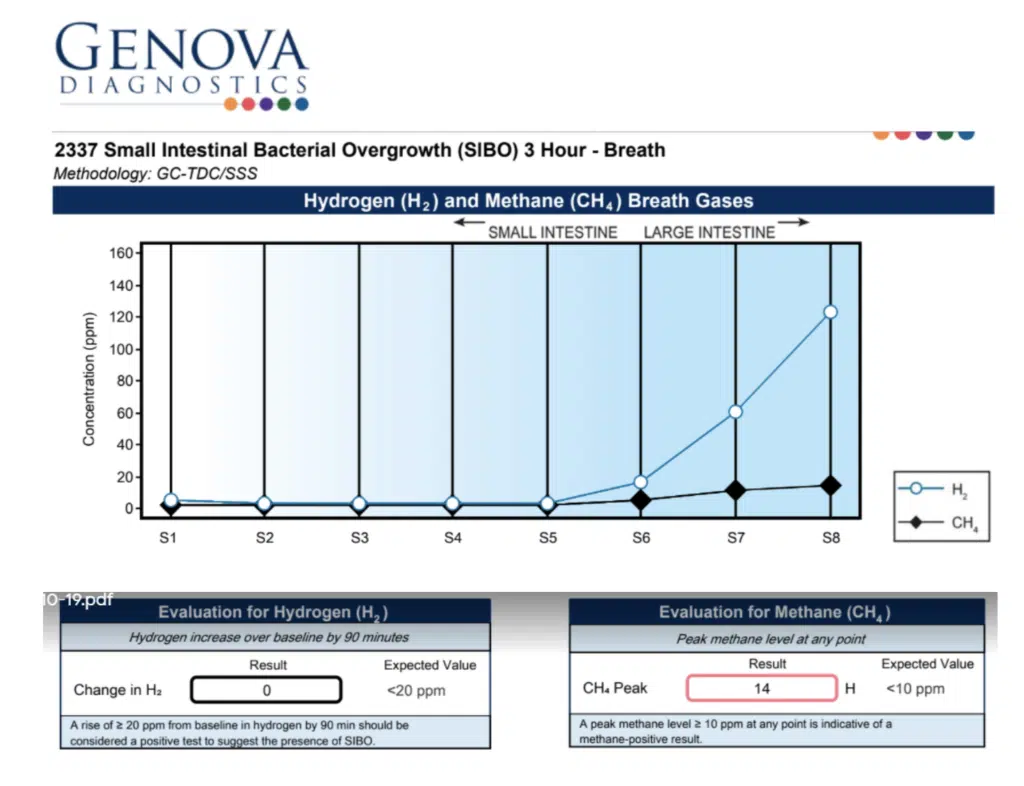
And what about Jane’s Organix test? That showed she was deficient in some nutrients. She needed B vitamins, especially vitamin B6.
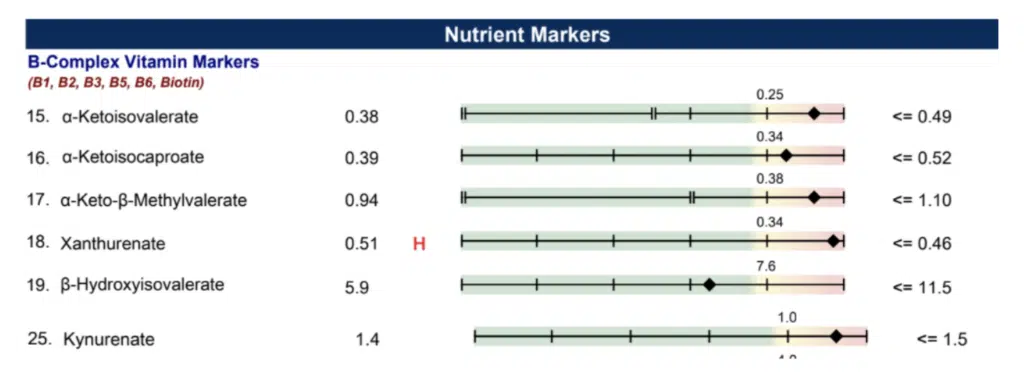
Helping a Pregnant Jane Feel Better
In most patients I would have treated the mycotoxin right away, but because she was pregnant I had to put the brakes on that approach. Otherwise, the mold could end up in her breast milk as she was detoxifying.
Until she finished nursing, I decided to focus more on healing her gut and resolving her gut symptoms. Here’s what I did at first:
- I gave her enzymes and hydrochloric acid to improve her digestion. I gave her some nutrients and herbs to help her with constipation.
- I put her on a low-FODMAP diet for the short term, but only because she was in such extremely bad shape. If you’re pregnant, don’t try this type of diet at home! It’s hard to follow this diet and get all the nutrients you need for you and the baby. You need a trained practitioner to supervise. However, for Jane, it reduced her symptoms and it was only for a short period, so it was worth it!
- I had her take several supplements including L-glutamine to heal the gut and butyrate and probiotics to balance her gut microbiome. I also gave her gentle herbs to reduce gas and bloating and encourage more frequent and complete bowel movements. For example, she used stone root (Collinsonia), a safe and effective way to promote better BMs in pregnancy.
- Suggested she avoid electromagnetic fields (EMFs) for the health of her and her baby. She noted that this dramatically shifted her symptoms in a short time.
Taking the Next Step to Feeling Well Again
After Jane finished nursing we went after her parasite first. Jane started doing coffee enemas and taking anti-parasitic herbal supplements. At the same time, I wanted to make sure she was making healthy amounts of bile, so I gave her phosphatidylcholine and a liver-supporting supplement known as TUDCA.
Next, we went after the mold toxins. I had her take supplements to detoxify her body of the Aspergillus mycotoxin. These included liposomal glutathione, binders specific to the mycotoxins she showed on her tests, antioxidants, and Quinton liquid, which helps transport toxins out of cells. I also suggested she have mold remediation done on her home. And aha! As I suspected, the problem went beyond the front-loading washer: the remediator found mold in the home’s air ducts.
This wasn’t an overnight treatment. She needed two rounds of the anti-mold supplements, three months per round, with retesting in between.
At the same time, Jane continued to work on healing her gut. She took digestive enzymes, L-glutamine, and Tributyrin-X™, a postbiotic butyrate supplement that promotes gut health, heals the intestinal walls, and encourages regular bowel movements.
At this point, as treatment unfolded, she had less indigestion and gas.
Getting rid of the mold was HUGE!
Things were looking up—but they still weren’t perfect.
Digging Deeper to Heal the Gut
Jane began an anti-Candida protocol. But those stubborn little fungi refused to be beaten.
I decided to retest her gut. And guess what showed up to the party? She was infected with high levels of two critters: C. difficile and H. pylori.
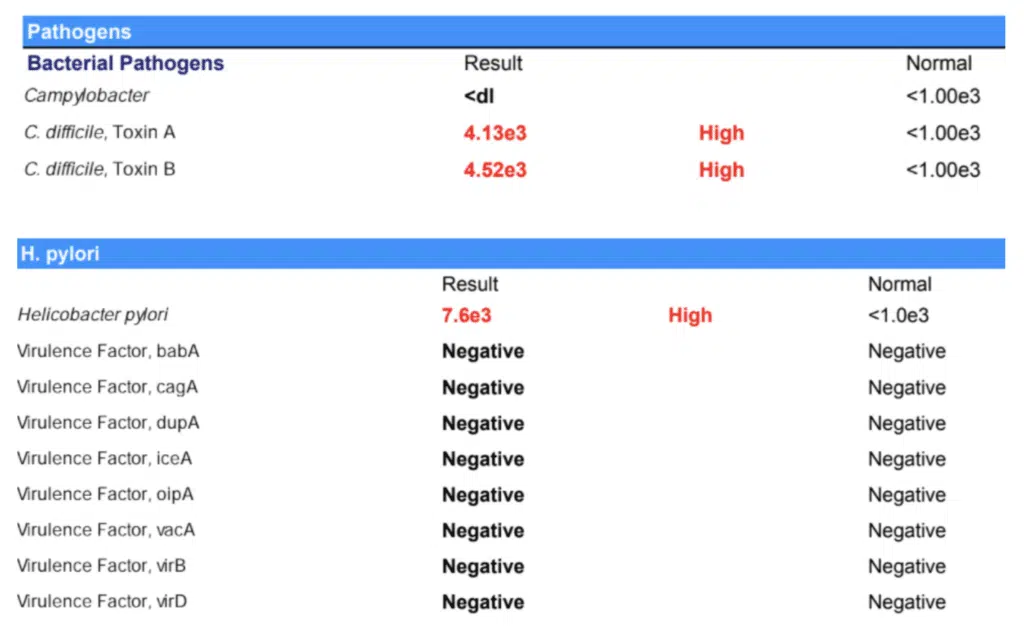
She’d probably picked up these bacteria after taking antibiotics for persistent diarrhea and fever during an earlier pregnancy with her third child. The antibiotics made the diarrhea and fever go away but she developed bronchitis. And guess what? The doctor gave her more antibiotics and she developed a vaginal infection. This was probably because the antibiotics caused a flare-up of the Candida. She was given yet more antibiotics. All that during pregnancy!
H. pylori and Candida often go hand in hand. As I’ve written about before, they often work as a team, so getting rid of one helped get rid of the other. Likewise, I have seen that C. difficile always exists in tandem with Candida overgrowth.
In order to tackle the C. difficile and H. pylori, we put the mold treatment on intermission. Once we got rid of these two bacteria, her symptoms were better. And she could finally say goodbye to her Candida overgrowth.
To address the vitamin B6 deficiency showing up in her Organix panel, she started supplementing with this nutrient. Vitamin B6 is important for brain development and keeping the nervous system and immune system healthy. Vitamin B6 plays an important role in the immune system of the intestines. The friendly flora of the gut also need vitamin B6 and other B vitamins to do their job well.
Take a look at her follow-up results for ochratoxin A. So much better! More importantly, this was associated with her symptom reduction. I always look at lab results in the context of how the patient is feeling. This is as much- or more- important than what we see on lab results!
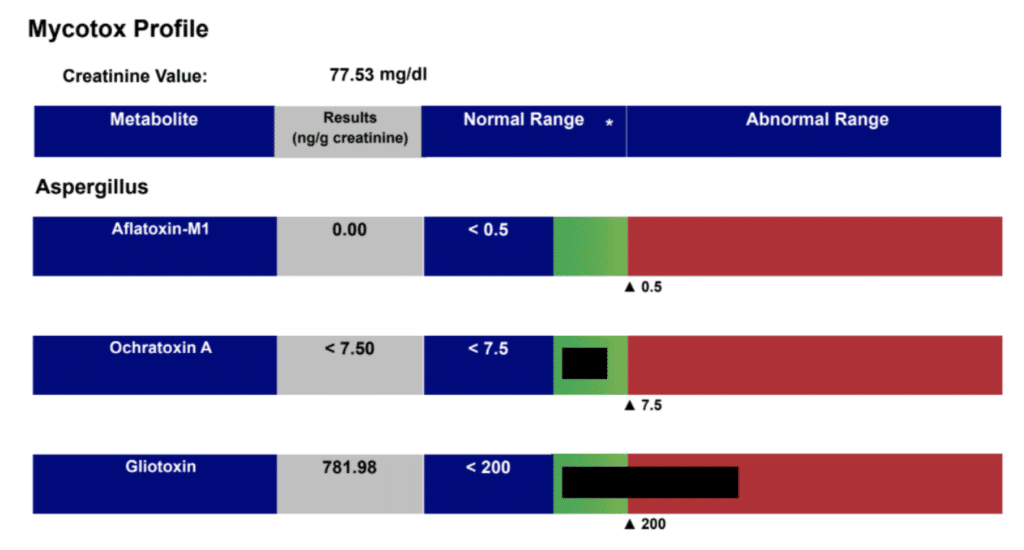
This whole process isn’t an overnight fix. It can take nine months or more. This is especially true for people like Jane who have had mycotoxins, bacteria, and other harmful organisms in their gut for a long time. Jane had symptoms almost her entire life. The longer you’ve been infected, the longer it may take to heal.
Be persistent!
Moving forward, we will focus on gut repair while nourishing and rebuilding Jane’s microbiome. We will support her detoxification processes for at least six months and maybe more.
Jane Doesn’t Have To Deprive Herself Anymore
Today, Jane is feeling amazing. She can tolerate a lot more foods. She no longer gets canker sores when she eats nuts. And what about her bloating, constipation, and abdominal pain? Virtually all gone!
Thanksgiving and the holiday season are now something Jane looks forward to for the first time in years. Her body can handle stuffing, potatoes, and pumpkin pie.
It’s the same on a daily basis. Within reason, Jane can tolerate less-than-perfect foods without going into a downward spiral.
Keep in mind that this journey is different for each person. Not everyone with food sensitivities can go back to eating a spectrum of allergenic foods in quick time. And some people may have to avoid a certain allergen for life because it harms their bodies. However, in general, when we improve gut health, people can resume eating foods (in moderation) that previously sent them into a tailspin.
Eat The Foods You Love Again
Do you have food sensitivities, gluten intolerance, or digestive symptoms like bloating, abdominal pain, and gas? You don’t have to live with these forever. Like Jane and I did, you and I can work together to unearth the root cause of your problem. I’ll help you eat your favorite foods again and feel healthier while you’re doing it. Your path to better gut health begins with a free 15-minute troubleshooting call.
Meet Your Gallbladder: The Essential Detox, Hormone, and Digestive Organ Most People Know Nothing About
More than 600,000 people have their gallbladder removed each year in the U.S.
That’s like if every single person in Las Vegas had their gallbladder removed!
Usually, the gallbladder is removed because of painful gallstones. It’s treated as a totally normal, safe procedure with no side effects.
But that’s just not true...
Your gallbladder is actually a crucial part of your digestive, detox, and hormonal systems.
And even if you haven’t had your gallbladder removed, gallbladder dysfunction is becoming more and more common, and can cause symptoms like:
- Digestive issues (pain, bloating, diarrhea)
- Fatigue
- Skin congestion (acne, rashes, eczema, etc.)
- Weight loss resistance
- Hormone imbalance (PCOS, estrogen dominance, etc)
- Fatty liver disease
- And more
Today, I want to explore the role of the gallbladder, common signs and symptoms of gallbladder dysfunction, and steps you can take to heal and optimize your gallbladder function. Learn about hormone imbalance after gallbladder removal.
What and Where Is The Gallbladder?
Your gallbladder is a small organ that sits underneath your liver. Your liver makes bile (the digestive liquid needed to break down and absorb fat) and the gallbladder stores it, concentrates it, and then releases it to the stomach on demand.
The gallbladder plays key roles not just in digestion, but also in detox and hormone balance, as bile is needed both for clearing toxins from the body and for the healthy production of hormones, as well as hormone removal and balance. For that reason, the gallbladder isn’t just a digestive organ - it’s also a hormone and detox organ.
In Chinese medicine, the gallbladder is also attributed with governing decision making and qualities like inspiration, action, and assertiveness (think of the saying “they have gall!”). A strong gallbladder is associated with a quick return to normal after a physical or emotional shock. On the other hand, a weak gallbladder is associated with timidity or hesitation, and problems making decisions or following through. Finally, the gallbladder is also seen as a pivot, a turning point for new decisions and stages of life.
What Bile Does
Although it’s not sexy, the bile created by the liver and then stored, concentrated, and secreted by the gallbladder is one of the most important secretions in your body. Bile consists of ~95% water, in which are dissolved bile salts, bilirubin phospholipid, and cholesterol, primarily.
Here are just some of the many roles of bile:
- Bile emulsifies fat, increasing fat absorption. Bile is an essential “degreaser” and “emulsifier” of dietary fats. Bile is also essential for the utilization of the fat-soluble vitamins A, D, E and K. Bile deficiency leads to vitamin deficiencies.
- Bile prepares nutrients for assimilation in the small intestine. Bile takes food that has been acidified in the stomach and alkalizes it, allowing it to be broken down and absorbed.
- Bile assists in detoxification. Bile contains the conjugated toxins - carcinogens, xenobiotic chemicals, pharmaceuticals, heavy metals like mercury, aluminium and lead, and deconjugated hormones - from the 2 phases of liver detoxification.
- Bile helps modulate the microbiome. It acts as an antimicrobial, keeping the balance of bacteria in check.
- Bile transports excess cholesterol out. In doing so, it prevents cholesterol levels from rising too high.
- Bile lubricates the intestines and plays a regulatory role in motility, allowing food to go through the digestive tract a lot easier and preventing constipation.
- Bile prevents the formation of gallstones by breaking down fats before crystallization, and also digests and dissolves gallstones, which are composed mostly of cholesterol and particles.
- Bile triggers the release of glutathione, which is considered the “master” antioxidant, and helps eliminate bilirubin.
- Bile breaks down fats, and as such, is essential for weight loss!
- Bile controls the rhythm of the gut - the circadian timing of your gut motility is controlled by the gallbladder. Changes in motility (the time it takes for food to move through the digestive system) can lead to issues like Small Intestine Bacterial Overgrowth (SIBO).
The Gallbladder, Bile, and PCOS
The gallbladder’s role in hormone balance deserves special attention, especially in relation to PCOS (Polycystic Ovarian Syndrome).
Dietary fat and bile (to absorb it) are both necessary for the production of hormones. Even more importantly - bile helps your body excrete excess and used hormones, like estrogen. In addition, estrogen dominance (either as a result of hormone imbalance or due to supplemental estrogen, like birth control pills) are known risk factors for sluggish bile (the precursor to gallstones) and gallstones themselves. This is believed to be because estrogen causes an increase in cholesterol levels in the bile, which can then thicken and form stones.
Interestingly, research has shown that in PCOS, bile acid levels are actually significantly elevated, and that high levels of bile acids correlated with higher levels of testosterone levels, meaning worse PCOS.
The exact mechanism is not yet known, but it is thought to be related to sluggish bile, which is more commonly seen in those with hormone imbalance and PCOS. The sluggish bile raises levels of bile acids in the blood. There, the bile acids act on the Farnesoid X receptor, which has hormonal actions throughout the body, and can lead to elevated testosterone.
In addition to increasing testosterone, high levels of bile acids can also contribute to insulin resistance, another major issue in PCOS.
Bile and Leaky Gut
Bile flow issues or lack of bile can also cause or worsen leaky gut (increased intestinal permeability).
While leaky gut is often attributed to toxins produced in the gut or pathogenic bacteria living there, insufficient bile is another major cause.
One role of bile is to bind with toxins and help them be safely excreted from the body. But if there is inadequate bile to bind with the toxins, they can damage the intestinal barrier, allowing toxins and undigested food into the bloodstream… creating “leaky gut.”
Leaky gut causes widespread, multi-system issues and may even be a major part of triggering autoimmune disease. It is common in IBS (Irritable Bowel Syndrome), ulcerative colitis, Crohn’s disease, Celiac disease, and more.
Signs of Gallbladder Dysfunction
The most common type of gallbladder dysfunction is the result of slow or sluggish bile. This can be a result of not enough water (remember, bile is 95% water!), but can also occur when bile is oversaturated with toxins. The sluggish bile is more like peanut butter than water, and is too thick to flow freely.
In addition, the removal of the gallbladder, as well as other conditions, can lead to reduced levels of bile salts in the bile and weakened bile.
Symptoms of sluggish or weak bile include:
- Abdominal tightness
- Bloating
- Difficulty digesting fats
- Diarrhea
- Constipation (fat can build up in the intestinal wall and cause slow movement in the digestive tract)
- Trapped gas
- Bad-smelling gas
- Stomach cramps
- Gallstones
- Fatigue and malaise
- Fatty stool that floats or is light in color or grayish white
- Increase in allergies, chemical sensitivities, or food intolerances
- worsening PMS/Estrogen dominance…
- Hormone imbalances like PCOS
- Heartburn
- Erratic bowel movements
- Weight loss
- Signs of Vitamin A deficiency: Dry eyes, night blindness, red or white acne-like bumps (on your cheeks, arms, thighs, and buttocks), and dry skin
Why Are So Many Gallbladders Removed?
Typically, the gallbladder is removed due to gallstones. Gallstones are crystallized masses of bile and cholesterol. Around 20% of females over the age of 40 have gallstones.
When gallstones become stuck in the duct of the gallbladder, they can cause pain and inflammation called cholecystitis. The most common treatment for gallstones is simply having the gallbladder removed. The surgeon then ‘“reroutes” the bile to go straight from the liver to the stomach.
Risk factors for gallstones include:
- Alcohol
- Excess reproductive hormones from supplementation or steroids (most commonly estrogen dominance)
- Oral contraceptive pills (birth control pills)
- High Endotoxin load causing sludgy bile
- Hereditary disorders like Gilbert's syndrome
- Thyroid issues or thyroid supplementation with T4
- Hepatitis
- Pregnancy
However, without the gallbladder, bile isn’t concentrated and lacks adequate bile salts - leading to the problems discussed above. That’s why gallbladder removal isn’t something you should just jump into.
Testing For Gallbladder Issues
If you suspect gallbladder issues, various tests can help pinpoint the problem:
- Blood test for cholesterol levels - if a person’s cholesterol production is low, bile production is also likely to be low. I look for cholesterol levels lower than 170.
- Digestive stool analysis - can help identify undigested fat in stool, which is caused by low bile availability.
- Bloodwork - to look for changes in serum bilirubin, alkaline phosphatase, serum glutamic oxaloacetic transaminase (SGOT), lactate dehydrogenase (LDH), aspartate aminotransferase (AST) and alanine transaminase (ALT). In early stages of gallbladder dysfunction, these levels might not change. However, functional medicine practitioners like me also use a more narrow interpretation of what normal is.
- A HIDA scan - this imaging test uses a radioactive material to measure the emptying function of the gallbladder, and can help diagnose:
- Gallbladder inflammation (cholecystitis)
- Gallstones, which can’t be seen, but can contribute to reduced flow or blockage to less bile flow if blocking
- Bile duct obstruction
- Congenital abnormalities in the bile ducts, such as biliary atresia
With my own patients, I use the ION panel by Genova (Organic Acids section) to evaluate the various pathways of liver detox and glutathione/antioxidant capacity. These results often illuminate when the liver or gallbladder are overburdened long before we see markers of pathology like elevated liver enzymes in labs. They also give more detail about exactly how the liver or gallbladder are compromised and can best be supported, in each individual.
Support for a Healthy Gallbladder
If you’re having signs of any gallbladder issues, step one is to get tested and find out exactly what’s going on.
In addition, here are some of the steps I turn to again and again with my patients:
- Switching out hormonal birth control (pill, patch, ring, etc.) for non-hormonal to reduce estrogen levels
- Supplements that support healthy gallbladder function
- Digestive enzymes and bitters
- Dietary changes: avoid excessive fried, fatty and greasy food and increase leafy greens
- Cut out alcohol
- Exercise regularly
In addition, addressing the emotional side of gallbladder health can be important. Try to express your emotion freely (journaling is an easy way to get started), address your past traumas (get help from a professional), and forgive.
And if you’ve already had your gallbladder removed? I can help you with strategies to support your digestion and hormones, even without your GB!
Want to learn more? Book a free 15 minute consult with my team now. It’s a zero-obligation opportunity to get a functional medicine opinion on your gallbladder health (and even if removal is something you should consider!).
P.S. Gallbladder issues are more common in women and those on hormones (like HRT or birth control). But if you catch gallbladder issues early on, you can avoid ever developing painful stones. Book a free 15 minute consult now.
The Surprising Truth About Low Stomach Acid (And How To Solve It Naturally)
Do you burp after meals? How about get so bloated, you want to unbutton your pants? Does food feel like it just sits in your stomach?
These are all tell-tale signs you might be suffering from a really common but not-well-known condition: low stomach acid, also called hypochlorhydria.
Stomach acid has a bad rap - most people are familiar with antacid medication for heartburn or indigestion, and (understandably) assume that stomach acid is bad for you and must be decreased.
But surprise - the complete opposite is actually true. In fact, adequate stomach acid is a crucial part of the healthy digestive process. And, in my clinical experience, far more people have low stomach acid than high!
Today, let’s talk about why stomach acid is so key, what it feels like when yours is low, and how we can treat this common issue easily and naturally.
The Truth About Stomach Acid
Stomach acid - scientific name hydrochloric acid (HCL) - is one of the key steps in the digestive process.
During the gastric phase of digestion, food you chew and swallow travels down the esophagus and into the stomach. There, distention (literally the stretching of the stomach by the addition of food), triggers the production of acetylcholine (ACh), which then triggers parietal cells in the stomach to release stomach acid.
But even before you start eating, just the sight, smell, and thought of food can also jumpstart the secretion of stomach acid via activation of the vagus nerve. This is called the cephalic phase of digestion.
The stomach is specially designed to handle the incoming acid - the stomach is lined with lipoprotein rich membranes that protect it from being burned by the acid. (Other parts of your body don’t have this same protection - which is why when stomach acid gets into the esophagus, it causes a burning sensation.)
Once secreted by the parietal cells, stomach acid performs several key functions:
- It kills any pathogens that may have come in with food (i.e. the kind of bacteria that cause food poisoning) or hitched a ride on the saliva from the mouth, where tons of bacteria live.
- It activates pepsin to start protein digestion
- It stimulates bile production and release by the liver and gallbladder, so fats can be emulsified and digested
- And finally, it triggers the release of pancreatic enzymes in the small intestine, where the partially digested food from the stomach (called chyme), is broken down and absorbed into the bloodstream
What Happens When Stomach Acid Is Low
When stomach acid is low for any reason, it can impact all aspects of digestion.
Low stomach acid can slow and stall out the digestive process - leading to discomforts like burping, bloating, stomach pain, and even (surprisingly) cause heartburn and acid reflux symptoms.
And while these are the symptoms most people notice (and complain about) first, they are actually just the tip of the iceberg.
More troublingly, low stomach acid can have a huge impact on your body’s ability to absorb nutrients from the food you eat. Stomach acid is essential for breaking down protein into digestible amino acids, and for the absorption of certain key nutrients like iron and vitamin B12. Without these key nutrients, the body is unable to repair tissues, produce hormones, and create neurotransmitters - all things necessary to feeling happy and vital!
Finally, low stomach acid also is a common factor in the development of food sensitivities, because it is stomach acid that triggers the release of digestive enzymes in the small intestine. Lack of enzymes is often to blame for food reactions - the one most people are familiar with is lactose intolerance, where a lack of lactase enzymes cause digestive issues like gas, diarrhea, and pain.
If you’re eating a high-quality, nutrient-dense diet but still struggling with symptoms of nutrient deficiency like brittle hair and nails, poor skin quality, cravings, and fatigue - or you have ever-increasing food sensitivity - low stomach acid could be the reason why.
What Causes Low Stomach Acid?
Stomach acid gradually decreases with age, and levels can start to drop as soon as age 40.
In most people, environmental factors are the main cause of low stomach acid. These include:
- Stress - the big one that no one likes to talk about! Stress impacts all phases of digestion, and especially the production of stomach acid and other digestive fluids
- Low protein diet - this is often a “chicken and the egg” situation, since eating less protein is often a result of those with low stomach recognizing protein-rich foods don’t make them feel well, and consciously or subconsciously cutting back. On the other hand, eating low protein can cause the body to naturally downregulate acid production (since less is needed to digest protein).
- Low zinc status - zinc is an essential cofactor for stomach acid production, and the modern diet is fairly low in zinc-rich foods like oysters.
- Eating on the go - like stress, eating in a hurry or while distracted can prevent the body from shifting into the “rest and digest” parasympathetic state needed to complete all the phases of digestion adequately.
- And finally - using over-the-counter or prescription acid-reducing medications.
Are You Using Antacids?
Antacids include over-the-counter and prescription PPIs (proton-pump inhibitors) like Prilosec or Nexium, H2 blockers like Pepcid or Zantac, and antacids like Rolaids or Tums. They work by either blocking the production of stomach acid, or neutralizing acid in the stomach.
These are some of the most commonly used drugs in the world. And, when used the right way, they can be extremely beneficial. But, many people take these drugs daily for years without any idea of the potential side effects.
Research has shown that PPI use can lead to the development of Small Intestine Bacterial Overgrowth (SIBO), which causes bloating, diarrhea, constipation, food intolerances, and stomach pain. In one study, more than half of people on a PPI for 12 weeks developed SIBO. In addition, research has shown PPI use is a risk factor for candida overgrowth, as well. The connection between PPIs and both candida and SIBO is likely due to the reduced ability of the body to kill pathogens that come in on the food you eat or with your saliva.
The irony with antacids is that most people take them to address the symptoms of low stomach acid - bloating, gas, indigestion - without realizing that they are actually just compounding the problem by further reducing acid levels.
How Do I Know If I Have Low Stomach Acid?
Testing for stomach acid levels is possible with a test called the Heidelberg acid test. However, this test is extremely difficult to come by, and most doctors and practitioners don’t have access to it.
Instead, I use an advanced stool panel to look for several key specific bacterial indicators of low stomach acid. Specifically, I look for these bacteria:
- Pseudomonas - this bacteria grows on poorly digested proteins that may be present due to low stomach acid. It also commonly occurs with food sensitivities, as undigested proteins are a main driver for triggering an immune response to foods. If you have high pseudomonas, and especially with food sensitivities, think about raising your stomach acid levels!
- Streptococcus and enterococcus - these gram-positive, aerobic species naturally occur in the oral microbiome, gut microbiome (found in the large intestine), and upper respiratory tract. However, they can overgrow or become infectious. Streptococcus commonly causes strep throat and upper respiratory infection, and if stomach acid is low, can infect the stomach. Enterococcus strains are common in dental infections (and found in up to 90% of infected root canals), and if stomach acid is low, can also infect the stomach.
- C. difficile - I always work on raising stomach acid levels in those with chronic or recurrent infection with this organism. C. difficile infection can be life-threatening in some cases, causing bloody or profuse diarrhea requiring hospitalization, and is commonly seen in medical settings after the use of broad-spectrum antibiotics. But it also often shows up on stool panels with minor or moderate symptoms, not requiring hospitalization. In addition to raising stomach acid levels I use herbs and probiotics to treat this.
- H. Pylori - this common infection thrives in a low-acid environment and even deconjugates stomach acid in order to make its host more hospitable. Ironically, PPIs are often used as part of the treatment for the ulcers and gastritis H. pylori can cause, continuing the cycle. Importantly, however, H. pylori is not always a problem. If levels are high or symptoms like ulcers, gastritis, rosacea, upper GI gas and bloating are also present, it may need treatment. For low or normal amounts of H. pylori, raising stomach acid levels is often all that is needed!
- Klebsiella- this bacteria is common in the oral microbiome, but high levels are associated with inflammatory bowel disease like ulcerative colitis and Crohn's disease. Because klebsiella is common in the mouth, elevated levels are often a sign stomach acid isn’t doing it’s job of killing bacteria in the stomach.
(Interested in a stool test like this? Book a free 15-minute consult here to learn more about stool testing and get started!)
How to Support Healthy Stomach Acid Levels Naturally
Creating a customized plan to support your digestion is what I do best. Every person is unique, and needs a unique protocol for best results. But, in general, these are some of the strategies I turn to again and again:
- Supplemental HCL - supplemental betaine HCL paired with pepsin (a digestive enzyme that specifically helps with protein digestion into amino acids) can be extremely helpful. One 6-week study in 97 people with indigestion found that taking betaine HCL and pepsin significantly reduced symptoms like stomach pain and burning.
One word of caution: supplemental betaine HCL may not be right for those with ulcers or gastritis. If you have these conditions, try one of the other suggestions or book a free consult for one-on-one support.
- Adequate B vitamins - B vitamins have thousands of benefits, one of which may be better stomach acid levels. One study found that increased B vitamin intake lowered risk of acid esophagitis. In addition, low stomach acid levels can hinder B vitamin absorption, increasing your need.
- Apple Cider Vinegar - this is a long-time fix for low stomach acid. Try taking a shot of ACV or dilute it with water to drink with meals. Be sure to rinse your mouth with plain water after drinking ACV.
- Ginger - helps to stimulate the digestive system. Try ginger tea or ginger chews.
- Bitters - bitter flavors stimulate the vagus nerve and tell the body food is coming, promoting the release of HCL and other digestive secretions like enzymes and bile. Try taking a bitter tincture directly on the tongue before eating.
Put Low Stomach Acid in Perspective
If you suspect low stomach acid, taking these simple steps to raise it can help you feel a lot better.
But in my clinical experience, low stomach acid is very rarely the only problem!
It either comes on as a result of other issues - like poor nutrient status and stress - that need to be dealt with, or causes other issues, like SIBO or candida overgrowth that require separate treatment.
If you’re dealing with digestive issues of any sort, I would be honored to support you in healing. Having struggled with health issues myself, I know exactly how debilitating they can be, and what vibrant health feels like (it’s AMAZING!) - and I want that for you, too.
We have a variety of plans and approaches to fit your health needs, schedule, and budget - but Step 1 is always a free, no-obligation chat with my team to learn about you and your concerns.
When H. pylori Met Candida: How They Team Up To Weaken Your Gut
If you have any sort of digestive problem—for example gas, bloating, inflammatory bowel disease (IBD), acid reflux, ulcers etc.—you’re probably wondering, why me? What’s causing me to suffer with bad indigestion or abdominal pain?
Some healthcare providers oversimplify the answer to that question. They try to blame all your digestive problems on one organism. For example, if you have acid reflux or ulcers, then Helicobacter pylori (H. pylori) must be the only organism to blame, right?
Wrong.
First of all, organisms like H. pylori, despite what you may have heard, aren’t always bad. Sometimes, they can actually benefit your health.
It’s actually when H. pylori gets together with its friend Candida albicans that it causes the most trouble.
Organisms that team up like this with other organisms may be called synergists or co-infections.
What does that mean for your digestive health? It means that if you’ve got two different potential troublemakers (certain bacteria or fungi) living in your GI tract, it might spell more trouble than if you only had one.
But it’s more complicated than that. Remember, most of the organisms or “good bugs” living in your gut are helpful or harmless. Scientists call them commensal bacteria. On the other hand, there is a small percentage that can be harmful, or pathogens. We will call those “bad bugs.”
The kicker is that your gut health determines whether a bad bug can cause trouble or not. For example, if you have good gut health with plenty of healthy bacteria and their beneficial byproducts, even a few different bad bugs won’t cause trouble. An unhealthy gut, on the other hand, can make your GI tract more vulnerable to even one type of bad bacteria or fungi that makes its home there.
In this blog post, I’ll use H. pylori and Candida to paint a picture of an example of commensal organisms that can turn bad. I’ll also show you how the presence of these two organisms can make or break your digestive and overall health.
What Is H. Pylori Anyway?
H. pylori is a bacterium that colonizes the lining of the stomach. Its presence is linked to duodenal and peptic ulcers, gastritis (inflammation of the stomach lining), and gastric cancer. Stool tests have also detected it in people with ongoing indigestion and abdominal pain. That’s why a lot of doctors go after H. pylori as a standard peptic ulcer or stomach ulcer treatment.
H. pylori really gets around. In fact, as many as 50% of adults carry this bacterium at some point in their lives but most have no symptoms.
H. pylori isn’t always a nasty bug as I will explain why later. But it can be nasty sometimes. With my clients, I will use agents that fight back an H. pylori overgrowth when any of these conditions are present:
- H. pylori overgrowth on testing.
- The presence of virulence factors. These are harmful substances that H. pylori makes to set up a home in the gut, avoid the immune system, and cause disease. Virulence factors increase the risk that H. pylori will cause digestive upset, ulcers, or cancers.
- Classic H. pylori symptoms such as ulcers, gastritis, upper GI bloating, acid reflux, acne, and more. When H. pylori overgrows in the gut, it tells me there is an underlying weakness. And while I do treat certain patients for it, at the same time I am asking the question: “Why?” Why did H. pylori take root and grow out of control?
What Causes H. Pylori?
H. pylori gains a foothold in your GI tract when levels of stomach acid take a nosedive. This can be a problem because when H. pylori turns bad, it can harm cells, cause inflammation, and damage the stomach lining. Here are some of the things that can cause low stomach acid:
- Drinking alcohol
- Drugs used to treat acid reflux (proton pump inhibitors)
- H. pylori itself
- Smoking
- Stress
H. Pylori: Not Always The Bad Guy
But here’s the thing about H. pylori: sometimes it’s actually your friend rather than your enemy. It has been co-evolving with us for millennia. At normal levels, H. pylori can be a commensal or friendly bacteria. While it has the potential to be a pathogen, it doesn’t cause disease in many people. In fact, it can:
- Reduce allergies, asthma, and skin diseases like eczema, especially in children.
- Lead to a lower risk of developing IBD. It does this by making some beneficial changes to the gut microbiome, the collection of bacteria, both good and bad, that live in the intestinal tract. This is why I often don’t want to get rid of H. pylori when I’m treating patients with inflammatory bowel disease.
Really, with H. pylori, what it comes down to is how many of these little guys do you have in your GI tract? And how virulent are they (meaning how likely are they to do damage)?
It’s also important to treat any underlying causes that made it too easy for H. pylori to set up shop.
And then there’s the question of: are you also infected with Candida?
What Is Candida?
Candida is a fungus that hangs out in nearly everyone’s intestinal tract. It’s part of the microbiome and thus a commensal fungus. In fact, Candida species appear in 40% to 80% of normal stool specimens.
However, when Candida goes from Jekyll to Hyde it can cause vaginal yeast infections and oral thrush. What is oral thrush? That’s when Candida builds up in the mouth and causes white sores on your tongue, lining of your mouth, gums, and throat. And that’s just the beginning. In functional medicine practice, I have seen Candida cause brain fog, fatigue, skin rashes, diarrhea, constipation, gas, anal itching, and joint pain.
Just like H. pylori, Candida can be a harmless wallflower in the gut or it can be a deadly pathogen.
What causes Candida to turn from harmless to health-harming? Here are some common reasons for Candida gone bad:
- Eating lots of sugary and processed foods
- Hormonal imbalances and birth control
- Stress
- Taking antibiotics, which kill off the good bacteria in your intestines
- Untreated diabetes
- Weak immune system
When Candida Meets H. Pylori
Candida and H. pylori are good friends. In fact, H. pylori can make itself comfy and at home inside Candida. And once Candida teams up with H. pylori, things go south quickly. Research found that if you’re infected with both these organisms you’re more likely to develop gastric ulcers or have more severe gastric damage than if you had H. pylori alone. Pairing up Candida with H. pylori also leads to a higher risk of peptic ulcer disease, hence the name “synergists.”
A lot of people have both of these infections at the same time. For example, in one study, out of 27 people positive for Candida, 18 were also positive for H. pylori. This is why I test for the presence of both of these organisms in my patients with GI problems.
The partnership between Candida and H. pylori is just one example of how synergistic organisms can impact your health. Candida is a real social butterfly. It has a lot of friends besides H. Pylori. These include the bacterium Clostridioides difficile (aka Clostridium difficile, the microbe responsible for bloody diarrhea). I used the friendship between Candida and H. pylori because it’s one of the best ways to show you how organisms can pair up to make your health worse.
Is Your Gut Ready To Face the Bad Guys?
In regards to GI issues, it’s really not about the “bad guy.” It’s all about whether you can tolerate the organisms that live in your gut. Some people with H. pylori and Candida have no symptoms at all.
The most important factor in this equation is your gut health. If H. pylori and Candida are present in excess it means you’ve got an underlying weakness in your GI tract. And we have to get at the bottom of why the weakness is there.
The answers to four questions will let you know how well your body will deal with invasions by these organisms:
- Are the good bacteria in your gut balancing out the bad bacteria?
- How effective is your stomach acid and digestion?
- How strong is your gut lining?
- How well is your immune system working?
It’s not possible to answer these questions on your own. That’s why, if you have GI problems, it’s best to work with me or another functional medicine provider to order the right testing, pinpoint the root causes, and design a customized protocol just for you.
Your path to better gut health begins with a free 15-minute troubleshooting call. During this chat, I’ll get to know more about what troubles you. If after the call you come on board as a patient, I’ll work with you to get rid of diarrhea, constipation, abdominal pain, gas, indigestion, acid reflux, and more. Book your call today and you can say goodbye to those frustrating, painful, and embarrassing GI problems and hello to great gut health!
What Your Gut Is Trying To Tell You About Your Thyroid (+ Tests That Can Reveal The Truth!)
Everything is connected.
It’s one of my key beliefs in medicine, and when it comes to your gut health and thyroid problems, it holds true.
If you’re struggling with thyroid symptoms OR gut issues, I want to take a look at both… because where we find one, we often find the other! And if you only try to fix one issue, you’ll wind up spinning your wheels, unable to fully heal.
And if you’re facing a thyroid issue, this is ESPECIALLY true.
Today, I want to explain exactly how gut infections and thyroid health are linked - and what you can do to find and address gut infections to achieve better thyroid health.
You - Yes, YOU - Could Have A Gut Infection
No one wants to think they could have any sort of gut infection or parasite. First of all, there is the “ick” factor associated with parasites and infections. Just talking about it might make your skin crawl!
Plus, most people think that gut infections only happen if they are drinking “dirty” water or travelling to far-flung countries.
But that just isn’t true! Even in North America, Europe, and Australia, gut infections happen all the time! Even very clean and careful people can become infected when doing everyday activities - like swimming, gardening, or eating out. If you have pets, kids, like to hike or spend any time outdoors, and eat or drink ANYTHING… you’re at risk of a gut infection.
So don’t panic… we’re exposed to potential pathogens all the time! You can likely think of one you know you’ve had… food poisoning.
Plus, one of the most common infections is actually overgrowth of commensal bacteria or fungi - which just means bacteria that belongs in the gut naturally either overgrows or grows where it doesn’t belong.
That’s why I bring up the topic of gut infections and parasites with all my patients.
Gut Red Flags To Beware Of
If you come to see me as a patient, I look for these warning signs that could indicate some sort of gut infection could be a factor:
- Diarrhea
- Constipation
- Abdominal pain
- Vomiting
- Gas and bloating
- Ulcers
- Weak immune system
- Autoimmunity
- Extreme fatigue
- Nutritional deficiencies
- Brain fog
- Sugar cravings
- Depression
- Anxiety
- Joint pain
- Obesity
- Food intolerances – especially developing new sensitivities
- Skin conditions – such as psoriasis, rosacea, and eczema
Or, any of these conditions, either diagnosed or suspected:
- Intestinal Permeability (leaky gut)
- Chronic and Acute Gastroenteritis
- Inflammatory Bowel Disease (IBD - Crohn’s or ulcerative colitis)
- Irritable Bowel Syndrome (IBS)
- Autoimmune Disease
- Small Intestine Bacterial Overgrowth (SIBO)
And of course, anyone with any type of hormonal issues - but especially thyroid or sex hormones - gets a closer look, since gut infections and hormones are so closely linked.
These Are The Tests I Order...
Have some red flags? It’s time to test!
First up are stool tests. This is where I start for almost all patients.
My personal favorite stool test is the GI Map.
Why do I like it? Compared to a regular stool test, the GI Map uses qPCR (quantitative) Technology, which is a more accurate way to detect and quantify organisms compared to more common culture, regular PCR, microscopy or DNA sequencing. qPCR works by amplifying and detecting DNA and RNA sequences, which is key because for results to be clinically meaningful, you need to know how much DNA is in the stool.
The GI Map test is also reproducible, which means that if you run it twice in a row, you get the same results - this is a key quality to look for in any diagnostic test. It’s used in research settings and it is the first pathogen assay that is FDA approved.
Other tests I like and sometimes use are:
- BiomeFx - this is a newer test that uses Whole Genome Sequencing to analyze over 25 pathogens measures their relative abundance as a percentage of your entire microbiome. This is different from traditional stool tests, which only look for any detectable number of pathogens present. While it isn’t uncommon to have a small number of pathogens present in your microbiome, the relative abundance in proportion to your other bacteria is what’s important.
- GI360 by Doctors Data
If you have constipation, diarrhea, gas, significant bloating or a history of food poisoning, I’ll also ask for a SIBO Breath Test.
If you have candida overgrowth symptoms like a history of antibiotic use, yeast infections, urinary tract infections or interstitial cystitis, chronic itching in groin, fungal toe nails, you’re reactive to yeast in foods, have been diagnosed with methane SIBO, have sugar or carb cravings, or stubborn weight issues, but the stool test doesn’t show candida, I will order Organic Acids, and/or Serum Antibodies to further suggest candida overgrowth treatment would be beneficial for you.
What Your Gut Test Results Can Reveal
Once I’ve got your test results back, the real fun can begin: interpretation and treatment!
But I don’t just glance at your results: I comb through all the details, connecting dots to put together a comprehensive picture of what’s happening with your health.
Here’s a peek at what I’m looking for in your test results:
Inflammation/Immune Markers
-
- Calprotectin - this is key for differentiating between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) (some tests also have lactoferrin). If below 120, it suggests infection, chronic NSAID use, or could be polyps, colorectal cancer or IBD. If above 120, it’s a sign of significant inflammation--which may be caused by an infection, but also generally receives a recommendation for referral to a GI doc if you’re working with me, as it can be suggestive of Celiac, or Inflammatory Bowel Disease such as Chrons’ or Ulcerative Colitis. (Gastroenterologists may suggest colonoscopy to rule these out when calprotectin levels cross a particular threshold). Each lab has a different range and sensitivity for calprotectin, so practitioners should use that lab's range. Should be rechecked at 4-6 weeks or after treatment.
-
- Zonulin - this is a keymarker of leaky gut.
-
- SIgA - this is a marker of gut secretory immunity and barrier function and can show loss of resilience and tolerance. I look at this for signs of chronic infection, immune suppression, and/or adrenal hormone dysfunction.
Digestion and Absorption
-
- Pancreatic Elastase-1 - this marker reflects levels of pancreatic digestive enzymes present. There are many reasons why someone might have sub-optimal digestive enzymes, but regardless of the cause, we will want to supplement with enzymes at least in the short term.
-
- Fecal Fat - this is a marker of fat breakdown and absorption. If really low, it’s a sign a patient is not eating enough fat (<5%). If high, it indicates fat malabsorption/digestion. I’ll want to consider bile flow/production issues, enzyme deficiency, or SIBO.
-
- Short-Chain Fatty Acids and Beta-Glucuronidase - these are functions of the bacteria in the microbiome that reflects if good bacteria are present in adequate numbers or if less desirable bacteria are overpopulated. SCFA are the main fuel for cellular repair of the barrier membrane. High beta-glucuronidase can be a cause of estrogen dominance, and can also signal overall issues with not just the gut, but liver detox, depending on the level.
Microbiome
-
- Commensal bacteria - these are your “good bacteria” - and this also shows which bacteria are in low number, and which are missing altogether
-
- Parasitology - looking for infections like campylobacter, giardia, Blastocystis hominis, entamoeba histolytica, etc are present.
-
- Mycology - this clues me in to what fungi and yeast are present.
-
- Pathogenic bacteria - aka bad bacteria, or bacteria that can be either bad or good (like H Pylori)
-
- Worms - Yes it is gross, but it’s not the end of the world!
What Does All This Have to Do with Your Thyroid?
Let’s bring this all back around to your main concern: your thyroid!
Research has actually linked multiple gut infections to thyroid issues. Here’s a breakdown of some of the most common ones:
Blastocystis hominis
This common gut infection (often called Blasto for short), which is spread via contaminated food or stool, can cause symptoms including bloating, diarrhea, nausea, flatulence, variable bowel habits, abdominal pain, hives, and fatigue. Additionally, this pathogen is notorious for causing multiple food sensitivities.
It’s also linked to Hashimotot’s thyroiditis: people with Hashimoto’s are more likely to develop the skin condition chronic spontaneous urticaria (also known as chronic hives), as well as irritable bowel syndrome (IBS). And a study of 54 people in Egypt with chronic urticaria (hives) revealed that Blastocystis hominis was found in 61 percent of them, while only eight percent of the healthy controls had the parasite, suggesting that Blasto could be linked to hives, IBS, and Hashimoto’s.
Epstein-Barr Virus
Epstein-Barr Virus is a common virus best known for causing the disease mononucleosis.
Research out of Poland supports my informed hunch that it’s also linked to Hashimoto’s. A 2015 study done there found the virus in the thyroid cells of 80 percent of people with Hashimoto’s, while controls did not have the Epstein-Barr virus in their thyroid gland.
Yersinia Enterocolitica
This infection is often caused by consuming undercooked meat or drinking contaminated water. There is some evidence that Y. enterocolitica is associated with autoimmune thyroid disorders including Graves’s disease and Hashimoto’s thyroiditis in genetically susceptible individuals because higher antibodies to Y. enterocolitica are often found in these patients.
Helicobacter Pylori
This ultra-common infection/overgrowth, best known as a cause of ulcers, is also linked to autoimmune thyroid disorders. In a Korean study, those who were positive for H. pylori were significantly more likely to also have anti-thyroid peroxidase antibodies present.
Small Intestine Bacterial or Fungal Overgrowth (SIBO or SIFO)
Both bacterial and fungal overgrowth in the small intestine is linked to hypothyroidism - research has shown as much as 54% of people with hypothyroidism also have SIBO or SIFO.
These overgrowths can also deplete iron, which is involved in thyroid hormone synthesis.
In my own clinical experience, many of those with Hashimoto’s often have a high degree of yeast overgrowth and symptoms to go with it: gas, bloating, brain fog, sinus congestion, GI distress, itchy skin or scalp, eczema, vaginal yeast infections, and intestinal permeability.
Giardia
Giardia is another common parasite most commonly caused by drinking contaminated water. Some research has shown it can prevent the absorption of thyroid hormones in the gut, leading to hypothyroidism. (While I don’t have studies to support it-- just my own observation with my clients-- I suspect this could be true for any parasite or overgrowth causing inflammation in the gut, and not just Giardia.) But the good news is clearing the infection reverses hypothyroidism!
Connecting the Dots & Creating Your Treatment
With the right testing, you might finally be able to “see” what caused your thyroid issues - or is exacerbating them: a gut infection.
All the testing and interpretation brings us to the most exciting point: treating your gut issues, And with that information in hand, we can co-create a 100% unique treatment plan for you.
For my clients, I always create a custom protocol based not only on their test results, but also with their budget and lifestyle in mind. I don’t believe in a one-size-fits-all approach to medicine, which means if you have a strict supplement budget to stick with, or really, really, REALLY don’t want to give up a particular food, we try our best to find a way to work with it so that you get the results you want, within your parameters.
If you want to learn more about what it’s like to work with me as a practitioner, sign up for a no-obligation 15-minute Intro Session here.
This is your chance to share your story with my team and get a realistic look at what working with us is like.
>>> Book an Intro Session Here
I hope this information was helpful to you - and you can find tons more over at my blog: https://briewieselman.com/
- Brie Wieseleman, L.Ac
Endometriosis 101 Part 2: How I Help My Patients Dealing with Endometriosis
Check out "Endometriosis 101 Part 1: What Is this Condition & Why Is it Happening to Me?" HERE
While functional medicine practitioners don’t know with certainty the root cause of endometriosis either (we’re still waiting on the science), we focus on what we do know about the condition by working to reduce inflammation and support the immune system.
Pain management and even surgery might be part of our treatment plan - but I would never see a woman in endometriosis pain and just throw the birth control pill at her! I am not interested in band-aids. I want real solutions for my patients.
Here’s how we address endometriosis (but remember that every treatment plan needs to be customized for your unique needs):
These steps can happen in any order or all at once, depending on your situation.
#1 Heal The Gut
Addressing gut health should always be high on your list for really any health concern, but especially for anything autoimmune.
I often see bacterial infections like SIBO (Small Intestine Bacterial Overgrowth), parasites, viruses, mold and toxin exposure, and food sensitivities. In studies, 80% of women with endometriosis also had SIBO.
These can all be signs and triggers for leaky gut, so addressing them and then working to heal the gut is key to recovery.
I like to start with a comprehensive stool test like the GI Map to find any gut health issues. Then we’ll work to clear any infections and implement dietary changes to support the gut (this could be an elimination diet, but that is not always the answer!).
One dietary change I do recommend? Cutting dairy and soy. There is a lot of research to support the idea that dairy and endometriosis are not good together. Dairy is hormonal, it’s a really common allergen, and it’s also pro-inflammatory. (As is soy.)
Do you have to quit them both forever? Absolutely not. Once you have endometriosis under control, you can probably enjoy them again in moderation. And of course, quality and quantity matter a lot. Go for grass-fed and organic, minimally-processed dairy when you do have it.
Another thing I look for on stool tests is high beta-glucuronidase. Beta-glucuronidase is an enzyme produced by gut bacteria and can be elevated by parasites and other gut infections. When beta-glucuronidase is high, it can lead to estrogen buildup. If you have high beta-glucuronidase, I’ll use calcium d-glucarate and Lactobacillus to help lower this and reduce the estrogen recirculation.
#2 Reduce Inflammation
Next, we’ll take a look at your lifestyle and see what could be leading to increased inflammation. It could be late nights at the office, too many meals out, drinking too much, or even “healthy” habits like over-exercise or a really restrictive diet.
Overtraining isn’t an issue for all women - but you might be surprised how easy it is to become “overtrained” with even a moderate exercise regimen. Remember, overtraining isn’t necessarily about too much exercise… it’s about too much exercise relative to too little recovery. That’s why Olympic athletes can exercise so much without overtraining - they spend all the rest of their time recovering! But for women who have to work, commute, get dinner on the table, do laundry, etc. etc. etc. there is rarely enough recovery time!
Stress in any form is incredibly inflammatory, but it’s not the only inflammatory element to look out for. The modern world is pretty rife with chemicals… and no one wants to think about the cumulative effect of the pollution we breathe (drink and eat, too!), the chemicals in all the products we use (from cleaning to personal care), or the added ingredients in most of our food (including unwanted pesticides and other chemicals). But - it all adds up to a lot of potential inflammation.
But, you don’t have to start living like a monk and throw away everything plastic in your home. I’ll help you choose where you can make a few key changes to reduce overall inflammation.
#3 Stabilize Blood Sugar
One big myth is that weight loss can help with endo symptoms. If you’re carrying a lot of excess weight, losing weight can potentially help with symptoms (since hormones are produced in fat cells) - but that doesn’t mean weight loss is a “cure.”
If you’re already lean, the extra stress on the body of trying to lose more weight can make your symptoms worse. And even if weight loss is one part of your healing plan, it’s definitely not the whole story.
Rather than emphasize weight loss, I like to focus on stabilizing blood sugar with a whole-foods based diet.
This is really important because higher blood sugar levels lead to increased insulin, which stimulates the conversion of testosterone into estrogen. This is just another contributor to the high estrogen levels that are linked to endometriosis.
#4 Balance Hormones
You can’t diagnose hormone imbalance based on symptoms, so I never start a hormone protocol without testing. I use the DUTCH Hormone Panel with my patients.
Once we’ve identified your imbalance, we’ll come up with a plan to correct it - everything from herbals and supplements to acupuncture, exercise, diet, and stress management can come into play.
Some of the herbs and supplements I use most often are:
Melatonin
Melatonin is an antioxidant that has been shown to be able to reduce pelvic pain associated with endometriosis. Now, I don’t want to give out a dose because it’s not the typical low dose that people use to help them sleep. It’s actually a pretty high dose. And it can definitely make people groggy. As a practitioner, I want to make sure it’s appropriate for you. But in the right dosage, melatonin can reduce endometriosis pain by as much as 40%. And it’s safer than the pharmaceutical options by far!
Before supplementing, you can also do things to naturally increase your own melatonin levels like have good sleep hygiene, avoid caffeine, avoid blue light after three in the afternoon, and sleep in a dark room.
Vaginal Probiotics
This is one of my favorite tools - and yes, it is what it sounds like: just take probiotics, and stick them up there! This is really safe and one of the easiest ways to shift the vaginal microbiome.
(If you have chronic yeast or bladder infections, or bacterial vaginosis, this can also help with those conditions in many cases!)
The brands I recommend are Jarrow’s Fem-Dophilus and FloraFemme.
Pycnogenol
Pycnogenol is another really well-known antioxidant that’s very specific to lowering pain and lesions in endometriosis. It’s safe and effective for many women.
Bioidentical Progesterone
This really depends on the woman and proper hormone testing. Please don’t go buy some natural progesterone cream and start self-supplementing! Getting the dose right and monitoring while you use it is so important.
But this works because proper progesterone levels balance and oppose estrogen. Think of it like a teeter totter. But in women with endometriosis, there is evidence that they may have progesterone resistance and therefore need slightly higher progesterone levels than the average woman to achieve that balance.
DIM
Diindolylmethane (DIM, in short) is a phytochemical found is cruciferous veggies (think broccoli, cauliflower, brussels sprouts etc.) and it’s one of my favorite tools for estrogen dominance. It helps balance levels of different types of estrogen and block androgen receptors. Get it from eating lots of veggies, or try a supplement.
#5 Support Better Detox
Your body knows how to detox itself (thanks to your liver, kidneys & more) - and you don’t need a 10-day juice fast to “cleanse.” But that doesn’t mean we can’t support detox.
Your detox symptoms can easily become overburdened when you consider the amount of toxins you’re exposed to (pollution, chemicals in cosmetics, pesticides on food to name a few). Your liver can get “jammed” trying to detox as much as possible - which can then burn through your glutathione stores and leave you feeling totally burnt out.
And remember - your liver also plays a major role in detoxing excess estrogen, so if it’s jammed up, you’re setting yourself up for estrogen dominance.
I’ll have you take a look at where you’re being exposed to toxins as well as teach you some easy tricks for supporting the body’s detox processes.
These are some of the supplements I love for supporting better detox:
Calcium D-Glucarate
Calcium d-glucarate is one I mentioned before for gut health. It is a supplement that’s pretty safe to play with if you have endometriosis because you can assume that you have some level of estrogen dominance. But again, I like to use it based on stool testing so we can be certain that excess beta-glucuronidase enzyme is in fact a part of your issue. Because why take excessive supplements that are not doing for you what you need? That’s a waste of time and money.
N-Acetylcysteine
I always say this is the supplement I would take if I was trapped on a deserted island… it’s just awesome. It has many uses and it supports the production of or master antioxidant, glutathione (which we all need more of!)
In a double-blind study, 92 women with endometriosis were either given NAC or no treatment. And during the NAC treatment, they saw a distinct reduction in the number of cysts or tissue implants, as well as size. In the women using NAC, lesions stayed the same or actually shrunk.
In the no treatment group, lesions tended to grow! The NAC was more effective than hormonal treatments.
And the crazy part is that 24 women in the NAC treatment group who had scheduled laparoscopy actually cancelled their surgery because they had such a great reduction in pain. One woman even got pregnant!
I can’t recommend NAC highly enough. But quality does matter - I usually use physicians-grade from brands like Pure Encapsulations, Thorne, or Designs for Health. I like to use 500 mg, 2-3 times daily.
One caveat: if you have acute gastritis (inflammation of the gut lining) NAC can thin the gut wall slightly, so it might not be right for you.
Don’t Just Accept Endometriosis or Painful Periods
I would never lie and tell you that I have a magical cure for endometriosis. I don’t (and no one does).
What I do have is a holistic approach to healing that takes into account not just symptom management - but also addressing the root causes so that you can experience true relief.
Because there are multiple layers to healing endometriosis, I recommend you get support from an experienced practitioner. A practitioner can help you assess your gut health, hormones, and detox symptoms and strategize healing. Working with an experienced practitioner can turn and a long and frustrating process into a much shorter one. (The majority of my clients see major, lasting improvements in just 3-6 months.)
It’s very possible to be symptom-free, even with endometriosis. It’s very possible to see heavy bleeding, painful periods, and PMS go away. I’d love to help you.
You can book a free 15-minute consult with my team right now. During the call, we’ll listen to you and explore how we could guide your health forward (no obligation!).
Periods shouldn’t be painful or something to dread! I’d be honored to help you take back control and feel better.
P.S. Do you feel like you’re already eating well, managing stress, and STILL struggling with endometriosis? I’d love to learn more and see if we can’t get you feeling better. Book a free 15-minute consult today.
A Functional Medicine Practitioner-Designed Postpartum Recovery Plan (For Mom & Baby)
It’s hard to believe my baby girl is coming up on 5 months old already!
All the mamas out there know… the postpartum period is a whirlwind!
Not only are you adjusting to taking care of baby, but your body is undergoing massive changes (just as big as during pregnancy!)
And you’re sleeping less, nursing (literally nourishing an entire other human with YOUR body!), and might even be going back to work around the 3-month mark if you’re in the U.S.
It’s a lot! That’s why I think your postpartum recovery plan is just as important as what you do before and during pregnancy (if not more important!)
Today I want to share my go-to supplements that I’ve used in my own postpartum recovery and first months of motherhood - I hope they help you as much as they have helped me over the past few months.
What I’m Taking For Postpartum Recovery & Surviving New Motherhood
Here’s a quick rundown of my daily supplement routine since giving birth. (Remember that this is what was appropriate for me, and may not be exactly right for you! Book a free consult with my team to learn more about customizing supplement plans for you).
#1 A good prenatal multivitamin
There’s nothing that depletes your body of nutrients quite like growing another human and then nursing them! You need the extra nutrients in a good prenatal just as much after birth as you do before.
I like Designs For Health Prenatal Pro because it contains chromium and other important micronutrients. Because I have a family history and personal tendency toward diabetes (and dealt with gestational diabetes), I specifically chose a prenatal that contains chromium. Research suggests that chromium can help lower fasting blood sugar and insulin levels.
#2 Magnesium
Magnesium - for everything! Magnesium has so many benefits…. But it’s especially good for mitochondrial energy, maintaining your calm, supporting healthy sleep, hormone support, and insulin signaling. I use Magnesium Buffered Chelate Glycinate by Designs for Health.
#3 Mushroom blend
I use a mushroom blend with reishi, cordyceps, and lions mane called Host Defense Stamets 7.
Mushrooms have so many benefits! Lion's mane helps with brain health, stress and anxiety, and diabetes prevention and management.
Cordyceps can help protect mitochondria and therefore have anti-aging benefits. And with how little sleep I’m getting, I definitely feel like I need the help! Contact me to learn more about mushrooms and breastfeeding.
#4 Adaptogens
Adaptogenic herbs (like goji berry, maca root, ginseng, and more) support adrenal health and mitochondrial function. With all the stress of a new baby and the limited sleep, adaptogens can be really useful. I use “The One” from Quicksilver Scientific.
#5 Flax seed meal
I have PCOS (Polycystic Ovarian Syndrome) and as a result my hormones need extra support to stay in balance. I personally tend toward estrogen dominance (not all women with PCOS do - so be sure to get your hormone levels tested with a practitioner!)
Flax seed meal has a “bad reputation” as an estrogenic food but the truth is that flax seed meal can help with estrogen detox, keeping the body’s hormone levels in better balance if you’re estrogen dominant like I am. I eat a couple tablespoons of ground flax daily.
#6 Probiotic & prebiotic
I rotate through 3 probiotics to keep my gut healthy: FloraMyces, Klaire Therbiotic, and MegaSporeBiotic.
I’m also taking a daily prebiotic. Prebiotics are indigestible fibers that act as food for the bacteria in the gut. I use MegaPreBiotic.
The probiotic and prebiotic are for my health - but also for baby girls’! Right now, my daughter’s microbiome is still “under construction”and is strongly influenced by who she has contact with - namely her dad and I. Moms transfer bacteria to baby through kissing, cuddling, and (most importantly) breastfeeding. That’s why gut health is even more of a priority right now than usual.
#7 Natural toothpaste & mouth rinse
Your oral microbiome seeds your gut microbiome, and with as much as my daughter open mouth kisses me and all the germs we pass back and forth, I’m doing everything I can to support a healthy microbiome body-wide. Research has shown that baby’s oral microbiome continues to develop up to 1 year.
I use PerioBiotic toothpaste from Designs for Health and Dentalicidin Mouth Rinse from BioBotanical Research.
Why I’m Passionate About Breastfeeding
I’m also taking supplements that have made breastfeeding easier and confer benefits to baby through breastmilk. I promise I’ll share all those with you - but first I want to cover why I’m so passionate about breastfeeding.
My intention is to breastfeed my daughter past one year - what’s called extended breastfeeding. That’s because there are so many benefits to breastfeeding:
- Breastfeeding prevents autoimmunity - research has shown being breastfed is associated with a lower incidence of diabetes, celiac disease, multiple sclerosis and asthma
- Breastfeeding builds a stronger immune system and may even help prevent development of disease later in life
- Breastfeeding boosts the brain - this study showed it improved cognitive development and this one showed those breastfed for 6+ months had better test results in school
And with my history of gestational diabetes and tendency toward high blood sugar, it was important to me that breastfeeding decreases the risk of diabetes in mom AND baby and especially helps prevent Type 2 diabetes for moms who had gestational diabetes.
That doesn’t cover even a fraction of all the health benefits of breastfeeding for mom and baby… not to mention the emotional and mental benefits.
While I understand that breastfeeding isn’t possible for all new moms, I highly recommend it… and if you’re struggling with low supply, keep reading for some of the solutions that made breastfeeding work for me.
Breastmilk Boosters
I struggled with low supply from day 1 (largely as a result of hormone disruption caused by my PCOS) - but luckily I found a few solutions that helped get my supply up to normal. If you’re a fellow PCOS sister, I hope you’ll consider these ideas.
#1 Myo-Inositol
Myo-inositol is a natural substance, found in plants and animals, which helps to regulate insulin in a similar way to metformin and may be useful for mothers with PCOS who are dealing with low supply.
It’s a major ingredient in breast milk and taking it supplementally can help boost breast milk production and increase baby’s brain health.
#2 Metformin
Metformin is a prescription drug that can help lower blood sugar to boost supply. It doesn’t work for all women - but if it helps you, it’s a powerful tool that’s safe for baby. Metformin is considered low-risk for baby.
The dosage starts at 500 mg, but talk to your doctor (you’ll need a prescription) to find what’s right for you.
For anyone nervous about using metformin: you should know this what what finally increased my supply to nearly normal levels!
I also take therapeutic levels of Fenugreek, Goat’s Rue, Moringa, and Shatavari-- all proven to improve milk production and flow safely. While different women will have different degrees of response to these herbs, they are generally safe to try. It can take up to 2 full weeks to notice a shift in supply or flow.
What I’m Taking For Baby’s Benefit
Nursing mamas aren’t just a milk machine... But everything you take in is transferred to your breast milk. And when that milk is baby’s only source of nutrition for 6 months, you want it to be as good as possible!
A healthy and diverse diet with more-than-enough calories is step one to make the best milk, but I also am using these supplements for “milk enhancement.”
#1 Lugol’s iodine
Pregnancy requires higher levels of iodine, and research has shown women who are iodine deficient in pregnancy and postpartum are more likely to have children with neurological and psychological deficits like attention deficit disorders and lower IQ.
Since I don’t eat iodized salt or iodine-rich foods regularly, I use 2 drops of 2% Lugol’s iodine solution daily.
#2 Calcium
Here’s a wild breastfeeding fact: if you’re not taking in sufficient dietary calcium while breastfeeding, your body will leech calcium from your bones to supply calcium in your breastmilk!
I don’t want to feed my baby my own bones - so I supplement with calcium to make sure I have adequate supply for both of us.
#3 DHA
The omega-3 fatty acid DHA is one of the most important nutrients for a healthy baby. It’s critical for healthy brain development plus vision and memory.
Lots of research has shown that supplementing with DHA can increase DHA levels in breastmilk and lead to better health outcomes for baby, so I use Nordic Natural Prenatal DHA.
#4 Coconut oil
Coconut oil is one of my favorite sources of healthy fat - and eating it regularly can increase lauric and caprylic acid content in breastmilk. Lauric and caprylic acid are powerful antimicrobials that can help strengthen your baby’s immune system and keep them healthy.
Studies have shown eating 3 tablespoons at a meal can significantly increase levels, so I aim for 3 tablespoons in my daily smoothie.
#5 Liver and organ powder
Liver and other organ meats are on the best sources of important nutrients like choline… but most of us are deficient! Choline is particularly important for healthy brain and memory development, so it’s important for breastfeeding moms to get enough.
I use a powdered form of organ meats made by Ancestral Supplements and try to eat 2 pasture-raised eggs (the yolks are a great source of choline!). Use code BRIEW10 at checkout for a 10% discount!
What To Give Baby
Right now, all baby girl gets is milk, milk, and more milk!
That’s all infants less than 6 months of age need - it’s the perfect food.
The only supplement I give to her is Klaire Therbiotic Infant 4 times a week to support her healthy microbiome development. I give this to her either on my nipple by dampening the skin with a little milk and then dabbing the powder on there, or, by mixing it in a bottle of milk, when she takes a bottle.
She’s getting her Vitamin D through my milk; you must take 5000 IU or more daily to accomplish this--test first to make sure that dose is safe for you.
That’s it!
Your Postpartum Recovery Strategy
As a hormone specialist, I’ve always loved working with moms in the postpartum period - but as a mom myself now, I have a profound respect for all my mom clients!
If you’re pregnant now, hope to be soon, or are in the postpartum period now, I’d love to support you in finding your own postpartum recovery strategy, tailored to your unique needs.
Book a free 15 minute consult with my team by clicking here. During the consult, we’ll talk about your experiences and needs and start on a strategy for long-term wellness, together.
To your health,
Brie
P.S. Are you interested in hearing more about my motherhood journey? Be sure to check out my Instagram where I share candid pics and commentary!
How To Treat Depression & Anxiety Holistically - Part One
Butterflies in your stomach before a first date. Sweaty palms before asking your boss for a raise. Grief when your dog dies. Crying over a breakup.
These are all normal and healthy moments of nervousness and sadness.
But then there’s a shift….
Laying awake at night with a pit in your stomach… when tomorrow’s just another Tuesday. Overwhelming sadness when everything is going OK. A feeling of despair you can’t shake…
These are signs of a more serious issue: anxiety and depression.
If you’ve ever experienced anxiety or depression, you’re currently dealing with them, or are supporting someone you love with one of these conditions all you care about is getting rid of them.
But it’s not always simple. Anxiety and depression are multifaceted issues. And that’s where the problem starts.
Doctors and practitioners want to put you onto one 2 paths:
- Treat the brain. This is everything from antidepressants and anti-anxiety meds to talk therapy with a psychologist. On this path, anxiety and depression are seen purely as a mental health issue - so treatment focuses on your brain.
- Treat the body. On this path, anxiety and depression are seen as symptom of a problem somewhere else in the body. Treatment often focuses on changing your diet (especially avoiding certain foods) and adding in exercise.
This gets me so frustrated!
Like nearly EVERY health condition, depression and anxiety are not problems of JUST the brain or JUST the body. There is a definite mind-body connection, and the best treatments (and prevention) for depression and anxiety treat both.
In this series, I want to do some real talk about anxiety and depression. We’re going to dig into the root causes - everything from childhood trauma to candida - and the solutions that might be able to help you.
Nothing is off limits and I’m not going to vilify any one kind of treatment.
I hope this can be an open and honest discussion about anxiety and depression like you’ve never experienced before.
Trauma, Circumstance, and Perception in Anxiety and Depression
Before I dive into some of coexisting conditions I see around anxiety and depression (and the steps you can take to help treat it), I want to make a very important distinction. While I believe (and the research shows) things like compromised gut health and hormone imbalance can cause anxiety and depression, it’s not the case for everyone.
Trauma, circumstance and perception can all be root causes of anxiety and depression.
And even if eating a blood-sugar balancing diet DOES help you manage anxiety and depression, it doesn’t mean that your anxiety was just caused by eating too much junk food. The trauma was real. This is a very sensitive issue, so I want to make sure this is clear.
Here’s what I see a lot in my practice: when a woman has co-existing conditions like leaky gut or a hormonal imbalance, when trauma happens (and it happens to almost all of us to varying degrees), it’s more likely that the temporary stress of the trauma develops into the long-term problems of anxiety and depression.
How you perceive trauma is important too. What qualifies as a trauma to one person wouldn’t be for another person - and neither one is right or wrong. Your perception is YOUR perception. But, you can learn tools that can help change the way you perceive things.
(It’s the difference between seeing your mother-in-law’s comments as a personal attack against you or just a manifestation of her own insecurities that you can brush off.)
If you’re equipped with self-care practices and coping mechanisms before the trauma happens, you’re much more likely to avoid depression and anxiety.
This is where “treating the brain” is so important.
For those of you who are dealing with past trauma or very difficult circumstances, I’d suggest looking into EMDR and Brainspotting in addition to everything else I lay out in this post.
- EMDR is shorthand for Eye Movement Desensitization and Reprocessing. It’s a kind of psychotherapy that combines aspects of traditional talk therapy with eye stimulus. Research has shown it helps you process through trauma much faster than talk therapy alone (think the work of 8 years of talk therapy in just a few EMDR sessions). It’s a recognized treatment by the World health Organization, the Department of Defense, and the American psychiatric Association. Learn more about it and find a clinician here.
- Brainspotting is a therapeutic tool that can be used in conjunction with other forms of therapy. It works by accessing the autonomic and limbics within the central nervous system to help work through traumas - especially those that are not in the conscious mind (and therefore hard to talk about and treat). Learn more about Brainspotting and find a clinician here.
And I encourage everyone - whether or not they’re dealing with anxiety and depression - to get started on the inner-work that makes you more resilient to trauma. It can be as simple as beginning a meditation practice or finding a counselor.
A note on antidepressants and anti-anxiety medications: I believe antidepressants and antianxiety medications can be life saving for some people. They also have serious side effects and address the symptoms over the root cause. No one other than you and your doctor can decide if medication is the right step for you. But, whether or not you use medication as part of your treatment, I encourage you to explore treating the coexisting conditions and root causes I share about in this post.
Gut Health and Depression
When I hear about depression and anxiety, I immediately think about gut health. I rarely (I mean rarely!) see a patient with symptoms of depression and anxiety who doesn’t have some sort of gut health problems.
And intuitively, it makes sense. We feel our emotions in our guts just as much as we feel them in our mind - the “stomach in your throat” feeling, butterflies in the stomach, a “gut punch” when you get bad news, needing to go to the bathroom when you’re anxious or nervous.
We also know that 90% of the body’s serotonin is actually produced in the gut - not the brain - and that other important mood chemicals are made in the gut, too.
Irritable Bowel Syndrome (IBS) is also closely associated with depression and anxiety.
In my practice, I see 2 kinds of gut health problems contributing to anxiety and depression over and over again: leaky gut and candida overgrowth.
How Leaky Gut Leads To Depression & Anxiety
One of the most famous studies on gut health and depression was conducted in 2008: “The gut-brain barrier in major depression.”
This study is famous (and still cited all the time) because the researchers made some amazing discoveries.
First, they concluded that “There is evidence that depression is accompanied by an activation of the inflammatory response system and that proinflammatory cytokines and lipopolysaccharide (LPS) may induce depressive symptoms.”
In layman’s terms, that means:
- Inflammation is one cause of depression
- There is evidence that leaky gut may cause symptoms of depression
The study measured antibodies produced by the body’s immune system against lipopolysaccharides (LPS) in depressed patients and in controls (without symptoms of depression). LPS are large molecules of dead cell wall of the gram-negative enterobacteria - also called endotoxins. LPS should NOT be in the bloodstream. If LPS are present in the bloodstream, it means the tight junction of the gut have become loose (aka leaky gut).
The researchers found that the immune markers against the LPS bacteria in the gut were much higher in depressed patients than in the control group.
This means that the depressed group had more leaky gut and gut microbiome dysbiosis than the control group.
In fact, researchers concluded that patients with major depression should be tested for leaky gut. (And I’d argue, anyone with any symptoms of depression or anxiety - not just major depression!)
What causes leaky gut?
LPS are dead bacterial cell walls - and generally having high levels of them in the bloodstream indicates dysbiotic flora in the gut in addition to leaky gut. This can too much of the wrong bacteria, too little of the right bacteria, or too much or too little bacteria in the wrong place.
Leaky gut can also be caused by parasites, SIBO (Small Intestine Bacterial Overgrowth), yeast overgrowth (more on that to come), and untreated food sensitivities and intolerances.
Food sensitivity symptoms are usually an immune system response to foods we eat. The reaction creates inflammatory compounds that get into the bloodstream, circulate, and can create anxiety, brain fog, depresion, and fatigue.
Low nutrient status can also contribute to depression. When food isn’t properly absorbed in the gut (due to dysbiosis or leaky gut) the body doesn’t have the “nutritional building blocks” like amino acids, folate, vitamin B6 and more it needs to create the chemicals to control mood. This can cause depression and anxiety.
Yeast Overgrowth, Depression
Other than leaky gut, the most common gut health problem I see in relation to anxiety and depression is candida overgrowth. Candida is a kind of yeast that almost all people have present in their body. Candida is responsible for thrush in babies and yeast infections in women. In normal amounts it is healthy - but it’s when it overgrows that it causes problems. And the way candida impacts depression is especially interesting!
Candida is a yeast - which means it produces alcohol (ethanol) and acetaldehyde (the chemical responsible for the main symptoms of hangovers!) Both these chemicals are toxins to the body.
In a normal healthy person, (who hasn’t been drinking!), there should be little to no alcohol in the bloodstream. But if that person has an overgrowth of Candida, the alcohol produced by the yeast is entering the bloodstream - we call this “auto brewery syndrome” and it literally makes you drunk.
In a study conducted by doctors at Biolab in London, UK, a number of chronically unwell patients were tested for blood ethanol levels an hour after ingesting a sugar solution. The study found the patients consistently had high blood levels of ethanol which the researchers concluded came from small intestinal yeast overgrowth.
And - even worse - when candida is well established, it transform into the fungal form its branching (hyphae) “feet” can penetrate the intestinal wall.This creates literal holes in the gut, enhancing leaky gut syndrome and allowing more alcohol and acetaldehyde into the bloodstream.
What does that do to you?
Ethanol metabolism…
- Interferes with energy metabolism; this results in fatigue & muscle aches
- Causes hypoglycemia or "low blood sugar"
- Creates nutritional deficiencies
Then the ethanol is converted into acetaldehyde which…
- Is responsible for most of the symptoms of a hangover
- Causes dilation of blood vessels in the brain which result in the characteristic severe headaches
- Is toxic and inflammatory to the brain’s neurons
- Binds glutathione - the body's main antioxidant - thus increasing oxidative stress and allowing free radicals to damage cells throughout the body. Without enough glutathione, the liver can’t detox properly
- Increases the release of adrenaline, causing heart palpitations, anxiety etc. Panic attacks become more common.
What causes candida to overgrow?
All of these factors make your body more hospitable to the overgrowth of candida:
- Antibiotics
- Oral contraceptive pills
- High sugar/starch alcohol diets
- Stress
- Having other GI infections, or
- Having immunosuppression related to adrenal fatigue
Candida overgrowth can be treated - but the root cause that began the overgrowth must also be addressed!
Action Steps For Healing Gut Issues
The first step to healing gut issues is to find out exactly what is going on.
I don’t like to “guess and check.” For patients in my clinic, I always start with specific stool tests for parasites, dysbiosis, and yeast overgrowth. For SIBO, I test using a lactulose breath test.
Once we identify exactly what issues are occuring, we tackle them - treating parasites and pathogens, and then using diet and supplements to heal leaky gut. Gut mucosa heal rapidly when the aggravating factors are resolved! On average, my patients see big changes in as little as 3 weeks.
Coming Up: Hormones & Toxins
I hope reading Part 1 of this post has left you feeling empowered - and maybe even hopeful. If gut issues are contributing to your anxiety and depression, treating them can help you take a big step forward.
In Part 2 of this post, I’m going to address two other major factors in anxiety and depression: exposure to toxins and hormone imbalances. There’s still a lot left to cover!
I’m passionate about helping women uncover the root causes of their health problems and address them naturally. If you’re dealing with anxiety or depression, I’d love for you to book a free 20-minute root cause symptom analysis consultation with my team. These appointments are TOTALLY free, and there’s no obligation to book any further appointments. See what time slots we have open here.
Are Worms The Next Frontier of Health? Everything You Need to Know About Helminth Therapy
I talk a LOT about clearing infections and overgrowths - Small Intestine Bacterial Overgrowth (SIBO), yeast overgrowth (candida), and of course, killing parasites.
So I was shocked when I first heard about a new treatment idea for treating disease and healing damaged gut: worm therapy. Not clearing worms. Giving them to the patient, to help heal disease.
No, I’m not joking. It’s called helminth therapy - named for the type of organism used Hymenolepsis Diminuta Cysticeroids (HDCs). HDCs are the larval form of a very specific type of worm that help to restore immune tolerance and diversity to the microbiome when it’s been damaged.
I was really skeptical when I first heard about this. But then I heard a presentation given by one of my medical heros, Dr. Sidney Baker (former faculty member of Yale Medical School, founder of Defeat Autism Now! and Autism360.org, Linus Pauling Award recipient) and Dr. Yehuda Shoenfeld at the Institute for Functional Medicine conference in May 2018.
They shared the latest research and their experience using helminth therapy - and I went from skeptical to excited. I slowly introduced helminth therapy in my own practice and saw amazing results.
Here’s what I want you to do: suspend all your judgement for the next 10 minutes and read the rest of this post. I promise you’ll be surprised by what you learn - and I bet you’ll want to learn more about helminth therapy.
HDCs Aren’t Just Any Worms
HDCs are the larval form (aka an intermediate life stage between egg and worm) of a small helminth. Helminth grows naturally in grain beetles, which were a common part of our food supply up until about 100 years ago.
HDCs are not a parasite. By definition, a parasite causes harm to an organism - HDCs cause no harm. HDCs stay in the gut - they cannot breach the gut wall.
Really important: HDCs cannot colonize in humans. That means they’ll never go from larvae to worm in a human. For that same reason, HDCs can’t be passed from human to human either. They’re NOT contagious from person to person.
Using helminth therapy is completely different from something like taking a tapeworm from Mexico. It’s produced in sterile lab conditions (just like probiotics are) and carefully controlled.
How Are HDCs Produced - And How Do You Take Them?
Therapeutic HDCs are grown in sterile conditions in a lab - much the same way probiotics or yeast for brewing beer or culturing yogurt are.
First, the eggs are grown in rodents in the lab. If that makes you squeamish, keep in mind that these animals are kept in MUCH more humane & clean conditions than most farm animals! Then the eggs are taken and are bred into larvae in grain beetles which eat only oatmeal. The HDCs are harvested from the grain beetles and suspended in salt water.
HDCs are given orally (again, just like probiotics!) through the salt water solution. You’ll take a tiny vial (about the size of the tip of your pinky finger!) that holds the microscopic organisms. If you hold the vial up to the light, you can just barely see the HDCs as tiny white flecks.
Unlike probiotics - which can contain billions of CFUs per capsule - HDC are given in very precise, small amounts: most people start with 10 HDC per vial and work up to 30 HDC. Strong, therapeutic doses of up to 100 HDC every 2 weeks can be used, too.
If you do ingest HDCs, they can only stay in your body for about 2 weeks.
How Does Helminth Therapy Work?
This is the part that’s really exciting:
Helminth therapy works by promoting microbiome diversity and restoring immune tolerance.
Remember - our body isn’t sterile. Our microbiome is teeming with important bacteria and other organisms that help it function: both flora (like probiotics) and fauna (beneficial things like HDCs). When the gut microbiome doesn’t have enough diversity of both flora and fauna it can’t perform its functions properly.
Our gut microbiome teaches our immune cells how and when to function and it establishes our intestinal barrier (which keeps pathogens out of our bloodstream). Our immune cells are our body’s defense team. Immune tolerance is what our immune cells won’t react to. It’s our body’s bouncer waving something through.
Immune tolerance is a good thing! It means your body won’t wage war on the strawberries you ate, or cause you to sneeze and cough when you’re outside around pollen.
If you have decreased immune tolerance, you’re more likely to experience these conditions:
- Allergies (both seasonal and to foods)
- Eczema
- Asthma
- ALL autoimmune conditions (things like endometriosis, multiple sclerosis, lupus, rheumatoid arthritis, vitiligo, Hashimoto’s, alopecia, ulcerative colitis, Crohn’s and more)
Today, 50 million Americans have been diagnosed with an autoimmune disease. That’s up from 9 million in 1997. (Still a huge leap even when you factor in increased testing/awareness.)
Experts like Dr. Baker and Dr. Shoenfeld agree: the best way to treat ANY chronic illness is to restore immune tolerance.
What Makes Our Microbiome Diversity & Immune Tolerance Decrease?
Up until the very recent past (like the past 100 years) our microbiome diversity was supported naturally by our environment. People interacted more frequently and directly with nature: farming, foraging, etc. They also had less hygiene practice: no antibacterial soap or hand sanitizer.
Worms - both beneficial ones like HDCs and pathogenic ones - were also something more people had when we lived hunter-gatherer lifestyles. (These persist in hunter-gatherer groups like the Hadza tribe today - and they have the most robust and diverse microbiomes of anyone known on the planet… and virtually no IBS, UC, Crohn's, diabetes or other autoimmune disease!)
Other things in the modern world that damage our microbiome diversity:
- Antibiotic use (kill beneficial bacteria in the gut)
- PPIs (impair digestion and promote bacterial and fungal overgrowth)
- Birth control pills (kill beneficial bacteria in the gut and promote yeast)
- C-section births (prevent transfer of microbiome from mother to infant in the vaginal canal)
- Vitamin D deficiency (too much time indoors)
- Chronic stress (go-go-go cultural attitude)
- Contaminated/nutrient poor food (Standard American Diet!)
- Excessive hygiene practices (overuse of antibacterial cleaning agents)
How To Restore Microbiome Diversity & Immune Tolerance
Diet has the biggest influence of all factors on the health of our microbiota. Less diversity in your diet = less diverse gut bugs.
Step 1 has to be eating a nutrient-dense diverse diet with plenty of gut-nourishing foods: fiber, healthy fats, and protein.
Making changes to your lifestyle & hygiene practices is important too:
- Put down the antibacterial soap!
- Get out in nature and interact with the earth
- Get adequate sunlight or supplement with Vitamin D
- Eat fermented foods or supplement with a high quality probiotic
But if you already have all these steps dialed in and are still dealing with symptoms of decreased immune tolerance or chronic illness, helminth therapy that can increase diversity and immune tolerance may be the next step for you.
What The Research Shows About Helminth Therapy (And Results in MY Practice!)
- In the largest randomized control trial in history (!), 1 million children in India were dewormed by researchers who hypothesized it would lead to an improvement in general health. Instead, they found no significant effect on weight, death rate, or health. This drew into question the premise that all worm are always harmful…
- In a 2005 study, 29 patients with Crohn's disease (most of whom were non-responsive to pharmaceutical treatments) were treated with helminth therapy every 3 weeks for 24 weeks. At 24 weeks, 79.3% of the participants had responded favorably and 72.4% had completely reversed their Crohn’s disease!
- In this 2014 study, people with IBD (either ulcerative colitis or Celiac Disease) were treated with either helminth therapy or a placebo for 12 weeks. Although this study was too small and too short to be conclusive, 10% of those who received the helminth achieved remission (compared to 4% in the placebo group).
In my own practice, I’ve seen these results using helminth therapy:
- Normalization of thyroid labs
- Remission of Crohn’s and Ulcerative colitis (when symptoms have already been improved and other co-infections addressed)
- Improvement of GI symptoms (diarrhea, constipation, gas, bloating, etc.)
- Reduction of arthritis symptoms
- Improvement of inflammatory symptoms like skin rashes, insomnia, and mood/brain issues
- Reduction of histamine intolerance symptoms
Other practitioners have reported improvement in children with autism and people with multiple sclerosis.
Who Helminth Therapy Is (And Isn’t For)
There’s no magic potion in medicine that will cure all your problems (i’m sorry!).
If you’re not eating right, moving, finding joy, and managing your stress, helminth therapy won’t work for you.
But if you’ve already got those “core” practices in place and are still struggling (or just want to see how good you can feel!), helminth therapy could be beneficial for you.
Typically people take 6 doses of HDCS 2 weeks apart to initially evaluate if they are or are not going to have a beneficial response. Then, if no benefit is seen, they can increase the dose for. Risk is almost non-existent, and the potential benefits are huge.
(But, anyone on immunosuppressive drugs - like those used in some types of inflammatory bowel disease or other autoimmune diseases - shouldn’t take HDCs. The helminth therapy is not beneficial if your immune system is suppressed by medication.)
What Do You Think?
I am so glad you stayed with me.
I know that “worm therapy” sounds really weird at first- but the idea of taking probiotics was once weird, too! I’m a supporter of anything we can do to improve our gut health - because our gut health radiates out into every aspect of our being.
Want to learn more about helminth therapy (and potentially give it a try?) - book a free 15 minute consult with my team where we can create an action plan for you.
Want to get healthier but NOT ready to try HDCs? That’s OK too - I’d love to teach you about how else you can support your gut. Book a free 15 minute consult with my team here.
My Top Travel Tips for A Healthy Gut
Traveling is one of my biggest passions. When I got married, we chose to do a destination ceremony and reception with all of our friends and family in Sayulita, Mexico, instead of a traditional wedding (no regrets there!).
Traveling hasn’t always been fun for me, though. When I was younger, I felt like EVERY time I traveled, I got sick. And I’m not talking about a cold, folks - I’m talking about the nemesis of every globetrotter: traveler’s diarrhea.
Traveler’s diarrhea, Montezuma’s revenge, Delhi/Bali belly - it’s all caused by food poisoning. And while it will definitely ruin your trip, it also has a more sinister side - food poisoning can cause lasting damage to your digestive system leading to a lifetime of #gutproblems.
Want to know how food poisoning can cause long-term digestive issues - and what I do to avoid traveler’s diarrhea (even in the most exotic locales!)? Keep reading!
(Not interested in the science? Skip here for my travel tips).
How Food Poisoning Can Wreck Your Gut Long Term
I can’t tell you how many patient in my clinic can trace their digestive symptoms back to a case of food poisoning. And the science backs them up! Food poisoning is a known cause of irritable Bowel Syndrome (IBS). IBS after food poisoning is called “post-infectious IBS.”
But this gets a little complex, so bear with me here...
IBS isn’t a disease - it’s a syndrome. That means it’s just a name for a group of symptoms (fun stuff like gas, bloating, diarrhea, constipation, and food intolerances). IBS is a diagnosis of exclusion, meaning your doctor will call your symptoms IBS when they can’t find any other cause for them.
For many people - perhaps as much as 60% - the actual cause of IBS symptoms is something called Small Intestine Bacterial Overgrowth (SIBO). SIBO occurs when bacteria that should be confined to the large intestine migrates up and into the small intestine. A healthy small intestine should have very little bacteria in it!
So how does bacteria get from the large intestine to the small to cause SIBO?
It’s usually do to a problem with the Migrating Motor Complex (MMC). The MMC is what creates movement in your intestines - called peristalsis - and moves food from your stomach down through your intestines and eventually out of your body.
So what can harm your MMC? The most common causes are chronic viruses like Lyme disease, structural abnormalities, high stress levels, and… food poisoning!
Stay with me here - food poisoning can cause your Migrating Motor Complex to malfunction. When the MMC malfunctions, bacteria can move from the large to small intestine and overgrow, causing SIBO - and SIBO is the cause for as much as 60% of IBS!
As you can see, it’s a complex chain of events - and that’s why for years doctors have missed the connection between IBS, SIBO, and food poisoning. Luckily they are catching up now.
Toxins & Autoimmune Responses
So how exactly does the food poisoning cause damage to the Migrating Motor Complex?
Common food poisoning bacterias like E. coli, salmonella, Campylobacter jejuni, and Shigella all produce a toxin called cytolethal distending toxin B. It sounds bad, doesn’t it?
Your body will start producing antibodies against the cytolethal distending toxin B. For some people, they’re able to fight it off over in a few days and move on without long-term problems, but for about 10% of us (raising my hand!) we can’t fight it off as quickly - and therefore we keep producing more and more antibodies.
These antibodies don’t just fight the cytolethal distending toxin B - they also reduce a kind of protein in our intestine called vinculin.
Vinculin is very important in the health of Migrating Motor Complex - vinculin is crucial for proper function of nerve cells in the gut that cause peristalsis. When the MMC isn’t functioning and movement of food through the gut is slowed down, bacteria can overgrow and cause SIBO - plus other symptoms like bloating and gas.
The good news is that your gut can recover vinculin over time. First, you need to heal the SIBO. But it’s also critically important that you don’t get food poisoning again. So if you already have some gut issues, don’t stop reading now!
Here’s What I Do To Avoid Traveler’s Diarrhea
The key to avoiding traveler’s diarrhea is being proactive - think about where you’re going, research, and prepare! There are supplements I take to prevent illness, supplements I bring with me for defense in case I start feeling sick, and hygiene practices I follow, too.
Supplements I Use When Traveling To Keep My Gut Happy
When I’m travelling, I always take a probiotic. My favorites are Floramyces (which contains the yeast Saccharomyces boulardii) or UltraFlora Acute Care (this one blends S. boulardii with Bifidobacterium and Lactobacillus). I take 1 capsule of either, 1-2 times daily.
I also take Biocidin Advanced Formula Liquid to help boost my immunity. I start with 3 drops per day and work up to 5-10 drops twice daily.
Finally, I always take an Adaptogen blend. Adaptogens are herbs that help mitigate the stress of traveling. Yes, traveling is fun - but it is also hard on our bodies! Moving through time zones, awkward sleep schedules, and even just enjoying all the “newness” are all registered as stress to our bodies. I like blends that contain herbs like rhodiola for emotional and mental stress and eleuthero for physical stamina. NanoMojo Liquid and HPA Axis Homeostasis are my two go-tos.
Don’t Eat That!
Hygiene practices are so important for avoiding traveler’s diarrhea.
I always carry hand sanitizer with me - but not the conventional kind! Commercial hand sanitizers are full of BPA and other chemicals. Instead I make my own from aloe vera gel with lavender and tea tree essential oils, plus some Silvercillin. If you don’t want to make your own, this is good alternative. And of course - wash your hands with hot soap and water whenever you can.
Only drink bottled water - and never get ice! (Yes, even on the plane and in fancy restaurants!)
Avoid salad and uncooked veggies - especially lettuce. Cooked veggies (and cooked, hot food in general) are better when traveling. Worried about missing your greens? I bring a greens powder with me and mix it with bottled water. This one is my favorite.
Make sure you wash any produce you buy. As tempting as it is, don’t eat fruit straight from the farmer’s market cart. Wash it with a non-toxic fruit and veggie disinfectant first!
When eating out, look for food carts and restaurants with long line and plenty of locals.
Do This If You Feel Something Coming On
The minute I start to feel “off” - fatigued, grumbling stomach, or even a headache - I switch from my prevention to my treatment protocol.
I up the Biocidin Liquid to 10 drops, 3x per day.
I double up the probiotic.
I add in Oregano Oil Gelcaps for several days - 2 caps 3x daily.
And if diarrhea strikes? I go to a classic Chinese remedy called Huang Lian Su. It’s a blend of berberine-containing herbs that always works for me. I use 4-5 tablets, 3-4 times daily.
Happy Trails To You!
I hope these suggestions helps ease your fears about traveler’s diarrhea - and allow you to travel the world without getting sick!
And if you think food poisoning is at the root of your SIBO or gut problems, I hope you’ll consider working one-on-one with me to get it resolved. There is hope for overcoming gut problems - even one you’ve had for years! You can book a free consult with my team anytime. We’d love to help you!
Why Your Gut Health and Microbiome Make-or-Break Your Hormone Balance
Acne worse than puberty, ten pounds that won’t budge, a period-induced mood swing that turns you into a totally different person-- these are sure signs your hormones are out of whack. The solution to hormone problems like these seems obvious: Fix your hormones.
But what if I told you that the first step to balanced, happy hormones (and clear skin, easy, regular periods, a healthy weight, and even-keeled moods) isn’t about estrogen, progesterone, or testosterone?
I’m going to let you in on a big secret about female hormones: They never break in isolation.
What does that mean? Simply that if something is not right with your hormones, it’s a sure sign that something ELSE is not working right in your body that is causing the hormone problems. If you’re having symptoms caused by imbalanced hormones, we have to do more than just treat the symptoms - and we even have to do more than just treat the hormone imbalance. (Prescribing artificial hormones is NOT the answer).
We have to go back even further and find out: What caused the hormone imbalance in the first place?
Finding and addressing the root cause of your hormone imbalance is the MOST important step to achieving hormone balance for life.
And 9 times out of 10, when we do the careful detective work to find the real root cause behind hormone imbalance, it’s actually related to gut health.
I know it sounds a little odd at first - but the health of our gut is actually closely tied to our hormone health. In this post, I’m going to explain the link between our gut and hormone health, and what you can do to optimize both.
The Gut-Hormone Dream Team
The gut and our hormones are meant to be in communication. They support each other and work together to make our body run smoothly. In fact, our intestinal cells have special receptors for hormones that allow them to detect hormonal shifts.
It’s intuitive that our hormone and gut interact, too - even women with symptom-free periods will report noticing slight changes in their bowel patterns before and during their menstrual cycle.
Both estrogen and progesterone impact gut motility & peristalsis - the rhythmic movement of the intestines that moves food from your stomach down through your intestines and eventually out of your body. Estrogen and progesterone play opposing roles in motility. Progesterone slows down motility in the gut by relaxing smooth muscle and slowing transit time (the time it takes for food to move out of your body). Even women without IBS or other digestive issues are more likely to feel mildly constipated, or just more “full” during the week prior to the period, when progesterone levels peak.
Estrogen, on the other hand, increases contractions of the smooth muscle in the intestines. When estrogen levels are just right, this helps keeps things moving. Estrogen also increases the diversity of your microbiome, which is a good thing for immune health. Estrogen levels drop off suddenly, twice, during a normal menstrual cycle: once right before ovulation, and again just prior to your period starting. This can cause spasm and fast motility in the digestive tract, which can cause diarrhea at these times (even in healthy women). For the same reason (sudden, dramatic drops in estrogen levels), this can also happen during perimenopause and menopause, too.
Pregnant women experience an increase in progesterone in early pregnancy and then again in the third trimester - this is responsible for the constipation so many women experience during pregnancy. The excess progesterone can also cause the sphincter in the upper GI tract to loosen, leading to heartburn and reflux.
When estrogen and progesterone are in balance, you’ll tend to have normal motility most of the time - neither constipation or diarrhea. (Unless you also have some gut infections like SIBO, Candida, or parasites….then you could still have constipation.)
The Estrobolome
Our gut and hormones do more than just “talk”-- your gut microbiome also regulates estrogen. The estrogen-regulating function of specific bacteria in the microbiome is called the “estrobolome.”
The estrobolome is really important to keeping healthy estrogen levels in the body -- but to understand why, you need to know how the estrogen cycle works. Here’s how it happens in a healthy system:
- Estrogen is produced in the ovaries (but also in the adrenal glands and adipose tissue to a lesser extent)
- Estrogens circulate in the blood, making their way to tissues in the breasts, brain, bones, uterus and elsewhere
- Eventually, the estrogens travel to the liver, where they are broken down and deactivated
- Detoxified estrogens are deposited in bile which is secreted into the intestines, and exits the body with the stool.
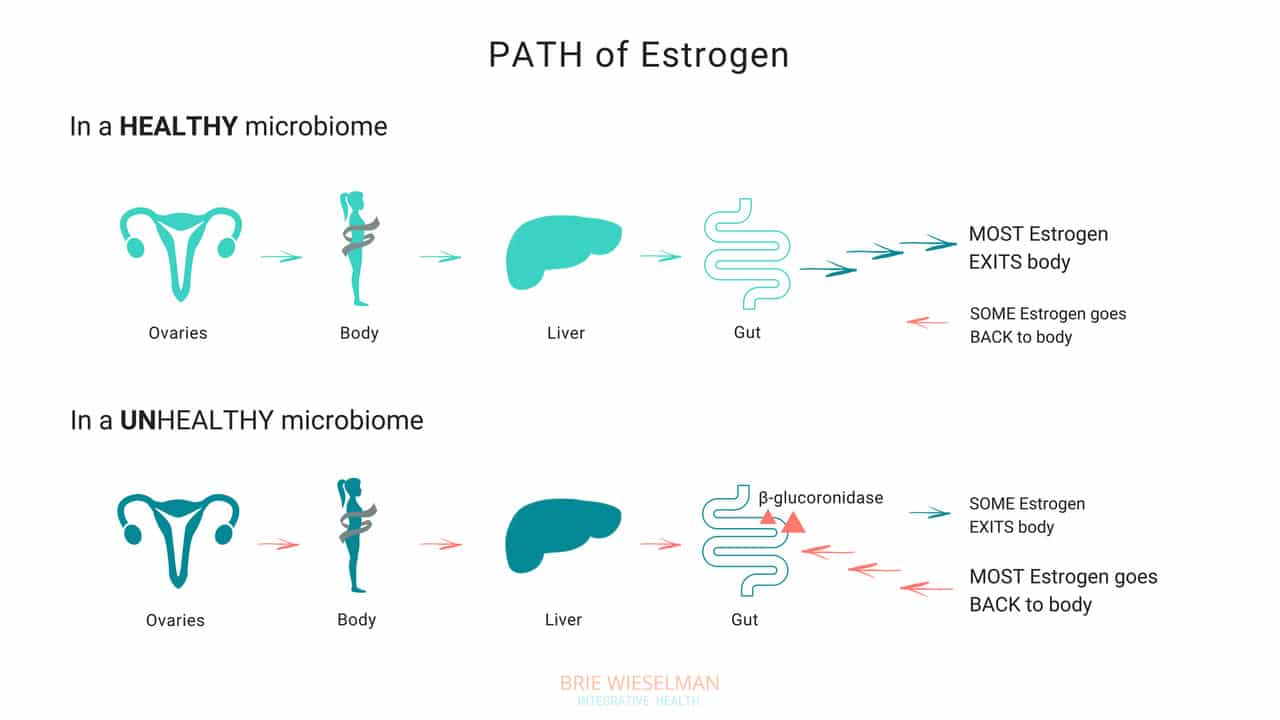
So, where does the gut come in? The gut - or more specifically, the estrobolome - regulates the amount of estrogens circulating in the bloodstream through the creation of β-glucuronidase, an enzyme which breaks down estrogen into to its “free”, or biologically active form.
But that isn’t all the gut does - it can also create its own estrogen, too!
Bacteria can manufacture estrogen-like compounds from foods that we eat. For example, lignans, found in plants like flax seeds, are converted into estrogen-like compounds when acted on by bacteria in the gut. On their own, they don’t have any hormonal properties, but once converted the can either promote uptake of our own more potent estrogens into receptor sites, or can compete for the same receptor sites,.
Newer research also suggests that the microbiome (and also specific types of probiotics) can produce its own estrogen and also signal glands around the body to produce it. We don’t yet fully understand exactly which strains of bacteria are responsible for all of these hormone modulating roles, but we do know that we want good overall proliferation, and greater species diversity.
When Things Go Wrong
The gut and your hormones are closely linked. You can see that both the gut and the hormone systems depend of each other to work properly - and when something goes wrong with either one, it spells trouble for the other.
Problems in the gut-hormone relationship usually start with the gut - but once the delicate balance is thrown off, it’s hard to know where to pin the blame. Imbalanced hormones cause gut problems, and gut problems cause imbalanced hormones.
Here are just some of the ways gut problems can lead to hormone imbalance:
Leaky Gut Syndrome: Leaky Gut Syndrome (aka Increased Intestinal Permeability) occurs when the tight junctions between cells in the intestine become “leaky” and allow toxins called LPS (which are fragments of dead bacterial cell walls) to pass from the intestine, into the bloodstream, and circulate through the body. It sounds crazy, but it’s actually common and causes a wide range of symptoms.
If you have leaky gut syndrome (with or without symptoms), you are more vulnerable to developing hormonal imbalances. Why? Because leaky gut causes widespread inflammation throughout the body. LPS is known to cause inflammation in any tissue that it comes into contact with, and in the ovaries, the result is suppressed progesterone production. (Women with higher levels of LPS in the blood had elevated markers of inflammation in fluid inside the ovary (follicular IL-6), and correspondingly low progesterone production.)
Studies show that infections, allergic reactions, being born by cesarean section, and even chronic stress can all cause inflammation in the gut, as well. And inflammatory conditions like obesity and inflammatory bowel disease are associated with disrupted menstrual cycles and infertility.
If you’re not having digestive symptoms like bloating, diarrhea, or constipation, you may think you don’t have leaky gut syndrome - but leaky gut may not show up as digestive symptoms, depending on the person. Even without digestive symptoms, the “silent” inflammation caused by leaky gut affects nearly every other aspect of health - especially our hormones.
Gut Dysbiosis: Your intestines are filled with trillions of bacteria, fungi, and even some viruses, that are all collaborating to keep your system running smooth and healthy. These bacterial cells and their genes are called your microbiome, and they live not just inside the intestines, but on every surface of your body, from your skin, to your eyes, your lungs, vaginal walls, and bladder. When the microbiome gets disturbed and the type or number of bacteria is damaged, we call it gut dysbiosis.
Along with your brain, your microbiome regulates the expression of your hormones, and can restrict or promote hormone production elsewhere in the body. The bacteria in your microbiome are like air-traffic control for hormones. In addition to signalling other glands in the body to dial up or down the volume on hormone production, your gut flora regulate hormone metabolism post-production, by either helping (or hindering) detoxification of already-used hormones, when they are being cleared from your system to make way for new fresh hormones.
To work properly, your microbiome needs the right bacteria, in the right amount. When the type or number of bacteria gets messed up (from something like poor diet & stress, an infection or parasite, or even just a course of antibiotics) your gut can no longer perform it’s hormone-regulating functions properly.
Increasing reactions to food, bloating, skin outbreaks, constipation, stubborn weight that won’t budge despite your best efforts, and even heavy periods— can all be signs that your microbiome is compromised and you’re unable to properly metabolize hormones like estrogen in the gut. Ultimately, this causes a build up of hormones in your system, which shows up as worsening of your PMS, period symptoms, or menopausal symptoms, and leaves you bloated and moody.
Estrobolome Dysfunction: Remember, the estrobolome are the specific bacteria in the microbiome responsible for regulating estrogen in the body through the production of the enzyme β-glucuronidase. Disruption of the estrobolome are really a type of dysbiosis. The estrobolome can be damaged in the same way the rest of the microbiome gets hurt: common triggers are stress, poor diet, and especially antibiotic use.
If the estrobolome bacteria become overgrown, the result is too much beta-glucuronidase being made. This causes already-detoxified estrogen to be reabsorbed and recirculated, in really high levels. This leads to a state of estrogen dominance. And estrogen dominance creates all kinds of chaos - PMS, cramps, fibroids and cysts, endometriosis, PCOS, heavy bleeding, infertility, a zapped sex drive, and weight gain. And of course, it can increase the risk of certain types of breast and uterine cancers.
And while it’s clear that we don’t want gut bacteria producing too much beta-glucuronidase enzyme, we actually don’t want them under-producing it either! When women have extremely low microbial diversity or even just extremely low levels of bacteria in the gut (think: excessive antibiotic use), the decrease in beta-glucuronidase causes a reduction in circulating free estrogens. Excess estrogen isn’t a good thing, but insufficient estrogen levels, especially in post-menopausal women, isn’t good for our health either! Estrogen is critical for maintaining healthy brain cognition, bone density, gut health, and cardiovascular health.
It isn’t just these gut problems that could be causing your hormone issues. The gut-hormone connection is a two-way street: here are some of the ways imbalanced hormones can wreak havoc on your gut health:
- Gallstones - women get gallstones twice as often as men! Estradiol (one of the types of estrogen) increases cholesterol levels in bile produced in the liver. (Cholesterol is the building block of our reproductive hormones, so when they are detoxified and broken down, cholesterol is released.) This increased saturation slows bile flow, which can lead to more stone formation.
- Leaky Gut - While inflammation caused by leaky gut can lead to hormone imbalances, low estrogen levels can also contribute to leaky gut. The epithelial layer of the intestinal wall needs estrogen to and keep it healthy and elastic. Leaky gut has been associated development of food sensitivities, autoimmune diseases, weight gain, acne, depression and anxiety, as well as almost every chronic illness you can think of.
- IBS - researchers know that estrogen and progesterone levels have an impact on the development of IBS (Irritable Bowel Syndrome). Symptoms of IBS include diarrhea, constipation, bloating, pain, and food intolerances.
Here’s the bottom line: if you want healthy hormones, you have to fix your gut!
Healthy Gut, Healthy Hormones
We know that we need a healthy gut to get healthy hormones - but what messed up your gut in the first place?
It’s a fair question, and not always easy to unravel. These are the most common causes for gut problems I see in my clinic - but there are many more (and most people have more than one contributing!)
Antibiotics: A single dose of the antibiotic Augmentin can kill off up to 90% of your gut flora - and most people are prescribed a 5-day course! Gut flora will regrow, (although it can take up to a year) but what types take hold and flourish impacts every aspect of our health. Generally we lose lactic-acid-producing species (like L. Acidophilus) first. This causes pH to go up in the intestines. Good colonic bacteria flourish in a more acidic environment, so in a less acidic environment, unfavorable strains can grow.
Toxins: Pesticides, herbicides, glyphosate from GMO corn and other foods, environmental chemicals, infections, and even stress can negatively shift the microbiome.
Diet: Eating a diet low in fermentable fibers and resistant starches (found in veggies, fruits, nuts, seeds, legumes, and grains) will also decrease bacterial diversity. Dairy, sugar, and gluten are major culprits in promoting bacterial imbalances.
The Pill: Contraceptive pills damage your microbiome as much as antibiotics do! The pill is known to promote candida overgrowth and SIBO (small intestine bacterial overgrowth) as well. Recent research has linked oral contraceptive use to development of inflammatory bowel diseases such as Crohn's Disease and Ulcerative Colitis, too.
The good news is there is a lot we can do to support better gut health - leading to better hormone health.
The best ways to support a healthy microbiome for healthy hormones, is through a diverse whole food diet, optimizing digestion, and taking steps to lower inflammation.
- Eat fermented foods - Sauerkraut, yogurt, kefir, kombucha, etc.
- Eat prebiotics/fiber - Found in root vegetables, flax seed, psyllium, beans, seeds, nuts, fruits and veggies. Women who eat more fibers from plants clear greater levels of estrogen in their stool.
- Take probiotics - In particular, Lactobacillus Acidophilus helps lower beta-glucuronidase!
- Optimize the environment of your digestive tract so good bacteria flourish there - This is similar to prepping the soil in your garden beds. Digestive secretions like pancreatic enzymes, stomach acid, and bile help optimize the conditions in the gut to promote the desirable bacteria. Taking these supplementally if you are deficient can help prime the gut for healthy colonization.
Get Your Gut & Hormones Humming
Every woman’s health is unique - but if a woman is having hormone symptoms, it almost always comes back to gut health! Heavy periods, adult acne, and PMS may not seem like they are related to your gut, but they so often are! That’s why I always test and treat the gut alongside hormone balance problems in my clinic.
Remember, our hormones don’t break in isolation! It’s almost always a sign of a problem somewhere else in the body. If you are struggling with your hormones, don’t forget to consider your gut health!
I hope this article and my suggestions for optimizing gut health help you. Need more help unraveling the root cause of your hormone issues? Want to run the right testing, so that you can really know for certain, what’s going on with your hormones and gut? I love to help women like you get back to radiant health so they can live big! If you’re interested in learning more about how I do this, you can book a free 20-minute prospective patient call here.